Abstract
Background
Tibia vara, or Blount’s disease, is a pathologic angular deformity of upper tibial physis causing a bow leg deformity. Adolescent Blount’s disease may be unilateral or bilateral and is diagnosed during or just before the adolescent growth spurt. In addition to predisposing genetic factors, biomechanical overload of the proximal tibial physis causes asymmetric growth leading to a varus deformity.
Surgical intervention is usually required for adolescent Blount’s disease. Hemiepiphysiodesis has had some success in arresting or correcting the deformity. Tibial osteotomy can achieve correction acutely with internal or external fixation or gradually with external fixation.
This article reports the outcomes of correcting adolescent tibia vara with a proximal opening wedge osteotomy (POWO) and internal fixation in nine patients with a primary diagnosis of Adolescent Blount’s Disease.
Methods
We conducted a retrospective review of patients treated with POWO between April 2007 and July 2015. Fifty charts were selected using ICD9 codes for tibia vara and CPT codes for osteotomy. Nine patients (11 tibia) meeting eligibility criteria were identified. In addition to pre-operative data; operative factors, such as blood loss; and post-operative outcomes such as radiographic accuracy of correction, time to healing, time to full weight-bearing, number of office visits and complication rates were collected.
Results
Pre-operative radiographic measurements showed the varus deformity was primarily tibial. Post-operative correction demonstrated a mean correction of 17.64° (range, 7°-26°). Patients returned to full weight bearing status around 67 days after surgery and required very few follow-up visits during the course of treatment. Three of nine patients experienced complications including seroma requiring drainage, metallosis mistaken for infection leading to hardware removal, and a wound abscess treated with antibiotics (one patient each). No patients lost correction, experienced nerve palsy, compartment syndrome nor complained of leg length discrepancy.
Conclusions
Proximal opening wedge osteotomy (POWO) is a reproducible, safe and effective technique for correction of adolescent tibia vara, with potential advantages of fewer return visits and sooner return to weight bearing than external fixation. In select patients, it is a useful alternative to external fixation or closing wedge osteotomy.
Level of Evidence: IV
Keywords: adolescent, blount’s disease, tibia vara, internal fixation, proximal opening wedge osteotomy
Introduction
Tibia vara, or Blount’s disease, is a pathologic angular deformity of the lower extremity focused at the upper tibial physis causing a bow leg deformity. The pathophysiology of Blount’s disease is thought to be due to improper distribution of biomechanical forces and predisposing genetic factors. Biomechanical overload of the proximal tibial physis causes asymmetric growth leading to a pathologic varus deformity1,2. Blount’s disease generally presents in two distinct age groups: infantile and adolescent. Adolescent Blount’s disease may be unilateral or bilateral and is diagnosed during or just before the adolescent growth spurt. Blount’s disease more commonly affects African-Americans and those with a body mass index (BMI) >40. The increase in body weight seen in individuals with Blount’s disease creates an excess force on the posteromedial portion of the proximal tibial physis. This compressive force leads to relative growth inhibition, as described by the Heuter-Volkmann principle, creating a varus deformity1,3,5. The deformity may be exacerbated by varus moments which result from the gait pattern of patients with increased BMI and thigh girth attempting to avoid contact between the thighs as described by Davids et al.1. Often times there may be associated deformities of the distal femur (varus or valgus) and the distal tibia6,7.
Surgical intervention is usually required for adolescent Blount’s disease. For the growing child with mild to moderate deformity, hemiepiphysiodesis has had some success in arresting or correcting the deformity. Tibial osteotomy is generally required in those with severe deformity or those nearing skeletal maturity. Tibial osteotomy can achieve correction acutely with internal or external fixation; or gradually with external fixation. Previous studies have reported success in the treatment of tibia vara with osteotomy with either gradual or acute correction and various forms of external fixation8,18. In this article, we will report the outcomes of correcting adolescent tibia vara with a proximal opening wedge osteotomy (POWO) of the tibia and internal fixation in a patient population with the primary diagnosis of Adolescent Blount’s Disease.
