Abstract
Study Objectives
To examine prospectively the associations of disaster experiences and social support with sleep problems in older adults.
Methods
Data came from a natural experiment caused by the 2011 Great East Japan earthquake and tsunami. Participants in an ongoing prospective cohort (3547 Japanese individuals aged 65 years or older) were inadvertently exposed to the disaster due to their residential location (Iwanuma city) after the 2010 baseline survey. We conducted a follow-up survey in 2013 to inquire about disaster-related experiences and short sleep duration, sleep insufficiency, poor sleep quality, insomnia symptoms, and sleep medication use. Poisson regression models adjusted for baseline socio-demographic and lifestyle covariates.
Results
Financial hardship predicted increased risks of short sleep duration (relative risk [RR] = 1.40; 95% confidence interval [CI] [1.03, 1.90]), sleep insufficiency (RR = 1.29; 95% CI [1.01, 1.66]), poor sleep quality (RR = 1.47; 95% CI [1.26, 1.70]), and insomnia symptoms (RR = 1.13; 95% CI [1.01, 1.28]). Home destruction predicted sleep medication use while health care disruption predicted poor sleep quality. Loss of close relatives or friends did not predict any sustained sleep problems. Additionally, having instrumental support reduced risks of all sleep problems while having emotional support reduced risk of poor sleep quality.
Conclusions
Approximately 2.5 years after the disaster, older survivors’ sleep problems were more durably linked to material aspects of disaster damage than to loss of loved ones. Findings could inform targeted recovery efforts for groups with greatest need to promote older survivors’ sleep health and overall well-being.
Keywords: disaster, social support, sleep, natural experiment, older adults, survivors, Japan
Statement of Significance
Sleep problems are among the most prevalent, yet understudied, health concerns of disaster survivors. We investigated prospective determinants of sleep problems among older survivors. Data from a natural experiment in Japan allowed us to evaluate the unique associations of different types of disaster damage and social support with several dimensions of sleep. Sleep problems were predicted by material impacts of disaster damage, but not loss of close relatives or friends (from which survivors seemed to have recovered). Instrumental support was more relevant to sleep problems than emotional support. Findings could inform interventions to alleviate survivors’ sleep problems and subsequent health outcomes, which could assist in disaster preparedness and recovery. Future research should explore the associations using objective measures of sleep.
Introduction
In recent decades, accompanying the rising incidence of natural disasters and increasing population growth and population density, the scale and scope of disaster damage have increased notably [1–3]. About 278 million people were affected by natural disasters in 1990, as compared to 332 million in 2011 [2]. Sleep is one of the most common health concerns of disaster survivors. Approximately half of the victims in Santa Rose Island continued to experience sleep disturbances 6 days after Hurricane Ivan (a Category 3 storm) [4]. Such sleep consequences of disaster exposure are not simply transient. One year after the 1999 Athens earthquake in Greece, 55% of the survivors developed sleep disorders [5]. Short sleep duration, poor sleep quality, or both has been associated with chronic diseases (e.g. type 2 diabetes and cardiovascular diseases) and mortality in various populations [6–17]. Sleep disturbances have also been linked to mental health problems such as depression, perceived stress, and post-traumatic stress disorder, particularly among disaster-affected populations [18–22].
Given the high prevalence of sleep problems and their extensive subsequent health effects on disaster survivors, it is essential to deepen our understanding of survivors’ sleep. Identifying factors that contribute to survivors’ sleep problems is critical for developing effective interventions to mitigate survivors’ sleep problems and the associated adverse health outcomes, which would assist in disaster preparedness and recovery efforts to promote reconstruction and community resilience after disaster.
In contrast to the wealth of evidence on the persistent mental health effects of disaster experiences [23–31], very little has been published on survivors’ lingering sleep problems during the disaster recovery phase, particularly among older adults. Initial studies on determinants of survivors’ sleep health have documented the importance of exposure to disaster [32–35]. These studies, while suggestive, are far from comprehensive. The usual absence of a comparable control group (unexposed to the disaster) hinders appropriate counterfactual comparisons. Moreover, much of previous research has included only one measure of sleep (such as sleep duration [33] or sleep quality [32]), and has addressed exposure to disaster as a general experience without differentiating between types of disaster damage or has only considered home destruction [32–35]. Furthermore, prior research on predictors of disaster survivors’ sleep has investigated younger populations with relatively short follow-ups (usually less than 1 year) [32–35], but not older adults who are disproportionately affected by disasters [36, 37].
On the other hand, some studies have suggested that lack of social support is associated with increased risks of sleep problems [38–42]. However, the cross-sectional design employed by prior studies constrains their ability to identify causality and renders their results to recall bias because the information about social support was gathered in the aftermath of a disaster. There has not yet been a study on survivors’ sleep in which pre-disaster social support information was used.
This study aims to advance this line of research by examining prospectively whether disaster damage and social support are associated with persistent sleep problems among older survivors of the 2011 Great East Japan earthquake and tsunami over 2.5 years of follow-up. It leverages a prospective study design – a natural experiment afforded by the JApan Gerontological Evaluation Study (JAGES) of community-dwelling adults aged 65 or older, as the 2011 disaster struck one of the field sites, Iwanuma city, between the baseline (2010) and the follow-up (2013) surveys. We evaluate multiple dimensions of sleep, including short sleep duration, sleep insufficiency, poor sleep quality, insomnia symptoms, and sleep medication use, to fully examine how disaster damage and social support are linked to a variety of sleep behaviors.
The primary aim is to determine the unique impacts of different types of disaster damage (financial hardship, home destruction, health care disruption, and loss of close relatives or friends) on sleep problems. We hypothesize that each type of disaster damage would predict higher risk of each sleep problem among older survivors in tsunami-affected areas over 2.5 years of follow-up. For instance, experiencing financial hardship would predict higher risk of short sleep duration at follow-up. The secondary aim is to evaluate the influences of instrumental support (help, aid, or assistance with tangible needs) and emotional support (the expression of empathy, reassurance, or trust) [43] on sleep. We hypothesize that availability of each form of social support would be associated with better sleep over 2.5 years of follow-up.
Methods
Study participants and study design
This paper used data collected as part of a national cohort study, the JAGES project, which was established in August 2010 to assess prospective predictors of disability onset among community-dwelling older adults in Japan. The municipal health authorities are responsible for maintaining accurate registers of every citizen residing in their catchment areas in Japan. A census of all residents aged 65 years or older was conducted and the baseline questionnaire was mailed to every citizen in the age range in 31 towns and cities across the country, using the official residential registry system (koseki touhon) provided by the city town hall as the sampling frame. Out of 169215 older adults invited, 112123 eligible individuals responded to the survey, yielding a response rate of 66.3%. The survey asked questions on participants’ socio-demographics, lifestyle habits, social support, as well as health behaviors and outcomes [30].
