Abstract
Objectives:
To evaluate the impact of cone beam CT (CBCT) in the diagnostic thinking efficacy, management and prognosis of patients with suspected Stage 0 medication-related osteonecrosis of the jaw (MRONJ).
Methods:
For 15 patients with suspected Stage 0 MRONJ, clinical photographs, a panoramic radiograph and selected CBCT sections were identified. 13 oral surgeons reviewed the material and answered 10 questions in two different sessions. First session included clinical photographs and panoramic radiographs, while second session also included CBCT images. Questions (Qs) referred to dental disease and bone abnormalities (Qs 1, 2 and 3), differential diagnosis (Qs 4 and 5), patient management (Qs 6 and 7) and prognosis (Qs 8 and 9). Q 10 queried indication (first session) and usefulness (second session) of CBCT images.
Results:
Qs 2, 3, 5, 7 and 9 scores increased between sessions, with statistical differences for Qs 2, 3, 5 and 7 (<0.05). Patients 2, 8 and 11 showed a significant increase in the average score of all Qs between sessions, while scores for patient 10 nearly reached statistical significance (p = 0.055). For Q 10, 57.4% of answers reported that CBCT was needed (first session) and was beneficial (second session).
Conclusions:
CBCT had a significant impact in differential diagnosis and management of patients with suspected Stage 0 MRONJ.
Introduction
Since the initial reports of bisphosphonate (BP)-related osteonecrosis of the jaw (ONJ) cases in 2003 and 2004, the number of reports has continued to increase steadily.1, 2 Additional medications associated with increased risk for ONJ, including the monoclonal antibodies denosumab and bevacizumab and the multikinase inhibitor sunitinib have been identified.3–13 The most recent position paper by the American Association of Oral and Maxillofacial Surgeons proposed the term medication-related ONJ (MRONJ) to accommodate the growing number of MRONJ cases associated with other antiresorptive agents (denosumab) and antiangiogenic therapies.14
MRONJ is defined as exposed bone or bone that can be probed through an intraoral or extraoral fistula(e) in the maxillofacial region that has persisted for more than 8 weeks in patients on current or previous treatment with antiresorptive agents, which include BPs and denosumab, or antiangiogenic agents, without a history of radiation therapy to the jaws or obvious metastatic disease to the jaws.14 BPs and denosumab induce similar severity and prevalence of classic MRONJ disease with bone exposure.11,15–17
The current staging system of MRONJ involves Stages 0 to 3 and is based on patient clinical presentation. Patients with Stages 1 to 3 are defined in part by bone exposed to the oral cavity. However, Stage 0 is defined as: “Patients with no clinical evidence of exposed necrotic bone, but present with non-specific symptoms or clinical and radiographic findings”14 i.e. Stage 0 will not present with any exposed bone, making it difficult to diagnose. Indeed, Stage 0 MRONJ is a presumptive diagnosis based on excluding other conditions. As a result, Stage 0 disease may be underestimated or overdiagnosed.18–23 Properly diagnosing patients with Stage 0 MRONJ is further emphasized by the report that up to 50% of such patients may progress to the development of clinical MRONJ with bone exposure.24
Cone-beam CT (CBCT) has several advantages over conventional radiography in evaluating patients with diseases of the orofacial complex, including MRONJ.25–32 CBCT provides a more sensitive and detailed evaluation of the extent of bony changes and thus allows more accurate diagnosis, assessment of disease status and disease management.28–30 However, to our knowledge, there have been no previous reports that evaluate the importance of CBCT in patients with suspected Stage 0 MRONJ. Here, the purpose of our study was to assess the contribution of CBCT in the diagnostic thinking efficacy, management and treatment planning of patients with suspected of Stage 0 MRONJ.
Methods and materials
15 patients on antiresorptive medications for the management of bone neoplasia or osteoporosis were selected for the study. All patients were referred to the Oral and Maxillofacial Surgery clinic at the UCLA School of Dentistry from general dentists in the community for assessment of dental symptomatology. Approval of the study by the UCLA Institutional Review Board was obtained. All experiments followed the guidelines of the World Medical Association Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects.
Upon clinical examination, most patients demonstrated non-specific symptoms, including dull, aching bone pain in the jaws, sinus pain, or altered neurosensory function. Some patients were asymptomatic but presented with jaw expansion or oedema (Table 1). None of the patients showed evidence of bone exposure or bone that could be probed through an intraoral or extraoral fistula. Thus, it was expected that some of these patients had only common dental disease, while some might have developed Stage 0 MRONJ with or without dental disease.
Table 1.
