Abstract
Objective:
To collect radiology trainees’ views on training for clinic-multidisciplinary team meetings (MDTMs), identify aspects requiring improvement and develop a guide to aid training. This is central to quality assurance and is within the core RCR curriculum.
Methods:
The Junior Radiology Forum National Training Survey 2015 was emailed to 1222 UK trainees. Questions related to role in MDTMs, training, use of the MDTM eportfolio tool and experience of leading meetings.
Results:
611 radiology trainees responded. 22% received teaching in MDTM preparation. 29% of trainees use the eportfolio MDT assessment tool. 76% of trainees who run MDTMs have adequate preparation time. 18% always review cases with a consultant prior to a meeting. 7% of trainees always debrief with a consultant. 9.7% have been asked to lead an MDTM which they did not feel comfortable with. Most trainees think trainees should be running MDTMs post FRCR2B.
Conclusion:
There are currently deficits in teaching and consultant supervision when trainees are learning to participate in MDTMs. Formal teaching sessions and timetabled preparation/debrief time with a consultant should be available. Trainees should not be asked to lead meetings without adequate support. This also ensures a safe MDTM environment for the patient. The eportfolio assessment tool can be used to sign off competence levels before independently leading an MDTM.
Advances in knowledge:
These results suggest shortfalls in the current model for preparing radiology trainees for their central role in clinico-MDT meetings. Using this data, a guide for trainees has been written to address these deficits.
Introduction
The Royal College of Radiologists (RCR) describes the role of a radiologist in a multidisciplinary team (MDT) meeting as to maximize patient benefit through prior review of imaging with appropriate time to form an opinion, to discuss differences in radiology opinion and to record the outcome in a supplementary report. The RCR states that MDT meetings form an essential part of quality assurance.1 As a generalist, the radiologist is in a good position to lead and direct an MDT meeting for the best patient outcome.2
Learning to participate in MDT meetings is part of the core radiology curriculum.3 The RCR makes recommendations for trainee participation. Recommendations include ensuring that trainees have adequate time to review cases prior to the meeting, demonstrate appropriate written and verbal communication skills during meetings, exhibit good presentation skills, work with MDT colleagues, appropriately manage time, participate in decision-making, demonstrate leadership and recognizing when to involve other people.4 The RCR e-portfolio Workplace Based Assessments include an MDT Assessment Tool which is mandatory for speciality trainees (STs) in years 4 and 5. This assesses a trainee's ability to prepare for and present at MDT meetings.
The Junior Radiology Forum (JRF) National Training Survey is sent to all UK radiology trainees and aims to collect trainees’ views on many aspects of their training so that improvements can be made. The survey in 2015 contained questions related to MDT participation. We reviewed the JRF National Training Survey and developed a guide and assessment tool for trainees to allow independent practice in the MDT and clinical meeting setting.
Methods And Materials
The JRF National Training Survey was emailed to 1222 radiology trainees across 38 training programmes in the UK. Data were collected anonymously over a period of 5 weeks in 2015.
The MDT and clinical meeting questions were subsequently analysed to assess responses related to the trainee's role in MDT meetings, the training they received for the meetings, their use of the MDT meeting eportfolio tool and their experience of leading meetings. The questions can be seen in Appendix 1.
Results
611 trainees responded to the survey giving a 50% response rate. 10% were less than full time trainees. All 611 trainees answered all of the MDT questions. The number of responses fell with increasing trainee seniority (Figure 1).
Figure 1.
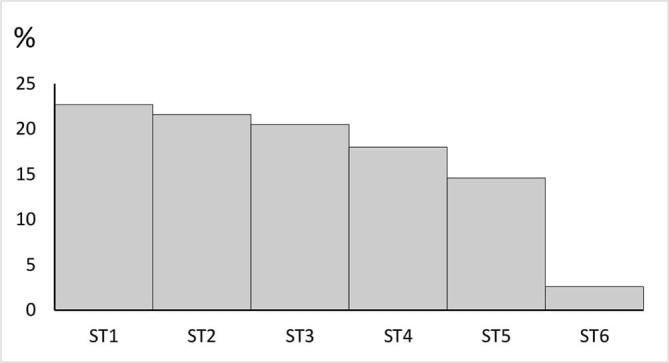
JRF National Training Survey response by ST level. JRF, Junior Radiology Forum; ST, speciality trainee.
