Abstract
Purpose
To assess the within-treatment efficacy of hot compresses (HC), HC plus tobramycin (Tobrex), and HC plus tobramycin/dexamethasone (Tobradex) for chalazia treatment.
Methods
Design
Multicenter, randomized clinical trial (ClinicalTrials.gov identifier, NCT01230593).
Setting
Two clinical sites in New York and 2 clinical sites in Ontario.
Study Population
149 patients with one or more chalazia on separate eyelids randomly assigned to receive HC (n=50), HC plus tobramycin (n=50), or HC plus tobramycin/dexamethasone (n=49).
Intervention
4-6 weeks of assigned treatment. Patients were measured for chalazion horizontal width and surveyed for pain and treatment satisfaction levels.
Main Outcome Measures
Primary outcome was complete resolution (100% size reduction). Secondary outcomes were size change in millimeters and patient reported pre and post treatment pain and satisfaction levels.
Results
In the intention to treat (ITT) population, complete resolution occurred in 36 (18%) lesions total, 13 (21%) treated with HC, 12 (16%) with HC plus tobramycin, and 11 (18%) with HC plus tobramycin/dexamethasone, with no significant difference between them (p = .78). Individually by paired t-test, there were statistically significant post-treatment mean size differences: HC 1.20 mm (p < 0.001), HC plus tobramycin 1.69 mm (p < .001), and HC plus tobramycin/dexamethasone 1.54 mm (p < 0.001), but no significant difference between them (p = .61). Lesions that completely resolved had a statistically significant lower pre-treatment duration (1.5 months) compared to lesions that did not completely resolve (2.2 months) (p = .04)
Conclusions
HC alone or in combination with tobramycin or tobramycin/dexamethasone drops and ointment are all effective first-line treatment options for chalazia. However, physicians may consider moving directly to the use of more invasive therapies, such as incision and curettage or steroid injections, for chalazia that have been present for more than 2 months, as older lesions are less likely to resolve with conservative therapies alone.
Keywords: chalazion, chalazia, tobramycin, hot compress, tobramycin/dexamethasone, orbit, eyelid lesions
Introduction
A chalazion is a chronic lipogranulomatous lesion affecting one or more of the upper or lower eyelids (Unal 2008). It can cause cosmetic distress, conjunctivitis or cellulitis when inflamed, and if large enough, may result in obscured vision or induced astigmatism from corneal pressure (Rumelt & Rubin 1996, Donaldson & Gole 2005). Higher incidences of chalazion have previously been found in patients with blepharokeratoconjunctivitis (BKC), as these patients have poor Meibomian gland function and morphology (Yin & Gong 2017). Chalazia are one of the most common eyelid lesions diagnosed in ophthalmologic, general practice, and emergency department settings (Gilchrist & Lee 2009). Despite this, there is a lack of consensus on a specific treatment algorithm, with available treatments falling into conservative and invasive categories. In up to 25% of cases, chalazia may also resolve spontaneously within a mean of six months from onset (Cottrell et al. 1983).
Conservative measures include the use of eyelid hygiene, hot compresses, and antibiotic and/or steroid drops. When using hot compresses alone, reported resolution rates range from 25-50% (Perry & Serniuk 1980). If initial conservative methods fail to resolve a chalazion, practitioners use intralesional corticosteroid injections or incision and curettage (I&C) to excise the lesion. The majority of prior studies have compared the efficacy of invasive treatment options, with intralesional corticosteroid injections found to be as effective as I&C and both options more effective than hot compresses (Simon et al. 2011, Goawalla & Lee 2007).
Despite the number of studies on invasive options, there have been no prospective randomized studies on conservative chalazion treatments alone, and no studies detailing the efficacy of antibiotic or combination antibiotic/steroid drops and ointment. The primary objective of our study was to determine the within-treatment efficacy of hot compresses alone, hot compresses plus tobramycin antibiotic drops and ointment (Tobrex), and hot compresses plus tobramycin/dexamethasone combination antibiotic/steroid drops and ointment (Tobradex). Secondary objectives included comparing patients’ subjective sense of chalazion size improvement after treatment.