Patient symptoms and clinical findings at initial visit
| Location | Symptoms | Intraoral presenting signs |
| Right Post. Maxilla | Pain | None |
| Right Post. Mand. | Pain | First molar residual root |
| Right Post. Mand. | Right facial pain | Large carious lesions of second premolar and first molar with gingival swelling |
| Right Post. Mand. | Pain and discomfort | Mandibular torus with oedema, erythema, tenderness |
| Left Post. Maxilla | Pain | Fistula in area of first molar |
| Right Post. Maxilla | Pain | None |
| Left Post. Mand. | Pain | Generalized caries |
| Right Post. Mand. | Pain and discomfort | Generalized caries |
| Right Post. Mand. | Diffuse pain and numbness | Large carious lesion in first molar |
| Left Post. Mand. | Pain and swelling | Erythema in area of missing second premolar and first molar without exposed bone |
| Right Post. Mand. | None | Mandibular expansion in area of second premolar to first molar |
| Right Post. Mand. | Pain | Missing crown of second molar |
| Right Post. Mand. | Pain | None |
| Left Ant. Maxilla | Discomfort | Erythema bone in canine area without exposed bone |
| Right Post. Mand. | Pain and swelling | Fistula in sockets of missing first and second molars without exposed bone |
The patient data included clinical photographs, panoramic radiographs and select CBCT images of the area of interests (Figure 1). CBCT images consisted of one corrected sagittal, three cross-sectional and one axial sections and one three-dimensional rendering of the area of interest. For all patients, the three-dimensional Accuitomo 170 scanner (J Morita USA, Irvine, CA) was used. The exposure factors were 90 kVp and 6 mA with a 17.5 s continuous exposure time, during 360° rotation, which were standard exposure settings. The field of view was 6 × 6 cm with a 0.125 mm isometric voxel or 10 × 14 cm with a 0.25 mm isometric voxel.
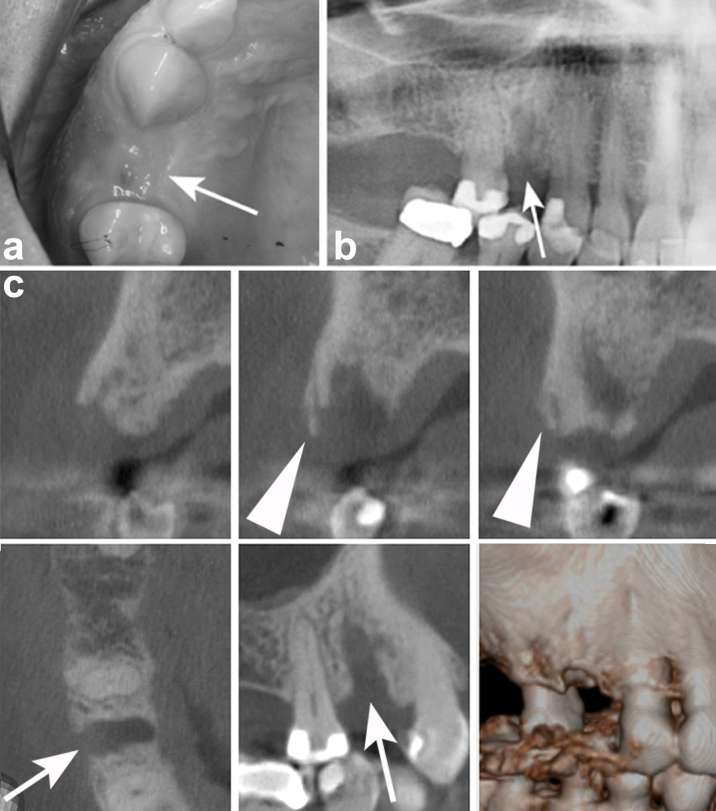
Figure 1.
Example of provided material for each patient: (a) clinical photograph, (b) panoramic radiograph (c) CBCT images of the area of interest. Arrows point to the extraction area of 14. Arrow heads point to possible sequestration of the buccal cortex of the maxilla in the area of 14. CBCT, cone beam CT.
A questionnaire consisting of 10 questions (Qs) per patient was created (Table 2). Each question was answered by checking one of nine checkboxes, from “Definitely Not (1)” to “Definitely Yes (9)”. 13 oral surgeons participated in the survey. All oral surgeons were private practitioners with a 5–10% volunteering commitment to the Oral and Maxillofacial Surgery Clinic at the UCLA School of Dentistry. The participants were informed that all patients were suspected of having Stage 0 MRONJ and were asked to review the images for each patient, and answer each question by checking only one of the nine checkboxes. Each case was presented on the 15.4-inch screen of a personal computer. The participants were surveyed twice, at least 1 month apart. In the first session, they were provided with clinical photographs and panoramic radiographs of the area of interest. In the second session, in addition to the clinical photographs and the panoramic radiographs, the participants were also provided with CBCT images of the area of interest. All cases for the first or second sessions were randomly ordered for each participant and for each session. The participants were assured that the purpose of the study was not to evaluate the accuracy of their answers, but, rather, to test the contribution of CBCT imaging in the differential diagnosis, management and prognosis of patients with suspected Stage 0 MRONJ.