Methods
After Institutional Review Board approval, 55 patient records were identified using ICD9 codes for Tibia Vara and CPT codes for osteotomy for the peroid April 2007 to July 2015. Retrospective chart review was performed. Inclusion criteria included primary diagnosis of adolescent Blounts, correction by POWO and follow-up to radiographic union. Exclusion criteria were insufficient follow up, inadequate radiographs to assess pre-operative deformity or postoperative correction, patients with a primary diagnosis infantile Blount’s, or diagnosed with tibia vara secondary to another pathophysiologic process.
Charts were reviewed for: the age at which the patient underwent surgical correction for tibia vara; estimated blood loss during the procedure; duration of surgery; time to full weight bearing status; weight at the time of procedure; weight at time of full weight bearing status; number of office visits from the time of surgery to full weight bearing status and time to last follow-up. The length of time until full weight bearing status was determined by the documentation by the primary surgeon stating that patient was able to fully bear weight without any limitations. Complications were described in one of the following categories: wound problems such as dehiscence or cellulitis, and deep infection; nerve injuries; nonunion; malunion; compartment syndrome; symptomatic limb length discrepancy that required long term use of a shoe insert; and need for reoperation secondary to infection, or need of realignment.
All radiographic measurements were performed by an independent observer. Seven full length lower extremity weight bearing films were selected at random to be reviewed by the pediatric orthopedist. Angulation measurements of preoperative and postoperative MAD, MPTA and LDFA were in good agreement with an intraclass correlation coefficient varying between 0.97 (95% CI, 0.87-0.99) and 1.0(95% CI, 1.0-1.0). Patients had preoperative and follow-up full-length standing anteroposterior films. Special care was taken to ensure the patients’ pelvis and femoral heads were adequately visualized with their knees in full extension and patella directed anteriorly for proper radiographic analysis. Analysis of frontal plane radiographs consisted of measurement of the lateral distal femoral angle (LDFA), the medial proximal tibial angle (MPTA), mechanical axis (MA) and mechanical axis deviation (MAD). These measurements were made preoperatively and postoperatively at the latest follow-up. The degree of correction was calculated by subtracting the MA at the latest follow-up from the preoperative MA.
Deformities were corrected acutely with a proximal opening wedge osteotomy with internal fixation using either a plate incorporating a block (Puddu, Arthrex, Naples, FL) or a locking plate designed for the proximal tibia (Tomofix, Synthes, West Chester, PA). The osteotomy was generally oriented obliquely toward the proximal tibia-fibula joint leaving the lateral cortex intact for stability. A fibular osteotomy is not performed. The osteotomy was gradually opened while monitoring the position of the weight bearing axis by using a bovie cord positioned over the femoral head and ankle. The goal is to recreate a mechanical axis that passes through the middle of the knee erring on the side of medialization. A piece of tricortical iliac crest allograft is fashioned to fit snugly into the gap and this is supplemented with cancellous allograft chips. The plate is then applied medially to stabilize the osteotomy further. The osteotomy was generally combined with a prophylactic anterior compartment fasciotomy performed through the same incision and placement of a drain (figure 1A-C). No postoperative immobilization was used and patients were made touch down weight bearing immediately with progression to full weight bearing between week 6 and week 10 postoperatively. Patients were typically left with intentional residual varus in order to improve ambulation and compensate for their large thigh girth.
