Description
The patient is a 73-year-old woman who was diagnosed with nodular melanoma of the calf almost 2 years prior to presentation. The melanoma was treated with wide-margin surgical resection (pT4b, 21 mitoses/high power field, 8 mm depth), followed by sentinel lymph node biopsy, which was negative. However, surveillance CT scan done less than a year after the original excision showed metastases to the liver, bone, lungs and adrenal glands. After oncological assessment, the patient had decided not to proceed with chemotherapy. The gastroenterology service was consulted when the patient presented with melena and significant anaemia (haemoglobin 54 g/L, haematocrit 0.17 L/L). Her haemoglobin level was normal 1 year prior (128 g/L). She also had mild renal impairment (creatinine 135 μmol/L, urea 11.4 mmol/L, glomerular filtration rate 32 mL/min/1.73 m2). She was resuscitated, including blood transfusions, and underwent urgent gastroscopy.
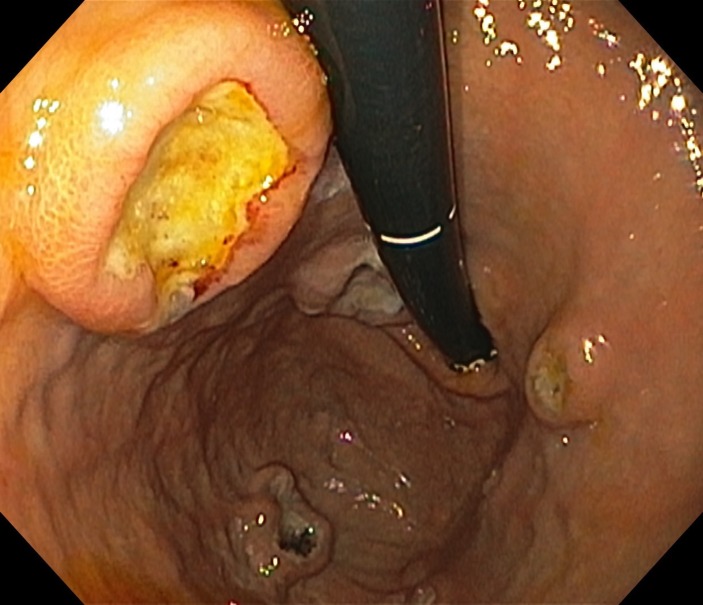
The gastroscopy showed multiple lesions in the fundus and body of the stomach (figure 1). The lesions were nodular with central areas of dark pigmentation and ulceration. One lesion was actively oozing and treated with endoscopic clips followed by application of Hemospray (Cook Medical) for adequate haemostasis. Three days later, repeat upper endoscopy showed resolution of gastric bleeding, and her haemoglobin had increased to 95 g/L.
Figure 1.
Retroflexed view on gastroscopy showing multiple nodular lesions with central areas of dark pigmentation and ulceration. These lesions are located throughout the body and fundus of the stomach.
Biopsies were taken from the non-bleeding lesions. Pathology results were consistent with metastatic melanoma with positive stains for S-100 and melanin-A.
Malignant melanoma is the most common metastatic tumour of the gastrointestinal (GI) tract.1 Metastases are most common to the small intestine, followed by the large intestine, rectum and least commonly to the stomach. Up to 60% of patients with melanoma have evidence of gastric metastases on autopsy; however, the majority are asymptomatic, with only 4.4% diagnosed prior to death.1 2 This patient presented with melena, which is the most common sign of gastric melanoma.3 These lesions are often asymptomatic. Therefore, GI complaints in a patient with known melanoma warrant gastroscopy.2 Endoscopically, melanoma metastases to the stomach are classified into three types: ulcerated melanotic nodules on normal rugae, ulcerated submucosal masses and pigmented mass lesions with necrosis.1 3 Typical endoscopic finding of gastric melanoma is that of multiple nodules located in the gastric fundus and body with ulcerations giving them a ‘bull’s eye’ appearance.3 The ‘bull’s eye’ appearance can be appreciated in the images presented (figure 2). While these lesions are commonly pigmented, this is not a consistent finding. Biopsy of non-bleeding lesions confirms the diagnosis. Acute bleeding can be treated with standard endoscopic haemostatic techniques. Melanoma does not respond well to radiation. Immunotherapeutic agents have shown some promise, and occasionally surgery has been used to control bleeding.2
Figure 2.
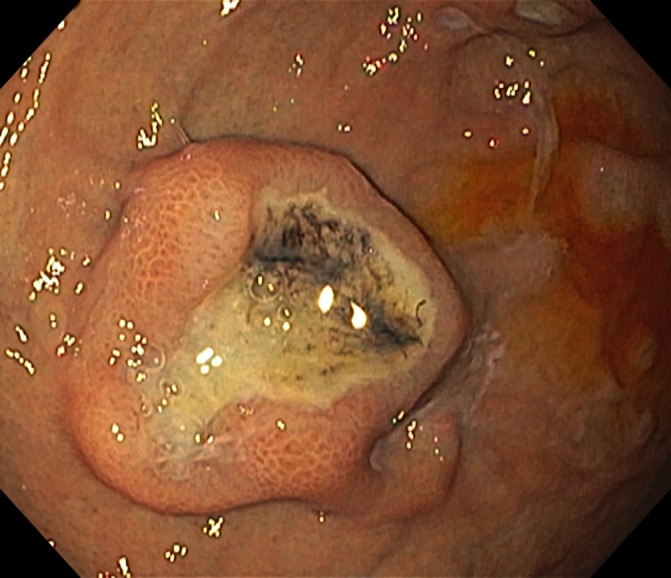
Close-up view of a single lesion showing the pigmented nodular appearance with central ulceration. This is commonly seen in malignant melanoma gastric metastases, sometimes referred to as ‘bull’s eye’.
Learning points.
Malignant melanoma has a predilection for spread to the gastrointestinal (GI) tract.
Despite their high prevalence, melanoma GI lesions are often asymptomatic; patients may present with decreased haemoglobin, occult bleeding or less commonly with a significant upper gastrointestinal bleed (UGIB).
Acute bleeding can be managed by standard endoscopic techniques; immunotherapy should be considered for appropriate patients with malignant melanoma and occult bleeding; and surgery is rarely indicated.
Footnotes
Contributors: VF reviewed the literature, co wrote and edited the manuscript. SZ-G co wrote and edited the manuscript. RS co wrote and edited the manuscript. AK collected the data and images, and co wrote and edited the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Casey S, Dvorkin L, Alsanjari N, et al. . Symptomatic malignant melanoma presenting as multiple gastrointestinal polyps. BMJ Case Rep 2011;2011:bcr0320102866 10.1136/bcr.03.2010.2866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Genova P, Sorce M, Cabibi D, et al. . Gastric and rectal metastases from malignant melanoma presenting with hypochromic anemia and treated with immunotherapy. Case Rep Oncol Med 2017;2017:1–4. 10.1155/2017/2079068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goral V, Ucmak F, Yildirim S, et al. . Malignant melanoma of the stomach presenting in a woman: a case report. J Med Case Rep 2011;5:11 10.1186/1752-1947-5-94 [DOI] [PMC free article] [PubMed] [Google Scholar]