Abstract
Distant metastases in nasopharyngeal carcinoma are fairly common. While the mainstay of treatment for metastatic nasopharyngeal carcinoma remains chemotherapy, it is now increasingly recognised that metastatic cases are a heterogenous group and can be stratified into oligometastatic cases versus those with widespread metastases, the former potentially benefiting more from local therapy. In this report, we describe a case of nasopharyngeal carcinoma with a solitary vertebral metastasis successfully treated with high-dose palliative radiotherapy alone, resulting in a long-term disease-free interval of more than 8 years at the time of writing. To our knowledge, this is the first report of a long-term survivor of metastatic nasopharyngeal carcinoma with oligometastatic bone disease who had received no chemotherapy. In view of this case, there may be potential for other patients with oligometastases from nasopharyngeal carcinoma to be treated solely with local therapy, thereby sparing them the toxicities of chemotherapy.
Keywords: Nasopharyngeal carcinoma, Metastasis, Radiotherapy
Introduction
Nasopharyngeal carcinoma, while rare in the West, is a common cancer in parts of Asia, with Southern Chinese being particularly susceptible. In Hong Kong, the incidence is about 20–30 per 100,000 per annum [1]. Risk factors include Epstein-Barr virus, hepatitis B infection, and alcohol intake. Tumours are divided into WHO Type I (keratinising SCC), Type II (non-keratinising), and Type III (undifferentiated), the last being the most common. Of these, type II carcinomas are more responsive to chemotherapy and radiotherapy; however, they also have a higher incidence of distant metastases [2]. Intensity-modulated radiotherapy is the primary treatment for non-metastatic nasopharyngeal carcinoma, with concurrent chemotherapy, usually cisplatin, being given for locally advanced cases. Despite good local control rates in various studies, distant metastases remain common, with rates of about 25–30% overall [3]. While the mainstay of treatment for metastatic nasopharyngeal carcinoma remains chemotherapy, it is now increasingly recognised that such metastatic cases are a heterogenous group and can be stratified further into oligometastatic cases versus those with widespread metastases, the former potentially benefiting more from local therapy.
Case Report
A 51-year-old Chinese male presented in January 2005 with a 4-month history of blocked left ear on a background of chronic sinusitis and bilateral submandibular gland swelling. On physical examination, bilateral prominent level IB/II cervical nodes were noted, and nasoendoscopy showed a mass in the left posterior nasal space. A biopsy showed undifferentiated carcinoma (WHO Type III). Fine needle aspiration of the left cervical node was negative for malignancy. An MRI of the post-nasal space showed involvement of the left paranasopharynx and left pterygopalatine fossa with perineural extension around the back of the left maxillary sinus, possibly involving the left zygomatic nerve. Cervical lymph nodes were not enlarged by size criteria. Chest X ray, ultrasound abdomen, and bone scan showed no distal metastases. Clinically, the patient had no cranial nerve deficits. The patient was staged as T2bN0M0 according to the AJCC 6th edition. He underwent radical intensity-modulated radiotherapy treatment to a dose of 69.96 Gy/33# from March to April 2005 without concurrent chemotherapy. He tolerated treatment well with some residual neck stiffness and Lhermitte's syndrome.
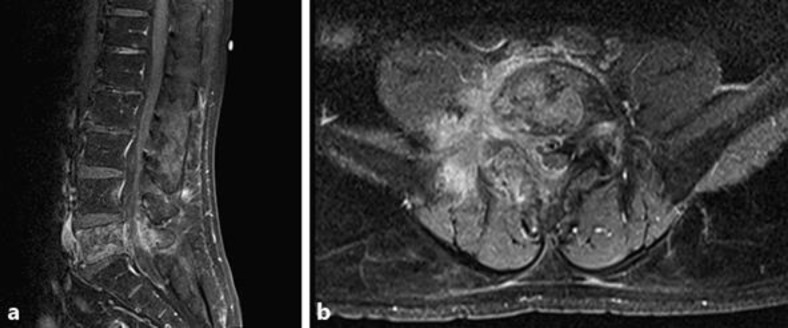
The patient remained disease-free on yearly follow-up CT scans until October 2009 (a disease-free interval of 4.5 years), when he presented with backache associated with right leg numbness. Spine MRI (Fig. 1) showed abnormal signal in the L5 vertebral body with bony expansion of the right pedicle and epidural soft tissue, highly suspicious for a bony metastatic deposit. There was encasement of the right L5 nerve root, probably accounting for the patient's symptoms of sciatica. Bone scan (Fig. 2a) and CTs showed no evidence of local recurrence or any other sites of metastases. He underwent a biopsy of the L5 lesion which showed metastatic carcinoma, consistent with an origin of undifferentiated carcinoma.
