H1N1pdm09 influenza A viruses lack extra-epitopic amino acid residues previously associated with reduced recognition by M158-66-specific CD8+ T cells. During >6 years of evolution, H1N1pdm09 virus accumulated alternative mutations outside the M158-66 epitope that did not reduce sensitivity to M158-66-specific CD8+ T cells.
Keywords: influenza A virus, H1N1pdm2009, CD8+ T-lymphocytes, escape, extra-epitopic amino acid residues
Abstract
Extra-epitopic amino acid residues affect recognition of human influenza A viruses (IAVs) by CD8+ T-lymphocytes (CTLs) specific for the highly conserved HLA-A*0201 restricted M158-66 epitope located in the matrix 1 (M1) protein. These residues are absent in the M1 protein of the 2009-pandemic IAV (H1N1pdm09). Consequently, stimulation with M1 protein of H1N1pdm09 IAV resulted in stronger activation and lytic activity of M158-66-specific CTLs than stimulation with seasonal H3N2 IAVs. During >6 years of circulation in the human population, descendants of the H1N1pdm09 virus had accumulated 4 other amino acid substitutions. However, these did not affect M158-66-specific CTL activation.
Influenza A virus (IAV) infections are an important cause of excess mortality during seasonal epidemics and pandemics [1–3]. Cross-reactive IAV-specific CD8+ T lymphocytes (CTLs) play an important role in viral clearance and reducing disease severity [4–6]. However, viral evasion from recognition by CTLs has been described [7] and includes mutations in epitopes at T-cell receptor contact residues and HLA-anchor residues, both of which are observed during evolution of seasonal IAVs [8, 9]. Recently, we described that also residues outside an epitope can affect recognition by influenza virus–specific CTLs. Extra-epitopic amino acid residues of human IAV signature (15V, 27R, 101R, 115I, and 121A) correlated with reduced activation and lytic activity of CTLs specific for the highly conserved and HLA-A*0201-restricted M158-66 epitope in the M1 protein of human H3N2 IAVs compared to its avian IAV counterpart. This human signature was present in all human IAV subtypes circulating before 2009 [10]. The M1 protein of the 2009 H1N1 pandemic (H1N1pdm09) IAV did not have this human signature and, therefore, we hypothesized that recognition of H1N1pdm09 influenza virus by M158-66-specific CTLs was not reduced [10]. The H1N1pdm09 pandemic was generally considered milder compared to previous pandemics [3, 11]. In particular, elderly persons were relatively resistant to infection [11] because they were previously exposed and developed antibodies to antigenically related H1N1 IAVs that circulated before 1957 [12, 13]. It was speculated that absence of the human signature in the M1 protein would render the H1N1pdm09 IAV more sensitive to M158-66-specific CTLs in HLA-A*0201+ individuals [10], which is in concordance with the observation that preexisting IAV-specific CTL immunity correlated with protection from disease severity caused by H1N1pdm09 IAVs [4, 5]. Moreover, the introduction of H1N1pdm09 IAV offered a unique opportunity to study the possible evolutionary accumulation of these or other extra-epitopic amino acid residues in a human influenza virus. After >6 years of circulation in the human population, descendants of the H1N1pdm09 IAV (H1N1pdm09/2016) have acquired mutations in the M1 protein outside the M158-66 epitope, albeit at other positions than those previously described [10].
Here, we investigated whether the absence of extra-epitopic amino acid residues associated with reduced CTL recognition in the H1N1pdm09 IAV enhanced M158-66-specific CTL recognition. In addition, we investigated if >6 years of selective pressure exerted by M158-66-specific CTLs in the human population were responsible for the observed extra-epitopic mutations and reduced recognition by M158-66-specific CTLs.
