Abstract
The rapid progression of medical imaging technology and the ability to leverage knowledge from non-invasive imaging means that Interventional Radiologists (IRs) and Interventional Neuroradiologists are optimally placed to incorporate minimally invasive interventional paradigms into clinical management to advance patient care. There is ample opportunity to radically change the management options for patients with a variety of diseases through the use of minimally invasive interventional procedures. However, this will need to be accompanied by an increased clinical role of IRs to become active partners in the clinical management of patients. Unfortunately, the development of IR clinical presence has lagged behind and is reflected by declining rates of IR involvement in certain areas of practice such as vascular interventions. Current and future IRs must be willing to take on clinical responsibilities; reviewing patients in clinic to determine suitability for a procedure and potential contraindications, rounding on hospital inpatients and be willing to manage procedure related complications, which are all important parts of a successful IR practice. Increasing our clinical presence has several advantages over the procedure-driven model including enhanced patient knowledge and informed consent for IR procedures, improved rapport with patients and other clinical colleagues through active participation and engagement in patient care, visibility as a means to facilitate referrals and consistency of follow-up with opportunities for further learning. Many of the solutions to these problems are already in progress and the use of IR as a “hired gun” or “technician” is a concept that should be relegated to the past, and replaced with recognition of IRs as clinicians and partners in delivering modern high quality multidisciplinary team-based patient care. The following article will review the history of IR, the challenges facing this rapidly evolving profession and discuss recent developments occurring globally that are essential in maintaining expertise, securing future growth and improving patient outcomes in the modern multidisciplinary practice of medicine.
Introduction
In 1964, Charles T Dotter performed the first minimally invasive treatment of an 82-year-old female patient with critical limb ischaemia of her left foot owing to peripheral vascular disease.1 Almost 10 years earlier in 1955, Goodwin et al2 published the first description of percutaneous nephrostomy. The term “interventional radiology” (IR) was subsequently coined by Alexander Margulis in 1967 and a new subspecialty was born. Since that time, we have seen an explosion of minimally invasive image-guided procedures and a paradigm shift in the treatment of many medical and surgical diseases from simple vascular interventions to biliary drainage in the late 1970s and percutaneous biopsy in the late 1970s and early 1980s followed by complex vascular interventions, new transcatheter embolization procedures and the new IR discipline of interventional oncology (IO).3 Interventional Radiologists (IRs) have been at the forefront of this minimally invasive approach to many diseases—developing and implementing new technologies through collaboration and partnership both within our specialty and with our medical and surgical colleagues.
As many medical and surgical specialities rapidly progress, the field of IR has similarly progressed in its ability to provide care to increasingly complex patients. The rapid progression of medical imaging technology and the ability to leverage knowledge from non-invasive imaging means that IRs are optimally placed to incorporate advanced imaging and minimally invasive interventional paradigms (both vascular and non-vascular) into clinical management of patients.
Contemporary IRs must be willing to work in a clinical capacity in order to maintain and improve the current standard of patient care. In 1968, Charles T Dotter, the father of IR, cautioned “If my fellow angiographers prove unwilling or unable to accept or secure for their patients the clinical responsibilities attendant on transluminal angioplasty, they will become high-priced plumbers facing forfeiture of territorial rights based solely on imaging equipment others can obtain and skills others can learn”.1 Similarly, almost 50 years later, Werner A Golder MD, poignantly points out that “hybrid operating” room and its associated C-arm fluoroscopy, digital subtraction angiography and interventional CT and intraoperative MRI machines now allow many specialists to manage both clinical responsibilities and perform IR procedures.4 As a consequence, in the USA and Europe, many IR practices have become increasingly clinically focused—IRs review patients in outpatient clinics, perform ward rounds and manage patients admitted under them. Similar trends are also seen in IR practice in Australia. This approach is becoming increasingly relevant with studies showing demand for both vascular and non-vascular IR services outpacing growth in new hospital patients over a two-decade period.3
The following article will review the history of IR, the challenges facing this rapidly evolving profession and discuss recent developments occurring globally that are essential in maintaining expertise and securing future growth in the modern multidisciplinary practice of medicine through ongoing collaboration and innovation.
Historical overview and recent developments
The history of IR has been that of a collaborative approach between multiple specialities with modern practice shaped through the innovative approaches taken by many IRs, surgeons and physicians. By understanding our history, we can continue to make advances collaboratively to the betterment of our patients.
Sven-Ivar Seldinger, a Swedish radiologist first described the percutaneous approach to opacify and visualize peripheral arteries in 1953. Prior to this, peripheral arteriography required a surgical "cut-down" onto a vessel. The technique, termed the "Seldinger technique", changed the landscape of peripheral angiography and still forms the bedrock of percutaneous vascular and non-vascular access to this day.5
Charles T Dotter (Figure 1) advanced a step further, utilizing the Seldinger technique and pioneering the minimally invasive treatment of peripheral vascular disease through percutaneous angioplasty with telescoping dilators which was successfully used for the first endovascular treatment of critical limb ischaemia in 1964.1 Subsequent innovations by surgical colleagues in the treatment of peripheral vascular disease saw the development of the first embolectomy catheter by Dr Thomas J Fogarty, a vascular surgeon. It was not long before endovascular surgery became the mainstay of therapy for many patients with peripheral vascular disease, with the vascular surgeon Juan C Parodi performing the first minimally invasive aortic aneurysm surgery in Argentina in 1990.6 Many IRs still play an important role in the treatment of peripheral vascular and aortic disease to this day.7
Figure 1.
