Abstract
Inflammatory linear verrucous epidermal nevus (ILVEN) is an epidermal nevus that clinically and histologically mimics linear psoriasis. The pathogenesis of psoriasis has been widely investigated, with recent studies focusing especially on targeting proinflammatory cytokines such as IL-17A, TNFα, IL-23, and IL-12, while little is known about ILVEN. Since the treatment for ILVEN varies widely from the administration of topical ointment for psoriasis to invasive methods such as carbon dioxide gas laser, the differential diagnosis between ILVEN and psoriasis is necessary. In this report, we describe a case of widely spread unilateral ILVEN that clinically and histologically mimicked psoriasis vulgaris and could be diagnosed by immunohistochemical staining focused on the IL-36γ/IL-17A axis.
Keywords: Inflammatory linear verrucous epidermal nevus, ILVEN, Psoriasis, IL-36Iγ, IL-17, Differential diagnosis
Introduction
The pathogenesis of psoriasis has been widely investigated, with recent studies focusing on the immunological microenvironment to develop biological drugs targeting proinflammatory cytokines such as IL-17A, TNFα, IL-23, and IL-12 [1, 2]. These reports strongly suggested the significance of these proinflammatory cytokines in the pathogenesis of psoriasis. Inflammatory linear verrucous epidermal nevus (ILVEN) is an epidermal nevus that clinically and histologically mimics linear psoriasis [3, 4, 5, 6, 7]. Since the treatment for ILVEN varies widely from the administration of topical ointment for psoriasis to invasive methods such as carbon dioxide gas laser8, the differential diagnosis between ILVEN and psoriasis is necessary. In this report, we describe a case of wide-spread unilateral ILVEN that clinically and histologically mimicked psoriasis vulgaris, diagnosed by immunohistochemical staining focused on the IL-36γ/IL-17A axis.
Case Report
A 14-year-old Japanese girl visited our outpatient clinic with therapy-resistant, unilateral, itchy plaques. She had been treated in a private clinic for what was considered psoriasis and was administered topical steroid and calcipotriol hydrate with inadequate effects. At her initial visit, physical examination revealed brown to skin-colored, infiltrated, scaly erythema and papules on her left trunk, upper limbs, and lower extremities along the Blashko line (Fig. 1a, b, c, d). A full blood count and biochemical profile were within normal ranges. A biopsy specimen showed elongated rete ridges, parakeratosis, and dilated tortuous vessels in the dermal papillae (Fig. 1d), and neutrophils were rarely detected in the specimen (Fig. 1f). From the above findings, we diagnosed wide-spread unilateral inflammatory linear verrucous epidermal nevus (ILVEN) in this patient.
Fig. 1.
Infiltrated scaly erythema and papules on our patient's left trunk (a), back (b), and lower extremities (c, d) along the Blashko line. Elongated rete ridges, parakeratosis, and dilated tortuous vessels in the dermal papillae (e, f). (Original magnification: ×50 [e], ×200 [f]).
Since the histological findings are mimicking psoriasis vulgaris, we further employed immunohistochemical (IHC) staining of IL-36γ, IL-36R, IL-17, and IL-17R for 5 additional cases of ILVEN and 5 cases of psoriasis vulgaris and compared them with our present case. IHC staining revealed that the epidermal keratinocytes in the lesional skin of psoriasis cases were positive for IL-36γ, whereas those of ILVEN were negative for IL-36γ in each of the 5 cases (Fig. 2a, b). In contrast, IL-36R-expressing cells were detected in the lesional skin of psoriasis and ILVEN cases (Fig. 2c, d). IL-17-producing cells were detected in ILVEN and psoriasis cases (Fig. 2e). On the epidermal keratinocytes in the lesional skin of both psoriasis and ILVEN cases, the epidermis was positive for IL-17R (Fig. 2f). Concerning our present case, IL-36γ production was decreased in the epidermis (Fig. 3a), whereas IL-17R was expressed on epidermal keratinocytes (Fig. 3b) with scattered IL-36R-expressing cells (Fig. 3c) and IL-17-producing cells (Fig. 3d).