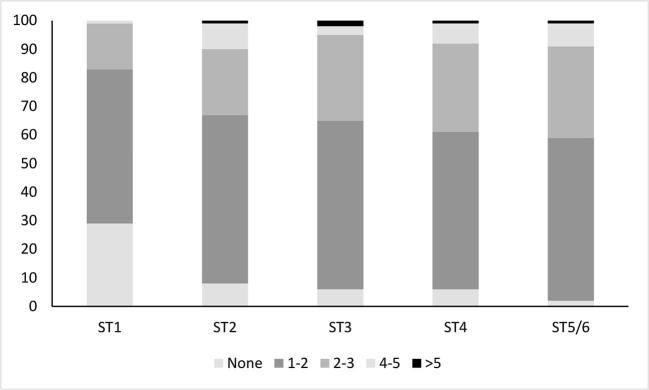
Figure 2 shows the number of MDT meetings attended per week by trainee level. Overall, as seniority increases the number of meetings attended per week increases.
Figure 2.
Number of MDT meetings attended per week by trainee level. MDT, multidisciplinary team; ST, speciality trainee.
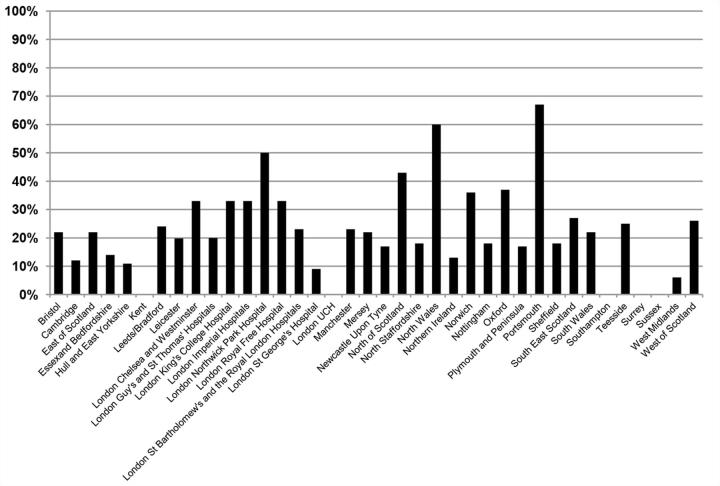
22% of trainees said they have had training on how to prepare for and run a successful MDT meeting. 78% reported that they did not have training. This data were analysed per deanery to assess whether a particular scheme was doing this well (Figure 3). Northwick Park, North Wales and Portsmouth were outliers with better than average teaching for MDT preparation and presentation. On further questioning of local JRF trainee representatives teaching was given informally rather than in timetabled sessions within a training/teaching programme.
Figure 3.
MDT preparation training given by training scheme. MDT, multidisciplinary team.
Trainees were asked to specify the form of training. The majority (50%) stated that their training had been informal consultant training. Only 1% trainees report having a formal tutorial. Other responses including learning by observation and learning from personal experience of running a meeting.
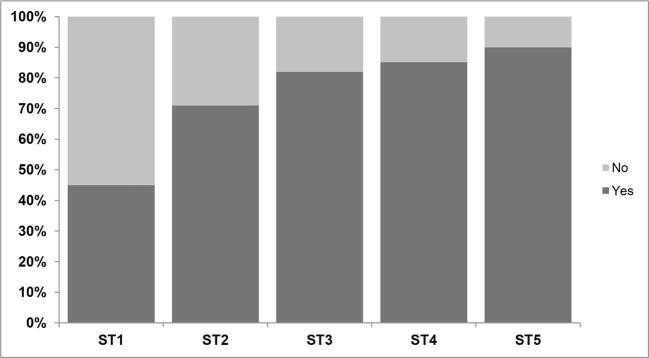
The RCR states that the aim of the eportfolio MDT assessment tool is to “assess a trainee’s ability to contribute effectively to MDT working and to assume a leadership role in multidisciplinary meetings”.4 27% of trainees are not aware of the eportfolio tool. 73% of trainees are aware of this tool and this increases with seniority (Figure 4).
Figure 4.
Awareness of eportfolio assessment tool by ST level. ST, speciality trainee.