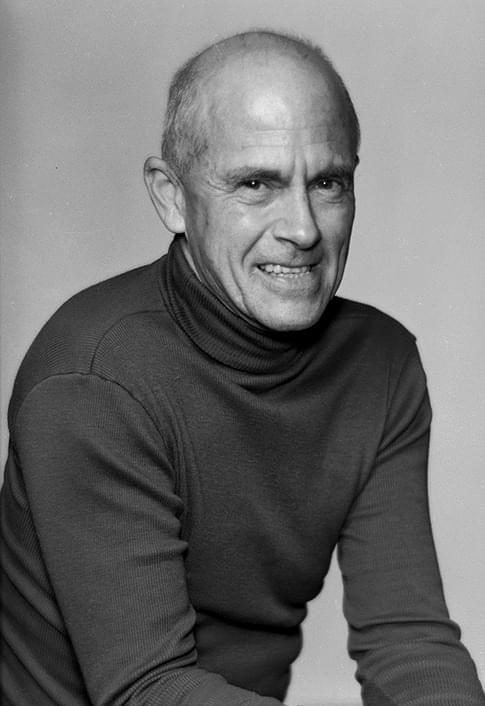
Charles T Dotter MD, the father of interventional radiology. For his work and achievements he received a nomination for the Nobel Prize in Physiology and Medicine in 1978 (image courtesy of Dotter Interventional Institute Archives).
Interventional cardiology finds its roots in the work of radiologist Melvin P Judkins who pioneered coronary angiography and the physician-scientist Andreas Gruentzig (Figure 2) who performed the first coronary artery balloon angioplasty in 1978.1,8 The Judkins catheters are still in routine clinical use in many cardiac catheterization laboratories today.
Figure 2.
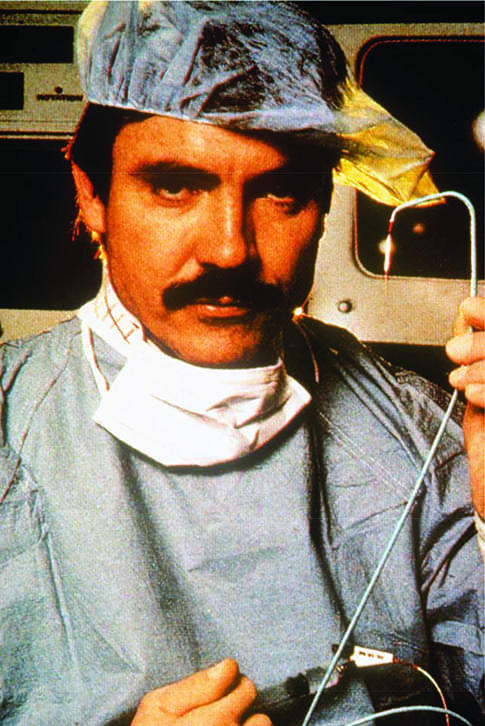
Andreas Gruentzig, a German physician-scientist, pioneered and performed the first coronary balloon angioplasty in 1977 for which he received a nomination for the Nobel Prize in Physiology or Medicine in 1978 (image courtesy of Emory University, Atlanta, GA).
While the first endovascular treatment of an intracranial aneurysm was performed in 1939, it wasn’t until the mid-1970’s that Gerard Debrun, the father of interventional neuroradiology, developed a detachable latex balloon catheter for the treatment of carotid-cavernous fistulae and giant intracavernous aneurysms.9 This was quickly followed by a report of 300 patients treated via an endovascular approach by Serbinenko using a modified version of Debruns catheter.10
By 1990, the invention of the Guglielmi detachable coils by Guido Guglielmi, an Italian Neurosurgeon, was set to change intracranial aneurysm treatment.10 The International Subarachnoid Aneurysm Trial in 2005 compared endovascular with open surgical treatment of ruptured intracranial aneurysms and showed that endovascular coiling resulted in better independent survival at 1 year, with absolute risk reduction of 7.4% [95% CI (3.6–11.2), p = 0.0001]. This treatment effect persevered for at least 7 years.11 Furthermore, recently published trials investigating the endovascular treatment of acute ischaemic stroke have revolutionized the treatment of a previously debilitating disease.12–17 Interventional neuroradiology or endovascular neurosurgery is now able to increasingly provide complex neurovascular interventions improving morbidity, mortality and quality of life across a range of neurovascular diseases, enhancing the lives of many patients.
Similarly, non-vascular IR has evolved through a series of technical innovations since the mid-1950s. Percutaneous nephrostomy was first described in 1955 by Goodwin et al.2 Biliary drainage techniques, percutaneous biopsy and abscess drainage followed some time later in the late 1970s and early 1980s.3
With the advent of ultrasound and CT the ability to perform non-vascular interventions increased with more complex drainages, biopsies and non-vascular stenting performed on an increasing number of patients.3
More contemporary IR procedures include percutaneous thermal ablation of tumours (such as renal cell and hepatocellular carcinomas), an important alterative or adjunct to endovascular approaches. Beyond visceral disease, percutaneous ablation is now commonly used for osseous lesions such as osteoid osteoma18 or even in the palliation of symptoms or local control of metastatic disease.19 Recently the description of real-time MRI guided percutaneous sclerotherapy for low-flow venous and lymphatic malformations of the head and neck has increased the armamentarium available to the practicing IR.20,21
Through a series of technical innovations, the history of our speciality tells us that IRs, through a continued partnership with other specialties, have continued to greatly enhance the care of patients. Through an understanding of our past we must continue to grasp opportunities into the future.