Table 2.
Questionnaire
| 1. In the area of interest, do you see any dental disease (caries, periodontal or periapical disease, tooth fractures etc.)? |
| 2. In the area of interest, do you see any abnormalities involving the periodontal/periapical bone? |
| 3. In the area of interest, do you see any changes extending into the alveolar bone beyond the confines of periodontal/periapical area? |
| 4. Do you think that the radiographic appearance is only due to dental disease? |
| 5. Do you feel that the clinical and radiographic findings are consistent with Stage 0 ONJ? |
| 6. Based on your findings, would you treat the patient only for dental-related problems? |
| 7. Based on your analysis of the case, in addition to the dental issues, would you also manage the patient as Stage 0 ONJ case? |
| 8. Given the clinical and radiographic findings, do you feel that after treatment this patient will have a favourable outcome? |
| 9. Given the clinical and radiographic findings, do you feel that after treatment this patient is likely to develop clinical ONJ with exposed bone? |
| 10a. Given the clinical and radiographic findings, do you want to order a CBCT exam for further evaluation of this patient? (first session) |
| 10b. Do you feel that the CBCT added significant information for the diagnosis and management of this patient? (second session) |
| Participants scored each question by checking one of nine checkboxes, as shown. |
| Definitely NOT □ □ □ □ □ □ □ □ □ definitely YES |
| 1 2 3 4 5 6 7 8 9 |
ONJ, osteonecrosis of the jaw.
All questions for the first and second sessions were the same, except for the last question (Q 10). Qs 1, 2 and 3, referred to clinical and radiographic observations, Qs 4 and 5 to interpretation of findings, Qs 6 and 7 to treatment decisions and Qs 8 and 9 to clinical prognosis. Q 10 inquired in the first session whether a CBCT scan for further evaluation of this patient was necessary, and in the second session whether the CBCT scan had added significant information for the participant’s decision.
Statistical analysis
First, we sought to investigate which questions tended to change the most after inclusion of CBCT exam results during the second scoring (Table 3). Our statistical model to formally test this was a generalized linear mixed effects model for each question (except Q 10) with the score as the outcome variable and a first/second indicator as the main predictor of interest with random patient and surgeon effects because all 13 surgeons scored the same set of patients.
Table 3.
Analysis of scores for each question
| Question | Mean (SD) | Difference (SD) | p-value | |
| First session | Second session | |||
| 1 | 7.22 (2.70) | 7.17 (2.76) | −0.04 (2.21) | 0.850 |
| 2 | 6.86 (2.75) | 7.43 (2.39) | 0.57 (2.40) | 0.009* |
| 3 | 6.29 (2.85) | 6.81 (2.76) | 0.51 (2.84) | 0.022* |
| 4 | 4.29 (2.66) | 4.14 (2.69) | −0.15 (2.35) | 0.450 |
| 5 | 5.04 (2.54) | 5.48 (2.58) | 0.44 (2.25) | 0.013* |
| 6 | 4.46 (2.84) | 4.17 (2.64) | −0.29 (2.52) | 0.150 |
| 7 | 5.30 (2.53) | 5.82 (2.52) | 0.52 (2.38) | 0.004* |
| 8 | 6.08 (1.80) | 5.95 (1.84) | −0.12 (2.05) | 0.410 |
| 9 | 4.75 (2.09) | 4.88 (1.91) | 0.13 (2.09) | 0.430 |
| 10 | 6.11 (2.80) | 7.13 (2.13) | N/A | N/A |
The scores in Qs 2, 3, 5 and 7 increased between first and second sessions with statistical differences (p < 0.05).
Next, we wanted to investigate which patients changed the most after inclusion of the CBCT exam results during the second scoring (Table 4), but only for the concrete questions that queried about diagnosis or management of osseous abnormalities (Qs 2, 3, 5, 7, 8 and 9). We formally tested for differences in each patient using a generalized linear mixed effects model with the average score of the questions mentioned above as the outcome variable and a first/second indicator variable as the main predictor of interest with a random surgeon effect.
Table 4. .