MATERIALS AND METHODS
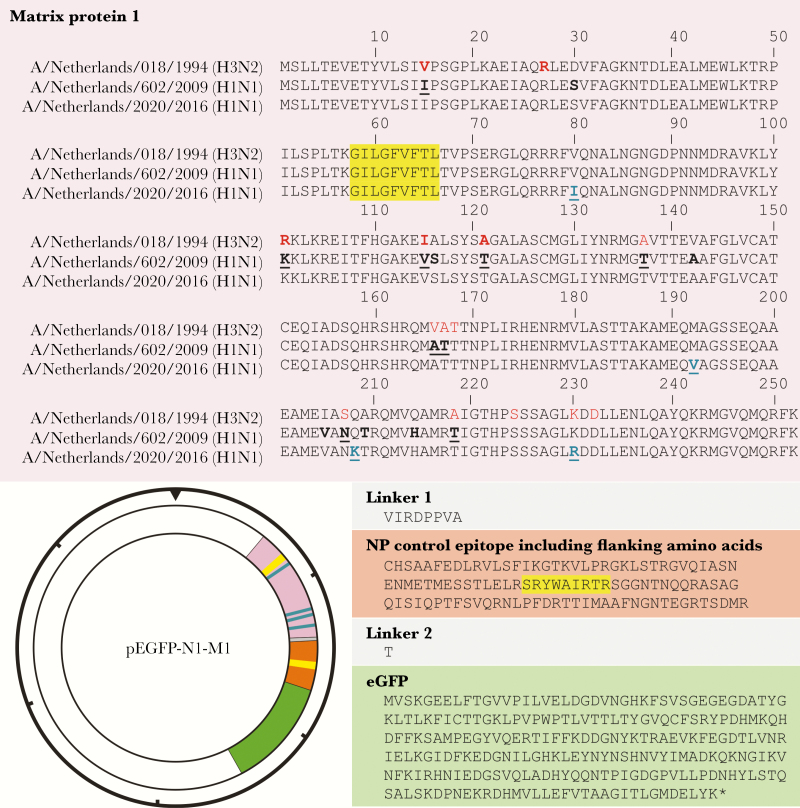
M1 amino acid sequences of seasonal H3N2 (A/Netherlands/018/1994, H3N2s1994) [10], H1N1pdm09 (A/Netherlands/602/2009), and descendants of H1N1pdm09 virus isolated in 2016 (H1N1pdm09/2016) were analyzed using the BioEdit software package version 7.2.5. The fluorescent antigen-transfected target cell (FATT)–CTL assay was used for the detection of lytic activity and activation of the M158-66- and nucleoprotein (NP)383-391-specific CTLs as described previously [10, 14]. In brief, in addition to the previously described M1(H3N2s1994)-NP-enhanced green fluorescent protein (eGFP) fusion plasmid [10], we constructed an M1(H1N1pdm09)-NP-eGFP and M1(H1N1pdm09/2016)-NP-eGFP plasmid. The M1(H3N2s1994) open reading frame (ORF) of the M1(H3N2s1994)-NP-eGFP plasmid was replaced by the ORF of the M1 protein of A/Netherlands/602/2009 or A/Netherlands/2020/2016 (representative descendant of H1N1pdm09 IAV), respectively, without their stop codons as described previously (Figure 1) [10]. These plasmids were used to transfect an HLA-A*0101/A*0201/B*0801/B*2705-positive B lymphoblastoid cell line as described previously [10]. The number of viable eGFP-positive cells was determined after 4 hours at 37°C. Quadruplicates of 1500 viable eGFP-positive cells were cocultured for another 3.5 hours with 80000 M158-66- or NP383-391-specific CTLs to assess the lytic activity of the CTLs using the following formula: 100 × [(number of viable eGFP-positive cells in the sample without effector – number of viable eGFP-positive cells in the sample with effector) / number of viable eGFP-positive cells in the sample without effector] [10].
Figure 1.
