Abstract
Variability in thyroid function in pregnant women is the result of 2 main determinants, each accounting for approximately half of it. The first is the genetically determined part of which the knowledge increases fast, but most remains to be discovered. The second determinant is caused by an ensemble of variables of which thyroid autoimmunity is the best known, but also by others such as parity, smoking, age, and BMI. More recently, new candidate variables have been proposed, such as iron, endocrine disruptors, and the ethnicity of the pregnant women. In the future, the diagnosis and treatment of thyroid (dys)function may be optimized by the use of each individual's pituitary-thyroid set point, corrected with a factor taking into account the impact of nongenetically determined variables.
Keywords: Thyroid function, Variables, Reference values
Introduction
Pregnancy is a condition leading to an increased demand in thyroid hormones (TH), resulting from the fetal need (especially before 18–20 weeks), increased renal iodide loss, increased levels of serum thyroxine-binding globulin, and increased degradation of TH by placental deiodinase type 3. Finally, around the 10–12th week of pregnancy, high hCG levels add strain to the maternal thyroid, and increase TH production [1].
In many studies, subclinical hypothyroidism (SCH) and thyroid autoimmunity (TAI) have been associated with adverse pregnancy outcomes, such as miscarriage and premature delivery [2, 3]. In addition, low T4 levels have been correlated with long-term neurocognitive problems in children [1, 2, 3]. For the diagnosis of SCH, the American Thyroid Association (ATA) guidelines recommend determining trimester- and population-specific ranges for serum TSH. These ranges should be determined in pregnant women without thyroid peroxidase antibodies (TPO-Abs) and severe iodine deficiency (ID) [4]. Furthermore, it is proposed to use serum TSH and not that of FT4 for the diagnosis of SCH [4]. An adequate diagnosis of SCH is a prerequisite to avoid unnecessary treatment with LT4 that can lead to adverse outcomes. Indeed, in a recent study, it has been shown that women receiving LT4 for SCH (at that period defined as a serum TSH between 2.5–4.0 mIU/L) had an increased prevalence of preterm delivery and preeclampsia [5].
The prevalence of SCH during pregnancy varies between 3.5 and 18% (depending on the reference range for serum TSH and the iodine intake of the population), and the main cause is the presence of TAI, most often diagnosed by increased levels of TPO-Abs [1, 3].
In a pilot study by Andersen et al. [6], it was shown that the intra-individual variability in TSH and FT4 levels is within a narrow range, whereas the interindividual variability is large. This suggests that every individual has its own unique hypothalamic pituitary thyroid axis set point [7, 8]. It is estimated that 45–65% of the total variation in thyroid function is determined by genetic factors, while the rest is determined by variables such as environmental factors (e.g., iodine status) and individual characteristics (e.g., BMI and parity) [8].
The knowledge of as much as possible variables with an influence on thyroid function could improve target screening of women at risk to develop SCH during pregnancy. However, the systematic screening for SCH in pregnant women leads to a higher detection rate than targeted screening [9, 10].
The aim of this review paper is to describe the impact of established variables on thyroid function such as smoking, parity, and BMI, and that of new candidate variables such as iron, ethnicity, endocrine disruptors, and placental vascular factors.
Established Variables Contributing to Variation in Thyroid Function
Thyroid Peroxidase Antibodies
The presence of increased TPO-Abs is the main variable leading to the development of SCH in iodine-sufficient areas. A positive correlation between TPO-Ab titers and thyroid function has been reported in the NHANES III study, what might be explained by the higher degree of lymphocytic infiltration of the thyroid [11, 12]. In a study in pregnant women by Vaidya et al. [10], the presence of a personal history of raised TPO-Abs increased the risk of high serum TSH (RR: 8.4; p < 0.001). In the study by Korevaar et al. [9], a prediction model for elevated TSH became more discriminative when positivity for TPO-Abs was added to the already included variables such as BMI, parity, and smoking.
Thyroglobulin Antibodies
Based on large epidemiological studies in the general population, it is generally accepted that TPO-Abs are more frequently increased than thyroglobulin antibodies (Tg-Abs) [11, 13]. In those studies, the prevalence of TPO-Abs was 13 and 24% versus 11.5 and 7% for Tg-Abs, respectively. The difference in the prevalence may be explained by less sensitive assays used at that period. It should, however, be noted that in 2 studies, the prevalence of positive antibodies in women aged 25–40 years was slightly higher for Tg-Abs than TPO-Abs [11, 14]. In a recent study by Unuane et al. [15] in an unselected group of women consulting for infertility, 5% had isolated positive Tg-Abs, compared with 4% with TPO-Abs only. In the NHANES III study, increased levels of Tg-Abs were not associated with thyroid function compared with increased TPO-Abs [11]. However, and in line with the improved detection of Tg-Abs, some studies have shown that they were also associated with higher serum TSH levels compared with those in TAI-negative women [14, 15]. Finally, the importance of Tg-Abs is now also noticed in the ATA guidelines on thyroid and pregnancy, but, at the same time, it is mentioned that in the vast majority of studies, TAI was defined by the presence of TPO-Abs, and, therefore, the committee recommends only measuring TPO-Abs [4].
FT4 and TSH Assay
FT4 testing in pregnancy is challenging, due to the decrease in albumin levels and increase in thyroxine-binding globulin. FT4 immunoassays (IAs) may be sensitive to these changes in a method-specific manner. In a study by Anckaert et al. [16], 3 automated FT4 IAs were compared with a reference procedure (equilibrium dialysis spectrometry), and it was confirmed that the IAs were sensitive to pregnancy-specific protein alterations but to a different extent. In another study by Berta et al. [17], FT4 levels were compared using 5 different assays in 40 pregnant women (at 8–22 weeks of gestation) without thyroidal disease, and the correlation coefficient between the different assays was 0.67–0.89. The ATA guidelines mention, therefore, that if FT4 is measured in pregnant women, assay method-specific and trimester-specific reference ranges should be used [4].
The Committee for Standardization of Thyroid Function Tests of the International Federation of Clinical Chemistry and Laboratory Medicine comparison studies report significant biases between different TSH methods, what prevents establishing universal population or trimester-specific TSH reference ranges that would apply across methods. Since TSH is a complex glycoprotein, no reference measurement procedure is available. However, a harmonization approach, where methods are recalibrated to the “all method mean,” has been shown to have the potential to eliminate between-method TSH differences [18]. In a recent study (but not in pregnant women), it was shown that differences between TSH assays could be as high as 37% [19]. However, that difference seems to be less prominent in pregnant women, as shown in the study by Berta et al. [17] with a correlation factor of 0.91–0.98 between 5 different TSH IAs.