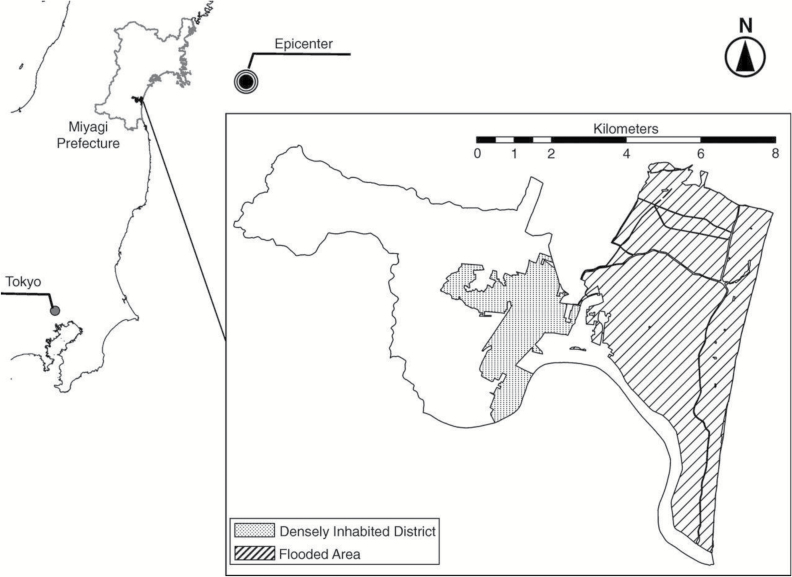
Seven months after the baseline survey, one of the field sites of JAGES, Iwanuma city, was directly struck by the 2011 Great East Japan earthquake and tsunami on March 11. The disaster killed 187 residents (out of a total population of 44187), damaged 5428 buildings, and inundated 48% of Iwanuma land area (Figure 1) [30, 44]. The research team obtained permission from the local government to repeat the survey in 2013. A follow-up survey was conducted among survivors in the city approximately 2.5 years after the disaster (October 2013 to January 2014), which inquired about participants’ experiences both during and after the disaster. The survey protocol was reviewed and approved by the human subjects committee of the Harvard T.H. Chan School of Public Health, as well as the human subjects committees of Tohoku University, Nihon Fukushi University, and Chiba University.
Figure 1.
Map of Iwanuma, in which 187 people died or are missing, 5428 buildings were damaged, and 48% of the area was flooded, Japan. Reproduced from ref. [30].
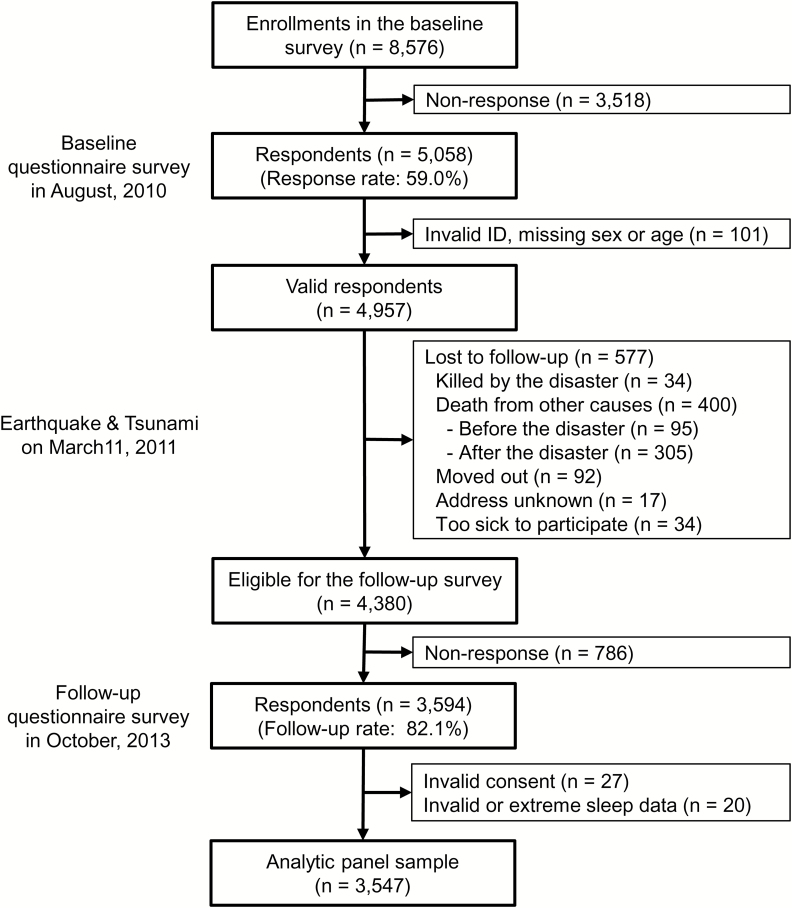
Figure 2 depicts study recruitment and retention. At baseline, invitations were sent to all residents aged 65 years or older in Iwanuma city. Five-thousand fifty-eight individuals agreed to participate (out of 8576, participation rate: 59.0%). Among 4380 participants eligible for the follow-up study, 3594 completed the survey (follow-up rate: 82.1%). After excluding 27 respondents with incompletely signed informed consent forms and 20 respondents who reported erroneous (>24 hours) or extreme sleep duration (<3 hours or >13 hours), the analytic panel sample consisted of 3547 individuals.
Figure 2.
Flow chart of the sample.
Assessment of outcomes
Post-disaster assessment of sleep
Five indicators of sleep problems were included: short sleep duration, sleep insufficiency, poor sleep quality, insomnia symptoms, and sleep medication use. The questions were derived from the Pittsburgh Sleep Quality Index (PSQI) [45] except for the item on sleep insufficiency. The survey had only these sleep-related questions but not the whole PSQI scale, which restricted our ability in examining an overall sleep quality score. However, looking at the variety of sleep indicators granted us the opportunity to assess how disaster damage and social support were associated with different aspects of self-reported sleep.
Sleep duration was determined by asking how many actual hours of sleep respondents got in the past month (PSQI #4a). Short sleep duration was defined as sleeping 5 hours or less per day. The cut-point was chosen because previous studies have shown that sleeping 5 hours or less is associated with elevated risk of mortality among older populations [46–48]. The National Sleep Foundation also recommends older adults aged 65 years or older not to sleep less than 5 hours as it is not likely conductive for health and well-being [49].