Amino acid sequences of viral matrix protein 1-nucleoprotein-enhanced green fluorescent protein (M1-NP-eGFP) fusion proteins and expression plasmid map. The amino acid sequence of the chimeric M1-NP-eGFP fusion construct is shown: M1 encoding sequences A/Netherlands/018/1994 (H3N2s1994), A/Netherlands/602/2009 (H1N1pdm09), and A/Netherlands/2020/2016 (H1N1pdm09/2016) (pink), NP (orange), eGFP (green), and linker sequences (gray), and M158-66 (GILGFVFTL) and NP383-391 (SRYWAIRTR) epitopes (yellow). Previously identified extra-epitopic amino acid residues of a human signature are indicated in bold red and additional extra-epitopic amino acid residues of a human signature are indicated in red [10]. Amino acid difference between the H3N2s1994 and H1N1pdm09 M1 proteins are indicated in bold, and those of avian/swine signature are bold underlined. Amino acid differences studied in this report between H1N1pdm09 and H1N1pdm09/2016 M1 proteins are indicated in blue, bold and underlined. These inserts were cloned into the pEGFP-N1 vector as indicated. The hash marks around the perimeter of the plasmid map indicate 1000-nucleotide increments.
To assess CTL activation, quadruplicates of 3000 viable eGFP-positive cells were cocultured for another 7 hours with 20000 M158-66- or NP383-391-specific CTLs and subsequently incubated with antibodies to CD3, CD8 (eBiosciences, Vienna, Austria), CD137 (BioLegend, London, United Kingdom), and CD107a (BD Biosciences, Breda, the Netherlands) labeled with PerCP-Cyanine5.5, Allophycocyanin, PECyanine7, and V450, respectively, and LIVE/DEAD Aqua Fixable Dead Cell Stain (L/D) (Invitrogen, Breda, the Netherlands) as described previously [10].
Data were analyzed using the independent-samples t test to calculate the respective P value between pairs of groups. These P values were then analyzed using the Benjamini–Hochberg method to correct for multiple hypothesis testing using a false discovery rate of 0.01 for all assays. Each experiment was performed at least twice. NP383-391-specific CTLs were used as an internal control as they display similar functional avidity as M158-66-specific CTLs.
RESULTS
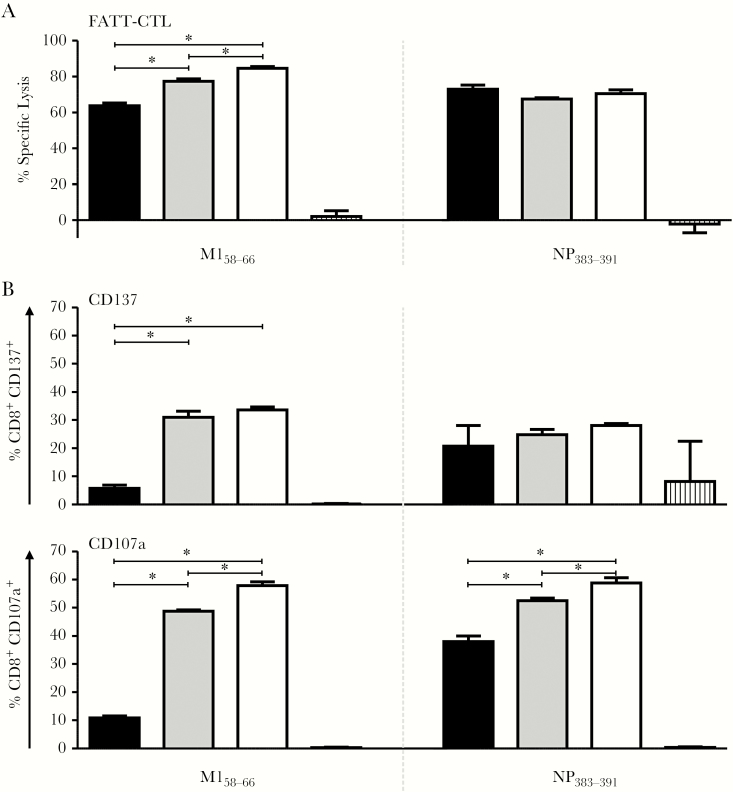
We previously reported that amino acid residues at positions 15, 101, 115, and 121 outside the M158-66 epitope in the M1 protein of H1N1pdm09 virus were of an avian-/swine-like signature, not associated with reduced recognition by M158-66- specific CTLs (Figure 1) [10]. So far, there is no evidence that the accumulation of mutations outside the M158-66 epitope that confer reduced recognition by M158-66-specific CTLs is an evolutionary trait [10]. The H1N1pdm09 virus completely replaced the previously circulating seasonal H1N1 IAV and continued to circulate during subsequent influenza seasons. To address the question if selective pressure exerted by M158-66- specific CTLs in previously infected HLA-A*0201-positive individuals (40% of the white population), has driven the accumulation of extra-epitopic mutations associated with reduced recognition by M158-66-specific CTLs, we compared the M1 amino acid sequences of various H1N1pdm09 descendant strains isolated in the 2015–2016 influenza season with that of the original H1N1pdm09 virus. Although the