Iodine
Severe and longstanding maternal ID can lead to overt hypothyroidism and cretinism in children. In case of mild-to-moderate ID, the thyroid is still able to keep TH levels within the normal range, but in the long run, SCH may occur and in the older population toxic nodular goiter with suppressed TSH levels [20]. In a study from China, thyroid function and urinary iodine was determined in > 7,000 pregnant women during the first trimester, and women with low urinary iodine (100–149 ug/L) had median serum TSH and FT4 levels comparable with those in the reference group (urinary iodine between 150 and 249 µg/L) [21]. Also, in a study performed in Belgium (an area with a moderate ID), serum TSH concentrations did not significantly vary according to the iodine status [22]. In areas with a longstanding ID, where an iodine fortification program was implemented, transient iodine-induced hyperthyroidism was observed, and, in the long run, an increased prevalence of hypothyroidism was reported, probably as a result of iodine-induced TAI and maybe a decreased deiodinase type 2 activity in the hypothalamus and pituitary [23].
Finally, it should be mentioned that high iodine intake (urinary iodine > 500 μg/L) was associated with an up to 2.2-fold higher risk of SCH and a 2.9-fold higher risk of hypothyroxinemia compared with the reference group (urinary iodine 150–249 μg/L) [21].
Serum hCG Levels and Gestational Week
Serum hCG has a weak thyroid-stimulating activity, especially when levels peak at 10–12 weeks of gestation. During that period, in 10–20% of pregnant women, serum FT4 and FT3 levels can be elevated, and TSH decreased. In one study, all women with serum hCG > 400,000 IU/L had temporarily suppressed TSH levels [24]. In another study, it was shown that mean free β-hCG levels of women with suppressed TSH were twice those of women without suppressed serum TSH (p < 0.05) [25]. Besides the amount of hCG levels, TSH action can also be impaired due to the presence of increased TPO-Abs, higher BMI, and parity (≥2) [26]. In 2 case reports, gestational thyrotoxicosis has been described in the presence of normal levels of serum hCG due to a mutation endowing the TSH receptor with increased sensitivity to serum hCG compared with that of the wild-type receptor [27, 28].
In a Danish study, it was nicely documented that during the first trimester of pregnancy, thyroid function varied according to the gestational week [29]. Therefore, the use of one reference limit for the entire first trimester is probably a simplification. Based on their study results, the authors proposed using TSH reference values of nonpregnant women up to the 7th week of pregnancy, and to decrease the upper TSH limit of nonpregnant women value with 0.4 mU/L during weeks 9–12. For the period between 7 and 9 weeks, a lower TSH reference limit of 0.1 mU/L was proposed. Serum FT4 variation seems to be limited to higher values during weeks 9–12, and it was, therefore, suggested to increase the nonpregnant reference limit by 4% [29].
Body Mass Index
In several studies, TSH values were different in pregnant women as BMI increased, with a TSH distribution shifted to higher values and FT4 to lower ones. In a study performed in Chile, BMI had a small but significant effect on TSH and FT4, which persisted after correction for maternal age, increased TPO-Abs, parity, gestational age, and smoking [30]. In a study in Finland, the upper limits for TSH in women with a BMI between 20 and 25 and with a BMI > 30 were 2.86 and 3.50 mU/L, respectively [31]. In some studies, higher serum TSH levels were not observed in women with higher BMIs, what may be explained by differences in iodine intake, the ethnic background, and the number of pregnant women included in the studies [32, 33].
The association between lower FT4 levels and higher BMI in the first trimester appears to be a uniform finding. In the study by Mannisto et al. [31], FT4 levels decreased from 12.3 to 11.6 pmol/L when women with BMI < 20 were compared with those with BMI > 30. Bestwick et al. [34] expressed FT4 values in multiples of the median and found a decrease in FT4 of 0.009 multiples of the median per 10-kg increase in BMI.
There are several mechanisms that may lead to increased TSH levels in obesity. Adipose tissue produced cytokines and other inflammatory factors, and leptin increased thyrotropin-releasing hormone (TRH) levels through a direct action on TRH neurons. Furthermore, an increased deiodinase activity has been described, which leads to a higher conversion of T4 to T3 [35]. Finally, obesity has been associated with a higher prevalence of TPO-Abs [36]. The guidelines of the ATA recommend TSH screening in morbidly obese pregnant women (BMI ≥40) [4].
Age
In a Danish study, a multivariate logistic regression analysis of demographic and environmental factors, maternal age > 30 years was a risk factor for the development of all types of thyroid disease before, during, and/or up to 5 years after pregnancy [37].
Also, in the general population, the prevalence of TAI and serum TSH increases with age [11]. In most studies in pregnant women, age > 30 years was not associated with increased serum TSH levels [9, 10, 38, 39] or TAI [39, 40]. In contrast, in the study by Veltri et al. [40] serum TSH was significantly lower in women > 30 years, and, in a study by Korevaar et al. [9], serum FT4 levels were significantly lower. Differences in serum TSH levels observed between studies may be explained by a different iodine and BMI status of the women. The guidelines of the ATA recommend TSH screening in pregnant women > 30 years [4].
Parity
In most studies, parity has been investigated in relation to the presence of TAI. The hypothesis is that after each pregnancy the risk for TAI increases through fetal microchimerism, implying that fetal cells that were transferred into the maternal circulation persist after birth and trigger autoimmune diseases [41]. However, the conclusions on this association are unequivocal, maybe due to the number of previous pregnancies that were included and differences in the definition of TAI [42, 43]. Furthermore, in a recent study, the significant association between parity and TAI was lost after adjustment for age [43]. Finally, in one study, a lower prevalence of TAI was observed in women with higher parity [9].
Some studies have investigated the impact of parity on TSH and FT4 levels, and the changes coincided often with those in TAI. In some studies, no impact was observed on serum TSH [9, 10], while in other studies, lower serum TSH levels were observed [29, 44]. Regarding FT4 levels, data are limited to one study in which lower values were noted in pregnant women [9] and another in which no impact was observed [29].
Smoking
In a recent study performed in pregnant women in Belgium, it was shown that 10% smoked, but that the prevalence varied between 3% in women with an African background and 23% in women with a Caucasian (Ca) background [45]. Smoking is known to affect thyroid function, but the magnitude and direction of the effect varied greatly between studies. Data can be summarized as no impact on serum TSH and a slight decrease in FT4 levels [9, 10, 29, 31].
Smoking has been associated with a lower risk for TAI, a change in deiodinase type 2 activity through the effects of nicotine [46], and, finally, with lower serum hCG levels [47].