Insomnia symptoms were assessed by asking how often respondents “could not fall asleep within half an hour of going to bed” (PSQI #5a) or “woke up in the middle of the night or early in the morning” (PSQI #5b), with response categories of never, less than once a week, one to two times a week, and three or more times a week. Respondents who experienced the symptoms three or more times a week were regarded as suffering from insomnia. The variable was dichotomized as having the symptoms more frequently might indicate more severe sleep problems and indicate more clinical significance because experiencing insomnia most of the time has been shown to be associated with increased risk of mortality [50].
Sleep insufficiency was defined as experiencing the symptom of “didn’t feel well-rested when woke up in the morning in the past month” 3 or more times a week [51, 52]. The item is similar to the Centers for Disease Control and Prevention (CDC) surveillance for state-level sleep insufficiency [53].
Sleep quality was measured by asking respondents to rate their sleep quality as a whole in the past month (PSQI #6), with responses ranging from 1 (very poor) to 4 (very good). A response of 1 (very poor) or 2 (poor) indicated poor sleep quality.
Sleep medication use was defined as taking medication (that was prescribed by a doctor or bought at a pharmacy or other vendors) to help sleep (PSQI #7).
Each sleep indicator was binary and was analyzed separately.
Assessment of Exposures
Post-disaster assessment of disaster damage
The main exposures of interest were types of disaster damage (primary aim) and types of pre-disaster social support (secondary aim). Disaster damage was measured by a series of questions asking the respondents their disaster-related experiences. Financial hardship was assessed by asking respondents if their financial conditions changed after the earthquake. Those who reported “worse” or “much worse” financial conditions were defined as experiencing financial hardship. Home destruction was measured by asking how badly respondents’ residences were damaged in the earthquake, with responses categorized into three levels (0 = no damage, 1 = partially destroyed, and 2 = half destroyed or worse). Health care disruption was defined as “unable to receive a medical examination because of the earthquake.” Loss of close relatives or friends was defined by asking the question “Did you lose a close relative or friend in the earthquake?” All damage variables were binary except for home destruction.
Pre-disaster assessment of social support
Two dimensions of social support was measured at baseline: instrumental and emotional support. Instrumental support was assessed by asking the question “Do you have someone who looks after you when you are sick and confined to a bed for a few days?” Emotional support was assessed by asking if the respondent had someone who listened to his/her concerns and complaints. Both social support variables were binary.
Covariates
Pre-disaster assessment of covariates
We controlled for respondents’ pre-disaster socio-demographic and lifestyle characteristics, which have been found to be important for sleep in prior research (see, e.g. ref. [54–56]). Adjusted covariates included gender, age, marital status, educational attainment, and equivalised income, as well as smoking and drinking status. We did not control for depressive symptoms as prior research has indicated that sleep problems are symptoms of and might be risk factors of depression [57]. Including depressive symptoms in the analyses might introduce the problem of over-control.
Statistical Analyses
For the main analyses, we conducted multiple Poisson regression analyses based on models of the form:
| (1) |
where is the post-disaster sleep problem indicator. The coefficient vector captures the effects of disaster damage , including financial hardship, home destruction, health care disruption, and loss of close relatives or friends (primary aim); captures the effects of pre-disaster social support , including instrumental and emotional support (secondary aim); captures the effects of pre-disaster covariates , including socio-demographic and lifestyle variables.
We used Poisson regression instead of logistic regression as the former provides relative risks (RRs), which some have argued are easier to interpret compared to odds ratios [58]. In addition, the odds ratio is often interpreted as if it were the risk ratio, although the odds ratio approximates the risk ratio only under certain conditions. The more frequent the outcome, the more odds ratio overestimates the RR when it is more than 1 or underestimates it when it is less than 1 [59]. To estimate 95% confidence intervals (CIs) and Wald-based p-values we used the robust sandwich estimator of the variance [58].
In supplementary analyses, we addressed the issue of missingness by applying multiple imputation with the chained equations to the main analyses (10 imputed datasets), under the assumption of missing at random. Multiple imputation uses the distribution of the observed data to estimate a set of plausible values for the missing data, incorporating random components to reflect uncertainty. Multiple (10) datasets were created and then analyzed individually but identically to obtain a set of parameter estimates, which were later combined to calculate the overall estimates, variances, and CIs [60].
All analyses were performed using STATA (version 14.0, StataCorp LP, College Station, TX). All tests were two-sided, with a significance level of 5%.
Results
Table 1 presents the descriptive traits of the Iwanuma cohort. As for pre-disaster socio-demographic and lifestyle characteristics, slightly more than half of the respondents were female. About 60% were between the ages of 65 and 74 while the rest were older. Approximately two-thirds of the participants were married. Thirty-six percent received less than 9 years of education or less. About half had an equivalised income below 2 million JPY. Participants who had never smoked and who had never consumed alcohol accounted for 61.2% and 59.9% of the sample, respectively. With respect to exposures of interest, 96.0% of the respondents reported having pre-disaster instrumental support and 93.8% emotional support. Twenty-four percent of the respondents experienced financial hardships after the disaster. Home destruction was the most prevalent type of disaster damage: 15.8% reported home being half destroyed or worse and 43.1% reported home being partially destroyed. Thirteen percent of the respondents experienced health care disruption and 37% experienced loss of close relatives or friends. In terms of sleep problems, the percentage of people experiencing insomnia symptoms was the highest (41.4%), followed by poor sleep quality (27.0%), sleep medication use (21.6%), sleep insufficiency (13.4%), and short sleep duration (8.7%).
Table 1.