Figure 1:
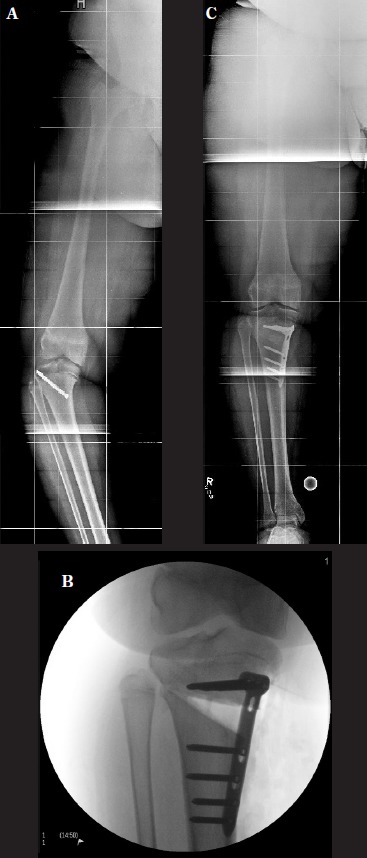
A. Pre-operative long leg radiograph reveals persistent tibia vara after failed screw epiphysiodesis. B. Intraoperative fluoroscopic image reveals completed osteotomy fixed with locking plate before placement of structural and morselized allograft. C. 10 week postoperative long leg radiograph reveals healed osteotomy.
Patient Results
Fifty five patients were initially identified. Nineteen had originally been diagnosed with infantile Blount’s, 14 received other treatment for adolescent Blount’s (e.g.: femur osteotomy or acute correction with monolateral external fixation or external fixation with Taylor Spatial Frame), and five received tibial osteotomy for other indications (e.g.: familial hypophosphatemic rickets), eight had inadequate medical records. The remaining nine had POWO (11 tibiae) (Figure 2). The mean age at operation was 15 years and mean preoperative weight was 137.1 kg (Table 1).
Figure 2:
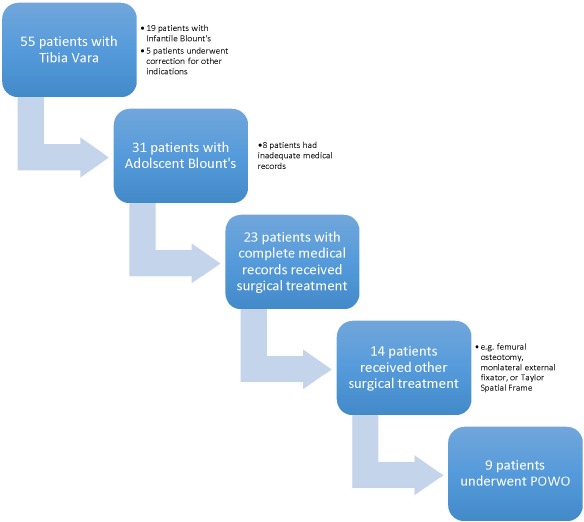
POWO; Proximal Opening Wedge Osteotomy
Table I.
Pre-Operative Radiographic Measurements
| POWO (n=11) | ||
|---|---|---|
| Variable | Mean | Range |
| MA, degree | 24.64 | 15.0 - 36.0 |
| MAD, cm | 8.87 | 4.3 - 13.2 |
| LDFA, degree | 95.82 | 90.0 - 101.0 |
| MPTA, degree | 79.00 | 70.0 - 84.0 |
| Age, years | 15.01 | 11.9 - 19.1 |
| Weight, kg | 137.1 | 72.0 - 184.3 |
POWO, proximal opening wedge osteotomy with internal fixation; MA, mechanical axis; MAD, mechanical axis deviation; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Radiographic Results
Pre-operative radiographic measurements (Table 1), showed the varus deformity was primarily in the tibia. Post operative correction as seen in Table 2 demonstrated a mean MA 7° varus and MAD of 2.48 cm medial, and mean correction of 17.64° (range, 7°-26°). Mean MPTA of 89.54° (range, 84.0° - 94.0°) and LDFA of 93.64° (range, 85.0° - 98.0°). In each case, MPTA and LDFA did not show significant unintended residual deformity in our sample.
Table II.