previously identified extra-epitopic amino acid residues associated with reduced M158-66-specific CTL recognition were absent in the M1 protein of H1N1pdm09/2016 viruses, 4 other fixed amino acid substitutions were observed at position outside the epitope (V80K, M192V, Q208K, and K230R) (Figure 1). Next, we wished to test the hypothesis that these amino acid substitutions could affect activation and lytic activity of M158-66- specific CTLs. To this end, matrix protein 1-nucleoprotein-enhanced green fluorescent protein (M1-NP-eGFP) plasmids were used in the FATT-CTL assay to monitor the lytic activity (Figure 2A) and activation (Figure 2B) of M158-66- and NP383-391- specific CTLs, as described previously [10, 14]. M158-66-specific CTLs displayed significantly higher lytic activity with target cells expressing the M1 protein of IAVs H1N1pdm09 or H1N1pdm09/2016 than with those expressing M1 protein of the H3N2s1994 virus (77.3%, 84.6%, and 63.8% respectively) (Figure 2A). The lytic activity of NP383-391-specific CTLs to all M1-NP-eGFP fusion proteins was similar (Figure 2A), indicating that the observed differences with M158-66-specific CTLs were not the result of differences in transfection efficiency of the respective plasmids used or protein expression. Upon stimulation with M1 protein of IAVs H1N1pdm09 or H1N1pdm09/2016, a significantly higher percentage of M158-66- specific CTLs expressed the activation marker CD137 (31% [H1N1pdm09] and 33.6% [H1N1pdm09/2016]) than after stimulation with M1 protein of H3N2s1994 (5.7%) (Figure 2B). A similar pattern was observed for the detection of the degranulation marker CD107a. Upon stimulation with M1 proteins of IAVs H1N1pdm09 or H1N1pdm09/2016, respectively 48.8% and 57.9% of the M158-66-specific CTLs expressed CD107a, which was significantly higher than after stimulation with M1 protein of H3N2s1994 (10.9%) (Figure 2B). Such differences were not observed for the NP383-391-specific CTLs, although CD107a expression was slightly higher after stimulation with M1 proteins of H1N1pdm09 and H1N1pdm09/2016 compared to stimulation with that of H3N2s1994 virus, but this difference was substantially smaller than that observed for the M158-66-specific CTLs (Figure 2B).
Figure 2.
Activation and lytic activity of M158-66- and NP383-391-specific CD8+ T lymphocytes (CTLs) after stimulation with matrix protein 1-nucleoprotein-enhanced green fluorescent protein (M1-NP-eGFP) transfected cells. M158-66- and NP383-391-specific CTLs were incubated with HLA-matched target cells transfected with chimeric M1-NP-eGFP fusion plasmids that encode the M1 protein of H3N2s1994 (black), H1N1pdm09 (gray) or H1N1pdm09/2016 (white) influenza A viruses, and lytic activity was determined by fluorescent antigen-transfected target cell (FATT)–CTL assay (A). In addition, expression of activation markers CD137 and CD107a by the respective CTLs was assessed (B). GFP (A) or mock (B) transfected stimulator cells served as a negative control (hatched bars). Data points represent the mean, and error bars indicate the standard deviation of quadruplicates (n = 4). * Indicates statistically significant differences between groups after correction for multiple hypothesis testing using a false discovery rate of 0.01.
