Abstract
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) is ubiquitous. However, it remains an oftentimes under-recognized risk factor for the development of strictures and small bowel obstruction. Herein we describe the case of a 63-year-old female with a prolonged course of abdominal pain and occult anemia found to have a diaphragmatic stricture in the small bowel related to chronic NSAID use.
Keywords: NSAIDs, Diaphragm disease, Small bowel stricture, Nonsteroidal anti-inflammatory drugs
Introduction
Strictures of the small bowel are a relatively uncommon phenomenon, with etiology most often related to conditions such as Crohn's disease and Behçet's disease [1]. Clinically, these cases often follow a protracted course wherein a patient presents with recurrent small bowel obstructions, occult abdominal pain, and/or recalcitrant anemia from gastrointestinal bleeding. Workup including esophagogastroduodenoscopy (EGD) and colonoscopies may be largely negative. Retained video capsule endoscopy is an important clue alerting the physician to this possible diagnosis [2, 3, 4].
Nonsteroidal anti-inflammatory drugs (NSAIDs) are one of the most commonly utilized medications with reports showing 13% of the US population using these medications regularly [5]. Mechanistically, NSAIDs work through inhibition of cyclooxygenase (COX) with resulting modulation of prostaglandin synthesis. However, the particular bowel wall alterations observed in chronic NSAID users appear to be related to direct mucosal toxicity rather than systemic COX modulation [6]. These local inflammatory changes, which are related to disruption of membrane phospholipids in the bowel wall [7] in addition to mitochondrial perturbations leading to the generation of reactive oxygen species [8, 9], result in the formation of circumferential strictures resembling a diaphragm. It has been proposed that the generation of such a stricture is the result of a chronic cycle of injury and repair with the deposition of a collagenous scar resulting in intraluminal narrowing akin to a “drawstring” [10, 11].
Case Presentation
A 63-year-old Caucasian female presented to the General Surgery outpatient clinic via her general practitioner with an 8-year history of chronic, intermittent abdominal pain and multiple workups unsuccessful in determining the etiology of her pain. She reported her pain to be sporadic “coming on in waves” and associated with bloating but without nausea or emesis. Her physical exam revealed poorly localized, nonspecific tenderness to abdominal palpation. She denied any related signs including diarrhea, constipation, blood per rectum, or weight loss but was recently diagnosed with iron deficiency anemia (hemoglobin 8.2 g/dL, hematocrit 28.3%, iron level 20 μg/dL, TIBC 514 μg/dL, iron saturation 4%, platelets 452,000/μL, fecal occult blood testing was negative) for which she was taking oral and occasionally parenteral iron supplementation. Prior workups had been extensive including several colonoscopies significant only for mild diverticulosis, internal hemorrhoids but no polyps. The patient had previously undergone laparoscopic lysis of adhesions for a presumed small bowel obstruction which had offered her temporary symptomatic relief. She had negative fecal occult blood testing and an upper endoscopy with biopsies had failed to demonstrate an etiology. She was previously diagnosed with small intestinal bacterial overgrowth and was treated with a course of rifaximin. A workup for intermittent porphyria was also pursued prior to her presentation, which likewise was negative.
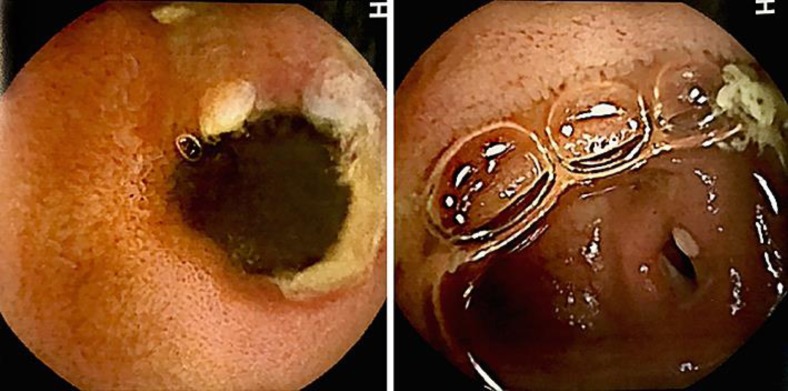
In light of her ongoing iron deficiency anemia and unresolved abdominal pain, a capsule endoscopy was performed to assess for arteriovenous malformation. A diaphragmatic stricture was identified in the small bowel following retention of the capsule at that level (Fig. 1).
Fig. 1.
Images of diaphragmatic small bowel stricture with circumferential erythema observed on review of capsule endoscopy.
The patient underwent a diagnostic laparoscopy with conversion to a mini-laparotomy and subsequent Heineke-Mikulicz strictureplasty in the ileum approximately 25 cm proximal to the ileocecal valve with resolution of her symptoms and iron deficiency.
Discussion
Initially termed “diaphragm disease,” the association between NSAID use and small bowel stricture formation has been known for some time [12, 13]; however, it was Debenham in 1996 who first demonstrated NSAID use as a causative agent in this enteropathy [14].
To date, there have been only 45 reported cases of diaphragmatic disease requiring surgical intervention [15]. While the cases included in Munipalle's review did not show any small bowel pathology, stricture formation has been shown to be induced by NSAIDs [12]. While this condition remains rare, there has been a substantial rise in the use of the most important etiologic factor; namely NSAIDs. Data from the 2010 National Health Interview Study demonstrated an estimated prevalence of regular NSAID use of nearly 43 million (19%) among US adults aged 18 years and older [5]. While most cases are chronic, this condition has been associated with NSAID use in as little as 2 months [16]. Diaphragm disease is associated with a female predominance with the onset of most cases seen in the seventh decade. The majority of these patients present with chronic symptoms with a median duration of 3 months. The most common presenting symptoms are anemia and abdominal pain [15]. Due to unfamiliarity with the condition and vague and often intermittent patient symptoms, delayed presentation is not uncommon with a reported range upward of 11.5 years [17].