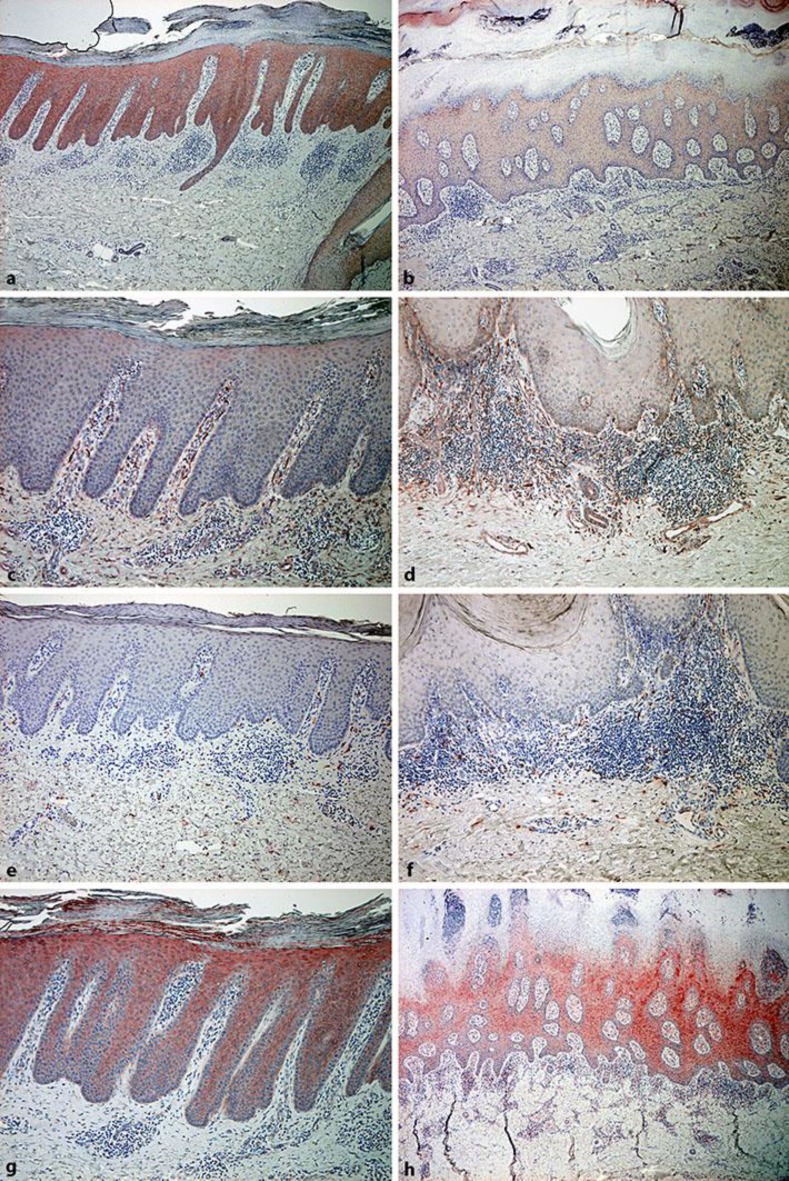
Fig. 2.
Representative figures of immunohistochemical staining for 5 historical samples of psoriasis and ILVEN. Paraffin-embedded psoriasis (a, c, e, g) and ILVEN (b, d, f, h) samples were deparaffinized and stained with anti-IL-36γ antibodies (a, b), anti-IL-36R antibodies (c, d), anti-IL-17 antibodies (e, f), and anti-IL-17R antibodies (g, h). The sections were developed with liquid permanent red. (Original magnification: ×50 [a, b], ×100 [c–h]).