Emerging Challenges
We believe that there remains enormous opportunity for the specialty of IR. However, as IR techniques and procedures come of age and gain widespread acceptance, it is becoming increasingly clear that with more complex treatments in patients with often, multiple comorbidities a more extensive clinical workup and engagement in clinical practice is required.
Unfortunately, the need for an increased clinical presence by IR has lagged behind the development of techniques and devices and is reflected by declining rates of IR involvement in some areas of practice such as peripheral vascular interventions. Between 1997 and 2002 procedure volume in percutaneous peripheral arterial interventions grew more rapidly among cardiologists, vascular surgeons and other physicians compared with radiologists with a reduction in share of this market during the studied interval.22 Furthermore, increasingly, particularly in the USA, vascular surgeons and cardiologists are publishing research into peripheral vascular disease intervention.7
Murphy and Soares (2005)23 summarized this problem and accredited the loss of many procedures pioneered by IR to other specialities to three factors, namely early poor reimbursement for procedures, lack of an adequate patient referral base and time allocated to the practice of IR in many departments where the focus is predominantly diagnostic service delivery.23 While this forms part of the problem, additional barriers exist. Difficulties in making referrals to IRs and a reliance on other specialists to specifically request a clinical procedure, lack of enthusiasm in managing complications or in patient follow-up, lack of admitting rights and lack of ward staff and administrative roadblocks to IR, discourage clinicians from referring their patients and even in some cases may encourage non-IRs to provide alternative services or perform image-guided procedures themselves.
78% of respondents in a 2008 Australian survey of radiology trainees demonstrated very strong support for striving to protect the practice of IR with 40% offering solutions including having a standard of excellence, credentialing, increasing audit and research, mortality and morbidity meetings, providing appropriate and timely interventions, encouraging IR training from an early stage and taking on more patient responsibilities.24
In response, and to meet the increasing demand for more complex care, IRs must adapt to the changing landscape of medicine and minimally invasive procedures to become clinicians. The aim should be to demonstrate to our patients that IRs also provide excellence in patient care like many other procedural specialities.
The Clinical Interventional Radiologist and Subspecialty Recognition
As far back as 1985, the need for increasing clinical presence was already finding its way into the literature. Kinnison et al25 described their admitting IR service and outpatient clinic over a 1-year period between 1982 and 1983. They authors concluded several advantages of assuming direct responsibility for clinical care including a broader patient referral base, improved rapport with clinical colleagues and patients, improved follow-up data, rapid evaluation and treatment and shorter hospital stays. Additionally, there was “an increased sense of camaraderie” when routine and less convenient aspects of patient care were shared.25
Despite these early publications, in a survey of Canadian IRs in 2006, 73% of respondents revealed that they still believed IRs should become more clinical but only 11% had a dedicated IR ward. 44% cited lack of time, 40% lack of hospital or administrative support and 14% inadequate remuneration behind the lack of admitting privileges.26
The need for “longitudinal clinical care of patients” is outlined in the “American College of Radiology: Clinical Practice of Interventional Radiology and Neurointerventional Radiology White Paper 2003” with many American IRs now already leading the way as clinicians, having taken on clinical duties over many years.27
In Europe too, the need for clinical integration is well known. A survey, in 2009, of IR clinical practice in 274 radiology departments throughout Europe revealed that while few institutions had inpatient hospital beds (17%), IR admitting rights were in place across many institutions (64% overall, 86% for inpatients and 89% elective outpatients) although few reported dedicated IR inpatient beds (17%). Only 26% had dedicated IR outpatient clinics.28 More recently, the “Interventional Radiologist as Clinical Specialist” has been outlined in the Cardiovascular and Interventional Radiology Society of Europe’s (CIRSE) recommendations for “The Provision of Interventional Radiology Services in Europe”.29 Therefore, IRs should be encouraged to change their practice model to incorporate the clinical care of patients before, during and after a procedure. There must be an improved emphasis on patient care, management of patients, setting up of clinic and office facilities, increasing the visibility and recognition of IRs and working to establish IR as a well-defined independent clinical specialty providing complementary value to diagnostic radiology. Clinical practice must include reviewing patients in the outpatient clinical setting to determine suitability for a procedure, discussing benefits, risk, alternatives and potential contraindications, taking informed consent, rounding on hospital inpatients and being willing to manage procedure related complications are all important parts of a successful interventional radiology practice.30,31 As outlined by Soares,32 that while the “shift to the clinical IR model is costly”, there is tangible financial value and many intangible benefits including improved patient care, political benefit and the potential for increased job satisfaction, which offset this initial investment.
In concert with an increase in clinical consulting responsibilities, it is important to recognize that certain patient groups would be best served if admitted primarily under the treating IR physician as an equal partner in the delivery of healthcare. The American College of Radiology/Society of Interventional Radiology/Society of Neurointerventional Surgery Practice Guidelines for Interventional Clinical Practice describes guidelines for the admission of patients, highlighting that IR and Interventional Neuroradiologists (INRs) should be “willing and able to take the lead responsibility while the patient is in the hospital”. Provided examples of appropriate direct IR admissions include:
Painful procedures which may require inpatient analgesia (e.g. uterine artery embolization).
Procedures requiring prolonged monitoring or with greater than minimal risk (e.g. neurovascular procedures).
For unexpected procedural complications.
Other considerations such as advanced age or increased distance between the patients primary residence and the treating facility33.