Analysis of scores for each patient, excluding scores for Qs 1, 4, 6 and 10
| Patients | Mean (SD) | Difference (SD) | Diff. p-value | |
| Firstst session | Second session | |||
| 1 | 5.79 (2.45) | 5.72 (2.42) | −0.08 (2.24) | 0.826 |
| 2 | 6.34 (1.95) | 6.95 (1.77) | 0.62 (2.03) | 0.033 |
| 3 | 6.69 (1.89) | 7.12 (1.75) | 0.42 (2.02) | 0.127 |
| 4 | 4.06 (2.77) | 4.50 (2.96) | 0.44 (2.17) | 0.341 |
| 5 | 6.45 (2.05) | 6.80 (1.94) | 0.35 (2.25) | 0.287 |
| 6 | 5.86 (2.33) | 5.76 (2.65) | −0.10 (2.55) | 0.764 |
| 7 | 6.58 (2.24) | 6.63 (2.08) | 0.05 (2.42) | 0.856 |
| 8 | 5.49 (2.38) | 6.26 (2.10) | 0.77 (2.73) | 0.029 |
| 9 | 6.97 (2.08) | 7.14 (2.24) | 0.17 (1.81) | 0.601 |
| 10 | 5.24 (2.65) | 5.92 (2.39) | 0.68 (2.51) | 0.055 |
| 11 | 3.62 (2.55) | 4.81 (2.40) | 1.19 (2.81) | 0.003 |
| 12 | 6.49 (1.99) | 6.80 (1.99) | 0.31 (2.42) | 0.334 |
| 13 | 5.86 (2.58) | 6.17 (2.39) | 0.31 (2.22) | 0.364 |
| 14 | 4.59 (2.31) | 4.59 (2.49) | 0.00 (2.74) | 0.999 |
| 15 | 5.56 (2.78) | 5.41 (2.93) |
−0.15 (1.73) | 0.689 |
Patients 2, 8 and 11 showed a significant increase in the average score of all Qs between first and second sessions (p < 0.05), while scores for patient 10 nearly reached statistical significance (p = 0.055).
Finally, we looked at Q 10 (pre/post) to see if those who thought the CBCT exam would be useful for further evaluation (pre) would feel like it added significant information to the diagnosis and management of the patient (post). This was coded as no if the score ranged from 1 to 4, neither if the score was 5, or yes if the score ranged from 6 to 9. Table 5 is a cross-tabulation of these questions across all patients and surgeons.
Table 5.
Analysis of scores for Q 10
| Second session | Total | ||||
| No | Neither Yes nor No | Yes | |||
| First session | No | 19 | 2 | 44 | 65 |
| Neither Yes nor No | 3 | 0 | 5 | 8 | |
| Yes | 7 | 3 | 112 | 122 | |
| Total | 29 | 5 | 161 | 195 | |
Scores 1–4 were defined as “No”, score 5 was defined as “Neither Yes nor No” and scores 6–9 were defined as “Yes”.
Statistical analyses were performed using SAS v. 9.3 (SAS Institute Inc. Cary, NY). Values are reported as mean (SD) unless otherwise noted. p-values < 0.05 were considered statistically significant.
Results
Table 3 shows the mean (SD) scores for each question in the first session, second session, the difference (SD) between the two sessions and corresponding p-values. Mean values ranged from 4.29 to 7.22 for the first session and from 4.14 to 7.43 for the second session. Q 1, 2 and 3 had the highest, while Q 4, 6 and 9 had the lowest scores for both sessions. The scores in Qs 2, 3, 5, 7 and 9 increased between first and second sessions, with statistical differences for Qs 2, 3, 5 and 7 (p < 0.05). Although the scores in Qs 1, 4, 6 and 8 decreased between first and second sessions, no statistical differences were detected.
We then explored whether CBCT was more useful for certain type of patients over others. Since CBCT appeared to affect the answers that referred to the diagnosis or management of osseous abnormalities, we calculated the average (SD) of all Qs except Qs 1, 4, 6 and 10 in the first and second session for each patient. Patients 2, 8 and 11 showed a significant increase in the average score of all Qs between sessions 1 and 2, while scores for patient 10 nearly reached statistical significance (p = 0.055). For the remaining 11 patients no statistical significance was observed (Table 4). Patient 8 is depicted in Figure 1. First premolar tooth in the right maxilla region is missing and the edentulous site is covered with nearly normal mucosa (Figure 1a, white arrow), with the exception of a small area of erythema on the distal aspect of the site. On the panoramic radiograph, a partially healed extraction socket of first premolar tooth in the right maxilla region is seen (Figure 1b, white arrow). On the CBCT sections, absence of the tooth socket healing, presence of a thickened lamina dura (Figure 1c, white arrows) and possible sequestration of the buccal cortex of the mandible (Figure 1c, white arrow heads) are noted.