Thus, activation and lytic activity of M158-66-specific CTLs against the M1 protein of H1N1pdm09 and H1N1pdm09/2016 virus was stronger than against the M1 protein of virus H3N2s1994. The newly identified amino acid substitutions outside the M158-66 epitope in the M1 protein of H1N1pdm09/2016 viruses did not affect activation or lytic activity of M158-66-specific CTLs.
DISCUSSION
In contrast to other IAVs that have circulated in the human population, the M1 protein of IAV H1N1pdm09 was of an “avian signature” and lacked extra-epitopic amino acid residues seen in human IAVs associated with reduced recognition by M158-66-specific CTLs [10]. Consequently, the activation and lytic activity of M158-66-specific CTLs upon stimulation with the M1 protein of H1N1pdm09 virus was stronger compared to stimulation with that of H3N2s1994 virus, which has reduced capacity to stimulate M158-66-specific CTLs compared to avian H5N1 virus [10]. The descendants of H1N1pdm09 virus accumulated extra-epitopic amino acid substitutions during their evolution in the years following the pandemic outbreak, but at other positions than those described previously for H3N2s1994 and historic IAVs. We hypothesized that selective immune pressure against the M158-66-epitope was responsible for driving the accumulation of these mutations. Because the M158-66 epitope is highly immunodominant [15] and its corresponding HLA*0201 allele has a high prevalence in the Caucasian population (>40%), selective immune pressure against the M158-66 epitope is likely to be high. However, the amino acid substitutions that accumulated in the M1 protein during >6 years of circulation and evolution in H1N1pdm09 descendant strains did not affect recognition by M158-66-specific CTLs. This suggests that for extra-epitopic mutations associated with reduced recognition by M158-66-specific CTLs to arise, IAVs need to circulate under M158-66-specific CTL immune pressure for extended periods. Alternatively, a reassortment event would allow descendants of H1N1pdm09 virus to acquire gene segment 7 encoding the M1 protein from seasonal H3N2 IAVs in order to escape the M158-66- specific CTL response.
To investigate if descendants of H1N1pdm09 virus had accumulated mutations in other CTL epitopes, we retrieved 24 functionally described epitopes from the Immune Epitope Database (www.iedb.org). Of these epitopes, 14 were present in the H1N1pdm09 IAV; of these 14, only the NA233-241 and overlapping NS122-130 and NS1123-132 epitopes displayed variability (Supplementary Table 1), which in the case of NA may have been caused by selective antibody pressure. Thus, so far descendants of H1N1pdm09 virus display minimal signs of escape from recognition by CTL to known epitopes.
Collectively, these results indicate that seasonal H3N2 and other historic human IAVs, which all share a common source for their M1 protein by genetic reassortment [10], may have benefited from extra-epitopic amino acid residues that allowed reduced recognition by M158-66-specific CTLs in previously infected HLA-A*0201-positive individuals. The M1 protein of H1N1pdm09 virus lacked these residues and indeed stimulated the M158-66-specific CTLs to a greater extent. This in turn, may have contributed to stronger CTL responses in immune HLA-A*0201-positive individuals and subsequently reduced disease severity and, potentially, limited spread of H1N1pdm09 virus in the human population. Finally, the extra-epitopic amino acid substitutions that have accumulated in the M1 protein of descendants of the H1N1pdm09 virus do not confer reduced recognition by M158-66-specific CTLs, and this immune adaptation may only be acquired after prolonged circulation of these viruses in the human population or by a genetic reassortment event.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. The authors thank David van de Vijver for technical advice.