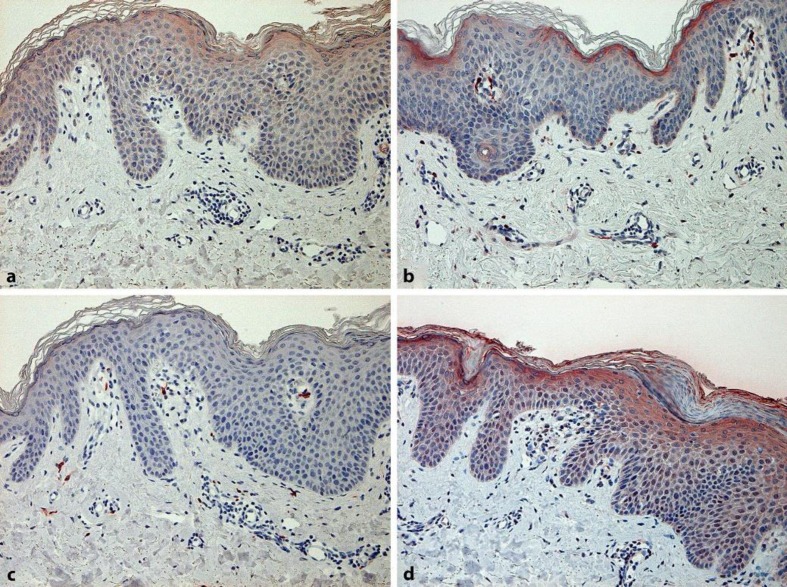
Fig. 3.
Immunohistochemical staining of the present case. Paraffin-embedded samples were deparaffinized and stained with anti-IL-36γ antibodies (a), anti-IL-36R antibodies (b), anti-IL-17 antibodies (c), and anti-IL-17R antibodies (d). The sections were developed with liquid permanent red. (Original magnification: ×200).
Discussion
ILVEN is an epidermal nevus that clinically and histologically mimics linear psoriasis [3, 4, 5, 6, 7]. In addition, ILVEN occasionally responds to the antipsoriatic drug calcipotriol, and even responds to anti-TNF antibodies such as etanercept [3]. Since the treatment of ILVEN is still challenging, and some of them (e.g., carbon dioxide gas laser) are invasive and should not be used for psoriasis patients [8], the precise diagnosis for ILVEN is mandatory when applying such invasive therapy.
As previous reports suggested, epidermal keratinocytes highly express IL-36α, IL-36β, and IL-36γ in the lesional skin and play a crucial role in the pathogenesis of psoriasis vulgaris [9]. Indeed, IL-36γ could be activated by cathepsin S expressed in keratinocytes [9], promoting the production of proinflammatory cytokines such as IL-17A, TNFα, IL-6, IL-8, and IL-22 [10]. In addition, IL-36 agonists promote human keratinocytes to express various chemokines, including CCL20, which can recruit Th17 in the lesional skin [11]. Since anti-IL-17A antibody is one of the optimal biological drugs [12], the IL-36Iγ/IL-17A axis could be the main pathway for the development of psoriasis.
From the above findings, we hypothesized that the IL-36γ/IL-17A axis in ILVEN and psoriasis might be different given the difference in their clinical course. To test our hypothesis, we employed IHC staining of IL-36hγ as well as IL-36R for the differential diagnosis of ILVEN and psoriasis vulgaris, using historical samples. Although IL-36R-possessing cells were detected, the expression of IL-36eγ was decreased on the epidermal keratinocytes in our present case compared with that in psoriasis lesions. Interestingly, the tendency of both IL-17-producing cells and IL-17R expression was similar in the two groups, suggesting similarities in the clinical findings of these two disorders. This report presents a small number of cases, but further cases may provide fundamental insights into the mechanisms of the effects of decreased expression of IL-36dγ on ILVEN.
Statement of Ethics
Our patient's parents gave written informed consent for this case to be published.
Disclosure Statement
The authors have no conflicting interests to declare.
Author Contributions
K.T. treated the patient and acquired the clinical data. T.F. is responsible for the conception and design of this study, the acquisition of the clinical data, the analysis and interpretation of the data, the writing, review, and/or revision of the manuscript, and study supervision. Y.S. performed immunohistochemical staining. C.L. performed immunohistochemical staining. S.A. acted as study supervisor.