Post-Operative Radiographic Measurements
| POWO (n=11) | ||
|---|---|---|
| Variable | Mean | Range |
| MA, degree | 7.00 | -2.0 - 15.0 |
| MAD, cm | 2.48 | 0.5 - 4.9 |
| MPTA, degree | 89.54 | 84.0 - 94.0 |
| LDFA, degree | 93.64 | 85.0 - 98.0 |
| Correction, degree | 17.64 | 7.0 - 26.0 |
| Correction, cm | 6.39 | 2.6 - 9.4 |
POWO, proximal opening wedge osteotomy with internal fixation; MA, mechanical axis; MAD, mechanical axis deviation; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle.
Clinical Results
Our group returned to full weight bearing status around 67 days after surgery. There were very few follow-up (average 2.55/patient) visits during the course of treatment and patients also experienced an average weight loss of 0.84 kg as a group (Table 3). Mean blood loss 168.64 mL, and mean duration of surgery was one hour and fifty-two minutes. Three of nine patients experienced complications including seroma requiring drainage, metallosis mistaken for infection leading to hardware removal, and a wound abscess treated with antibiotics (one patient each). No patients lost correction, experienced nerve palsy, compartment syndrome nor complained of leg length discrepancy.
Table III.
Follow up Variables
| POWO (n=11) | ||
|---|---|---|
| Variable | Mean | Range |
| Time to last follow up, years | 1.45 | 0.19 - 5.38 |
| Follow up visits | 2.55 | 2 - 3 |
| Time to full weight bearing status, days | 66.91 | 33 - 91 |
| Blood loss, mL | 168.64 | 10.0 - 1000 |
| Surgery Time, hr:min | 1:52 | 0:38 - 2:40 |
| POWO (n=9) | ||
| Variable | Mean | Range |
| Weight at full weight bearing status, kg | 132.4 | 69.7 - 162.4 |
| Weight change during treatment, kg | -0.84 | -5.0 - 4.0 |
POWO, proximal opening wedge osteotomy with internal fixation.
Discussion
The obesity epidemic assures a continued need to correct adolescent tibia vara. The goals of reestablishing normal joint alignment, correcting the gait pattern, and possibly delaying the onset of osteoarthritis can be pursued using a variety of correction techniques, but further comparative studies are needed. We have described the outcomes of POWO and found that similar radiographic outcomes could be obtained with POWO compared to other techniques with few clinic visits and early return to full weight bearing. Further, POWO patients did not experience weight gain during the treatment period, a significant positive in this already overweight population.
Gilbody et al. published a systematic review using two major medical literature databases comparing acute and gradual correction after a single level tibal osteotomy for primary treatment with children with idiopathic tibia vara and concluded there was weak evidence that the Taylor Spatial frame provides a more accurate correction of the MA. In this review, there were five studies that reported gradual correction with external fixation with a mean MA ranging from 1° to 7.5° of valgus19. The final range of MA for the POWO group in our study was within this range.
Surgeons may be reluctant to perform POWO in adolescent tibia vara due to concerns about compartment syndrome, neurovascular injury and wound complications related to obesity and ability to achieve and maintain satisfactory correction8,18,22. Most patients in this series were obese. We did have three wound complications, with two requiring re-operation, but none compromising the final result. Acute correction has been implicated as being more likely to result in compartment syndrome and neurovascular compromise,19,23, but in our series all patients with POWO had prophylactic fasciotomy and there were no compartment syndromes or neurovascular complications in either group. Regarding correction, the senior author prefers to leave patients with slight varus in order to help with gait, our POWO patients maintained correction to healing with no loss of fixation.
Advantages of POWO, as compared to alternative methods such as gradual correction with Taylor Spatial, included fewer return visits and earlier time to weight bearing, avoidance of pins, as well as avoidance of a mandatory second procedure for Ex-Fix removal. Avoiding weight gain during treatment could prove to be very impactful, as a prior study has shown that patients gain an average of 3.7 kg over the course of Ex-Fix treatment24.
Despite some of the potential advantages of POWO, it does have limitations. More severe deformities may make the size of wedge required impractical. Also, this technique does not allow for correction of additional deformities such as leg length difference and rotational deformities.