Financial support. C. E. S. and G. F. R. received funding from European Union grant FLUNIVAC (project ID 602604). R. A. M. F., T. M. B., and M. I. S. received funding from the National Institute of Allergy and Infectious Diseases of the National Institutes of Health (contract number HHSN272201400008C).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Presented in part: Sixth European Scientific Working Group on Influenza Conference, Riga, Latvia, September 2017.
References
- 1. Palese P, Shaw ML.. Orthomyxoviridae: the viruses and their replication. Fields virology. 5th ed Vol. 2 Philadelphia, PA: Lippincott Williams & Wilkins, 2007:1647–89. [Google Scholar]
- 2. Murray CJ, Lopez AD, Chin B, Feehan D, Hill KH. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918-20 pandemic: a quantitative analysis. Lancet 2006; 368:2211–8. [DOI] [PubMed] [Google Scholar]
- 3. Mathews JD, Chesson JM, McCaw JM, McVernon J. Understanding influenza transmission, immunity and pandemic threats. Influenza Other Respir Viruses 2009; 3:143–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sridhar S, Begom S, Bermingham A, et al. Cellular immune correlates of protection against symptomatic pandemic influenza. Nat Med 2013; 19:1305–12. [DOI] [PubMed] [Google Scholar]
- 5. Hayward AC, Wang L, Goonetilleke N, et al. Flu Watch Group Natural T cell-mediated protection against seasonal and pandemic influenza. Results of the flu watch cohort study. Am J Respir Crit Care Med 2015; 191:1422–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang Z, Wan Y, Qiu C, et al. Recovery from severe H7N9 disease is associated with diverse response mechanisms dominated by CD8⁺ T cells. Nat Commun 2015; 6:6833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. van de Sandt CE, Kreijtz JH, Rimmelzwaan GF. Evasion of influenza A viruses from innate and adaptive immune responses. Viruses 2012; 4:1438–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Berkhoff EG, Geelhoed-Mieras MM, Fouchier RA, Osterhaus AD, Rimmelzwaan GF. Assessment of the extent of variation in influenza A virus cytotoxic T-lymphocyte epitopes by using virus-specific CD8+ T-cell clones. J Gen Virol 2007; 88:530–5. [DOI] [PubMed] [Google Scholar]
- 9. Voeten JT, Bestebroer TM, Nieuwkoop NJ, Fouchier RA, Osterhaus AD, Rimmelzwaan GF. Antigenic drift in the influenza A virus (H3N2) nucleoprotein and escape from recognition by cytotoxic T lymphocytes. J Virol 2000; 74:6800–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van de Sandt CE, Kreijtz JH, Geelhoed-Mieras MM, et al. Differential recognition of influenza A viruses by M158-66 epitope-specific CD8+ T cells is determined by extraepitopic amino acid residues. J Virol 2015; 90:1009–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dawood FS, Iuliano AD, Reed C, et al. Estimated global mortality associated with the first 12 months of 2009 pandemic influenza A H1N1 virus circulation: a modelling study. Lancet Infect Dis 2012; 12:687–95. [DOI] [PubMed] [Google Scholar]
- 12. Hancock K, Veguilla V, Lu X, et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N Engl J Med 2009; 361:1945–52. [DOI] [PubMed] [Google Scholar]
- 13. Ikonen N, Strengell M, Kinnunen L, et al. High frequency of cross-reacting antibodies against 2009 pandemic influenza A(H1N1) virus among the elderly in Finland. Euro Surveill 2010; 15. [PubMed] [Google Scholar]
- 14. van Baalen CA, Kwa D, Verschuren EJ, et al. Fluorescent antigen-transfected target cell cytotoxic T lymphocyte assay for ex vivo detection of antigen-specific cell-mediated cytotoxicity. J Infect Dis 2005; 192:1183–90. [DOI] [PubMed] [Google Scholar]
- 15. Boon AC, de Mutsert G, Fouchier RA, Osterhaus AD, Rimmelzwaan GF. The hypervariable immunodominant NP418-426 epitope from the influenza A virus nucleoprotein is recognized by cytotoxic T lymphocytes with high functional avidity. J Virol 2006; 80:6024–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.