Fig. 1.
Sagittal (a) and axial (b) views of contrast-enhanced MRI scan showing tumour at L5.
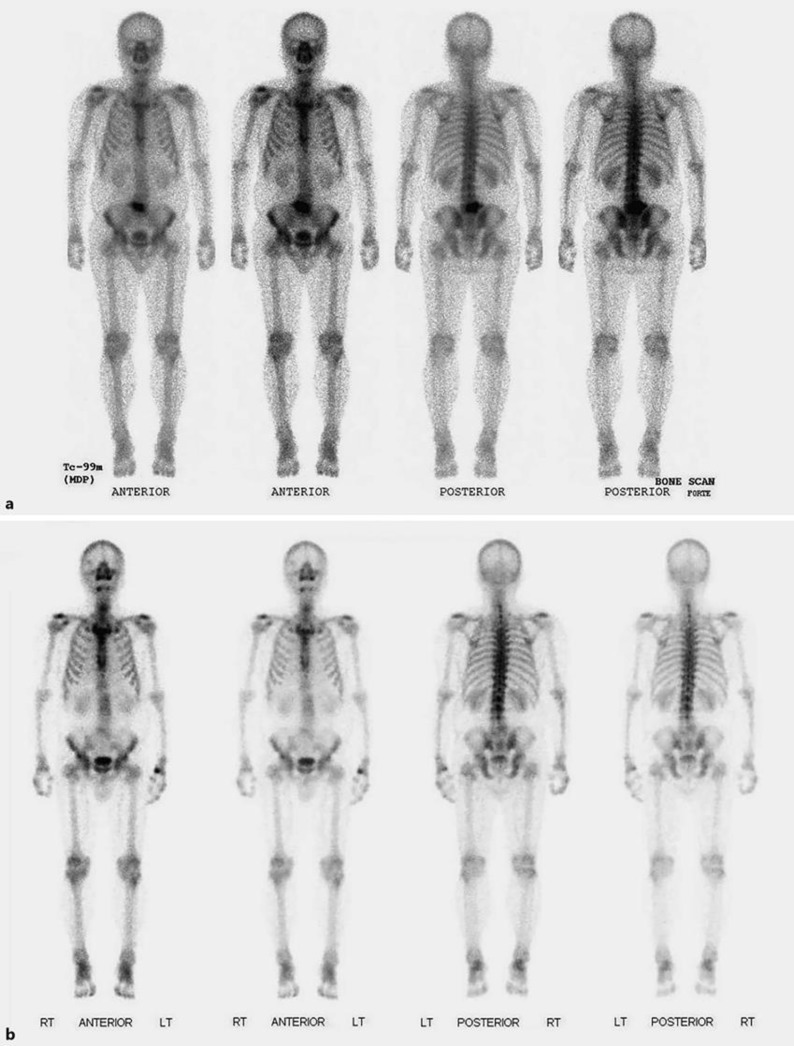
Fig. 2.
Bone scans in 2009 (a) and 2017 (b) showing pre-treatment disease at L5, and subsequent resolution on long-term follow-up.
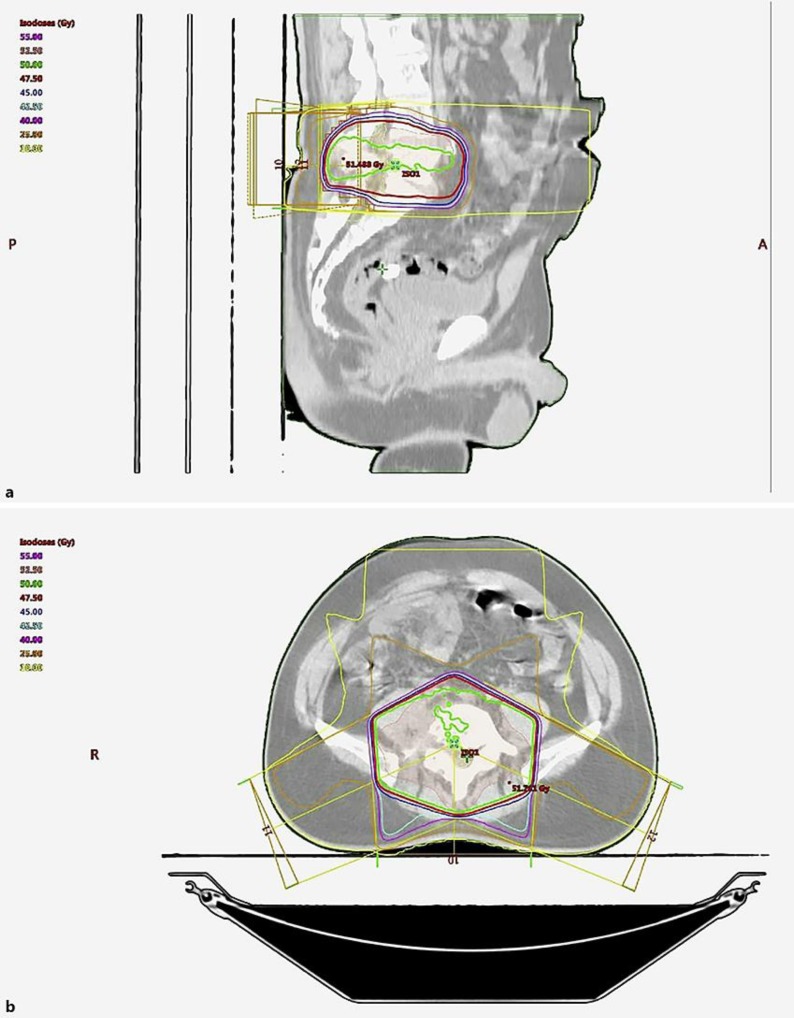
The patient went on to receive high-dose palliative radiotherapy to the vertebral metastasis at a dose of 50 Gy/20# (2.5 Gy per fraction) between November and December 2009. The treatment field included the L4 vertebrae as well as the bilateral sacroiliac joints. A 3D conformal plan with 1 posterior and 2 oblique wedged fields was used (Fig. 3). The cauda equina received a maximum point dose of 50.8 Gy and mean dose of 24.8 Gy. Other organs at risk, i.e. bladder and femoral heads, received minimal doses.
Fig. 3.
Sagittal (a) and axial (b) views of the radiotherapy treatment plan.
During this course of radiotherapy, the patient complained of worsening pain after the 3rd fraction with pain radiating to the right L5 dermatome. This was controlled with analgesia. His power and sensation remained intact. By the 3rd week of treatment, his pain had improved. He completed 20 fractions of treatment successfully and has remained disease free to the time of writing on serial CT and bone scans (Fig. 2b). On his latest clinical examination in March 2018, he was well with no neurological deficits – a disease-free interval of over 8 years.
Discussion
Metastases in nasopharyngeal carcinoma are fairly common. Around 6% of patients have metastatic disease at diagnosis, and around 25–30% of patients develop metastases eventually. Like several other cancers, bone metastases are the most frequent site of metastases in nasopharyngeal carcinoma, other common sites being lung and liver [3]. Traditionally, chemotherapy is the mainstay of treatment for metastatic nasopharyngeal carcinoma, with platinum-containing doublet