Descriptive traits of Iwanuma cohort (n = 3547)
| Variables | N | % | Variables | N | % |
|---|---|---|---|---|---|
| Pre-disaster socio-demographics | Disaster damage | ||||
| Gender | Financial hardship | ||||
| Male | 1542 | 43.5% | Yes | 821 | 23.7% |
| Female | 2005 | 56.5% | No | 2640 | 76.3% |
| Age | Home destruction | ||||
| 65–74 years | 2122 | 59.8% | Half destroyed or worse | 543 | 15.8% |
| 75 years or older | 1425 | 40.2% | Partially destroyed | 1487 | 43.1% |
| Marital status | No damage | 1417 | 41.1% | ||
| Married | 2445 | 71.4% | Health care disruption | ||
| Unmarried | 981 | 28.6% | Yes | 453 | 12.8% |
| Education | No | 3094 | 87.2% | ||
| <6 years | 45 | 1.3% | Loss of close relatives/friends | ||
| 6–9 years | 1174 | 34.4% | Yes | 1321 | 37.2% |
| 10–12 years | 1484 | 43.5% | No | 2226 | 62.8% |
| >12 years | 709 | 20.8% | Post-disaster sleep problems | ||
| Equivalised income | Short sleep duration | ||||
| < 2 million JPY | 1413 | 48.8% | Yes | 302 | 8.7% |
| 2–4 million JPY | 1200 | 41.4% | No | 3168 | 91.3% |
| >4 million JPY | 284 | 9.8% | Sleep insufficiency | ||
| Pre-disaster lifestyle | Yes | 462 | 13.4% | ||
| Smoking status | No | 2979 | 86.6% | ||
| Current | 363 | 11.2% | Poor sleep quality | ||
| Used to | 898 | 27.6% | Yes | 942 | 27.0% |
| Never | 1990 | 61.2% | No | 2541 | 73.0% |
| Drinking status | Insomnia symptoms | ||||
| Current | 1272 | 36.7% | Yes | 1448 | 41.4% |
| Used to | 119 | 3.4% | No | 2052 | 58.6% |
| Never | 2075 | 59.9% | Sleep medication use | ||
| Pre-disaster social support | Yes | 753 | 21.6% | ||
| Instrumental support | No | 2732 | 78.4% | ||
| Yes | 3314 | 96.0% | |||
| No | 137 | 4.0% | |||
| Emotional support | |||||
| Yes | 3196 | 93.8% | |||
| No | 212 | 6.2% | |||
Table 2 reports results from Poisson regression models separately estimating short sleep duration, sleep insufficiency, poor sleep quality, insomnia symptoms, and sleep medication use. Financial hardship predicted the majority of sleep problems. It was significantly associated with higher risks of short sleep duration (RR = 1.40; 95% CI [1.03, 1.90]), sleep insufficiency (RR = 1.29; 95% CI [1.01–1.66]), poor sleep quality (RR = 1.47; 95% CI [1.26–1.70]), and insomnia symptoms (RR = 1.13; 95% CI [1.01–1.28]), after adjusting for pre-disaster socio-demographic, lifestyle, and social support variables. Home destruction was significantly linked to sleep medication use (half destroyed or worse vs. no damage: RR = 1.36; 95% CI [1.06–1.74]; partially destroyed vs. no damage: RR = 1.37; 95% CI [1.15–1.63]). Health care disruption was significantly tied to poor sleep quality (RR = 1.34; 95% CI [1.13–1.58]). Surprisingly, loss of close relatives or friends was not significantly associated with any indicators of sleep problems. With respect to pre-disaster social support, having instrumental support significantly protected the older adults from short sleep duration (RR = 0.57; 95% CI [0.34–0.98]), sleep insufficiency (RR = 0.46; 95% CI [0.31–0.69]), poor sleep quality (RR = 0.63; 95% CI [0.48–0.82]), insomnia symptoms (RR = 0.70; 95% CI [0.57–.087]), and sleep medication use (RR = 0.70; 95% CI [0.49–0.99]). Emotional support significantly protected the older adults from poor sleep quality (RR = 0.74; 95% CI [0.58–0.95]).
Table 2.
Poisson regression models estimating persistent sleep problems
| Short sleep duration | Sleep insufficiency | Poor sleep quality | Insomnia symptoms | Sleep medication use | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| RR | [95% CI] | RR | [95% CI] | RR | [95% CI] | RR | [95% CI] | RR | [95% CI] | |
| Disaster damage | ||||||||||
| Financial hardship (vs. no) | 1.40 | [1.03, 1.90]* | 1.29 | [1.01, 1.66]* | 1.47 | [1.26, 1.70]*** | 1.13 | [1.01, 1.28]* | 1.08 | [0.88, 1.31] |
| Home destruction (vs. no) | ||||||||||
| Half destroyed or worse | 0.82 | [0.52, 1.27] | 0.98 | [0.70, 1.37] | 0.90 | [0.73, 1.11] | 0.99 | [0.84, 1.16] | 1.36 | [1.06, 1.74]* |
| Partially destroyed | 1.13 | [0.85, 1.50] | 1.20 | [0.96, 1.50] | 1.12 | [0.97, 1.29] | 1.09 | [0.98, 1.20] | 1.37 | [1.15, 1.63]*** |
| Health care disruption (vs. no) | 1.07 | [0.73, 1.58] | 1.04 | [0.75, 1.42] | 1.34 | [1.13, 1.58]*** | 1.08 | [0.93, 1.24] | 1.14 | [0.91, 1.42] |
| Loss of close relatives/friends (vs. no) | 1.07 | [0.83, 1.39] | 1.14 | [0.92, 1.40] | 1.06 | [0.93, 1.21] | 0.97 | [0.88, 1.07] | 0.95 | [0.81, 1.12] |
| Pre-disaster social support | ||||||||||
| Instrumental support (vs. no) | 0.57 | [0.34, 0.98]* | 0.46 | [0.31, 0.69]*** | 0.63 | [0.48, 0.82]*** | 0.70 | [0.57, 0.87]** | 0.70 | [0.49, 0.99]* |
| Emotional support (vs. no) | 0.97 | [0.54, 1.73] | 0.89 | [0.59, 1.35] | 0.74 | [0.58, 0.95]* | 1.00 | [0.83, 1.22] | 1.22 | [0.80, 1.87] |
| Pre-disaster covariates | ||||||||||
| Female (vs. male) | 1.27 | [0.80, 2.01] | 0.98 | [0.72, 1.34] | 1.32 | [1.07, 1.64]** | 0.94 | [0.81, 1.10] | 2.18 | [1.66, 2.87]*** |
| Age, years | 0.98 | [0.96, 1.01] | 1.02 | [1.00, 1.04]+ | 1.00 | [0.99, 1.01] | 1.02 | [1.01, 1.03]*** | 1.04 | [1.02, 1.05]*** |
| Married (vs. no) | 0.70 | [0.50, 0.99]* | 0.91 | [0.71, 1.17] | 1.03 | [0.87, 1.22] | 1.01 | [0.89, 1.15] | 1.03 | [0.85, 1.24] |
| Education (vs. 10–12 years) | ||||||||||
| <6 years | 0.31 | [0.04, 2.32] | 0.73 | [0.27, 1.97] | 1.21 | [0.74, 1.99] | 1.14 | [0.79, 1.66] | 1.13 | [0.68, 1.89] |
| 6–9 years | 0.92 | [0.68, 1.25] | 0.91 | [0.72, 1.16] | 0.95 | [0.81, 1.11] | 0.98 | [0.87, 1.09] | 0.90 | [0.75, 1.08] |
| >12 years | 0.67 | [0.46, 0.98]* | 0.88 | [0.67, 1.15] | 0.99 | [0.83, 1.17] | 0.97 | [0.86, 1.09] | 1.08 | [0.88, 1.32] |
| Equivalised income (vs. 2–4 million JPY) | ||||||||||
| < 2 million JPY | 1.01 | [0.78, 1.32] | 1.05 | [0.84, 1.30] | 1.05 | [0.92, 1.21] | 1.04 | [0.94, 1.15] | 1.23 | [1.04, 1.45]* |
| > 4 million JPY | 0.94 | [0.58, 1.51] | 1.11 | [0.77, 1.58] | 0.98 | [0.76, 1.25] | 0.89 | [0.74, 1.06] | 1.17 | [0.89, 1.54] |
| Smoking status (vs. never) | ||||||||||
| Current | 0.88 | [0.50, 1.53] | 1.27 | [0.88, 1.83] | 1.03 | [0.80, 1.32] | 1.08 | [0.91, 1.29] | 1.02 | [0.72, 1.44] |
| Used to | 1.32 | [0.88, 1.99] | 1.19 | [0.88, 1.61] | 1.24 | [1.02, 1.51]* | 1.24 | [1.09, 1.42]** | 1.12 | [0.85, 1.46] |
| Drinking status (vs. never) | ||||||||||
| Current | 0.75 | [0.54, 1.04]+ | 0.79 | [0.62, 1.02]+ | 1.00 | [0.85, 1.18] | 1.11 | [0.99, 1.24]+ | 0.88 | [0.70, 1.09] |
| Used to | 0.62 | [0.25, 1.50] | 0.82 | [0.47, 1.43] | 0.95 | [0.67, 1.36] | 0.93 | [0.72, 1.20] | 1.43 | [0.95, 2.14]+ |
| Observations | 2477 | 2470 | 2482 | 2496 | 2485 | |||||
Exponentiated coefficients.