The guidelines suggest working in conjunction with local hospital-based physicians where available. Additional patient types include those admitted strictly for diagnostic tests or urgent referrals from outpatient offices for interventional services.34
Furthermore, increasing our clinical presence allows patients to ask questions of the doctor performing the procedure and not a surrogate who may know little about the nuances of the particular procedure. Many of the solutions to these problems are already in play and the IR as a “hired gun” is a concept that should be relegated to the past.35
Clinics
Increasingly, it will be necessary to determine suitability of elective outpatients for radiological-guided treatments in a clinic-based setting. Patients not only need to understand the goals of the proposed interventional procedure but also should be appropriately counselled regarding risks, benefits and alternatives. This can be clearly highlighted in many clinical scenarios: (1) the treatment of patients with complications of chronic liver disease including hepatocellular carcinoma where clinical and biochemical indicators often guide and determine suitability for image-guided treatment such as percutaneous radiofrequency ablation, transarterial chemoembolization or selective internal radiation therapy (2) prostate artery embolization (PAE) in the treatment of benign prostatic hypertrophy and the need for and comprehensive review of lower urinary tract symptoms, urodynamic parameters, symptom and quality of life scoring (3) uterine artery embolization for the treatment of symptomatic uterine fibroids where a sensitive discussion surrounding symptoms, treatment options and potential treatment side effects (e.g. post-embolization pain) is of utmost importance and (4) endovascular treatment of intracranial aneurysms requiring comprehensive review including presenting symptoms, cerebrovascular risk factors and evaluation for pre-existing neurological deficit and the ability to discuss aneurysm rupture risk, potential treatment approaches, procedural risks and need for long-term follow-up to assess for aneurysm recurrence.36,37 Furthermore, the importance of diagnostic radiology knowledge in procedure work-up cannot be understated. As an example, PAE requires an understanding of computed tomography angiography (CTA), maximum intensity projections and dynamic CTA in order to safely prepare the patient for an uncomplicated procedure.
The IR clinic is also an important platform to prepare patients for a procedure through screening for relevant medical comorbidities and medications which may impact on a proposed procedure. This may include antiplatelet or anticoagulation regimens which may need to be withheld or appropriate correction of haematological or biochemical parameters such as platelet transfusions, e.g. in the setting of leukaemia prior to port or tunnelled catheter insertion. Patients with impaired renal function undergoing angiography will also benefit from alternative contrast agents such as carbon dioxide to avoid contrast-induced nephropathy.
Many hurdles exist, including physical space for clinics, appropriately trained support staff, appointment scheduling and departmental support and the ability to appropriate market and promote services and receive direct patient referrals.31 Patient satisfaction is progressively becoming a driving force in an increasingly consumer driven healthcare system in Australia, Europe and the USA with studies demonstrating improved patient perceptions regarding the quality of their care when attending an IR clinic.38 There has been progress, with IR/INRs already consulting in outpatient clinics in many hospitals.28
Ward rounds
In 1991, Goldberg et al39 highlighted the importance of daily rounds on patients with indwelling catheters in the chest and abdomen over a 7-week period. A problem was identified in 21% of patient reviews with up to 59% having at least one catheter related problem during their stay with 29% necessitating additional imaging or intervention by the radiologist. Many of these problems were detected through direct IR involvement on the ward.
More recently, a 2015 study by Bui et al investigated the utility of daily IR ward rounds in a tertiary centre in Australia, reviewing a total of 473 patients undergoing a variety of vascular and non-vascular procedures over a 1-year period (including 141 percutaneous drains, 138 angiographic procedures, 98 percutaneous biopsies, 26 joint injections, 33 lumbar punctures, 19 central line insertions and 15 ureteric stents). They concluded that routine post procedure ward rounds have a useful role in detecting early post-procedure complications, allows for constructive feedback from patients and identifying areas for improvement for IR.40
The IR ward-round is a simple approach to future proofing the speciality. Ward rounds form the bedrock of all medical and surgical specialties allowing a review of an inpatients clinical status through history and examination pre- and post-procedure, also allowing an opportunity for teaching IR fellows and colleagues and enhancing rapport between the treating IR and the patient.
Ward et al30 outline several important advantages from the clinical IR ward round including.
The ability to have a postprocedural discussion, in detail, when the patient has fully recovered.
Post procedural communication allows patient grievances to be heard, “taking the edge of a difficult procedure”.
The early recognition or problems such as catheter repositioning or upsizing and the opportunity for earlier intervention if needed.
Elevation of status of the IR from technician to valued consultant and member of the patient care team30.
As IR increasingly transforms into a clinical speciality, the time-tested ward-round will become increasingly more relevant. Additionally, maintaining a presence on the ward and adequately engaging with patients prior to their procedure will help demystify their forthcoming image-guided procedure and potentially help to allay patient anxiety and facilitate compliance before, during and after the procedure.41 In some departments, trained specialist nurses, known as clinical nurse specialists (UK and Australia), nurse practitioners (NPs) or physician assistants (PAs) in North America are being trained to assist the IR practitioner in providing continuity of clinical presence on the wards.
Enhanced interactions with fellow clinicians on the ward with the potential for “hallway consults”, will also allow for enhanced communication between radiology and traditional “clinical” specialities with opportunities for learning and feedback. Furthermore, a strong clinical presence and public profile for IR allows primary care physicians and specialists a chance to refer patients to an IR clinic to discuss individual treatment options for individual patients, particularly if they are uncomfortable or unaware of the benefits of a particular IR procedure.