In a recent study in pregnant women without TAI, smoking was associated with higher serum TSH levels [44]. Disparities between study results may reflect variations in populations and the iodine status. Furthermore, the duration of smoking cessation (that is associated with a higher prevalence of new-onset TAI) and the number of pack-years are not always documented [31, 48].
TSH Diurnal Variation
In a small study including 4 pregnant women during late pregnancy (weeks 34–38), and 2 studies performed during early pregnancy, women had a clear diurnal rhythm, with the highest levels in late evening or early night. Sampling frequency was insufficient for pulsatility analysis, but the data were in line with those in nonpregnant women [49]. This variation does not influence the diagnostic interpretation of test results since most TSH measurements are performed in pregnant women between 8 a.m. and 6 p.m. However, whether reference interval determinations are adjusted for the collecting time is never clearly stated in most studies.
New Candidate Variables Contributing to Variation in Thyroid Function
Iron Status
Iron plays an important role in the normal functioning of TPO, a heme-dependent protein, and it also facilitates the actions of iodine in the thyroid [50, 51]. In pregnant women, iron deficiency (Fe-D) arises since physiological requirements cannot be met by iron absorption from the diet. In industrialized countries, the prevalence of Fe-D in pregnant women ranges from 24 to 44%. Fe-D can be diagnosed by low serum ferritin levels (< 15 μg/L has a specificity of 98% and a sensitivity of 75% for Fe-D) [52].
The pilot study investigating the impact of Fe-D on thyroid function in pregnant women in the second and third trimester of pregnancy was published in 2007 by Zimmerman et al. [53] and performed in Switzerland (a borderline ID region). In the third trimester, nearly 40% of women had Fe-D, and 6% had TSH > 4.0 mIU/L. Serum ferritin was inversely correlated with serum TSH (ρ: −0.506; p < 0.0001) and total T4 (ρ: 0.679; p < 0.0001). In a study performed in a Chinese area without ID in 7,953 pregnant women during the first trimester, FT4 levels were lower in pregnant women with Fe-D (p < 0.05). Logistic regression indicated that Fe-D was an independent risk factor for hypothyroxinemia (OR: 2.440, 95% CI: 1.324–4.496, p = 0.004; and OR: 3.278, 95% CI: 1.443–7.446, p = 0.005, respectively) [54]. In both studies, TAI was not taken into account or an exclusion criterion. In a recent study by Veltri et al. [40] in 1,900 pregnant women performed in Belgium (mild ID), TAI was also analyzed in relation to Fe-D. In the Fe-D group (all over 35%), the prevalence of TAI and SCH was higher than in the non-Fe-D group (10 vs. 6 and 20 vs. 16%, respectively; p = 0.011 and 0.049, respectively). Ferritin was inversely correlated with serum TSH (ρ = −0.076; p = 0.001) and positive with FT4 levels (ρ = 0.112; p < 0.001). In the logistic regression and after correction for confounding factors, Fe-D remained associated with TAI (p = 0.017) but not with SCH. Finally, it is important to highlight that in the multivariable analysis, Fe-D explained < 1% of the variability in log TSH [40].
The pathophysiological mechanisms explaining this association between Fe-D and SCH/TAI remain largely speculative. One explanation could be impaired TPO activity, with decreased iodine incorporation into Tg and the coupling of iodotyrosines, finally leading to lower FT4 and higher TSH levels [51, 55]. Fe-D can also be a consequence of TAI due to the concomitant presence of autoimmune gastritis, which was present in 33% of TAI patients in one study [56].
Concerning the higher TSH levels/SCH, besides a lower TPO activity, the binding of T3 to hepatic nuclear receptors, oxygen transport, and finally the conversion from T4 to T3 can be impaired [51, 55]. Another hormone that plays an important role in iron metabolism is hepcidin, a systemic iron-regulatory hormone. Only in one study in nonpregnant women with Graves disease, hepcidin levels were correlated with TH, and they were lower in the euthyroid phase than in the hyperthyroid phase when measured with mass spectrometry [57]. No difference in hepcidin levels was found when measured with an ELISA method, and this methodological problem is one of the reasons why few studies investigated the relationship between hepcidin and thyroid function.
In daily practice, pregnant women often receive multivitamins, of which some contain iron (18 mg) and iodine (150 μg). In this regard, it also deserves attention that the intake of these preparations should be separated from that of LT4 by at least 4 h to avoid LT4 malabsorption. To date, no studies in pregnant women have been published providing evidence that iron supplements ameliorate thyroid function. Fe-D as such is a known risk factor associated with obstetrical complications, and this impact might thus in part have been mediated through the thyroid pathway [58]. In order to know whether Fe-D, TAI, or SCH hampers a normal pregnancy evolution, prospective studies are needed.
Ethnic Background
In many metropolitan areas, the population is multiethnic. Ethnicity is a whole of genetic, dietary, environmental, and cultural factors. Several studies have shown a difference in the prevalence of thyroid function and TAI between individuals with different ethnic backgrounds, both in pregnant women and the general population [11]. In one study in the USA, the prevalence of TAI was lower in African-American women than in women with a Ca background [59]. In one study in the Netherlands, no difference was observed in the prevalence of TAI between pregnant women of Turkish, Moroccan, Surinamese, and Dutch origin, but in a more recent Dutch study, women of Turkish origin had a higher prevalence of TAI [60, 61]. In 2 studies in the USA, African-American women had significantly lower TSH levels than Ca women [62, 63]. In one of the Dutch studies, no differences in serum TSH levels were observed [61].
The most recent results on this issue come from a cross-sectional study performed in Belgium in 1,683 pregnant women [45]. The prevalence of TAI was significantly lower in women of sub-Saharan descendent (Sa) compared with that in women with a North African (Na), and Ca background (3.3 vs. 8.6 and 11.1%; p < 0.001, respectively). Median TSH was significantly lower in Sa and Na than in Ca women (1.3 and 1.4 vs. 1.5 mIU/L; p = 0.006 and 0.014, respectively). The prevalence of SCH was significantly higher in Ca than Na women (5.4 vs. 2.1%, p = 0.008).
The reason for the lower prevalence of TAI in African-American and Sa women remains speculative. Smoking and smoking cessation have been associated with a lower and a higher prevalence of Hashimoto disease, respectively [46, 48]. In the Belgian study, women with a Ca background smoked more than the other women, but they had the highest prevalence of TAI [45]. The impact of smoking might have been wrongly interpreted since smoking cessation was not recorded, and the latter has been associated with the appearance of TAI [48]. In the study of La'ulu and Roberts [59], the lower age of women in the African-American study group compared with the Ca group was a possible explanation for the lower prevalence of TAI. However, in the study by Veltri et al. [45], mean ages were comparable between the groups. Obesity has also been associated with an increased prevalence of TAI, but the prevalence of obesity was the highest in women with other backgrounds than Sa or African-American [35, 36, 45]. Low vitamin D levels have been linked with the presence of TAI [for review, cf 64]. However, in the Belgian context, low vitamin D levels were equally distributed among women with different backgrounds [65]. Furthermore, urinary iodine (median: 117 μg/L; interquartile range: 70–189 μg/L) was not associated with a particular ethnicity [22, 66]. According to Walker et al. [63], the lower TSH levels in African-American women were due to higher hCG levels compared with Ca women. Also, in the study by Korevaar et al. [61], Ca women had lower hCG levels than Moroccan women.