+ p < .10, *p < .05, **p < .01, ***p < .001.
As loss of close relatives or friends was correlated with financial hardship (r = 0.16; p < .001) and with home destruction (r = 0.13; p < .001), we evaluated whether the nonsignificant relationships between loss of close relatives or friends and the sleep outcomes were due to collinearity across the disaster-related factors by removing the other disaster damage variables from the regression models. Results from the simplified regression models were similar to those from the full model in that loss of close relatives or friends was not significantly associated with any sleep indicators.
We conducted a series of sensitivity analyses by adopting different coding strategies for the sleep variables. First, we adopted a 6-hour cutoff for short sleep duration and reran the regression model so that the results could be compared to studies that used a 6-hour cutoff. The direction of the effect of financial hardship on short sleep duration was the same as that in the main analyses (5-hour cutoff), but it was no longer statistically significant with a p-value of .109 (RR = 1.15; 95% CI [0.97, 1.36]). The effect of instrumental support (RR = 0.74, 95% CI [0.56, 0.98]) remained in the same direction as that in the main analyses and stayed statistically significant. We also did sensitivity analyses modeling the sleep outcomes as continuous variables using linear regression. The substantive conclusions were unchanged in that material aspects of disaster damage were associated with more sleep problems and social support protected people from sleep problems. We further explored the relationships between post-disaster sleep and predictors of interest by constructing a global sleep score from the sleep indicators. A continuous composite sleep score was calculated by summing the responses of the sleep indicators (sleep duration categorized following PSQI scoring guidelines), with higher values indicating worse sleep health. The results were consistent with our main analyses in that financial hardship, home destruction, and health care disruption were significantly associated with worse global sleep health and instrumental support was significantly associated with better global sleep health.
Additionally, we reran the insomnia regression models looking at sleep onset insomnia (could not fall asleep within half an hour of going to bed) and sleep maintenance insomnia (woke up in the middle of the night or early in the morning) separately. While the directions of the effects of financial hardship on sleep onset/maintenance insomnia were the same, financial hardship was only significantly associated with sleep onset insomnia (RR = 1.33, 95% CI [1.07, 1.65]) but not sleep maintenance insomnia (RR = 1.07, 95% CI [.94, 1.23]). The findings suggested that individuals who had trouble falling asleep were more vulnerable to financial hardship compared to those who had trouble maintaining sleep.
The main analyses used data from observations with complete information on all variables included, which was about 70% of the panel (e.g. 2477 out of 3547 participants with complete information in the short sleep duration model). The supplementary analyses, in which we used multiple imputation to address missing data, spoke to the robustness of the study findings in the main analyses. The directions of the effects of disaster damage and social support were the same, and the statistical significance levels remained largely unchanged (Supplementary Table S1).
Discussion
This study investigated the associations of disaster damage and social support with persistent sleep problems among older survivors of the 2011 Great East Japan earthquake and tsunami. We hypothesized that each type of disaster damage and social support would predict each dimension of sleep problems, but the results painted a more complicated picture. Specifically, financial hardship predicted higher risks of short sleep duration, sleep insufficiency, poor sleep quality, and insomnia symptoms. Home destruction was associated with more sleep medication use. Health care disruption was linked to poor sleep quality. Unexpectedly, loss of close relatives or friends was not associated with any indicators of sleep problems. Social support in the form of instrumental support was linked to lower risks of all sleep problems whereas emotional support was tied to lower risk of poor sleep quality.
The material impacts of damage caused by the disaster (financial hardship, home destruction, and health care disruption) emerged as salient predictors of sustained sleep problems whereas there was no evidence that loss of close relatives or friends was associated with sleep problems over 2.5 years of follow-up. This might arise from the fact that our sample consisted of participants aged 65 years or older. It was likely that older survivors endured on-going struggles to rebuild their lives. For instance, survivors with financial hardships might be unable to afford tangible life essentials such as replacing an inundated mattress or buying quality food, which would affect their sleep. They might also have to deal with other sources of stress such as the hassles of getting insurance payments and government compensation. Most of the older adults were retired and their capacity to earn money (besides pension) might be limited, which might make them more vulnerable to financial hardship. Additionally, compared to those with no home destruction, people whose homes were partially or completely destroyed lived in a worse physical environment. The limited living space, the thin walls, together with the suboptimal thermal environment and sanitary conditions might contribute to sleep problems. Moreover, older adults might be more sensitive to health care disruption compared to younger generations if frailer and in greater need of health care. They might not have recovered from such damage after 2.5 years. On the other hand, loss of close relatives or friends might be a more normative experience as people age. Thus, older adults might become more resilient and might have recovered from loss of close relatives or friends over 2.5 years. The associations that we observed might be different had the follow-up been conducted closer to the trauma. For instance, significant relationships between loss of close relatives or friends and sleep problems might emerge if the follow-up was within a year of the disaster. The implication from our findings, that the material aspects of disaster damage, but not loss of loved ones, had persistent impacts on older survivors’ sleep over 2.5 years of follow-up is consistent with findings from previous research on disaster damage’s impacts on depressive symptoms and cognitive decline among older survivors [31, 61].