regimens typically being used as first-line treatment. Second-line capecitabine, gemcitabine, and docetaxel monotherapy can be used in platinum-resistant patients. Targeted therapies such as cetuximab and sunitinib have been used; however, overall effectiveness has been limited. Typical response rates to chemotherapy in published studies have been about 20–40%, with a median survival of 7–14 months [3, 4].
Despite various chemotherapeutic options, reports of long-term survivors with proven metastatic nasopharyngeal carcinoma are few and far between. In a report of 17 patients who survived past 2 years after diagnosis of metastatic disease, the only patients who survived more than 5 years were those with only intrathoracic metastases who showed complete response to chemotherapy, as well as 1 patient with a thyroid metastasis that was completely resected [5]. Interestingly, a comparison between transarterial chemoembolisation (TACE) and partial hepatectomy of patients with liver metastases from nasopharyngeal carcinoma showed that patients undergoing partial hepatectomy had increased survival, showing some advantage for locally ablative treatment of oligometastases. While most of these patients undergoing partial hepatectomy and TACE progressed eventually, one patient survived 168 months after partial hepatectomy without progression [6].
Multimodality treatment combining both chemotherapy and radiotherapy has been proposed for patients with good performance status and few metastases. For instance, Shen et al. [7] showed that combined chemoradiotherapy could significantly benefit patients with solitary bone metastases. Of 58 patients that were studied with solitary metastases, 28 received both chemotherapy and radiotherapy (to a median dose of 40 Gy), and these had significantly improved overall survival. However, differing radiotherapy and chemotherapy regimens have made overall comparisons difficult.