Q 10 addressed the anticipated contribution of CBCT imaging in patient assessment (Table 5). In session 1, Q 10 queried whether a CBCT exam was needed for patient evaluation. Although in 122 (62.6%) instances surgeons thought that CBCT would provide additional important information, in 65 (33.3%) instances they thought that the clinical photographs and panoramic radiographs were sufficient for diagnosis and patient management. In the second session, Q 10 asked if CBCT imaging provided additional useful information for patient management. 161 (82.6%) indicated that CBCT had indeed provided significant information, while 19 (9.7%) responses indicated that CBCT was not useful. Importantly, in 44 of the 65 (67.7%) instances the “No” response in session 1 converted to “Yes” in session 2. These 44 instances also represent 22.6% of all responses.
Discussion
Stage 0 MRONJ is characterized by an absence of clinically exposed bone in patients presenting with non-specific symptoms or clinical and radiographic findings.14 As data are being collected in large clinical trials, the importance of Stage 0 diagnosis for complete assessment of MRONJ is apparent. However, Stage 0 disease may be underestimated,18–22 with up to 30% of MRONJ cases possibly presenting without exposed bone.24, 33 Approximately half of Stage 0 patients progress to Stage 1, 2 or 3 with clinical bone exposure.24, 34 Prompt and proper diagnosis of Stage 0 MRONJ will allow earlier patient management, including the removal of local instigating factors and the systemic control of chronic symptomatology with pain medication or infection with antibiotics, as well as frequent patient monitoring.14 On the other hand, it has been stated that “over-diagnosing patients with MRONJ could lead to detrimental effects in their skeletal health, especially if modification or discontinuation of the anti-resorptive medication is entertained”.23
Clinical MRONJ, in patients with history of BP treatment and bone exposure, usually does not pose a diagnostic challenge. However, no definitive diagnostic criteria for Stage 0 MRONJ have been established23 and diagnosis of the disease results by excluding other more common conditions, such as periodontal or periapical disease, occlusal trauma, neuropathic pain etc. In this process, radiographs can provide critical information to assist in the proper identification of the patient with Stage 0 MRONJ.
Two-dimensional (2D) intraoral or extraoral radiographs, such as periapical, bitewing and panoramic, are commonly used in everyday dental practice to radiographically evaluate the status of the dental, periodontal and osseous structures.35 CBCT is becoming more prevalent in the radiographic assessment of the dental patient. Because it is not affected by the intrinsic problems of structure superimposition and unpredictable magnification, CBCT provides clear advantages over 2D radiographs in identification and diagnosis of diseases affecting the jaws.35, 36
Diagnostic imaging contributes to the patient management process at multiple levels. Fryback and Thornbury have introduced a hierarchical model assessing the efficacy of diagnostic imaging.37 In this model, contribution of diagnostic imaging to the patient management process progresses from technical efficacy (Level 1), to diagnostic accuracy efficacy (level 2), to diagnostic thinking efficacy (level 3), to therapeutic efficacy (level 4), to patient outcome efficacy (level 5) and to societal efficacy (level 6). Following this six-tiered model, our study was designed to explore the diagnostic thinking efficacy (Level 3) of CBCT for the patient with Stage 0 MRONJ. As such, we designed our questionnaire to explore whether CBCT imaging was judged as “helpful” to making the diagnosis, and whether there was a difference in clinicians’ subjectively estimated diagnosis probabilities, treatment planning and prognosis. Thus, our questionnaire intended to assess participant’s assessment of the extent of radiographic changes (Qs 1–3), diagnosis (Qs 4 and 5), management (Qs 6 and 7) and prognosis (Qs 8 and 9) of dental disease vs osseous abnormalities.
CBCT availability statistically increased the scores for Qs addressing involvement of periodontal and osseous structures, and thus the diagnosis and management of patients for suspected Stage 0 MRONJ. However, CBCT did not affect diagnosis and management of dental disease. These findings suggest that while clinical photographs and panoramic radiographs provided sufficient information for evaluation of dental structures, CBCT images offered additional evidence for the assessment of osseous morphology of the alveolar ridge. Importantly and somewhat surprisingly, CBCT availability did not change anticipated patient outcomes, suggesting that the clinical scenario in combination with the clinical photograph and panoramic radiograph were the major determinants of decision-making.
We also observed that CBCT availability differentially altered scores in various patients. Figure 1 depicts one of the patients where availability of CBCT imaging statistically significantly increased the scores between the two sessions. Interestingly, salient features of altered socket healing and alveolar bone architecture, not clearly visualized on the panoramic radiographs, were captured on CBCT sections, possibly leading the participants to increase their scores.
Q 10 addressed the anticipated contribution of CBCT imaging in patient assessment. Our findings demonstrate the preference of oral surgeons for CBCT imaging in evaluation of patients with suspected Stage 0 MRONJ, and suggest that in approximately a quarter of instances CBCT provided unanticipated diagnostic information, significant for patient management.
