Abstract
Stroke is the leading cause of serious long-term disability in the USA. Recent clinical trials, DAWN and DEFUSE 3, have expanded the endovascular therapeutic time window which has been adopted by the American Heart Association stroke guideline. However, there continues to be a dilemma as to what is the best approach for patients who present beyond the time window set by these trials and the current guideline. The interval from arterial occlusion to completion of brain tissue infarction varies from patient to patient and depends on the actual time and also a physiological clock or a tissue time window. Offering endovascular treatment based solely on a rigid time criterion excludes patients who may have a clinical benefit because of potentially salvageable tissue. We present a case of a patient who underwent successful stroke thrombectomy 6 days after stroke onset.
Keywords: stroke, thrombectomy, intervention, ct perfusion
Background
Stroke is the second cause of mortality around the globe and the leading cause of serious long-term disability in the USA.1 Recent clinical trials have demonstrated endovascular recanalization with medical management to be superior to medical management alone in the treatment of large vessel occlusions (LVO).2 These trials, however, limited endovascular treatment to patients who presented within the early hours from stroke onset.3 More recently, DAWN and DEFUSE 3 studies expanded the endovascular therapeutic time window to 24 hours from symptom onset in selected patients based on imaging and clinical mismatch.4 5 Their results have brought about a paradigm shift in our rigid adherence to a time window and who can benefit most from endovascular thrombectomy based on their physiological clock or tissue window. We present a case of a patient successfully treated 6 days after stroke onset and discuss our rationale for management.
Case presentation
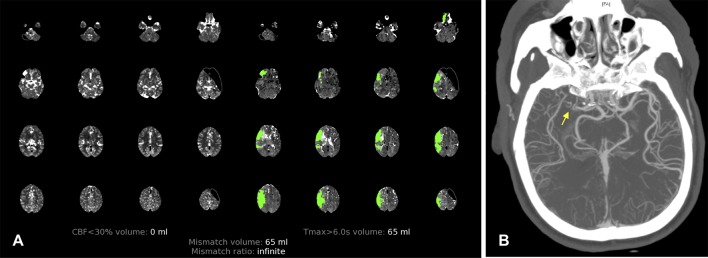
A 75-year-old woman with a past medical history of chronic hypertension, hyperlipidemia, and tobacco abuse presented to our emergency department with fluctuating left-sided weakness. Last known well (LKW) was 24 hours prior to hospital arrival and admitting NIH Stroke Scale (NIHSS) score was 1 (minor facial paralysis; figure 1). Non-contrast head CT showed an Alberta Stroke Program Early CT Score (ASPECTS) of 9 (1 point for insula) and ruled out hemorrhage. CT angiography demonstrated right middle cerebral artery (MCA) M1 division occlusion with good collaterals (equal to the contralateral hemisphere, collateral score of 3)6 and CT perfusion (CTP; RAPID software, iSchemaView, Menlo Park, California, USA) demonstrated 65 mL of maximum time to peak greater than 6 s (penumbra) in the same vascular territory with no core ischemic area identified (figure 2A and B). The patient was outside the tissue plasminogen activator therapeutic window and immediate thrombectomy was not performed due to the low NIHSS score. However, the patient was admitted to the neuro ICU for medical management, considering the evidence of LVO and sizeable penumbra on imaging.
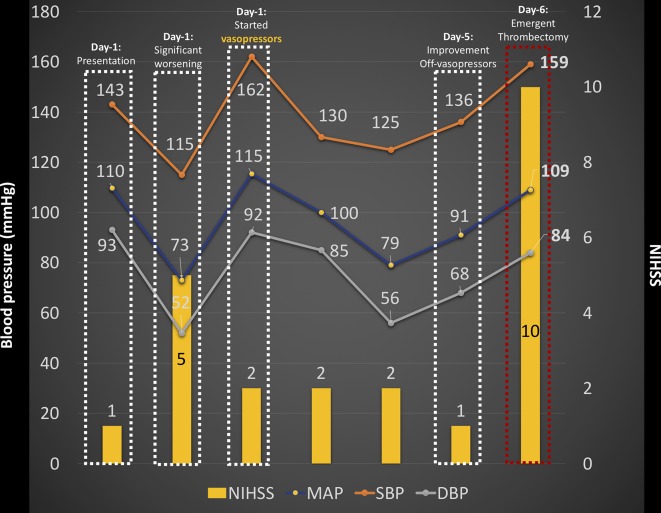
Figure 1.
Summary of blood pressure changes and neurological symptoms from hospital arrival to mechanical thrombectomy.
Figure 2.