Most prior studies focusing on sleep have treated disaster damage as a general experience but not differentiated between types of disaster damage. An exception in this regard is Matsumoto and colleagues’ work [41, 42]. They conducted a cross-sectional survey on 4176 household members in the Ishinomaki area 6–12 months after the 2011 Great East Japan earthquake and tsunami. They found that lack of pleasure in life and lack of interaction with neighbors were associated with sleep difficulties, but none of the disaster exposure variables predicted sleep difficulties [41]. The same team of investigators reported similar results using cross-sectional data on 2593 respondents in the same area 1–2 years after the disaster [42]. There are at least three reasons why they did not find associations between disaster damage and sleep difficulties but we did. First, the different definitions of sleep outcomes made it difficult to directly compare the results. Specifically, Matsumoto and colleagues assessed sleep with just one question asking whether or not the participants had sleep difficulties. The question was answered by the representatives of households but not necessarily by the individuals who had actually experienced the symptoms, which might have induced more measurement error. In contrast, we incorporated five indicators of sleep problems that were reported by the individuals who experienced the symptoms themselves. Second, the study populations were different in that Matsumoto and colleagues assessed younger populations while our study examined older populations. Third, the follow-up times were different as Matsumoto and colleagues evaluated the question in shorter periods (6 months to 2 years) compared to that of our study (2.5 years).
Our findings also contribute to the broader stress and sleep/insomnia literature. For instance, financial strain (as a measure of chronic stress) has been associated with decreased sleep quality in older adults [62, 63]. Our result that financial hardship was associated with sleep onset insomnia (but not sleep maintenance insomnia) provides evidence along this line. Specifically, financial hardship might lead to chronic pre-sleep rumination. Prolonged worries about safety and food might induce cognitive arousal, which might delay sleep onset. Prior research on stress and sleep is usually limited by potential endogeneity problems in that unobserved confounders in observational studies could bias the results. If a person has an intrinsic characteristic for risk-taking or gambling, he/she would be more likely to have more financial strain and have worse sleep because of risk-taking behaviors. In comparison to most prior studies on stress and sleep, our study, a natural experiment, is much less likely to have the endogeneity problem as the instruments for stress (e.g. financial hardship) were imposed by a natural disaster and were thus exogenous.
With regards to social support, the results revealed a similar pattern as that of disaster damage: the tangible form—instrumental support—had protected the older adults from more adverse sleep indicators than emotional support did. This might be true because older people generally had worse physical health compared to younger age groups and had more needs for people to take care of them while sick. Our findings are in line with previous research showing that social support protects people from sleep problems [38–40, 42]. We made a contribution by using pre-disaster social support information that removed recall bias and distinguished between forms of social support and by showing that instrumental support was more relevant to sleep outcomes than emotional support among older disaster survivors.
We also tested for interaction effects between disaster damage and social support variables on sleep indicators. There was no evidence of an interaction between disaster damage and social support, suggesting that they had independent effects on older survivors’ sleep.
Strengths, Limitations, and Future Directions
This study features three strengths. First, it took advantage of a unique prospective design that strengthened causal inference by providing pre-disaster information that established temporality and protected inference from recall bias, and by providing an appropriate control group such that comparisons were made between residents living in the same municipality who happened to be in locations that tsunami did or did not reach.
Second, this study incorporated several indicators on the outcome of interest (sleep) and the predictors of interest (disaster damage and social support). This allows us to identify which dimensions of sleep are sensitive to which aspects of disaster damage and social support. The differential and interesting associations of disaster damage and social support call for more research on this topic to elucidate the mechanisms.
Third, the focus on older adults followed for an extended period (2.5 years) helped us to understand the long-term struggles of those in greatest needs. Older adults are disproportionally affected both during and after disasters, because of chronic diseases or conditions, impaired physiological and cognitive changes experienced as part of aging, as well as social and economic limitations that prevent adequate preparation before disasters and impede recovery after disasters [36, 37]. For these reasons, CDC urges that the frail older adults are recognized as a special-needs population in emergency management and strategies should be developed to meet their needs [64].
The first limitation of the study was that sleep, disaster damage, and social support, were all self-reported, which might induce common-method bias. When the same respondent provides information on measures of both the predictor and the outcome, artifactual covariance between the two variables might arise [65]. For instance, distress induced by exposure to disaster might lead participants to amplify the extent to which their financial situations or health care access deteriorated after the disaster and to amplify the severity of their sleep problems, which might induce spurious relationships between the exposures and the outcomes. Home destruction and loss of close relatives or friends should be less prone to such bias as they were defined more operationally. Also, while the self-reported sleep indicators capture different dimensions of sleep health, they have not been validated to the same extent as the PSQI scale. Future research could consider using objective measures of sleep such as actigraphy data.
In addition, the main analyses did not control for pre-disaster sleep. Only a quarter of the sample was asked the sleep questions at baseline, and so we did not have adequate power to evaluate how sleep changed over time in relation to disaster damage and social support. Moreover, one might also be concerned about selection bias as the pre-disaster sleep questions were administered based on Iwanuma’s school districts such that respondents who were asked the pre-disaster sleep questions (in districts of South Iwanuma, Iwanuma, and West Iwanuma) lived further away from the coastline compared to those who were not asked the questions (in district of Tamaura). In this case, controlling for pre-disaster sleep might introduce selection bias as those who were most severely hit by the disaster would be excluded. We, therefore, chose to focus our research question on predictors of persistent post-disaster sleep problems among older disaster survivors. In exploratory analyses, we looked at sleep changes from pre- to post-disaster in the subsample where pre-disaster sleep assessment was available. The crude prevalence decreased slightly for most sleep problems (short sleep duration: 8.7% to 6.3%; sleep insufficiency: 14.7% to 11.2%; poor sleep quality: 28.0% to 24.8%; insomnia symptoms: 42.0% to 39.0%; sleep medication use: 16.7% to 17.7%). Result from regression models controlling for pre-disaster sleep showed that the majority of the effects remained in the same directions yet were attenuated (e.g. effect of financial hardship on short sleep duration: RR decreased from 1.40 to 1.12; effect of financial hardship on insomnia symptoms: RR decreased from 1.13 to 1.06). Most effects were no longer statistically significant. This was expected due to the sharp decrease in sample size. In this subsample, we also explored interaction effects between indicators of pre-disaster sleep and disaster damage. There was no evidence that poor pre-disaster sleepers were more vulnerable to sleep problems after exposure to disaster. It would be of interest for future studies to take pre-disaster sleep into consideration.