The natural progression of an increasing clinical presence is the integration of the IR as an integral part of a multidisciplinary team. Recent studies investigating the initiation of pulmonary embolism response teams highlights the optimization of risk stratification and expedited management strategies in improving patient outcomes.42–44 These teams include subspecialists from cardiology, pulmonology, hematology, interventional radiology and cardiac surgery. A recent meta-analysis including 30 studies examined the effectiveness of these "rapid response teams". There was a demonstrable significant decrease in hospital mortality [relative risk (RR) = 0.88, 95% CI (0.83–0.93)] and a significant decrease in the number of non-ICU cardiac arrests [relative risk = 0.62, 95% CI (0.55–0.69)]. Similar multidisciplinary approaches have been established in the areas of endovascular stroke and aneurysm management.11–17
Teaching and education
Raising awareness of IR as a subspeciality and the minimally invasive procedures offered among medical students, junior and senior medical and surgical staff and general practitioners will not only improve the quality of referrals received but also will enhance the specialty as a potential career path.
A study in 2014 demonstrated that after an educational lecture series outlining IR procedures and clinical involvement of the interventional radiologist, the understanding of the specialty markedly improved with the number of students who would consider a career in IR increasing from 60 to 73%.45
Additionally, active involvement of radiology trainees, IR fellows and IRs in the teaching of junior and other medical staff not only enhances rapport and allows an avenue for mentoring, but also enhances the perceived expertise of the IR among junior staff.
CIRSE has published an IR curriculum for the teaching of medical students, a curriculum that may be of benefit if introduced into early medical student and junior resident teaching. The focus of the curriculum is on common acute clinical problems, and their identification, as well as the role of IR and covers areas such as vascular and non-vascular IR, interventional oncology and musculoskeletal intervention.46
More importantly, studies investigating the impact of active participation in IR clinical practice through student electives and dedicated internship rotations have demonstrated an increase in the visibility of IR as a specialty, improved perceptions of changes in training pathways and increased interest in IR as a potential career pathway.47,48 Specifically, a study assessing a 10 week IR elective demonstrated improved perceptions regarding patient interaction, percentage of procedural work and safety from radiation exposure, although the results were non-significant.47 A survey of 353 practicing IRs and US medical students regarding a dedicated IR clinical clerkship showed that the majority felt that taking call with the attending IR (60.1%), access to a simulation centre (81%) and a properly structured IR rotation (82% IR, 71% medical students) would be a “critical tool in creating and cultivating medical student interest in IR”.48
Radiology trainees in early years of training could be increasingly encouraged and educated to perform "core" IR procedures such as biopsies, drainages and vascular access including tunnelled or totally implantable venous access devices. This not only increases the capacity for radiology departments to provide this service but also allows trainees to hone interventional skills and encourages interest in IR. For those not interested in a dedicated IR career, this at least enhances their understanding of correct vascular access device placement and potential complications when interpreting diagnostic images.
Research
Active engagement and collaboration in medical research both between IRs and with other medical and surgical specialists has many advantages. It demonstrates to our colleagues that IRs are experts in their domain, and across many fields; and can add value to the management of patients. Additionally, involvement and collaboration in cutting edge research means IRs can contribute to novel interventions improving the care of patients with many different conditions.
Recently, INRs have been among the principal investigators for trials in stroke, investigating and validating the endovascular treatment for acute ischaemic stroke; IRs have also led trials demonstrating the efficacy of percutaneous vertebroplasty for the treatment of acute painful osteoporotic crush fractures.12,16
While IR has been involved with endovascular intervention for over half a century, increasingly more non-IR specialists now work within the field. Despite this, studies show that research and publications in endovascular intervention for peripheral arterial disease continues to be produced by IR particularly in Europe. Furthermore, IR continues as a leader in new territories and frontiers, as an example, in the field of below knee intervention, pedal intervention and drug-eluting technologies. This reflects the skill set and expertise of IR in these newly emerging and challenging interventional approaches to peripheral arterial disease.7 Remaining active in research in peripheral arterial disease and aortic intervention [abdominal endovascular aneurysm repair (EVAR) and Thoracic Endovascular aneurysm Repair (TEVAR)] will also allow IRs to increase their procedural volume as they maintain a presence as experts within these areas.
Furthermore, IRs should also have an understanding and knowledge of journals and research relevant to our medical and surgical colleagues as a means to understanding the evidence base that influences their decision making and where minimally invasive procedures have a role in management.
Accreditation
CIRSE has outlined a series of recommendations to the provision IR services in Europe, which is progressing shoulder to shoulder with the recommendations put together by the European Society for Minimally Invasive Neurological Therapy (ESMINT).29 Furthermore, the European Curriculum and Syllabus for Interventional Radiology, now in its second edition, and the establishment of the European Board of Interventional Radiology (EBIR) and European Diploma in Interventional Neuroradiology (EDiNR) qualifications allow a new generation of IRs and INRs to demonstrate accredited expertise in the field of minimally invasive image-guided procedures “after completing a satisfactory period of IR and INR training following certification in Diagnostic Radiology”.49 This ensures an appropriate standard of care, quality of work and raises the profile of IR and INR. The European Board of Interventional Radiology has been widely adopted as the exam for accrediting IR training in Europe and also recently in Australia and New Zealand. Where direct IR training pathways are available, a dedicated specialist exam or board certification would further help to establish IR/INR in the clinical sphere, emphasizing the dedicated knowledge and expertise required to pursue a strong clinical IR/INR practice.