(A) CT perfusion with RAPID software on arrival at hospital demonstrating 65 mL of maximum time to peak greater than 6 s (penumbra) and no core ischemic area. (B) CT angiography showing occlusion of the right middle cerebral artery (MCA; yellow arrow) and good collaterals (>50%) of the right MCA territory.
Treatment
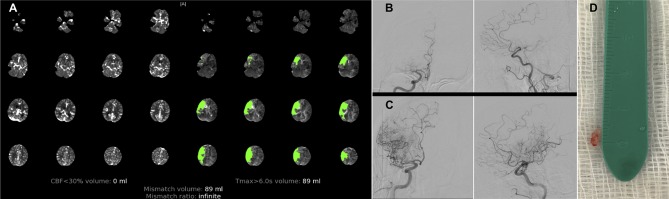
The patient was placed on dual antiplatelet therapy (aspirin and clopidogrel) with permissive hypertension and close neurological monitoring. Over the course of her first day of hospitalization the patient had mild fluctuating neurological symptoms (left upper extremity drift) which coincided with a decrease in her blood pressure (figure 1). Her symptoms resolved with initiation of vasopressors. On day 2 of hospitalization, head imaging was repeated which showed a similar ASPECTS score and persistent right MCA M1 occlusion was again noted with stable collateral blood flow. While in the ICU the patient had no new symptoms despite increased activity including independent mobilization. She was transferred out of the ICU on day 5. Of note, the patient was unable to have a brain MRI due to remote history of arterial stent that was not able to be cleared. On the sixth day, however, while at rest the patient was noted to have new and worsening symptoms including right gaze preference and left-sided hemiparesis with NIHSS score of 10 despite higher blood pressure (figure 1). Head CT showed no changes in the ASPECTS score and CTP demonstrated an 89 mL penumbra area in the right hemisphere (figure 3A). At that point the patient underwent successful mechanical thrombectomy and, after one pass via stent retriever combined with manual aspiration, a Thrombolysis in Cerebral Infarction (TICI) 2B score was achieved (figure 3B and C). A relatively hard thrombus (figure 3D) was retracted and the patient showed clinical improvement without any complications or hemorrhagic transformation after the procedure. Because of the suspicion of a cardioembolic source, the patient had an implantable heart monitor to detect atrial fibrillation.
Figure 3.
(A) On the sixth day after stroke onset the patient worsened neurologically (NIH Stroke Scale score 10) and CT perfusion demonstrated a greater area of risk (89 mL). A decision was made to perform a mechanical thrombectomy. (B) Initial catheter-based angiography demonstrated a right middle cerebral artery occlusion. (C) After mechanical thrombectomy (one pass), a Thrombolysis in Cerebral Infarction (TICI) 2B score was achieved. (D) A relatively hard thrombus was retracted and the patient did not have any complications or hemorrhagic transformation after the procedure.
Outcome and follow-up
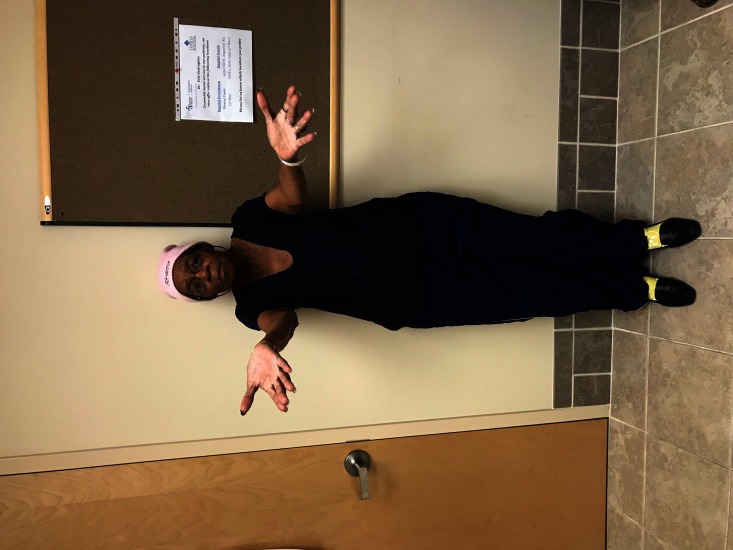
At 30-day clinical follow-up the patient remained neurologically intact with a modified Rankin Scale (mRS) score of 1 and NIHSS score of 0 (figure 4).
Figure 4.
At the 30-day clinical follow-up the patient was neurologically intact with a modified Rankin Scale score of 1 and NIH Stroke Scale score of 0.