Limitations of the current study include the retrospective nature with lack of standardized protocols for weight bearing or specific selection criteria for particular procedures. In addition, the inclusion criteria utilized to select a consistent patient population resulted in small numbers.
This technique is a valuable treatment option for surgical correction of Adolescent Blount’s Disease and it is a useful alternative to an external fixator or closing wedge osteotomy in selected patients. This technique was performed on 11 knees with tibia vara, and it was completely successful in all cases. In conclusion, POWO is a reproducible, safe and effective technique for correction of adolescent tibia vara, with potential advantages of fewer return visits and sooner return to weight bearing.
Source of Funding
This study was supported internally by the University of at Birmingham.
References
- 1.Davids JR, Huskamp M, Bagley AM. A dynamic biomechanical analysis of the etiology of adolescent tibia vara. Journal of pediatric orthopedics. 1996 Jul-Aug;16(4):461–468. doi: 10.1097/00004694-199607000-00008. PMID 8784698. [DOI] [PubMed] [Google Scholar]
- 2.Henderson RC. Tibia vara: a complication of adolescent obesity. The Journal of pediatrics. 1992 Sep;121(3):482–486. doi: 10.1016/s0022-3476(05)81811-6. PMID 1517931. [DOI] [PubMed] [Google Scholar]
- 3.Bradway JK, Klassen RA, Peterson HA. Blount disease: a review of the English literature. Journal of pediatric orthopedics. 1987 Jul-Aug;7(4):472–480. PMID 3301898. [PubMed] [Google Scholar]
- 4.Greene WB. Genu varum and genu valgum in children: differential diagnosis and guidelines for evaluation. Comprehensive therapy. 1996 Jan;22(1):22–29. PMID 8654021. [PubMed] [Google Scholar]
- 5.Kling TF., Jr. Angular deformities of the lower limbs in children. The Orthopedic clinics of North America. 1987 Oct;18(4):513–527. PMID 3313160. [PubMed] [Google Scholar]
- 6.Sabharwal S, Zhao C, McClemens E. Correlation of body mass index and radiographic deformities in children with Blount disease. The Journal of bone and joint surgery. American volume. 2007 Jun;89(6):1275–1283. doi: 10.2106/JBJS.F.01135. PMID 17545431. [DOI] [PubMed] [Google Scholar]
- 7.Zionts LE, Shean CJ. Brace treatment of early infantile tibia vara. Journal of pediatric orthopedics. 1998 Jan-Feb;18(1):102–109. PMID 9449110. [PubMed] [Google Scholar]
- 8.Coogan PG, Fox JA, Fitch RD. Treatment of adolescent Blount disease with the circular external fixation device and distraction osteogenesis. Journal of pediatric orthopedics. 1996 Jul-Aug;16(4):450–454. doi: 10.1097/00004694-199607000-00006. PMID 8784696. [DOI] [PubMed] [Google Scholar]
- 9.de Pablos J, Franzreb M. Treatment of adolescent tibia vara by asymmetrical physeal distraction. The Journal of bone and joint surgery. British volume. 1993 Jul;75(4):592–596. doi: 10.1302/0301-620X.75B4.8331114. PMID 8331114. [DOI] [PubMed] [Google Scholar]
- 10.Fowler JL, Gie GA, Maceachern AG. Upper tibial valgus osteotomy using a dynamic external fixator. The Journal of bone and joint surgery. 1991 British Volume. Jul;73(4):690–691. doi: 10.1302/0301-620X.73B4.2071665. PMID 2071665. [DOI] [PubMed] [Google Scholar]
- 11.Ganel A, Heim M, Farine I. Asymmetric epiphyseal distraction in treatment of Blount’s disease. Orthopaedic review. 1986 Apr;15(4):237–240. PMID 3453930. [PubMed] [Google Scholar]