Selection bias was a potential problem due to the 59.0% baseline response rate and the 82.1% follow-up response rate. However, it was shown in prior research that the Iwanuma cohort at baseline was representative of the whole older adult population in Iwanuma city in terms of demographic characteristics [30]. Thanks to the cooperation of the Iwanuma city administration using the official residential registry, only 17 respondents could not be tracked at follow-up. Five-hundred sixty other respondents were successfully tracked but lost to follow-up due to sickness, death, or relocation. Out of 4380 participants eligible for the follow-up survey, 786 did not respond. We found that people who responded to the follow-up survey did not differ significantly from those who did not respond, especially in terms of disaster damage. While we did not have disaster damage information from people who did not respond to the follow-up survey, residential distance from coastline information was collected at baseline, which could serve as a proxy for disaster damage. The distributions of distance from coastline among people who responded and who did not respond were very similar (Supplementary Table S2).
Future research could evaluate if exposure to disaster damage modifies the associations between health disruption and sleep disturbances. It is possible that experiences of disaster might amplify health disruption’s effects on sleep as people in poorer health might be more vulnerable to the physical and psychological impacts caused by the trauma, which could impair their sleep.
Lastly, while our findings contribute to knowledge on persistent sleep problems among older survivors, future research is warranted to assess if the findings are generalizable to populations in other age groups and/or from other countries.
Conclusions
We have demonstrated that different types of disaster damage and social support were associated with older survivors’ persistent sleep problems in many but very different ways. The findings could shed light on targeted interventions to mitigate lingering sleep problems and the associated adverse health outcomes among older disaster survivors. For instance, in addition to grief counseling, long-term reconstruction efforts for older survivors could be directed to the provision of material support such as financial assistance, home repair and shelter assistance, and continued access to health care, in order to promote recovery after the disaster. Efforts could also be directed to the promotion of instrumental support to protect older adults. These efforts would contribute to higher resilience, better disaster preparedness, and faster recovery among disaster-affected communities.
Supplementary material
Supplementary material is available at SLEEP online.
Funding
This work was supported by a grant from National Institutes of Health (R01 AG042463), several Health and Labour Sciences Research Grants (Comprehensive Research on Aging and Health) from the Japanese Ministry of Health, Labour and Welfare (H22-Choju-Shitei-008, H24-Choju-Wakate-009, H25-Choju-Ippan-003, and H28-Choju-Ippan-002), Grants-in-Aid for Scientific Research from the Japanese Society for the Promotion of Science (KAKENHI 23243070, 22390400, 24390469, and 15H01972), a grant from the Strategic Research Foundation Grant-Aided Project for Private Universities from the Japanese Ministry of Education, Culture, Sports, Science and Technology (S0991035), and Research and Development Grants for Longevity Science from the Japan Agency for Medical Research and Development.
Acknowledgments
The authors would like to thank the Iwanuma Mayor’s office, the staff of the Department of Health and Welfare of the Iwanuma city government, as well as the other investigators and the participants of the study for their valuable support and contributions. We are also grateful to the anonymous reviewers’ constructive input.
Notes
Conflict of interest statement. The authors have indicated no financial conflicts of interest. Outside of the current work, Dr. Buxton received two subcontract grants to Pennsylvania State University from Mobile Sleep Technologies (NSF/STTR #1622766, NIH/NIA SBIR R43AG056250).
References
- 1. Leaning J, et al. Natural disasters, armed conflict, and public health. N Engl J Med. 2013;369(19):1836–1842. [DOI] [PubMed] [Google Scholar]
- 2. Guha-Sapir D, et al. Annual Disaster Statistical Review 2011: The Numbers and Trends. Brussels, Belgium: Centre for Research on the Epidemiology of Disasters; 2012. [Google Scholar]
- 3. World Bank. The recent earthquake and tsunami in Japan: implications for East Asia. East Asia Pac Econ Update. 2011;1:1–2. [Google Scholar]
- 4. Bayleyegn T, et al. Rapid assessment of the needs and health status in Santa Rosa and Escambia counties, Florida, after Hurricane Ivan, September 2004. Disaster Manag Response. 2006;4(1):12–18. [DOI] [PubMed] [Google Scholar]
- 5. Varela E, et al. Psychological consequences among adults following the 1999 earthquake in Athens, Greece. Disasters. 2008;32(2):280–291. [DOI] [PubMed] [Google Scholar]
- 6. Patel SR, et al. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008;16(3):643–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buxton OM, et al. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. [DOI] [PubMed] [Google Scholar]
- 8. Cappuccio FP, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cappuccio FP, et al. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McAllister EJ, et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr. 2009;49(10):868–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gottlieb DJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. [DOI] [PubMed] [Google Scholar]
- 12. Hall MH, et al. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep. 2008;31(5):635–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Laugsand LE, et al. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124(19):2073–2081. [DOI] [PubMed] [Google Scholar]
- 14. Vgontzas AN, et al. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mallon L, et al. High incidence of diabetes in men with sleep complaints or short sleep duration: a 12-year follow-up study of a middle-aged population. Diabetes Care. 2005;28(11):2762–2767. [DOI] [PubMed] [Google Scholar]
- 16. Grandner MA, et al. Mortality associated with short sleep duration: the evidence, the possible mechanisms, and the future. Sleep Med Rev. 2010;14(3):191–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wingard DL, et al. Mortality risk associated with sleeping patterns among adults. Sleep. 1983;6(2):102–107. [DOI] [PubMed] [Google Scholar]
- 18. Mohsenin S, et al. Diagnosis and management of sleep disorders in posttraumatic stress disorder: a review of the literature. Prim Care Companion CNS Disord. 2014;16(6). doi:10.4088/PCC.14r01663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Smid GE, et al. Stress sensitization following a disaster: a prospective study. Psychol Med. 2012;42(8):1675–1686. [DOI] [PubMed] [Google Scholar]
- 20. van Griensven F, et al. ; Thailand Post-Tsunami Mental Health Study Group. Mental health problems among adults in tsunami-affected areas in southern Thailand. JAMA. 2006;296(5):537–548. [DOI] [PubMed] [Google Scholar]
- 21. Tachibana A, et al. Psychological distress in an earthquake-devastated area with pre-existing high rate of suicide. Psychiatry Res. 2014;219(2):336–340. [DOI] [PubMed] [Google Scholar]