CBCT has clear advantages over 2D imaging in characterizing the features of MRONJ. Especially, in early Stages of MRONJ, increased trabecular density may not be detected on panoramic radiographs but may be seen on CT.38 Indeed, conventional radiographs can underestimate the presence and extent of cortical and trabecular changes in patients with clinical MRONJ.39, 40 Thus, advanced imaging, including CBCT, has been recommended for patients with suspected Stage 0 MRONJ.41
There are three limitations associated with the present study. First, the sample size of 15 cases with suspected MRONJ was relatively limited. This was due to the overall low incidence of MRONJ, as well as to the practicality of executing the study, since all oral surgeons had to review all cases. Second, the participants were informed that all patients were suspected of having Stage 0 MRONJ, as well as of the purpose of the study. This information might have a priori biased on the participants’ decision making. However, we elected to provide this information because we wanted to reflect a real clinical scenario with pertinent information from medical history. Third, ground truth for the absence or presence of Stage 0 MRONJ was not possible to establish, since no definitive diagnostic criteria for Stage 0 MRONJ have been established.23 Thus, the sensitivity and specificity of CBCT in Stage 0 MRONJ could not be determined from our study.
Conclusions
CBCT had a significant impact in the diagnostic thinking efficacy and treatment planning of patients with suspected Stage 0 MRONJ. Given the challenging diagnosis and significant adverse effects of under- or over- diagnosing the disease, CBCT could provide valuable diagnostic tools for the management of patients with suspected Stage 0 MRONJ.
ACKNOWLEDGMENTS
This work was supported in part by NIH/NIDCR DE019465 (ST).
Contributor Information
Hiroaki Shimamoto, Email: h-shima@dent.osaka-u.ac.jp.
Tristan R Grogan, Email: TGrogan@mednet.ucla.edu.
Tomomi Tsujimoto, Email: tomo-mac@dent.osaka-u.ac.jp.
Naoya Kakimoto, Email: kakimoto-n@hiroshima-u.ac.jp.
Shumei Murakami, Email: shumei@dent.osaka-u.ac.jp.
David Elashoff, Email: DElashoff@mednet.ucla.edu.
Tara L Aghaloo, Email: taghaloo@dentistry.ucla.edu.
Sotirios Tetradis, Email: stetradis@dentistry.ucla.edu.
REFERENCES
- 1.Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003; 61: 1115–7. doi: 10.1016/S0278-2391(03)00720-1 [DOI] [PubMed] [Google Scholar]
- 2.Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 2004; 62: 527–34. doi: 10.1016/j.joms.2004.02.004 [DOI] [PubMed] [Google Scholar]
- 3.Estilo CL, Fornier M, Farooki A, Carlson D, Bohle G, Huryn JM. Osteonecrosis of the jaw related to bevacizumab. J Clin Oncol 2008; 26: 4037–8. doi: 10.1200/JCO.2007.15.5424 [DOI] [PubMed] [Google Scholar]
- 4.Greuter S, Schmid F, Ruhstaller T, Thuerlimann B. Bevacizumab-associated osteonecrosis of the jaw. Ann Oncol 2008; 19: 2091–2. doi: 10.1093/annonc/mdn653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serra E, Paolantonio M, Spoto G, Mastrangelo F, Tetè S, Dolci M. Bevacizumab-related osteneocrosis of the jaw. Int J Immunopathol Pharmacol 2009; 22: 1121–3. doi: 10.1177/039463200902200429 [DOI] [PubMed] [Google Scholar]
- 6.Guarneri V, Miles D, Robert N, Diéras V, Glaspy J, Smith I, et al. Bevacizumab and osteonecrosis of the jaw: incidence and association with bisphosphonate therapy in three large prospective trials in advanced breast cancer. Breast Cancer Res Treat 2010; 122: 181–8. doi: 10.1007/s10549-010-0866-3 [DOI] [PubMed] [Google Scholar]
- 7.Hopp RN, Pucci J, Santos-Silva AR, Jorge J. Osteonecrosis after administration of intravitreous bevacizumab. J Oral Maxillofac Surg 2012; 70: 632–5. doi: 10.1016/j.joms.2011.02.104 [DOI] [PubMed] [Google Scholar]
- 8.Katsenos S, Christophylakis C, Psathakis K. Osteonecrosis of the jaw in a patient with advanced non-small-cell lung cancer receiving bevacizumab. Arch Bronconeumol 2012; 48: 218–9. doi: 10.1016/j.arbres.2012.01.007 [DOI] [PubMed] [Google Scholar]