29% of all trainees said they had used the eportfolio tool, 71% had not, even though 73% were aware of its existence. Completion of the MDT eportfolio assessment tool is mandatory for satisfactory Annual Review of Competence Progression (ARCP) at ST4 and above. However, only 46% of ST4s and 66% of ST5s had used it.
10% of trainees reported that they had had an introduction to the tool. This was assessed by deanery to identify a successful programme which could be shared nationally but no single region was highlighted.
Of trainees who ran an MDT, 76% felt they had adequate MDT meeting preparation time whereas 24% did not. 99% felt they had time to discuss cases with a consultant prior to the meeting.
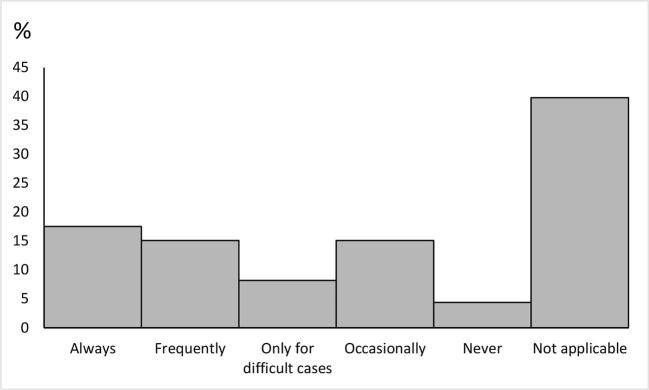
Trainees were asked whether they reviewed cases with a consultant before a meeting (Figure 5). Only 18% said they always review cases with a consultant prior to a meeting. 4% said they never do. This changes with ST level: 29% of ST5s are always able to review cases and 18% of ST5s say they never do. 33% of ST4s are always able to review cases with a consultant prior to a meeting and only 4% of ST4s say they never do. Some trainees responded that the question was not applicable to them. This may include junior trainees who do not yet present cases at an MDT or senior trainees who are independently leading MDTs.
Figure 5.
How regularly do you review cases before a meeting with a consultant?
Trainees were asked whether they debrief with a consultant after a MDT meeting. Only 7% of trainees always debrief with a consultant. 14% of trainees never do this. 12% of ST5s said they always debriefed but 18% of ST5s said they never did. Results are similar for ST4s.
9.7% of trainees said they had been asked to give a meeting that they did not feel comfortable with.
Trainees who answered “Yes” were asked how they dealt with this. Figure 6 shows the responses. Of the trainees who ran the meeting without help, some trainees commented that they were the only person available to run the meeting and some informed the meeting of their inexperience.
Figure 6.
If you have been asked to run a meeting you have not felt comfortable with how did you deal with this?
Trainees were asked at what stage of training they felt trainees should be running an MDT and the results are shown in Figure 7. The highest proportion think that trainees should be running MDTs at ST4 level post FRCR 2b.
Figure 7.
The stage of training when trainees feel they should be running an MDT. MDT, multidisciplinary team; ST, speciality
36.5% of trainees say that an addendum is added to the patient’s report to reflect the meeting outcome. 26.8% say this is not done. 36.7% say they do not know if an addendum is added.
Conclusion and Discussion
The results of the JRF survey highlight some important points which can be used to improve MDT meeting training. The 50% trainee response rate is sufficiently high to allow for significant conclusions to be made.
The majority of trainees do not have teaching on MDT meeting participation and the available teaching is mostly informal. An improvement would be for training schemes to schedule formal group teaching sessions to create a more reliable learning environment which is uniform across training programmes.
Responses reported that preparation time for meetings and discussion of cases with a consultant before and after a meeting is not always adequate. At times trainees are asked to lead meetings when they are not comfortable doing so which is concerning. The majority of consultants have timetabled sessions within their job plan for MDT meeting preparation and should have time to review cases with trainees.5 However, this time can be limited with the current climate of workforce shortage.6 Trainees should have sufficient preparation and feedback or debrief time within their training timetable if they are expected to lead MDT meetings. Consultant feedback is an important tool to facilitate reflection and subsequent improvement of performance, particularly early in training. A lack of feedback could be detrimental to trainee development. Trainees should have access to senior support as needed depending on trainee level. This ensures that queries can be addressed in a timely manner and ensures a safe MDT environment for the patient. More senior trainees may be happy with less structured consultant input and indirect supervision. However, it is important to remember that the consultant is the core member of a cancer MDT meeting.