For INRs in Australia and New Zealand, the Conjoint Committee for Recognition in Interventional Neuroradiology (CCINR) oversees the provision of interventional neuroradiology services. This committee sets a standard of care by certifying individual practitioners to ensure appropriate training and experience to perform minimally invasive treatment of intracranial vascular disease.50 The Australian and New Zealand Society of Neuroradiology, the Neurosurgical Society of Australasia and the Australian and New Zealand Association of Neurologists support this certification.
Subspecialty status
With the continued expansion of IR services globally the need for subspecialty recognition is increasingly being recognized. IR was recognized as a subspecialty in 2009 by the Union of European Medical Specialists. In the US and Canada, subspecialty status has been known for many years.51 In UK, trainees pursuing a 6-year IR training pathway are awarded a certificate of completion of training in clinical radiology with interventional radiology subspecialization. Subspecialty status allows IRs to determine the future of their specialty and streamlines those with a career interest into IR and INR pathways. Moreover, it enhances the ability of IRs to advocate for their specialty at a local hospital level and at a state and national level (e.g. on faculty boards).
Practice guidelines
IRs can and should continue to contribute and develop practice guidelines both nationally and internationally (e.g. through CIRSE or the Society of Interventional Radiology) for minimally invasive procedures. Furthermore, active representation on multidisciplinary guideline panels to advocate for IRs role in treating many diseases has many advantages. As an example, uterine fibroid embolization is now accepted as first-line treatment for many symptomatic fibroids and is outlined in the National Institute for Health and Clinical Excellence, Royal College of Obstetricians and Gynaecologists and Royal College of Obstetricians and Gynaecologists (ACOG) guidelines.52–56 This was achieved through active partnership and IR representation and participation in panels as well as through continued research by IRs driving a methodological sound evidence base to validate these treatments. Similar ongoing collaborative efforts may yield success in the treatment of benign prostatic hyperplasia through PAE and for proximal lower limb deep venous thrombosis through pharmacomechanical thrombectomy.
Enhanced training pathways in interventional and neurointerventional radiology
In many countries across Europe and Australasia, the current training model requires prospective interventional radiologist to undergo 4–5 years of diagnostic radiology training, followed by 2 years of subspecialty fellowship training. This is a model that currently works well and has many advantages for the practicing IR/INR including maintaining adequate diagnostic abilities that are an important part in deciding if minimally invasive treatments are appropriate (e.g. the interpretation of non-contrast CT brain, CT angiography and CT perfusion as selection tools for endovascular clot retrieval). However, alternative models of training such as a direct IR pathway for US radiology residents have been proposed, consisting of 1 clinical year of rotations, 3 years basic diagnostic training and 2 years of IR training with the aim of producing competent IRs.57 For those not matching to the direct IR pathway in the US, the traditional model of 1 clinical year of internship, 4 years of radiology residency and 2 years of IR fellowship remains an option.
Conclusion
As a profession, IRs and INRs must adapt and evolve to ensure our speciality is visible to our patients, other medical and surgical disciplines and allied health professionals and the public. IRs must be able to provide a level of care that meets the expectations of a procedural speciality. The practice of IR/INR worldwide has moved toward pursuit of clinical excellence in addition to technical excellence, increased credentialing, clinical audit and research. IRs and INRs need to adapt to increasingly manage complex patients and treatment approaches, engage and collaborate with other clinicians, engage directly with patients and promote IR/INR services within hospitals and to the public. IRs and INRs are well placed to provide a major contribution to the increasingly minimally invasive and multidisciplinary practice of medicine in the future.
Contributor Information
Julian Maingard, Email: julian.maingard@gmail.com.
Hong Kuan Kok, Email: terrykok@gmail.com.
Dinesh Ranatunga, Email: dinesh.ranatunga@gmail.com.
Duncan Mark Brooks, Email: Mark.Brooks@austin.org.au.
Ronil V. Chandra, Email: ronilc@gmail.com.
Michael J. Lee, Email: mlee@rcsi.ie.
Hamed Asadi, Email: asadi.hamed@gmail.com.