Indeed, our case is unusual in that this long-term survivor did not receive chemotherapy during the course of his treatment. High-dose palliative radiotherapy is also not frequently given, with the most common palliative regimens for bone metastases being 8 Gy/1#, 20 Gy/5#, and 30 Gy/10# [8, 9]. More recently, higher doses of radiotherapy for isolated (or few) bone metastases have become more commonly used in the form of stereotactic body radiotherapy (SBRT), a highly conformal high-dose radiation treatment with a small margin, which has shown excellent pain control and disease control results though with some incidences of vertebral fractures and myelopathy [9, 10, 11]. Indeed, a case published in 2014 regarding an adolescent male with a left iliac bone metastasis from nasopharyngeal carcinoma was treated with induction chemotherapy followed by SBRT, 40 Gy/5# to the left iliac metastasis. He had shown a 4-year progression-free survival period at the time of publication in 2014 [12].
To our knowledge, this is the first report of a long-term survivor of metastatic nasopharyngeal carcinoma with a solitary bone metastasis who had received no chemotherapy, and was treated with high-dose palliative radiotherapy. In view of this case, there may be potential for other patients with oligometastases from nasopharyngeal carcinoma to be treated with local therapy alone, thereby sparing them the toxicities of chemotherapy.
Statement of Ethics
Informed consent from the patient has been obtained.
Disclosure Statement
The authors declare no conflicts of interest.
References
- 1.British Association of Otorhinolaryngology . Head and Neck Cancers Multidisciplinary Management Guidelines. 4th ed. London: ENT UK; 2011. [Google Scholar]
- 2.Hanna L, Crosby T, Macbeth F. Practical Clinical Oncology. 2nd ed. Cambridge: Cambridge University Press; 2015. [Google Scholar]
- 3.Bensouda Y, Kaikani W, Ahbeddou N, Rahhali R, Jabri M, Mrabti H, et al. Treatment for metastatic nasopharyngeal carcinoma. Eur Ann Otorhinolaryngol Head Neck Dis. 2011 Apr;128((2)):79–85. doi: 10.1016/j.anorl.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Prawira A, Oosting SF, Chen TW, Delos Santos KA, Saluja R, Wang L, et al. Systemic therapies for recurrent or metastatic nasopharyngeal carcinoma: a systematic review. Br J Cancer. 2017 Dec;117((12)):1743–52. doi: 10.1038/bjc.2017.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teo PM, Kwan WH, Lee WY, Leung SF, Johnson PJ. Prognosticators determining survival subsequent to distant metastasis from nasopharyngeal carcinoma. Cancer. 1996 Jun;77((12)):2423–31. doi: 10.1002/(SICI)1097-0142(19960615)77:12<2423::AID-CNCR2>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 6.Huang J, Li Q, Zheng Y, Shen J, Li B, Zou R, et al. Partial hepatectomy for liver metastases from nasopharyngeal carcinoma: a comparative study and review of the literature. BMC Cancer. 2014 Nov;14((1)):818. doi: 10.1186/1471-2407-14-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen L, Dong J, Li S, Wang Y, Dong A, Shu W, et al. M1 stage subdivision and treatment outcome of patients with bone-only metastasis of nasopharyngeal carcinoma. Oncologist. 2015 Mar;20((3)):291–8. doi: 10.1634/theoncologist.2014-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nielsen OS, Bentzen SM, Sandberg E, Gadeberg CC, Timothy AR. Randomized trial of single dose versus fractionated palliative radiotherapy of bone metastases. Radiother Oncol. 1998 Jun;47((3)):233–40. doi: 10.1016/s0167-8140(98)00011-5. [DOI] [PubMed] [Google Scholar]
- 9.De Felice F, Piccioli A, Musio D, Tombolini V. The role of radiation therapy in bone metastases management. Oncotarget. 2017 Apr;8((15)):25691–9. doi: 10.18632/oncotarget.14823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huo M, Sahgal A, Pryor D, Redmond K, Lo S, Foote M. Stereotactic spine radiosurgery: review of safety and efficacy with respect to dose and fractionation. Surg Neurol Int. 2017 Feb;8((1)):30. doi: 10.4103/2152-7806.200581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joaquim AF, Ghizoni E, Tedeschi H, Pereira EB, Giacomini LA. Stereotactic radiosurgery for spinal metastases: a literature review. Einstein (Sao Paulo) 2013 Apr-Jun;11((2)):247–55. doi: 10.1590/S1679-45082013000200020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farnia B, Louis CU, Teh BS, Paulino AC. Stereotactic body radiation therapy (SBRT) for an isolated bone metastasis in an adolescent male with nasopharyngeal carcinoma. Pediatr Blood Cancer. 2014 Aug;61((8)):1520. doi: 10.1002/pbc.24963. [DOI] [PubMed] [Google Scholar]