Ethnicity is strongly related to genetics, determining up to 50–60% of the variation in thyroid function [8]. In a recent study, it was shown that mean TSH levels differed according to the ethnicity of the babies in blood spots performed for birth screening [67].
Some studies investigated what the impact of ethnic-specific reference ranges was on the prevalence of SCH in pregnant women [45, 61]. In studies by Korevaar et al. [61] and Veltri et al. [45], it was shown that this would change the diagnosis of SCH in 13 and 16%, respectively. Ethnic-specific reference ranges could be useful in certain groups, but their real additional value should be investigated in relation to pregnancy outcomes before they would be implemented in daily practice. In the ATA guidelines, it is not proposed to determine ethnic-specific TSH reference ranges [4].
Pollutants/Endocrine Disruptors
Perchlorate and thiocyanate decrease thyroidal iodine uptake by competitively inhibiting the sodium iodide symporter (NIS), and, therefore, they can influence thyroid function. Pregnant women with increased iodine needs are more vulnerable to the side effects [68]. This statement was confirmed in a study in 200 nonsmoking pregnant women in Thailand (mild ID area), in which it was shown that low-level exposure to perchlorate was positively correlated with TSH and inversely with FT4. These associations persisted after correction for gestational age and urinary disruptor concentration to creatinine ratio [69]. In a recent study in pregnant women in New York, the co-occurring exposure to perchlorate, nitrate, and thiocyanate was investigated by using the weighted quantile sum regression (examining mixture effects in epidemiological studies) and suggested that increasing exposure to perchlorate was associated with a significant increase in the odds of a serum TSH in the highest 10th percentile. Perchlorate had the largest weight in the index, and no associations between any exposure and FT4 were found [70]. Discrepancies in the study results may be explained by differences in urinary iodine levels, the degree of exposure, the fact that one or more disruptors were investigated, the use of different statistical methods, and other detection techniques. Endocrine disruptors used in plastics and flame retardants are also able to exert thyroid effects. However, long-term studies on thyroid-related outcomes such as growth and development are lacking [71].
Placental Factors besides hCG
The thyroid has a high vascular density that may be influenced by pregnancy-specific angiogenic factors, both proangiogenic (placental growth factor) and antiangiogenic (vascular endothelial growth factors), such as the soluble FMS-like tyrosine kinase-1 [72].
In a cohort of Norwegian pregnant women with preeclampsia, serum TSH levels were increased 2.42 times above baseline compared with 1.48 in controls, and FT3 levels decreased (case ratio to control ratio: 0.96, 95% CI: 0.92–0.99). Both in women who developed preeclampsia and in controls, the increase in serum TSH levels was strongly associated with increasing levels of predelivery soluble FMS-like tyrosine kinase 1 (p < 0.001). Furthermore, women with a history of preeclampsia in their first pregnancy were more likely to have TSH levels > 3.5 mIU/L (adjusted OR: 1.7, 95% CI: 1.1–2.5), and the association persisted after the exclusion of TAI [73]. These results were confirmed in a Dutch study, in which the impact of high placental growth factor levels led to a decrease in TSH levels (p < 0.001) and an increased risk of hypothyroxinemia (OR: 1.77; 95% CI: 1.02–3.06) [74]. In analogy with the Norwegian study, the antiangiogenic factors were also associated with a decrease in (F)T4 (p < 0.001), an increased risk of SCH (OR: 2.37; 95% CI: 1.16–4.83) and isolated hypothyroxinemia (OR: 3.05; 95% CI: 1.42–6.55). The presence of TPO-Abs amplified both the effect of the antiangiogenic profile and proangiogenic placental growth factors.
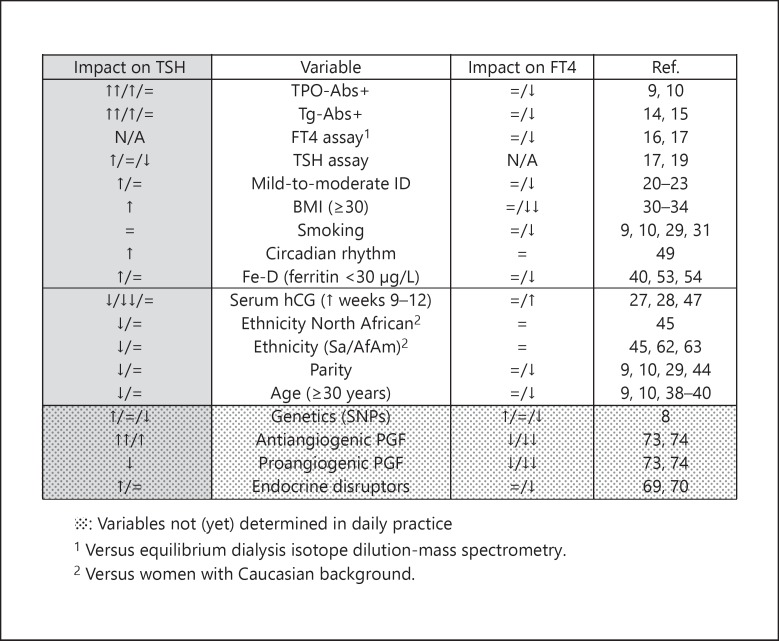
In Figure 1, the impact of variables on thyroid function is shown in a semiquantitative way.
Fig. 1.
Illustration of the impact of variables on thyroid function is shown in a semiquantitative way. =, no impact; ↑ or ↓, mild impact; ↑↑ or ↓↓, moderate or severe impact; N/A, not applicable; ID, iodine deficiency; Fe-D, iron deficiency; Sa, sub-Saharan; AfAm, African-American; SNPs, single nucleotide polymorphisms; PGF, platelet growth factor; Tg-Abs, thyroglobulin antibodies; TPO-Abs, thyroid peroxidase antibodies.