- 22. Wu ZH, et al. Sleep quality among low-income young women in Southeast Texas predicts changes in perceived stress through Hurricane Ike. Sleep. 2015;38(7):1121–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Goenjian AK, et al. Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. Am J Psychiatry 2000;157(6):911–916. [DOI] [PubMed] [Google Scholar]
- 24. Kumar MS, et al. Prevalence of posttraumatic stress disorder in a coastal fishing village in Tamil Nadu, India, after the December 2004 tsunami. Am J Public Health. 2007;97(1):99–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zwiebach L, et al. Resource loss, resource gain, and mental health among survivors of Hurricane Katrina. J Trauma Stress. 2010;23(6):751–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Galea S, et al. The epidemiology of post-traumatic stress disorder after disasters. Epidemiol Rev. 2005;27:78–91. [DOI] [PubMed] [Google Scholar]
- 27. Norris FH, et al. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981-2001. Psychiatry. 2002;65(3):207–239. [DOI] [PubMed] [Google Scholar]
- 28. Breslau N, et al. Psychiatric sequelae of posttraumatic stress disorder in women. Arch Gen Psychiatry. 1997;54(1):81–87. [DOI] [PubMed] [Google Scholar]
- 29. Rubonis AV, et al. Psychological impairment in the wake of disaster: the disaster-psychopathology relationship. Psychol Bull. 1991;109(3):384–399. [DOI] [PubMed] [Google Scholar]
- 30. Hikichi H, et al. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 Tohoku earthquake and tsunami. Am J Epidemiol. 2016;183:902–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tsuboya T, et al. Predictors of depressive symptoms following the Great East Japan earthquake: a prospective study. Soc Sci Med. 2016;161:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Alderman K, et al. Assessment of the health impacts of the 2011 summer floods in Brisbane. Disaster Med Public Health Prep. 2013;7(4):380–386. [DOI] [PubMed] [Google Scholar]
- 33. Usami M, et al. Sleep duration among children 8 months after the 2011 Japan earthquake and tsunami. PLoS One. 2013;8(5):e65398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tempesta D, et al. Long-term impact of earthquakes on sleep quality. PLoS One. 2013;8(2):e55936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Thordardottir EB, et al. Posttraumatic stress and other health consequences of catastrophic avalanches: a 16-year follow-up of survivors. J Anxiety Disord. 2015;32:103–111. [DOI] [PubMed] [Google Scholar]
- 36. Aldrich DP. The power of people: social capital’s role in recovery from the 1995 Kobe earthquake. Nat Hazards. 2011;56(3):595–611. [Google Scholar]
- 37. Fernandez LS, et al. Frail elderly as disaster victims: emergency management strategies. Prehosp Disaster Med. 2002;17(2):67–74. [DOI] [PubMed] [Google Scholar]
- 38. Geng F, et al. Sleep problems among adolescent survivors following the 2008 Wenchuan earthquake in China: a cohort study. J Clin Psychiatry. 2013;74(1):67–74. [DOI] [PubMed] [Google Scholar]
- 39. Nomura K, et al. Social determinants of self-reported sleep problems in South Korea and Taiwan. J Psychosom Res. 2010;69(5):435–440. [DOI] [PubMed] [Google Scholar]
- 40. Steptoe A, et al. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008;64(4):409–415. [DOI] [PubMed] [Google Scholar]
- 41. Matsumoto S, et al. ; Teikyo Ishinomaki Research Group and Health and Life Revival Council in the Ishinomaki district (RCI). Social ties may play a critical role in mitigating sleep difficulties in disaster-affected communities: a cross-sectional study in the Ishinomaki area, Japan. Sleep. 2014;37(1):137–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Matsumoto S, et al. ; Teikyo Ishinomaki Research Group. Implications for social support on prolonged sleep difficulties among a disaster-affected population: second report from a cross-sectional survey in Ishinomaki, Japan. PLoS One. 2015;10(6):e0130615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Berkman LF. et al. , eds. Social Epidemiology. 2nd ed Oxford, New York, Auckland: Oxford University Press; 2014. [Google Scholar]
- 44. Ishigaki A, et al. The Great East-Japan earthquake and devastating tsunami: an update and lessons from the past great earthquakes in Japan since 1923. Tohoku J Exp Med. 2013;229(4):287–299. [DOI] [PubMed] [Google Scholar]
- 45. Buysse DJ, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. [DOI] [PubMed] [Google Scholar]
- 46. Gangwisch JE, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. 2008;31(8):1087–1096. [PMC free article] [PubMed] [Google Scholar]
- 47. Yeo Y, et al. A prospective cohort study on the relationship of sleep duration with all-cause and disease-specific mortality in the Korean Multi-center Cancer Cohort study. J Prev Med Public Health. 2013;46(5):271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kim Y, et al. Insufficient and excessive amounts of sleep increase the risk of premature death from cardiovascular and other diseases: the Multiethnic Cohort Study. Prev Med. 2013;57(4):377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hirshkowitz M, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. [DOI] [PubMed] [Google Scholar]
- 50. Li Y, et al. Association between insomnia symptoms and mortality: a prospective study of U.S. men. Circulation. 2014;129(7):737–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Buxton OM, et al. Relationship of sleep deficiency to perceived pain and functional limitations in hospital patient care workers. J Occup Environ Med. 2012;54(7):851–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Olson R, et al. A workplace intervention improves sleep: results from the randomized controlled work, family, and health study. Sleep Health. 2015;1(1):55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Department of Health and Human Services, Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 54. Stamatakis KA, et al. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Phillips BA, et al. Cigarette smoking and sleep disturbance. Arch Intern Med. 1995;155(7):734–737. [PubMed] [Google Scholar]
- 56. Palmer CD, et al. Association between smoking and drinking and sleep duration. Ann Hum Biol. 1980;7(2):103–107. [DOI] [PubMed] [Google Scholar]
- 57. Franzen PL, et al. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10(4):473–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 59. Subramanian SV, et al. Income inequality and health: what have we learned so far?Epidemiol Rev. 2004;26:78–91. [DOI] [PubMed] [Google Scholar]
- 60. White IR, et al. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399. [DOI] [PubMed] [Google Scholar]
- 61. Hikichi H, et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan earthquake and tsunami. Proc Natl Acad Sci. 2016;113(45):E6911–E6918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Hall M, et al. Financial strain is a significant correlate of sleep continuity disturbances in late-life. Biol Psychol. 2008;77(2):217–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Hall MH, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32(1):73–82. [PMC free article] [PubMed] [Google Scholar]
- 64. Benson WF. CDC’s Disaster Planning Goal: Protect Vulnerable Older Adults. Atlanta, GA:CDC Healthy Aging Program; 2007. [Google Scholar]
- 65. Podsakoff PM, et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol. 2003;88(5):879–903. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.