- 9.Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol 2010; 28: 5132–9. doi: 10.1200/JCO.2010.29.7101 [DOI] [PubMed] [Google Scholar]
- 10.Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 2011; 29: 1125–32. doi: 10.1200/JCO.2010.31.3304 [DOI] [PubMed] [Google Scholar]
- 11.Fizazi K, Carducci M, Smith M, Damião R, Brown J, Karsh L, et al. Denosumab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind study. Lancet 2011; 377: 813–22. doi: 10.1016/S0140-6736(10)62344-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koch FP, Walter C, Hansen T, Jäger E, Wagner W. Osteonecrosis of the jaw related to sunitinib. Oral Maxillofac Surg 2011; 15: 63–6. doi: 10.1007/s10006-010-0224-y [DOI] [PubMed] [Google Scholar]
- 13.Fleissig Y, Regev E, Lehman H. Sunitinib related osteonecrosis of jaw: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: e1–e3. doi: 10.1016/j.tripleo.2011.06.023 [DOI] [PubMed] [Google Scholar]
- 14.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw--2014 update. J Oral Maxillofac Surg 2014; 72: 1938–56. doi: 10.1016/j.joms.2014.04.031 [DOI] [PubMed] [Google Scholar]
- 15.Dranitsaris G, Hatzimichael E. Interpreting results from oncology clinical trials: a comparison of denosumab to zoledronic acid for the prevention of skeletal-related events in cancer patients. Support Care Cancer 2012; 20: 1353–60. doi: 10.1007/s00520-012-1461-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saad F, Brown JE, Van Poznak C, Ibrahim T, Stemmer SM, Stopeck AT, et al. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol 2012; 23: 1341–7. doi: 10.1093/annonc/mdr435 [DOI] [PubMed] [Google Scholar]
- 17.Smith MR, Saad F, Coleman R, Shore N, Fizazi K, Tombal B, et al. Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet 2012; 379: 39–46. doi: 10.1016/S0140-6736(11)61226-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel S, Choyee S, Uyanne J, Nguyen AL, Lee P, Sedghizadeh PP, et al. Non-exposed bisphosphonate-related osteonecrosis of the jaw: a critical assessment of current definition, staging, and treatment guidelines. Oral Dis 2012; 18: 625–32. doi: 10.1111/j.1601-0825.2012.01911.x [DOI] [PubMed] [Google Scholar]
- 19.Junquera L, Gallego L. Nonexposed bisphosphonate-related osteonecrosis of the jaws: another clinical variant? J Oral Maxillofac Surg 2008; 66: 1516–7. doi: 10.1016/j.joms.2008.02.012 [DOI] [PubMed] [Google Scholar]
- 20.Diniz-Freitas M, López-Cedrún JL, Fernández-Sanromán J, García-García A, Fernández-Feijoo J, Diz-Dios P. Oral bisphosphonate-related osteonecrosis of the jaws: clinical characteristics of a series of 20 cases in Spain. Med Oral Patol Oral Cir Bucal 2012; 17: e751–e758. doi: 10.4317/medoral.18041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lazarovici TS, Yahalom R, Taicher S, Elad S, Hardan I, Yarom N. Bisphosphonate-related osteonecrosis of the jaws: a single-center study of 101 patients. J Oral Maxillofac Surg 2009; 67: 850–5. doi: 10.1016/j.joms.2008.11.015 [DOI] [PubMed] [Google Scholar]
- 22.Mawardi H, Treister N, Richardson P, Anderson K, Munshi N, Faiella RA, et al. Sinus tracts-an early sign of bisphosphonate-associated osteonecrosis of the jaws? J Oral Maxillofac Surg 2009; 67: 593–601. doi: 10.1016/j.joms.2008.09.031 [DOI] [PubMed] [Google Scholar]
- 23.Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, et al. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res 2015; 30: 3–23. doi: 10.1002/jbmr.2405 [DOI] [PubMed] [Google Scholar]
- 24.Fedele S, Porter SR, D'Aiuto F, Aljohani S, Vescovi P, Manfredi M, et al. Nonexposed variant of bisphosphonate-associated osteonecrosis of the jaw: a case series. Am J Med 2010; 123: 1060–4. doi: 10.1016/j.amjmed.2010.04.033 [DOI] [PubMed] [Google Scholar]
- 25.Fleisher KE, Doty S, Kottal S, Phelan J, Norman RG, Glickman RS. Tetracycline-guided debridement and cone beam computed tomography for the treatment of bisphosphonate-related osteonecrosis of the jaw: a technical note. J Oral Maxillofac Surg 2008; 66: 2646–53. doi: 10.1016/j.joms.2008.07.021 [DOI] [PubMed] [Google Scholar]