References
- 1.Rösch J, Keller FS, Kaufman JA. The birth, early years, and future of interventional radiology. J Vasc Interv Radiol 2003; 14: 841–53. [DOI] [PubMed] [Google Scholar]
- 2.Goodwin WE, Casey WC, Woolf W. Percutaneous trocar (needle) nephrostomy in hydronephrosis. J Am Med Assoc 1955; 157: 891–4. [DOI] [PubMed] [Google Scholar]
- 3.Hahn PF, Guimaraes AR, Arellano RS, Mueller PR, Gervais DA. Nonvascular interventional procedures in an urban general hospital: analysis of 2001-2010 with comparison to the previous decade. Acad Radiol 2015; 22: 904–8. [DOI] [PubMed] [Google Scholar]
- 4.Golder WA. Radiologists - Threatened by a veritable identity crisis? J Med Imaging Radiat Oncol 2017; 61. [DOI] [PubMed] [Google Scholar]
- 5.Seldinger SI. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol 1953; 39: 368–76. [DOI] [PubMed] [Google Scholar]
- 6.Friedman SG. A History of Vascular Surgery. New Jersey, USA: Wiley; 2008. [Google Scholar]
- 7.Asadi H, Lee RJ, Sheehan M, Thanaratam P, Lee DM, Lee AM, et al. Endovascular therapy research in lower limb peripheral arterial disease published over a 5-year period: who is publishing and where? Cardiovasc Intervent Radiol 2017; 40: 343–50. [DOI] [PubMed] [Google Scholar]
- 8.Barton M, Grüntzig J, Husmann M, Rösch J. Balloon angioplasty - the legacy of Andreas Grüntzig, M.D. (1939-1985). Front Cardiovasc Med 2014; 1: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Debrun G, Lacour P, Caron JP, Hurth M, Comoy J, Keravel Y. Inflatable and released balloon technique experimentation in dog -- application in man. Neuroradiology 1975; 9: 267–71. [DOI] [PubMed] [Google Scholar]
- 10.Guglielmi G. History of endovascular endosaccular occlusion of brain aneurysms: 1965-1990. Interv Neuroradiol 2007; 13: 217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet 2005; 366: 809–17. [DOI] [PubMed] [Google Scholar]
- 12.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–18. [DOI] [PubMed] [Google Scholar]
- 13.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–30. [DOI] [PubMed] [Google Scholar]
- 14.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–306. [DOI] [PubMed] [Google Scholar]
- 15.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–95. [DOI] [PubMed] [Google Scholar]
- 16.Clark W, Bird P, Gonski P, Diamond TH, Smerdely P, McNeil HP, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2016; 388: 1408–16. [DOI] [PubMed] [Google Scholar]
- 17.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–31. [DOI] [PubMed] [Google Scholar]
- 18.Foster RC, Stavas JM. Bone and soft tissue ablation. Semin Intervent Radiol 2014; 31: 167–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Health Quality Ontario. Vertebral augmentation involving vertebroplasty or kyphoplasty for cancer-related vertebral compression fractures: a systematic review. Ont Health Technol Assess Ser 2016; 16: 1–202. [PMC free article] [PubMed] [Google Scholar]
- 20.Partovi S, Vidal L, Lu Z, Nakamoto DA, Buethe J, Clampitt M, et al. Real-time MRI-guided percutaneous sclerotherapy of low-flow head and neck lymphatic malformations in the pediatric population - a stepwise approach. Pediatr Radiol 2017; 47: 755–60. [DOI] [PubMed] [Google Scholar]
- 21.Partovi S, Lu Z, Vidal L, Nakamoto DA, Buethe J, Coffey M, et al. Real-time MRI-guided percutaneous sclerotherapy treatment of venous low-flow malformations in the head and neck. Phlebology 2017; 268355517710110. [DOI] [PubMed] [Google Scholar]
- 22.Levin DC, Rao VM, Parker L, Bonn J, Maitino AJ, Sunshine JH. The changing roles of radiologists, cardiologists, and vascular surgeons in percutaneous peripheral arterial interventions during a recent five-year interval. J Am Coll Radiol 2005; 2: 39–42. [DOI] [PubMed] [Google Scholar]
- 23.Murphy TP, Soares GM. The evolution of interventional radiology. Semin Intervent Radiol 2005; 22: 6–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGuinness B, Holden A. Interventional radiology: a survey of trainees. J Med Imaging Radiat Oncol 2008; 52: 155–60. [DOI] [PubMed] [Google Scholar]
- 25.Kinnison ML, White RI, Jr, Auster M, Hewes R, Mitchell SE, Shuman L, et al. Inpatient admissions for interventional radiology: philosophy of patient management. Radiology 1985; 154: 349–51. [DOI] [PubMed] [Google Scholar]
- 26.Baerlocher MO, Asch MR, Hayeems E, Collingwood P. The clinical interventional radiologist: results of a national survey by the Canadian Interventional Radiology Association. Can Assoc Radiol J 2006; 57: 218–23. [PubMed] [Google Scholar]
- 27.American College of Radiology, American Society of Interventional and Therapeutic Neuroradiology, Society of Interventional Radiology. Practice guideline for interventional clinical practice. J Vasc Interv Radiol 2005; 16(2 Pt 1): 149–55. [DOI] [PubMed] [Google Scholar]
- 28.Keeling AN, Reekers JA, Lee MJ. The clinical practice of interventional radiology: a European perspective. Cardiovasc Intervent Radiol 2009; 32: 406–11. [DOI] [PubMed] [Google Scholar]
- 29.Tsetis D, Uberoi R, Fanelli F, Roberston I, Krokidis M, van Delden O, et al. The Provision of Interventional Radiology Services in Europe: CIRSE Recommendations. Cardiovasc Intervent Radiol 2016; 39: 500–6. [DOI] [PubMed] [Google Scholar]
- 30.Ward MB, Javier C, Jenkins R. The top 10 things I learned on clinical interventional radiology rounds. Semin Intervent Radiol 2006; 23: 366–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siskin GP, Bagla S, Sansivero GE, Mitchell NL. The interventional radiology clinic: what you need to know. Semin Intervent Radiol 2005; 22: 39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soares GM. The value of clinical interventional radiology. J Am Coll Radiol 2011; 8: 318–24. [DOI] [PubMed] [Google Scholar]