References
- 1.Hawkes JE, Chan TC, Krueger JG. Psoriasis pathogenesis and the development of novel targeted immune therapies. J Allergy Clin Immunol. 2017 Sep;140((3)):645–53. doi: 10.1016/j.jaci.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Furue K, Yamamura K, Tsuji G, Mitoma C, Uchi H, Nakahara T, et al. Highlighting Interleukin-36 Signalling in Plaque Psoriasis and Pustular Psoriasis. Acta Derm Venereol. 2018 Jan;98((1)):5–13. doi: 10.2340/00015555-2808. [DOI] [PubMed] [Google Scholar]
- 3.Renner R, Colsman A, Sticherling M, ILVEN is it psoriasis? Debate based on successful treatment with etanercept. Acta Derm Venereol. 2008;88((6)):631–2. doi: 10.2340/00015555-0522. [DOI] [PubMed] [Google Scholar]
- 4.Abbasi N, Fangman WL, Rosenman KS, Schaffer JV. ILVEN-like persistent psoriasiform dermatitis confined to a congenital Becker nevus. Pediatr Dermatol. 2008 Pediatr Dermatol;25((3)):390–1. doi: 10.1111/j.1525-1470.2008.00690.x. [DOI] [PubMed] [Google Scholar]
- 5.Happle R. Linear psoriasis and ILVEN: is lumping or splitting appropriate? Dermatology. 2006;212((2)):101–2. doi: 10.1159/000090647. [DOI] [PubMed] [Google Scholar]
- 6.Vissers WH, Muys L, Erp PE, de Jong EM, van de Kerkhof PC. Immunohistochemical differentiation between inflammatory linear verrucous epidermal nevus (ILVEN) and psoriasis. Eur J Dermatol. 2004 Jul-Aug;14((4)):216–20. [PubMed] [Google Scholar]
- 7.Lee SH, Rogers M. Inflammatory linear verrucous epidermal naevi: a review of 23 cases. Australas J Dermatol. 2001 Nov;42((4)):252–6. doi: 10.1046/j.1440-0960.2001.00530.x. [DOI] [PubMed] [Google Scholar]
- 8.D'Antuono A, Balestri R, Zauli S, Bardazzi F, Bellavista S, Banzola N, et al. Carbon dioxide laser: first-line therapy in vulvar inflammatory linear verrucous epidermal nevus. Dermatol Ther (Heidelb) 2012 Dermatol Ther (Heidelb)25((1)):92–4. doi: 10.1111/j.1529-8019.2012.01429.x. [DOI] [PubMed] [Google Scholar]
- 9.Ding L, Wang X, Hong X, Lu L, Liu D. IL-36 cytokines in autoimmunity and inflammatory disease. Oncotarget. 2017 Dec;9((2)):2895–901. doi: 10.18632/oncotarget.22814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrier Y, Ma HL, Ramon HE, Napierata L, Small C, O'Toole M, et al. Inter-regulation of Th17 cytokines and the IL-36 cytokines in vitro and in vivo: implications in psoriasis pathogenesis. J Invest Dermatol. 2011 Dec;131((12)):2428–37. doi: 10.1038/jid.2011.234. [DOI] [PubMed] [Google Scholar]
- 11.Foster AM, Baliwag J, Chen CS, Guzman AM, Stoll SW, Gudjonsson JE, et al. IL-36 promotes myeloid cell infiltration, and inflammatory activity in skin. J Immunol. 2014 Jun;192((12)):6053–61. doi: 10.4049/jimmunol.1301481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Frieder J, Kivelevitch D, Menter A. Secukinumab: a review of the anti-IL-17A biologic for the treatment of psoriasis. Ther Adv Chronic Dis. 2018 Jan;9((1)):5–21. doi: 10.1177/2040622317738910. [DOI] [PMC free article] [PubMed] [Google Scholar]