Most trainees feel that trainees should be running MDT meetings at post Fellowship of the Royal College of Radiologists (FRCR) 2B level. At this stage trainees are developing their confidence in independent cross-sectional imaging reporting and are more able to address clinician’s questions with minimal consultant input. However, if trainees lead meetings without a consultant present it is imperative that they have been signed-off on their eportfolio for the relevant examinations. Ideally, they should be signed-off as independent for that particular MDT meeting using the eportfolio assessment tool.
However, the majority of trainees do not use the eportfolio MDT assessment tool and many trainees are not aware of it. This may be because completion is mandatory for ST4 and above and the majority of respondents are within the lower training levels. However, the completion rate for the MDT assessment tool for ST4 and ST5 was only 46 and 66% respectively, suggesting training schemes are not enforcing the requirement of completion for satisfactory progression at Annual Review of Competence Progression. Participation of more junior trainees could be improved by including a formal introduction and including it in formal JRF MDT meeting guidance. Trainees should be encouraged to obtain formal feedback to aid learning and the eportfolio tool is a means for this.
Over a quarter of trainees report that no addendum is added to reflect the outcome of the MDT discussion. This is useful as a formal record of the outcome and aids in the emergency setting as an easily accessible management plan. A limitation of this question is that outcomes may be documented by other means not captured by the survey. Other limitations are that results vary depending on the trainee grade as experience of these meetings increases. Clinico-MDT meetings include a range of different meetings and these results represent a general overview.
From these points, a guideline for trainees learning to run clinic-MDT meetings has been developed (Appendix 2). Active learning guidance is included for trainees attending and observing clinico-MDT meetings.7 These guidelines aim to reflect differences in learning needs as trainees progress and can be applied to the variable range of clinico-MDT meetings in which radiologists are involved.
Acknowledgments
Acknowledgments
Junior Radiology Forum, Royal College of Radiologists.
Appendix 1: Questions related to MDT and clinical meetings used in the JRF survey
Radiologists and radiology trainees attend many formal multidisciplinary meetings and clinical meetings, e.g. chest meeting, colorectal cancer MDT and also informal meetings, e.g. ITU meeting, care of the elderly meeting. We are keen to know what you think about MDT/clinical meetings.
Q41. How many MDT/clinical meetings do you attend per week? Please specify your role(s). 4-5/2-3/1-2/None/Your role
Q42. Has anyone given you training on how to prepare for and run a successful MDT/clinical meeting? Yes/No
Q43. If yes, please specify
Q44. Are you aware of the RCR MDT/clinical meeting eportfolio assessment tool? Yes/No
Q45. Have you used the RCR MDT/clinical meeting eportfolio assessment tool? This tool can be used by any trainee but it is mandated for those in years 4 and 5. Yes/No
Q46. Did you have an introduction to the eportfolio MDT/clinical meeting assessment tool from anyone in your training scheme? Yes/No
Q47. If you run an MDT or clinical meeting, do you get adequate time to prepare the cases? Yes/No/Not applicable
Q48. If yes, is there time to discuss the cases with a consultant about any queries prior to the meeting? Yes/No
Q49. How regularly do you review the cases before MDT or clinical meeting with a consultant? Always/Frequently/Only for difficult cases/Occasionally/Never/Not applicable
Q50. How regularly do you debrief after MDT or clinical meetings with a consultant? Always/Frequently/Occasionally/Never/Not applicable
Q51. Does a radiologist add an addendum to reports to document the MDT management plan? Yes/No/Don't know
Q52. Have you ever been asked to run an MDT/clinical meeting that you did not feel comfortable doing? Yes/No/Not applicable
Q53. If yes, how have you dealt with this?
Q54. What stage of training do you think trainees should be running an MDT/clinical meeting? Year 5/Year 4 post FRCR 2b/Year 4 pre FRCR 2b/Year 3/Year 1–2
Appendix 2: JRF guideline for trainees learning to run clinico-MDT meetings
Introduction
Learning to participate in clinico-multidisciplinary team (MDT) meetings is part of the core curriculum for radiology trainees.3 The Royal College of Radiologists (RCR) recommends that trainees4:
Have adequate time to review cases and previous imaging prior to the meeting
Demonstrate appropriate written and verbal communication skills during meetings
Exhibit good presentation skills
Work with MDT colleagues
Appropriately manage time
Participate in decision-making with regard to patient management and leadership skills
Recognize when to involve other people
The RCR eportfolio Workplace Based Assessments include an MDT Assessment Tool, which is mandatory for speciality trainees (STs) in years 4 and 5 and assesses a trainee's ability to prepare for and present at MDT meetings.