- 33.American College of Radiology, Society of Interventional Radiology, Society of Neurointerventional Surgery, Society of Pediatric Radiology. Practice parameter for interventional clinical practice and management. J Vasc Interv Radiol 2015; 26: 1197–204. [DOI] [PubMed] [Google Scholar]
- 34.Mezrich JL. Hospital-admitting privileges in interventional radiology: how IR should reposition itself in the wake of one hospital's policy change. J Vasc Interv Radiol 2013; 24: 1667–9. [DOI] [PubMed] [Google Scholar]
- 35.Baerlocher MO, Asch MR. The future interventional radiologist: clinician or hired gun? J Vasc Interv Radiol 2004; 15: 1385–90. [DOI] [PubMed] [Google Scholar]
- 36.Ward TJ, Madoff DC, Weintraub JL. Interventional radiology in the multidisciplinary management of liver lesions: pre- and postoperative roles. Semin Liver Dis 2013; 33: 213–25. [DOI] [PubMed] [Google Scholar]
- 37.Pisco J, Campos Pinheiro L, Bilhim T, Duarte M, Rio Tinto H, Fernandes L, et al. Prostatic arterial embolization for benign prostatic hyperplasia: short- and intermediate-term results. Radiology 2013; 266: 668–77. [DOI] [PubMed] [Google Scholar]
- 38.Abboud S, Partovi S, Nakamoto D, Azar N. The radiologist will see you now: patients' perceptions of an outpatient interventional clinic. Curr Probl Diagn Radiol 2016; 45: 137–8. [DOI] [PubMed] [Google Scholar]
- 39.Goldberg MA, Mueller PR, Saini S, Lee MJ, Girard MJ, Dawson SL, et al. Importance of daily rounds by the radiologist after interventional procedures of the abdomen and chest. Radiology 1991; 180: 767–70. [DOI] [PubMed] [Google Scholar]
- 40.Bui P, Dodd E, Loh H. The utility of the post-interventional radiology ward round: Experience of a tertiary centre in New South Wales, Australia. J Med Imaging Radiat Oncol 2015; 59: 73–106. [Google Scholar]
- 41.Schupp CJ, Berbaum K, Berbaum M, Lang EV. Pain and anxiety during interventional radiologic procedures: effect of patients' state anxiety at baseline and modulation by nonpharmacologic analgesia adjuncts. J Vasc Interv Radiol 2005; 16: 1585–92. [DOI] [PubMed] [Google Scholar]
- 42.Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. JAMA 2006; 295: 324–7. [DOI] [PubMed] [Google Scholar]
- 43.Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: a systematic review and meta-analysis. J Hosp Med 2016; 11: 438–45. [DOI] [PubMed] [Google Scholar]
- 44.Kabrhel C, Rosovsky R, Channick R, Jaff MR, Weinberg I, Sundt T, et al. A multidisciplinary pulmonary embolism response team: Initial 30-month experience with a novel approach to delivery of care to patients with submassive and massive pulmonary embolism. Chest 2016; 150: 384–93. [DOI] [PubMed] [Google Scholar]
- 45.Shaikh M, Shaygi B, Asadi H, Thanaratnam P, Pennycooke K, Mirza M, et al. The introduction of an undergraduate interventional radiology (IR) curriculum: impact on medical student knowledge and interest in IR. Cardiovasc Intervent Radiol 2016; 39: 514–21. [DOI] [PubMed] [Google Scholar]
- 46.Interventional Radiology Curriculum for Medical Students Cardiovascular and Interventional Radiological Society of EuropeCardiovascular and Interventional Radiological Society of Europe. 2012. Available from: http://www.cirse.org/index.php?pid=828
- 47.Kumar V, Lehrman E, Diaz A, Vinson A, Conrad M, LaBerge J. Early exposure improves medical student perceptions on female and minority physician inclusion in interventional radiology. J Vasc Interv Radiol 2017; 28: S22. [Google Scholar]
- 48.Pillai R, McLennan G, Chung M, Warhadpande S, Kalra-Lall A. The makings of an ideal interventional radiology clinical clerkship: survey results of medical students and interventional radiology educators to improve medical student training in preparation for the IR/DR residency. J Vasc Interv Radiol 2016; 27: S77–S78. [Google Scholar]
- 49.European Curriculum and Syllabus for Interventional Radiology Cardiovascular and Interventional Radiological Society of Europe. 2012. Available from: http://www.cirse.org/index.php?pid=378
- 50.Conjoint Committee Guidelines for Recognition of Training in Interventional Neuroradiology (INR). Conjoint Committee for Recognition of Training in Interventional Neuroradiology. 2014. Available from: http://www.ccinr.org.au/downloads/
- 51.Lee MJ, Belli AM, Brountzos E, Morgan R, Reekers JA. Specialty status for interventional radiology: the time is now. Cardiovasc Intervent Radiol 2014; 37: 862. [DOI] [PubMed] [Google Scholar]
- 52.American College of Obstetricians and Gynecologists ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol 2008; 112(2 Pt 1): 387–400. [DOI] [PubMed] [Google Scholar]
- 53.Uterine artery embolisation for the treatment of uterine fibroids. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists; 2014. Available at: https://www.ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical%20-%20Gynaecology/Uterine-Artery-Embolisation-(C-Gyn-23)-Review-November-2014.pdf?ext=.pdf [Google Scholar]
- 54. Royal College of Obstetricians and Gynaecoloists. 2013. Available at: www.rcog.org.uk/en/guidelines-research-services/guidelines/uterine-artery-embolisation-in-the-management-of-fibroids/
- 55.Interventional procedure overview of uterine artery embolisation for fibroids. National Institute for Health and Clinical Excellence. 2010.
- 56.Uterine artery embolisation for fibroids. National Institute for Health and Care Excellence. 2010.
- 57.Nissim L, Krupinski E. Vascular and IR/Diagnostic and IR Enhanced Clinical Training Pathway: survey of graduates and trainees from this pilot IR training program. J Vasc Interv Radiol 2015; 26: 297–9. [DOI] [PubMed] [Google Scholar]