Given the extensive use of NSAIDs, we offer this case to both familiarize clinicians with this disease entity and as a reminder to consider NSAID-induced small bowel stricture in the differential diagnosis of otherwise unexplained recurrent abdominal pain and occult gastrointestinal bleeding.
Statement of Ethics
The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.May A, Nachbar L, Pohl J, Ell C. Endoscopic interventions in the small bowel using double balloon enteroscopy: feasibility and limitations. Am J Gastroenterol. 2007 Mar;102((3)):527–35. doi: 10.1111/j.1572-0241.2007.01063.x. [DOI] [PubMed] [Google Scholar]
- 2.Pennazio M, Eisen G, Goldfarb N. ICCE: ICCE consensus for obscure gastrointestinal bleeding. Endoscopy. 2005 Oct;37((10)):1046–50. doi: 10.1055/s-2005-870319. [DOI] [PubMed] [Google Scholar]
- 3.Flicek KT, Hara AK, De Petris G, Pasha SF, Yadav AD, Johnson CD. Diaphragm disease of the small bowel: a retrospective review of CT findings. AJR Am J Roentgenol. 2014 Feb;202((2)):W140–5. doi: 10.2214/AJR.13.10732. [DOI] [PubMed] [Google Scholar]
- 4.Li F, Gurudu SR, De Petris G, Sharma VK, Shiff AD, Heigh RI, et al. Retention of the capsule endoscope: a single-center experience of 1000 capsule endoscopy procedures. Gastrointest Endosc. 2008 Jul;68((1)):174–80. doi: 10.1016/j.gie.2008.02.037. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Y, Boudreau DM, Freedman AN. Trends in the use of aspirin and nonsteroidal anti-inflammatory drugs in the general U.S. population. Pharmacoepidemiol Drug Saf. 2014 Jan;23((1)):43–50. doi: 10.1002/pds.3463. [DOI] [PubMed] [Google Scholar]
- 6.van Oijen MG, Dieleman JP, Laheij RJ, Sturkenboom MC, Jansen JB, Verheugt FW. Peptic ulcerations are related to systemic rather than local effects of low-dose aspirin. Clin Gastroenterol Hepatol. 2008 Mar;6((3)):309–13. doi: 10.1016/j.cgh.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 7.Higuchi K, Umegaki E, Watanabe T, Yoda Y, Morita E, Murano M, et al. Present status and strategy of NSAIDs-induced small bowel injury. J Gastroenterol. 2009;44((9)):879–88. doi: 10.1007/s00535-009-0102-2. [DOI] [PubMed] [Google Scholar]
- 8.Wallace JL. Mechanisms, prevention and clinical implications of nonsteroidal anti-inflammatory drug-enteropathy. World J Gastroenterol. 2013 Mar;19((12)):1861–76. doi: 10.3748/wjg.v19.i12.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whittle BJ. Mechanisms underlying intestinal injury induced by anti-inflammatory COX inhibitors. Eur J Pharmacol. 2004 Oct;500((1–3)):427–39. doi: 10.1016/j.ejphar.2004.07.042. [DOI] [PubMed] [Google Scholar]
- 10.Going JJ, Canvin J, Sturrock R. Possible precursor of diaphragm disease in the small intestine. Lancet. 1993 Mar;341((8845)):638–9. doi: 10.1016/0140-6736(93)90407-8. [DOI] [PubMed] [Google Scholar]
- 11.Zhao B, Sanati S, Eltorky M. Diaphragm disease: complete small bowel obstruction after long-term nonsteroidal anti-inflammatory drugs use. Ann Diagn Pathol. 2005 Jun;9((3)):169–73. doi: 10.1016/j.anndiagpath.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Lang J, Price AB, Levi AJ, Burke M, Gumpel JM, Bjarnason I. Diaphragm disease: pathology of disease of the small intestine induced by non-steroidal anti-inflammatory drugs. J Clin Pathol. 1988 May;41((5)):516–26. doi: 10.1136/jcp.41.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheers R, Williams WR. NSAIDs and gut damage. Lancet. 1989 Nov;2((8672)):1154. doi: 10.1016/s0140-6736(89)91515-8. [DOI] [PubMed] [Google Scholar]
- 14.Debenham GP. Ulcer of the cecum during oxyphenbutazone (tandearil) therapy. Can Med Assoc J. 1966 May;94((22)):1182–4. [PMC free article] [PubMed] [Google Scholar]
- 15.Munipalle PC, Garud T, Light D. Diaphragmatic disease of the colon: systematic review. Colorectal Dis. 2013 Sep;15((9)):1063–9. doi: 10.1111/codi.12218. [DOI] [PubMed] [Google Scholar]
- 16.Aftab AR, Donnellan F, Zeb F, Kevans D, Cullen G, Courtney G. NSAID-induced colopathy: A case series. J Gastrointestin Liver Dis. 2010 Mar;19((1)):89–91. [PubMed] [Google Scholar]
- 17.Püspök A, Kiener HP, Oberhuber G. Clinical, endoscopic, and histologic spectrum of nonsteroidal anti-inflammatory drug-induced lesions in the colon. Dis Colon Rectum. 2000 May;43((5)):685–91. doi: 10.1007/BF02235589. [DOI] [PubMed] [Google Scholar]