This guide hopes to help trainees develop the skills required to present radiological findings at MDT meetings. Many of the suggestions are most pertinent to cancer MDT meetings, however the general format can be applied to non-cancer MDT meetings and clinicoradiological meetings.
General Tips
Eportfolio MDT meeting assessment tool
This is mandatory for ST4 and 5 but is a useful tool at any stage to gather formal feedback on performance, identify areas for improvement and evidence engagement with the MDT component of the core curriculum.
Once a trainee feels confident leading an MDT meeting without a consultant present it is imperative that they have been signed off for the particular examinations reviewed in the meeting and ideally signed off as independent for the specific MDT meeting using the eportfolio assessment tool.
The completion guidance is available on the eportfolio system or the RCR website. https://www.rcr.ac.uk/sites/default/files/docs/radiology/pdf/MDT%20Guidance%20for%20Assessors.pdf
Formal teaching sessions for MDT preparation and presentation
Formal teaching sessions should be delivered locally to ensure a good standard of training as MDT preparation and presentation is a core part of the curriculum.
If this is not available within a training programme, trainees are encouraged to ask their programme director if a session can be arranged.
Essential documents to read prior to the MDT meeting
Current staging guidelines.
Criteria used to assess for treatment response.
Local management pathways.
Active learning guidance for trainees attending and observing MDT meetings (ST1-2)
-
The best opportunity for optimizing learning is to attend the radiology consultant's MDT preparation session.
Ask the consultant in advance if they are happy for you to do this. This can be a busy session. It may be that they only have time to go through a few cases with you.
Preparation includes more than reviewing the most recent imaging. Take note of everything else involved. Things to review may include clinical history, previous imaging, blood results and biopsy results.
When reviewing imaging take note of the salient points that the consultant looks for. Some findings change the stage of disease and have important implications for treatment whilst other findings are less relevant. Certain findings are important for the surgeons to know if they will affect the surgical approach.
This is a good time to note management issues such as how to deal with scans needed for the meeting which have not been reported or issues with imported imaging.
If you are not able to sit with the consultant, ask the MDT meeting co-ordinator for a copy of the meeting list so that you can familiarize yourself with the patients and review the imaging by yourself. Make a note of any questions you have to ask at a later time.
-
Maximizing learning during the meeting:
Make sure you have a copy of the patient list.
Ask to sit next to the consultant radiologist if possible so that you can see the high resolution screens and ask questions discretely if appropriate.
Observe the leader of the meeting and reflect on good aspects of leadership that you could use in the future.
Note the radiology consultant's presenting style and what information is given.
Observe the use of PACS and how it can be maximized to aid the meeting. Ensure you are fully aware of useful PACS tools such as bookmarking images and adding labels.
Note the clinical team's questions and the imaging findings which are important to them.
Note any questions you have to ask the consultant afterwards if it is not appropriate to ask during the meeting.
Keep a note of interesting patients and patients who you may want to follow up.
Guidance on how to begin running an MDT meeting (ST3-4)
The supervising consultant should give you details of the MDT co-ordinator so you can be added to the mailing list to receive pre-MDT meeting documentation and outcome details.
When starting to take MDT meetings (ST3) ask to be given a small selection of cases rather than the whole meeting. For example, five new cases and five follow-up cases.
Aim to present these cases to the consultant radiologist prior to the meeting initially before subsequently progressing to presenting at the meeting. Ask to present your cases first when the meeting is likely to be less time pressured.
ST4 trainees should aim to prepare the whole meeting.
A consultant radiologist who is a core MDT member should be present to offer support until the trainee is confident to run an MDT with indirect support (which is expected during ST4-5).
Ensure that your timetable includes time for adequate preparation and debrief with a consultant to facilitate feedback on performance.
Aim to run MDT meetings at post Fellowship of the Royal College of Radiologists (FRCR) 2B level.
Before leading an MDT meeting independently, it is essential that a trainee has been signed off for the particular examinations reviewed in the meeting and ideally signed off as independent for the specific MDT meeting using the eportfolio assessment tool.