- 26.Singer SR, Mupparapu M. Plain film and CBCT findings in a case of bisphosphonate-related osteonecrosis of the jaw. Quintessence Int 2009; 40: 163–5. [PubMed] [Google Scholar]
- 27.Treister NS, Friedland B, Woo SB. Use of cone-beam computerized tomography for evaluation of bisphosphonate-associated osteonecrosis of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 753–64. doi: 10.1016/j.tripleo.2009.12.005 [DOI] [PubMed] [Google Scholar]
- 28.Barragan-Adjemian C, Lausten L, Ang DB, Johnson M, Katz J, Bonewald LF. Bisphosphonate-related osteonecrosis of the jaw: model and diagnosis with cone beam computerized tomography. Cells Tissues Organs 2009; 189: 284–8. doi: 10.1159/000151451 [DOI] [PubMed] [Google Scholar]
- 29.Olutayo J, Agbaje JO, Jacobs R, Verhaeghe V, Velde FV, Vinckier F. Bisphosphonate-related osteonecrosis of the jaw bone: radiological pattern and the potential role of CBCT in early diagnosis. J Oral Maxillofac Res 2010; 1: e3. doi: 10.5037/jomr.2010.1203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guggenberger R, Koral E, Zemann W, Jacobsen C, Andreisek G, Metzler P. Cone beam computed tomography for diagnosis of bisphosphonate-related osteonecrosis of the jaw: evaluation of quantitative and qualitative image parameters. Skeletal Radiol 2014; 43: 1669–78. doi: 10.1007/s00256-014-1951-1 [DOI] [PubMed] [Google Scholar]
- 31.Wilde F, Heufelder M, Lorenz K, Liese S, Liese J, Helmrich J, et al. Prevalence of cone beam computed tomography imaging findings according to the clinical stage of bisphosphonate-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114: 804–11. doi: 10.1016/j.oooo.2012.08.458 [DOI] [PubMed] [Google Scholar]
- 32.Torres SR, Chen CS, Leroux BG, Lee PP, Hollender LG, Santos EC, et al. Mandibular cortical bone evaluation on cone beam computed tomography images of patients with bisphosphonate-related osteonecrosis of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 695–703. doi: 10.1016/j.oooo.2011.11.011 [DOI] [PubMed] [Google Scholar]
- 33.Fusco V, Galassi C, Berruti A, Ciuffreda L, Ortega C, Ciccone G, et al. Osteonecrosis of the jaw after zoledronic acid and denosumab treatment. J Clin Oncol 2011; 29: e521–e522. doi: 10.1200/JCO.2011.35.1551 [DOI] [PubMed] [Google Scholar]
- 34.O'Ryan FS, Khoury S, Liao W, Han MM, Hui RL, Baer D, et al. Intravenous bisphosphonate-related osteonecrosis of the jaw: bone scintigraphy as an early indicator. J Oral Maxillofac Surg 2009; 67: 1363–72. doi: 10.1016/j.joms.2009.03.005 [DOI] [PubMed] [Google Scholar]
- 35.Boeddinghaus R, Whyte A. Current concepts in maxillofacial imaging. Eur J Radiol 2008; 66: 396–418. doi: 10.1016/j.ejrad.2007.11.019 [DOI] [PubMed] [Google Scholar]
- 36.Suomalainen A, Pakbaznejad Esmaeili E, Robinson S. Dentomaxillofacial imaging with panoramic views and cone beam CT. Insights Imaging 2015; 6: 1–16. doi: 10.1007/s13244-014-0379-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making 1991; 11: 88–94. doi: 10.1177/0272989X9101100203 [DOI] [PubMed] [Google Scholar]
- 38.Taguchi A, Akiyama H, Koseki T, Shimizutani K. Recognition of bisphosphonate-related osteonecrosis of the jaw among oral and maxillofacial radiologists: results from a questionnaire-based survey in Japan. Oral Radiol 2013; 29: 98–104. doi: 10.1007/s11282-012-0114-0 [DOI] [Google Scholar]
- 39.Arce K, Assael LA, Weissman JL, Markiewicz MR. Imaging findings in bisphosphonate-related osteonecrosis of jaws. J Oral Maxillofac Surg 2009; 67(5 Suppl): 75–84. doi: 10.1016/j.joms.2008.12.002 [DOI] [PubMed] [Google Scholar]
- 40.Bianchi SD, Scoletta M, Cassione FB, Migliaretti G, Mozzati M. Computerized tomographic findings in bisphosphonate-associated osteonecrosis of the jaw in patients with cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104: 249–58. doi: 10.1016/j.tripleo.2007.01.040 [DOI] [PubMed] [Google Scholar]
- 41.Aghaloo TL, Dry SM, Mallya S, Tetradis S. Stage 0 osteonecrosis of the jaw in a patient on denosumab. J Oral Maxillofac Surg 2014; 72: 702–16. doi: 10.1016/j.joms.2013.09.008 [DOI] [PMC free article] [PubMed] [Google Scholar]