Conclusions and Perspectives
Although clinical characteristics affect reference ranges within populations, they are poor predictors of (subclinical) hypothyroidism in individuals. Therefore, it remains to be elucidated whether the implementation of trimester-, BMI- or ethnicity-based reference ranges can improve the management and outcome of pregnancy. Future studies should aim to identify the impact of novel variables such as endocrine disruptors, iron, and placental factors on the development of thyroid disease to relevant patient subgroups. In the future, all of these markers could be added as a correction factor to an individual's pituitary-thyroid set point and then be used as optimal individual treatment target.
For the time being, TAI remains the variable that is the strongest associated with SCH and altered pregnancy outcomes, and, therefore, its diagnosis should be improved for example with the measurement of Tg-Abs and/or a thyroid echography.
Disclosure Statement
Flora Veltri received no support from any organization.
Kris Poppe was supported by speaker fees for a satellite meeting of the European Thyroid Association (ETA) (IBSA Institut Biochimique SA) in 2016 and the ETA Educational Thyroid Meeting (Berlin-Chemie AG Company) in 2017.
References
- 1.Krassas GE, Poppe K, Glinoer D. Thyroid function and human reproductive health. Endocr Rev. 2010;31:702–755. doi: 10.1210/er.2009-0041. [DOI] [PubMed] [Google Scholar]
- 2.Chan S, Boelaert K. Optimal management of hypothyroidism, hypothyroxinaemia and euthyroid TPO antibody positivity preconception and in pregnancy. Clin Endocrinol (Oxf) 2015;82:313–326. doi: 10.1111/cen.12605. [DOI] [PubMed] [Google Scholar]
- 3.Korevaar TIM, Medici M, Visser TJ, Peeters RP. Thyroid disease in pregnancy: new insights in diagnosis and clinical management. Nat Rev Endocrinol. 2017;13:610–622. doi: 10.1038/nrendo.2017.93. [DOI] [PubMed] [Google Scholar]
- 4.Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, Grobman WA, Laurberg P, Lazarus JH, Mandel SJ, Peeters RP, Sullivan S. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017;27:315–389. doi: 10.1089/thy.2016.0457. [DOI] [PubMed] [Google Scholar]
- 5.Maraka S, Mwangi R, McCoy RG, Yao X, Sangaralingham LR, Singh Ospina NM, O'Keeffe DT, De Ycaza AE, Rodriguez-Gutierrez R, Coddington CC, 3rd, Stan MN, Brito JP, Montori VM. Thyroid hormone treatment among pregnant women with subclinical hypothyroidism: US national assessment. BMJ. 2017:356–i6865. doi: 10.1136/bmj.i6865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andersen S, Pedersen KM, Bruun NH, Laurberg P. Narrow individual variations in serum T4 and T3 in normal subjects: a clue to the understanding of subclinical thyroid disease. J Clin Endocrinol Metab. 2002;87:1068–1072. doi: 10.1210/jcem.87.3.8165. [DOI] [PubMed] [Google Scholar]
- 7.Roef GL, Taes YE, Kaufman JM, Van Daele CM, De Buyzere ML, Gillebert TC, Rietzschel ER. Thyroid hormone levels within reference range are associated with heart rate, cardiac structure, and function in middle-aged men and women. Thyroid. 2013;23:947–954. doi: 10.1089/thy.2012.0471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medici M, Visser TJ, Peeters RP. Genetics of thyroid function. Best Pract Res Clin Endocrinol Metab. 2017;31:129–142. doi: 10.1016/j.beem.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Korevaar TI, Nieboer D, Bisschop PH, Goddijn M, Medici M, Chaker L, de Rijke YB, Jaddoe VW, Visser TJ, Steyerberg EW, Tiemeier H, Vrijkotte TG, Peeters RP. Risk factors and a clinical prediction model for low maternal thyroid function during early pregnancy: two population-based prospective cohort studies. Clin Endocrinol (Oxf) 2016;85:902–909. doi: 10.1111/cen.13153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaidya B, Anthony S, Bilous M, Shields B, Drury J, Hutchison S, Bilous R. Detection of thyroid dysfunction in early pregnancy: universal screening or targeted high-risk case finding? J Clin Endocrinol Metab. 2007;92:203–207. doi: 10.1210/jc.2006-1748. [DOI] [PubMed] [Google Scholar]
- 11.Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, Braverman LE. Serum TSH, T4, and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III) J Clin Endocrinol Metab. 2002;87:489–499. doi: 10.1210/jcem.87.2.8182. [DOI] [PubMed] [Google Scholar]
- 12.Yoshida H, Amino N, Yagawa K, Uemura K, Satoh M, Miyai K, Kumahara Y. Association of serum antithyroid antibodies with lymphocytic infiltration of the thyroid gland: studies of seventy autopsied cases. J Clin Endocrinol Metab. 1978;46:859–862. doi: 10.1210/jcem-46-6-859. [DOI] [PubMed] [Google Scholar]
- 13.Strieder TG, Prummel MF, Tijssen JG, Endert E, Wiersinga WM. Risk factors for and prevalence of thyroid disorders in a cross-sectional study among healthy female relatives of patients with autoimmune thyroid disease. Clin Endocrinol (Oxf) 2003;59:396–401. doi: 10.1046/j.1365-2265.2003.01862.x. [DOI] [PubMed] [Google Scholar]
- 14.Pedersen IB, Knudsen N, Jorgensen T, Perrild H, Ovesen L, Laurberg P. Thyroid peroxidase and thyroglobulin autoantibodies in a large survey of populations with mild and moderate iodine deficiency. Clin Endocrinol (Oxf) 2003;58:36–42. doi: 10.1046/j.1365-2265.2003.01633.x. [DOI] [PubMed] [Google Scholar]