How to prepare for the MDT meeting
Check that you have timetabled time for MDT meeting preparation. Ensure that the timing of the preparation time gives time to discuss the cases with your consultant. Time required to prepare for each case will vary depending on your experience and the nature and complexity of the case.
Focus on previous imaging, creating key images and make written notes to review during the meeting.
Note the TNM stage or treatment response for cancer MDT meetings.
-
Remember to note important incidental findings. The “palliative sweep”8 is a useful review tool in cancer imaging used to identify incidental findings which can be treated to improve quality of life. Examples include:
Cord compression.
Tube blockage: bowel, bile duct, ureters, trachea etc.
Complications: therapy induced lung damage and venous or pulmonary thromboembolism.
Presenting in MDT meetings
Arrive 10 min early. Familiarize yourself with the MDT room and projection/image display hardware.
Introduce yourself to the MDT members. Sign the register as a record of your attendance.
Ask that cases are reviewed in the order of the agenda when you start out to reduce the stress of finding your notes and images.
Do not review cases ad hoc in the meeting where you have not had preparation time.
-
Present images in a timely fashion:
Demonstrate communication skills and learn to concisely summarize findings. Use your preparation notes.
Create key images on PACs. Arrows may be helpful.
Coronal reformats aid understanding for non-radiology colleagues.
Show pertinent findings that may influence management.
Actively contribute to decision-making regarding patient management and address the radiological issues.
Learn to lead a team and resolve conflict within a team. The radiologist as a generalist is often in a good position to direct the meeting. Be aware of time keeping and encourage the team to draw conclusions.
Know your limits and when to ask for help
Ensure that senior help is available if necessary during preparation and during the meeting. Indirect supervision may be appropriate for more senior trainees who have been signed off to an appropriate level.
If you are asked to run a meeting on your own and you do not feel comfortable with this, ask for a consultant help. If this is not available, more senior trainees may be in a position to help. If help is not available raise the issue with your clinical or educational supervisor. Patient safety is paramount and is at risk if you feel out of your depth with no help to run a meeting.
At any level of training if you are not sure and there is no direct help available, explain this to the meeting; it may be appropriate to seek advice after the meeting and relay the outcome back to the MDT members.
Documenting MDT outcomes
An addendum or other form of formal documentation should be made to record the discussion and outcome of the meeting. This facilitates easy access to the management plan for future care.
Ask what the local policy is. If there isn’t one, consider introducing one as a quality improvement project.
Contributor Information
Sarah R. Hudson, Email: sarah.hudson10@nhs.net.
David Little, Email: dhlittle@gmail.com.
Anup Mathew, Email: anupvmathew@gmail.com.
Diana Rosof-Williams, Email: americandiana@gmail.com.
Fiona Pathiraja, Email: fionapathiraja@gmail.com.
Kabir Varghese, Email: kabir.varghese1@gmail.com.
James Stephenson, Email: james.stephenson@uhl-tr.nhs.uk.
References
- 1. The Royal College of Radiologists. Cancer multidisciplinary team meetings – standards for clinical radiologists. London: The Royal College of Radiologists; 2014. 1–16. [Google Scholar]
- 2.Eigenmann F. Multidisciplinary team meetings encourage overtreatment. BMJ 2015; 351: h4630. [DOI] [PubMed] [Google Scholar]
- 3. The Royal College of Radiologists. Speciality training curriculum for clinical radiology. London: The Royal College of Radiologists; 2014. 1–187. [Google Scholar]
- 4. The Royal College of Radiologists. Assessment guidance for MDT. London: The Royal College of Radiologists; 2016. 1. [Google Scholar]
- 5. The Royal College of Radiologists. A guide to job planning in clinical radiology: The Royal College of Radiologists; 2013. 1–16. [Google Scholar]
- 6. The Royal College of Radiologists. Clinical radiology UK workforce census 2015 report: The Royal College of Radiologists; 2016. 1–57. [Google Scholar]
- 7. Junior Radiology Forum. Exam Guidance on the Fellowship of the Royal College of Radiologists. London: The Royal College of Radiologists; 2015. 1–16. [Google Scholar]
- 8.Morgan B, Stephenson JA, Griffin Y. Minimising the impact of errors in the interpretation of CT images for surveillance and evaluation of therapy in cancer. Clin Radiol 2016; 71: 1083–94. [DOI] [PubMed] [Google Scholar]