Discussion
Endovascular treatment for patients with acute LVO has been widely accepted after proving clinical benefit at 90 days. However, this strategy has been limited to a few patients due to the restricted time window barrier of 6 hours in many clinical trials. The interval from arterial occlusion to the completion of brain tissue infarction varies from patient to patient and depends on the actual time, and also on the hemodynamic reserve compensating the tissue at risk with arterial recruitment, the availability of collateral blood flow and compensatory capacity, and the ischemic tolerance of the brain tissue. Offering endovascular treatment based solely on time criterion excludes patients who may have a clinical benefit because of potentially salvageable tissue. This concept was underscored by the recent positive trials (DAWN and DEFUSE 3)4 5 which expanded the endovascular treatment time window to 24 hours, and is also highlighted in this case.
The best treatment option for patients with a low NIHSS score and acute LVO is unclear at this point. There is no doubt these patients need to have close neurological monitoring. Further randomized trials are required to assess the benefit of endovascular treatment for patients with a low NIHSS score and acute LVO as well as the effect of collateral blood flow, since at this point it is difficult to predict which patients will deteriorate over time. Vascular imaging soon after an ischemic stroke is paramount to identify patients at risk of further deterioration despite the presenting NIHSS score. Patient selection for thrombectomy is essential in extended time windows and advance imaging such as MRI or CTP can certainly assist in such cases.
In our patient, several mechanisms favoured her clinical outcome: (1) slow progression of the ischemic stroke most likely due to robust collaterals; (2) detection of LVO with a sizeable penumbra; (3) close medical care and management in the neuro ICU with specific attention to neurological examination, blood pressure augmentation, and supportive care. On the sixth day the collateral reserve most likely began to fail, deeming it necessary to perform a mechanical thrombectomy. Our case represents a successful intervention beyond 24 hours based on an individual’s physiological clock. Other anecdotal experiences have also challenged the paradigm of time with positive outcomes.7
This paper is limited to a single case report and the results may not be generalizable to other patients. Additionally, stroke is an unstable dynamic process and, although imaging only provides information at one point in time, it adds extra value for individual treatment decisions when the extension of the core, the penumbra, and the collateral status are known. It is well known that larger core infarcts at presentation are associated with worse clinical outcomes despite revascularization.8 Further studies are required to determine which patients would still benefit from revascularization beyond 24 hours after stroke onset.
In the current era of stroke treatment, patient selection for thrombectomy should be individualized based on tissue window rather than being restricted by a rigid time window.
Learning points.
The DAWN and DEFUSE 3 clinical trials expanded the endovascular therapeutic time window to 24 hours of symptom onset in selected patients based on imaging and clinical mismatch.
The interval from arterial occlusion to completion of brain tissue infarction varies from patient to patient and depends on the actual time and also on a physiological brain tissue window.
Further studies are required to determine which patients would still benefit from revascularization beyond 24 hours after stroke onset.
Footnotes
Contributors: PA-S and AA were responsible for study concept and design. MFG and RS contributed to acquisition of the data. All the authors were responsible for analysis and interpretation of the data. PA-S, RS, and MFG contributed to the drafting of the manuscript. ES, RH, and AA contributed to critical revision of the manuscript for important intellectual content. All the authors were responsible for administrative, technical and material support. AA contributed to study supervision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: RH is a consultant for Medtronic, Stryker, Codman, and MicroVention. The other authors have nothing to disclose.
Patient consent: Obtained.
Ethics approval: BMC IRB, #16-58.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 2017;135:e146–603. 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31. 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, van der Lugt A, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 2016;316:1279–88. 10.1001/jama.2016.13647 [DOI] [PubMed] [Google Scholar]
- 4.Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2018;378:11–21. 10.1056/NEJMoa1706442 [DOI] [PubMed] [Google Scholar]
- 5.Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 2018;378:708–18. 10.1056/NEJMoa1713973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Souza LC, Yoo AJ, Chaudhry ZA, et al. Malignant CTA collateral profile is highly specific for large admission DWI infarct core and poor outcome in acute stroke. AJNR Am J Neuroradiol 2012;33:1331–6. 10.3174/ajnr.A2985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gunawardena R, Cheung A, Spira P, et al. Successful endovascular thrombectomy 90h after stroke onset. J Clin Neurosci 2017;46:69–71. 10.1016/j.jocn.2017.08.047 [DOI] [PubMed] [Google Scholar]
- 8.Jovin TG, Yonas H, Gebel JM, et al. The cortical ischemic core and not the consistently present penumbra is a determinant of clinical outcome in acute middle cerebral artery occlusion. Stroke 2003;34:2426–33. 10.1161/01.STR.0000091232.81947.C9 [DOI] [PubMed] [Google Scholar]