- 15.Unuane D, Velkeniers B, Anckaert E, Schiettecatte J, Tournaye H, Haentjens P, Poppe K. Thyroglobulin autoantibodies: is there any added value in the detection of thyroid autoimmunity in women consulting for fertility treatment? Thyroid. 2013;23:1022–1028. doi: 10.1089/thy.2012.0562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anckaert E, Poppe K, Van Uytfanghe K, Schiettecatte J, Foulon W, Thienpont LM. FT4 immunoassays may display a pattern during pregnancy similar to the equilibrium dialysis ID-LC/tandem MS candidate reference measurement procedure in spite of susceptibility towards binding protein alterations. Clin Chim Acta. 2010;411:1348–1353. doi: 10.1016/j.cca.2010.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Berta E, Samson L, Lenkey A, Erdei A, Cseke B, Jenei K, Major T, Jakab A, Jenei Z, Paragh G, Nagy EV, Bodor M. Evaluation of the thyroid function of healthy pregnant women by five different hormone assays. Pharmazie. 2010;65:436–439. [PubMed] [Google Scholar]
- 18.Thienpont LM, Van Uytfanghe K, Van Houcke S, Das B, Faix JD, MacKenzie F, Quinn FA, Rottmann M, Van den Bruel A. IFCC Committee for Standardization of Thyroid Function Tests (C-STFT): a progress report of the IFCC Committee for Standardization of Thyroid Function Tests. Eur Thyroid J. 2014;3:109–116. doi: 10.1159/000358270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coene KL, Demir AY, Broeren MA, Verschuure P, Lentjes EG, Boer AK. Subclinical hypothyroidism: a “laboratory-induced” condition? Eur J Endocrinol. 2015;173:499–505. doi: 10.1530/EJE-15-0684. [DOI] [PubMed] [Google Scholar]
- 20.Leung AM, Pearce EN, Braverman LE. Iodine nutrition in pregnancy and lactation. Endocrinol Metab Clin North Am. 2011;40:765–777. doi: 10.1016/j.ecl.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shi X, Han C, Li C, Mao J, Wang W, Xie X, Li C, Xu B, Meng T, Du J, Zhang S, Gao Z, Zhang X, Fan C, Shan Z, Teng W. Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7,190 pregnant women in China. J Clin Endocrinol Metab. 2015;100:1630–1638. doi: 10.1210/jc.2014-3704. [DOI] [PubMed] [Google Scholar]
- 22.Moreno-Reyes R, Glinoer D, Van Oyen H, Vandevijvere S. High prevalence of thyroid disorders in pregnant women in a mildly iodine-deficient country: a population-based study. J Clin Endocrinol Metab. 2013;98:3694–3701. doi: 10.1210/jc.2013-2149. [DOI] [PubMed] [Google Scholar]
- 23.Bliddal S, Boas M, Hilsted L, Friis-Hansen L, Tabor A, Feldt-Rasmussen U. Thyroid function and autoimmunity in Danish pregnant women after an iodine fortification program and associations with obstetric outcomes. Eur J Endocrinol. 2015;173:709–718. doi: 10.1530/EJE-15-0358. [DOI] [PubMed] [Google Scholar]
- 24.Lockwood CM, Grenache DG, Gronowski AM. Serum human chorionic gonadotropin concentrations greater than 400,000 IU/L are invariably associated with suppressed serum thyrotropin concentrations. Thyroid. 2009;19:863–868. doi: 10.1089/thy.2009.0079. [DOI] [PubMed] [Google Scholar]
- 25.Springer D, Zima T, Limanova Z. Reference intervals in evaluation of maternal thyroid function during the first trimester of pregnancy. Eur J Endocrinol. 2009;160:791–797. doi: 10.1530/EJE-08-0890. [DOI] [PubMed] [Google Scholar]
- 26.Korevaar TI, Steegers EA, Pop VJ, Broeren MA, Chaker L, de Rijke YB, Jaddoe VW, Medici M, Visser TJ, Tiemeier H, Peeters RP. Thyroid autoimmunity impairs the thyroidal response to human chorionic gonadotropin: two population-based prospective cohort studies. J Clin Endocrinol Metab. 2017;102:69–77. doi: 10.1210/jc.2016-2942. [DOI] [PubMed] [Google Scholar]
- 27.Rodien P, Bremont C, Sanson ML, Parma J, Van Sande J, Costagliola S, Luton JP, Vassart G, Duprez L. Familial gestational hyperthyroidism caused by a mutant thyrotropin receptor hypersensitive to human chorionic gonadotropin. N Engl J Med. 1998;339:1823–1826. doi: 10.1056/NEJM199812173392505. [DOI] [PubMed] [Google Scholar]
- 28.Coulon AL, Savagner F, Briet C, Vernin M, Munier M, Chabre O, Rodien P. Prolonged and severe gestational thyrotoxicosis due to enhanced hCG sensitivity of a mutant thyrotropin receptor. J Clin Endocrinol Metab. 2016;101:10–11. doi: 10.1210/jc.2015-3670. [DOI] [PubMed] [Google Scholar]
- 29.Laurberg P, Andersen SL, Hindersson P, Nohr EA, Olsen J. Dynamics and predictors of serum TSH and fT4 reference limits in early pregnancy: a study within the Danish National Birth Cohort. J Clin Endocrinol Metab. 2016;101:2484–2492. doi: 10.1210/jc.2016-1387. [DOI] [PubMed] [Google Scholar]
- 30.Mosso L, Martinez A, Rojas MP, Latorre G, Margozzini P, Lyng T, Carvajal J, Campusano C, Arteaga E, Boucai L. Early pregnancy thyroid hormone reference ranges in Chilean women: the influence of body mass index. Clin Endocrinol (Oxf) 2016;85:942–948. doi: 10.1111/cen.13127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mannisto T, Surcel HM, Ruokonen A, Vaarasmaki M, Pouta A, Bloigu A, Jarvelin MR, Hartikainen AL, Suvanto E. Early pregnancy reference intervals of thyroid hormone concentrations in a thyroid antibody-negative pregnant population. Thyroid. 2011;21:291–298. doi: 10.1089/thy.2010.0337. [DOI] [PubMed] [Google Scholar]
- 32.Pop VJ, Biondi B, Wijnen HA, Kuppens SM, Lvader H. Maternal thyroid parameters, body mass index and subsequent weight gain during pregnancy in healthy euthyroid women. Clin Endocrinol (Oxf) 2013;79:577–583. doi: 10.1111/cen.12177. [DOI] [PubMed] [Google Scholar]
- 33.Gowachirapant S, Melse-Boonstra A, Winichagoon P, Zimmermann MB. Overweight increases risk of first trimester hypothyroxinaemia in iodine-deficient pregnant women. Matern Child Nutr. 2014;10:61–71. doi: 10.1111/mcn.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bestwick JP, John R, Maina A, Guaraldo V, Joomun M, Wald NJ, Lazarus JH. Thyroid stimulating hormone and free thyroxine in pregnancy: expressing concentrations as multiples of the median (MoMs) Clin Chim Acta. 2014;430:33–37. doi: 10.1016/j.cca.2013.12.030. [DOI] [PubMed] [Google Scholar]