- 12.Gaudinez R, Adar U. Use of Orthofix T-Garche fixator in late-onset tibia vara. Journal of pediatric orthopedics. 1996 Jul-Aug;16(4):455–460. doi: 10.1097/00004694-199607000-00007. PMID 8784697. [DOI] [PubMed] [Google Scholar]
- 13.Kamegaya M, Shinohara Y, Shinada Y. Limb lengthening and correction of angulation deformity: immediate correction by using a unilateral fixator. Journal of pediatric orthopedics. 1996 Jul-Aug;16(4):477–479. doi: 10.1097/00004694-199607000-00010. PMID 8784700. [DOI] [PubMed] [Google Scholar]
- 14.Miller S, Radomisli T, Ulin R. Inverted arcuate osteotomy and external fixation for adolescent tibia vara. Journal of pediatric orthopedics. 2000 Jul-Aug;20(4):450–454. PMID 10912599. [PubMed] [Google Scholar]
- 15.Monticelli G, Spinelli R. A new method of treating the advanced stages of tibia vara (Blount’s disease) Italian journal of orthopaedics and traumatology. 1984 Sep;10(3):295–303. PMID 6519965. [PubMed] [Google Scholar]
- 16.Price CT, Scott DS, Greenberg DA. Dynamic axial external fixation in the surgical treatment of tibia vara. Journal of pediatric orthopedics. 1995 Mar-Apr;15(2):236–243. PMID 7745101. [PubMed] [Google Scholar]
- 17.Smith SL, Beckish ML, Winters SC, Beckish ML, Winters SC. Treatment of late-onset tibia vara using afghan percutaneous osteotomy and orthofix external fixation. Journal of pediatric orthopedics. 2000 Sep-Oct;20(5):606–610. doi: 10.1097/00004694-200009000-00011. PMID 11008739. [DOI] [PubMed] [Google Scholar]
- 18.Stanitski DF, Dahl M, Louie K, Dahl M, Louie K. Management of late-onset tibia vara in the obese patient by using circular external fixation. Journal of pediatric orthopedics. 1997 Sep-Oct;17(5):691–694. doi: 10.1097/00004694-199709000-00021. PMID 9592012. [DOI] [PubMed] [Google Scholar]
- 19.Gilbody J, Thomas G, Ho K. Acute versus gradual correction of idiopathic tibia vara in children: a systematic review. Journal of pediatric orthopedics. 2009 Mar;29(2):110–114. doi: 10.1097/BPO.0b013e31819849aa. PMID 19352233. [DOI] [PubMed] [Google Scholar]
- 20.Feldman DS, Madan SS, Koval KJ, Madan SS, Koval KJ. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. Journal of pediatric orthopedics. 2003 May-Jun;23(3):387–391. PMID 12724607. [PubMed] [Google Scholar]
- 21.Gordon JE, Heidenreich FP, Carpenter CJ, Heidenreich FP, Carpenter CJ. Comprehensive treatment of late-onset tibia vara. The Journal of bone and joint surgery. 2005 American Volume. Jul;87(7):1561–1570. doi: 10.2106/JBJS.02276. PMID 15995124. [DOI] [PubMed] [Google Scholar]
- 22.Sabharwal S. Blount disease. The Journal of bone and joint surgery. American volume. 2009 Jul;91(7):1758–1776. doi: 10.2106/JBJS.H.01348. PMID 19571101. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy JJ, Aruther MK, Davidson RD. Treatment of angular deformities of the tibia in children: acute versus gradual correction. Journal of surgical orthopedic advances. 2007;16(3):118–122. PMID. [PubMed] [Google Scholar]
- 24.Culotta BA, Gilbert SR, Sawyer JR, Ruch A, Sellers T. Weight gain during external fixation. Journal of children’s orthopaedics. 2013 Mar;7(2):147–150. doi: 10.1007/s11832-012-0468-1. PMID 24432073. [DOI] [PMC free article] [PubMed] [Google Scholar]