Methods
Study Design
This was a 5-year multicenter prospective randomized treatment study (ClinicalTrials.gov identifier, NCT01230593). Patients with either one palpable chalazion on a single eyelid or multiple palpable chalazia each on separate eyelids (a single lesion per eyelid) who presented to four oculoplastics clinics at Mount Sinai Medical Center (New York, NY), Elmhurst Hospital Center (Elmhurst, NY), University of Toronto (Toronto, ON), and McMaster Hospital (Hamilton, ON) between May 2011 and March 2016 were invited to participate in the study. All patients who agreed to enroll gave written, informed consent. Prospective Institutional Review Board (IRB)/Ethics Committee approval was obtained at all sites (Icahn School of Medicine IRB, Queens/Elmhurst Research Committee, and the McMaster Research Ethics Board). The study was HIPAA-compliant and its procedures adhered to the principles of the Declaration of Helsinki. This study was funded in part by the National Eye Institute (P30-EY026877) and Research to Prevent Blindness, Inc. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Subjects
Eligible patients were aged 18 years or older and could have one palpable chalazion on a single eyelid or multiple palpable chalazia on separate eyelids (only one lesion per eyelid). Patients included also had normal eyelid anatomy enabling lid eversion. Patients were seen in one of four oculoplastics clinics and had been referred by comprehensive ophthalmologists, optometrists, emergency department physicians, or primary care physicians. Patients who had tried conservative therapies for their chalazia prior to enrollment, such as eyelid hygiene, hot compresses, topical or oral antibiotics and/or steroids, were still eligible to participate. Patients under 18 years of age, unable to give consent, with multiple chalazia on a single eyelid, concurrent eyelid infection (cellulitis or conjunctivitis), previous surgery to the affected eyelid, history of allergy to the study drugs, or chalazia with atypical features (recurring chalazion, abnormal surrounding lid tissue, associated loss of eyelashes) suspicious for malignancy were excluded. Eligible patients enrolled at 4 centers in the United States and Canada. Patients completed study visits at baseline and 4-6 weeks after 4-week treatment.
Randomization
Patients were randomized to receive one of three conservative treatments: hot compresses alone, hot compresses plus tobramycin drops and ointment, or hot compresses plus combination tobramycin/dexamethasone drops and ointment. Randomization (1:1:1 ratio) was by permuted blocks of 3 or 6 stratified by center, with assignments produced by SPSS (Release 18.0.0, PASW Statistics 18, Polar Engineering and Consulting) by the principal investigator. Treatment groups were initially concealed by serially numbered, opaque envelopes from three study coordinators who enrolled participants and assigned interventions. After patients were consented, treatment assignments were revealed to patients, study coordinators, and care providers, thus this trial employed no blinding methods. The hot compress group was considered the control group in this study, as it employed no form of medication for treatment, as in the groups combining hot compress with either tobramycin or tobramycin/dexamethasone.
Study Treatments
Patients in the hot compress group were instructed to place a hot compress (washcloth under hot tap water) against their eyelid(s) and gently massage for ten minutes in the morning and night. Those in the hot compress plus tobramycin group were prescribed tobramycin 0.3% solution, 1 drop three times a day to the eye and tobramycin ointment to apply to their chalazion externally (on the eyelid skin) before bed. Patients in the hot compress plus tobramycin/dexamethasone group were prescribed tobramycin/dexamethasone 0.3%/0.1% suspension, 1 drop three times a day to the eye and tobramycin/dexamethasone ointment externally before bed. Three oculoplastic surgeons across all four centers gave treatment instructions and prescriptions on the same day patients were examined and consented into the study. Patients whose chalazia failed to respond to their original assigned treatment were given the option to lance their chalazia or attempt another form of conservative treatment apart from the study.