- 35.Rotondi M, Magri F, Chiovato L. Thyroid and obesity: not a one-way interaction. J Clin Endocrinol Metab. 2011;96:344–346. doi: 10.1210/jc.2010-2515. [DOI] [PubMed] [Google Scholar]
- 36.Marzullo P, Minocci A, Tagliaferri MA, Guzzaloni G, Di Blasio A, De Medici C, Aimaretti G, Liuzzi A. Investigations of thyroid hormones and antibodies in obesity: leptin levels are associated with thyroid autoimmunity independent of bioanthropometric, hormonal, and weight-related determinants. J Clin Endocrinol Metab. 2010;95:3965–3972. doi: 10.1210/jc.2009-2798. [DOI] [PubMed] [Google Scholar]
- 37.Andersen SL, Olsen J, Laurberg P. Maternal thyroid disease in the Danish National Birth Cohort: prevalence and risk factors. Eur J Endocrinol. 2016;174:203–212. doi: 10.1530/EJE-15-0816. [DOI] [PubMed] [Google Scholar]
- 38.Dieguez M, Herrero A, Avello N, Suarez P, Delgado E, Menendez E. Prevalence of thyroid dysfunction in women in early pregnancy: does it increase with maternal age? Clin Endocrinol (Oxf) 2016;84:121–126. doi: 10.1111/cen.12693. [DOI] [PubMed] [Google Scholar]
- 39.Potlukova E, Potluka O, Jiskra J, Limanova Z, Telicka Z, Bartakova J, Springer D. Is age a risk factor for hypothyroidism in pregnancy? An analysis of 5223 pregnant women. J Clin Endocrinol Metab. 2012;97:1945–1952. doi: 10.1210/jc.2011-3275. [DOI] [PubMed] [Google Scholar]
- 40.Veltri F, Decaillet S, Kleynen P, Grabczan L, Belhomme J, Rozenberg S, Pepersack T, Poppe K. Prevalence of thyroid autoimmunity and dysfunction in women with iron deficiency during early pregnancy: is it altered? Eur J Endocrinol. 2016;175:191–199. doi: 10.1530/EJE-16-0288. [DOI] [PubMed] [Google Scholar]
- 41.Lepez T, Vandewoestyne M, Hussain S, Van Nieuwerburgh F, Poppe K, Velkeniers B, Kaufman JM, Deforce D. Fetal microchimeric cells in blood of women with an autoimmune thyroid disease. PLoS One. 2011;6:e29646. doi: 10.1371/journal.pone.0029646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Greer LG, Casey BM, Halvorson LM, Spong CY, McIntire DD, Cunningham FG. Antithyroid antibodies and parity: further evidence for microchimerism in autoimmune thyroid disease. Am J Obstet Gynecol. 2011;205:471.e1–e4. doi: 10.1016/j.ajog.2011.06.060. [DOI] [PubMed] [Google Scholar]
- 43.Yehuda M, Wang CH, Pak Y, Chiu KC, Gianoukakis AG. Parity and risk of thyroid autoimmunity based on the NHANES (2001–2002, 2007–2008, 2009–2010, and 2011–2012) J Clin Endocrinol Metab. 2017;102:3437–3442. doi: 10.1210/jc.2017-00290. [DOI] [PubMed] [Google Scholar]
- 44.Veltri F, Kleynen P, Grabczan L, Salajan A, Rozenberg S, Pepersack T, Poppe KG. Pregnancy outcomes are not altered by variation in thyroid function within the normal range in women free of thyroid disease. Eur J Endocrinol. 2017;178:191–199. doi: 10.1530/EJE-17-0628. [DOI] [PubMed] [Google Scholar]
- 45.Veltri F, Belhomme J, Kleynen P, Grabczan L, Rozenberg S, Pepersack T, Poppe K. Maternal thyroid parameters in pregnant women with different ethnic backgrounds: do ethnicity-specific reference ranges improve the diagnosis of subclinical hypothyroidism? Clin Endocrinol (Oxf) 2017;86:830–836. doi: 10.1111/cen.13340. [DOI] [PubMed] [Google Scholar]
- 46.Wiersinga WM. Smoking and thyroid. Clin Endocrinol (Oxf) 2013;79:145–151. doi: 10.1111/cen.12222. [DOI] [PubMed] [Google Scholar]
- 47.Korevaar TI, Steegers EA, de Rijke YB, Schalekamp-Timmermans S, Visser WE, Hofman A, Jaddoe VW, Tiemeier H, Visser TJ, Medici M, Peeters RP. Reference ranges and determinants of total hCG levels during pregnancy: the Generation R Study. Eur J Epidemiol. 2015;30:1057–1066. doi: 10.1007/s10654-015-0039-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carle A, Bulow Pedersen I, Knudsen N, Perrild H, Ovesen L, Banke Rasmussen L, Jorgensen T, Laurberg P. Smoking cessation is followed by a sharp but transient rise in the incidence of overt autoimmune hypothyroidism – a population-based, case-control study. Clin Endocrinol (Oxf) 2012;77:764–772. doi: 10.1111/j.1365-2265.2012.04455.x. [DOI] [PubMed] [Google Scholar]
- 49.Roelfsema F, Veldhuis JD. Thyrotropin secretion patterns in health and disease. Endocr Rev. 2013;34:619–657. doi: 10.1210/er.2012-1076. [DOI] [PubMed] [Google Scholar]
- 50.Zimmermann MB, Kohrle J. The impact of iron and selenium deficiencies on iodine and thyroid metabolism: biochemistry and relevance to public health. Thyroid. 2002;12:867–878. doi: 10.1089/105072502761016494. [DOI] [PubMed] [Google Scholar]
- 51.Hess SY, Zimmermann MB, Arnold M, Langhans W, Hurrell RF. Iron deficiency anemia reduces thyroid peroxidase activity in rats. J Nutr. 2002;132:1951–1955. doi: 10.1093/jn/132.7.1951. [DOI] [PubMed] [Google Scholar]
- 52.Pavord S, Myers B, Robinson S, Allard S, Strong J, Oppenheimer C. British Committee for Standards in Haematology: UK guidelines on the management of iron deficiency in pregnancy. Br J Haematol. 2012;156:588–600. doi: 10.1111/j.1365-2141.2011.09012.x. [DOI] [PubMed] [Google Scholar]
- 53.Zimmermann MB, Burgi H, Hurrell RF. Iron deficiency predicts poor maternal thyroid status during pregnancy. J Clin Endocrinol Metab. 2007;92:3436–3440. doi: 10.1210/jc.2007-1082. [DOI] [PubMed] [Google Scholar]
- 54.Yu X, Shan Z, Li C, Mao J, Wang W, Xie X, Liu A, Teng X, Zhou W, Li C, Xu B, Bi L, Meng T, Du J, Zhang S, Gao Z, Zhang X, Yang L, Fan C, Teng W. Iron deficiency, an independent risk factor for isolated hypothyroxinemia in pregnant and nonpregnant women of childbearing age in China. J Clin Endocrinol Metab. 2015;100:1594–1601. doi: 10.1210/jc.2014-3887. [DOI] [PubMed] [Google Scholar]
- 55.Beard JL, Brigham DE, Kelley SK, Green MH. Plasma thyroid hormone kinetics are altered in iron-deficient rats. J Nutr. 1998;128:1401–1408. doi: 10.1093/jn/128.8.1401. [DOI] [PubMed] [Google Scholar]
- 56.De Block CE, De Leeuw IH, Van Gaal LF. High prevalence of manifestations of gastric autoimmunity in parietal cell antibody-positive type 1 (insulin-dependent) diabetic patients. The Belgian Diabetes Registry. J Clin Endocrinol Metab. 1999;84:4062–4067. doi: 10.1210/jcem.84.11.6095. [DOI] [PubMed] [Google Scholar]
- 57.Fischli S, von Wyl V, Trummler M, Konrad D, Wueest S, Ruefer A, Heering K, Streuli R, Steuer C, Bernasconi L, Recher M, Henzen C. Iron metabolism in patients with Graves' hyperthyroidism. Clin Endocrinol (Oxf) 2017;87:609–616. doi: 10.1111/cen.13450. [DOI] [PubMed] [Google Scholar]
- 58.Allen LH. Anemia and iron deficiency: effects on pregnancy outcome. Am J Clin Nutr. 2000;71:1280S–1284S. doi: 10.1093/ajcn/71.5.1280s. [DOI] [PubMed] [Google Scholar]
- 59.La'ulu SL, Roberts WL. Second-trimester reference intervals for thyroid tests: the role of ethnicity. Clin Chem. 2007;53:1658–1664. doi: 10.1373/clinchem.2007.089680. [DOI] [PubMed] [Google Scholar]
- 60.Benhadi N, Wiersinga WM, Reitsma JB, Vrijkotte TG, van der Wal MF, Bonsel GJ. Ethnic differences in TSH but not in free T4 concentrations or TPO antibodies during pregnancy. Clin Endocrinol (Oxf) 2007;66:765–770. doi: 10.1111/j.1365-2265.2007.02803.x. [DOI] [PubMed] [Google Scholar]
- 61.Korevaar TI, Medici M, de Rijke YB, Visser W, de Muinck Keizer-Schrama SM, Jaddoe VW, Hofman A, Ross HA, Visser W, Hooijkaas H, Steegers EA, Tiemeier H, Bongers-Schokking JJ, Visser TJ, Peeters RP. Ethnic differences in maternal thyroid parameters during pregnancy: the Generation R study. J Clin Endocrinol Metab. 2013;98:3678–3686. doi: 10.1210/jc.2013-2005. [DOI] [PubMed] [Google Scholar]
- 62.La'ulu SL, Roberts WL. Ethnic differences in first-trimester thyroid reference intervals. Clin Chem. 2011;57:913–915. doi: 10.1373/clinchem.2010.161240. [DOI] [PubMed] [Google Scholar]
- 63.Walker JA, Illions EH, Huddleston JF, Smallridge RC. Racial comparisons of thyroid function and autoimmunity during pregnancy and the postpartum period. Obstet Gynecol. 2005;106:1365–1371. doi: 10.1097/01.AOG.0000185475.61612.ea. [DOI] [PubMed] [Google Scholar]
- 64.D'Aurizio F, Villalta D, Metus P, Doretto P, Tozzoli R. Is vitamin D a player or not in the pathophysiology of autoimmune thyroid diseases? Autoimmun Rev. 2015;14:363–369. doi: 10.1016/j.autrev.2014.10.008. [DOI] [PubMed] [Google Scholar]
- 65.Vandevijvere S, Amsalkhir S, Van Oyen H, Moreno-Reyes R. High prevalence of vitamin D deficiency in pregnant women: a national cross-sectional survey. PLoS One. 2012;7:e43868. doi: 10.1371/journal.pone.0043868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vandevijvere S, Mourri AB, Amsalkhir S, Avni F, Van Oyen H, Moreno-Reyes R. Fortification of bread with iodized salt corrected iodine deficiency in school-aged children, but not in their mothers: a national cross-sectional survey in Belgium. Thyroid. 2012;22:1046–1053. doi: 10.1089/thy.2012.0016. [DOI] [PubMed] [Google Scholar]
- 67.Peters C, Brooke I, Heales S, Ifederu A, Langham S, Hindmarsh P, Cole TJ. Defining the newborn blood spot screening reference interval for TSH: impact of ethnicity. J Clin Endocrinol Metab. 2016;101:3445–3449. doi: 10.1210/jc.2016-1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pearce EN, Braverman LE. Environmental pollutants and the thyroid. Best Pract Res Clin Endocrinol Metab. 2009;23:801–813. doi: 10.1016/j.beem.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 69.Charatcharoenwitthaya N, Ongphiphadhanakul B, Pearce EN, Somprasit C, Chanthasenanont A, He X, Chailurkit L, Braverman LE. The association between perchlorate and thiocyanate exposure and thyroid function in first-trimester pregnant Thai women. J Clin Endocrinol Metab. 2014;99:2365–2371. doi: 10.1210/jc.2013-3986. [DOI] [PubMed] [Google Scholar]
- 70.Horton MK, Blount BC, Valentin-Blasini L, Wapner R, Whyatt R, Gennings C, Factor-Litvak P. Co-occurring exposure to perchlorate, nitrate and thiocyanate alters thyroid function in healthy pregnant women. Environ Res. 2015;143:1–9. doi: 10.1016/j.envres.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Boas M, Feldt-Rasmussen U, Main KM. Thyroid effects of endocrine disrupting chemicals. Mol Cell Endocrinol. 2012;355:240–248. doi: 10.1016/j.mce.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 72.Coolman M, Timmermans S, de Groot CJ, Russcher H, Lindemans J, Hofman A, Geurts-Moespot AJ, Sweep FC, Jaddoe VV, Steegers EA. Angiogenic and fibrinolytic factors in blood during the first half of pregnancy and adverse pregnancy outcomes. Obstet Gynecol. 2012;119:1190–1200. doi: 10.1097/AOG.0b013e318256187f. [DOI] [PubMed] [Google Scholar]
- 73.Levine RJ, Vatten LJ, Horowitz GL, Qian C, Romundstad PR, Yu KF, Hollenberg AN, Hellevik AI, Asvold BO, Karumanchi SA. Pre-eclampsia, soluble fms-like tyrosine kinase 1, and the risk of reduced thyroid function: nested case-control and population based study. BMJ. 2009;339:b4336. doi: 10.1136/bmj.b4336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Korevaar TI, Steegers EA, de Rijke YB, Visser WE, Jaddoe VW, Visser TJ, Medici M, Peeters RP. Placental angiogenic factors are associated with maternal thyroid function and modify hCG-mediated FT4 stimulation. J Clin Endocrinol Metab. 2015;100:e1328–e1334. doi: 10.1210/jc.2015-2553. [DOI] [PubMed] [Google Scholar]