Outcomes
At their initial visit, patients were measured subjectively by questionnaire (Figure 1) and objectively by direct measurement of the horizontal width of their chalazion via slit-lamp measurement. Since chalazia are 3-dimensional structures, the total volume of each lesion would in theory be the most clinically meaningful measurement to obtain. However, given the difficulty in assessing this measurement, horizontal width of each lesion was used as a proxy for this value. Patient questionnaires employed an 11-point Numerical Rating Scale for pain before and after treatment and a 0 to 4 scale for lesion improvement post-treatment, where 0 represented no change in lesion size post-treatment and 4 represented a lesion completely resolving post-treatment. There were no specific criteria given to patients for rating size improvement post-treatment. Patient ratings were based solely on a subjective sense of whether or not each lesion had improved, and patients were not surveyed about why they chose certain ratings. Thus, if a patient noted complete resolution of a lesion, this may have been due to any number of factors including but not limited to the patient not physically feeling a palpable lesion or not seeing a previously visible lesion any longer. Similar questionnaire rating scaled were utilized in a prior chalazion study comparing the efficacy of hot compresses to I&C and triamcinolone (TA) injections (Goawalla & Lee 2007).
Figure 1.
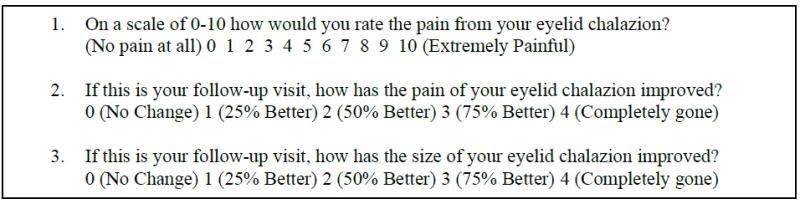
Pre and post-treatment patient questionnaire on chalazion pain and treatment satisfaction levels. Patients were asked to complete a questionnaire before and after 4-6 week treatment with either hot compress alone, hot compress plus tobramycin drops and ointment, or hot compress plus tobramycin/dexamethasone drops and ointment.
Patients were examined 4-6 weeks after treatment, at which point they were again measured subjectively by questionnaire and objectively by slit lamp exam by the same physician who had initially enrolled the patient at their site (one of three oculoplastics surgeons). Primary outcome measured was complete resolution (100% size reduction). Secondary outcomes measured were size change in millimeters and patient reported pre and post treatment pain levels (0-10 scale) and resolution rates (0-4 scale) (Figure 1). Patients who missed their follow up visit were called by study physician or study coordinators and given the questionnaire over the phone. They were then rescheduled for follow-up visit within 1 week of telephone conversation.
Statistical Analysis
The primary goal of this study was to detect a situation where there was complete chalazion resolution (100% size reduction). Using a two-sample pooled t test with equal numbers of subjects in each group, a sample size of n = 50 patients per group was found to achieve the above goal with 80% power and a significance level of p = 0.05. No interim analyses were performed during the study.
An intention to treat (ITT) analysis was performed using SPSS (SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. Chicago: SPSS Inc.). Missing data were imputed using the last-observation-carried-forward (LOCF) method for the final chalazion size at post-randomization visit. The Student t test and Fisher exact test were used to compare average values and proportions, respectively. A logistic regression model fitted by a generalized estimating equation approach assuming an exchangeable correlation between outcomes in each eyelid was used to account for the fact that some patients enrolled had multiple chalazia, with a single chalazion per eyelid. The Kruskal-Wallis test was used to compare the difference in patient questionnaire data measured on an ordinal scale between the three groups. Analyses were repeated in the per protocol (PP) population to supplement primary analyses. The cutoff for P value significance was P < .05 (2-tailed) at a 95% confidence interval.
Patient Involvement
There was no patient involvement in the design or conduct of the study itself.
Results
One hundred and fifty patients (198 eyelids) were initially enrolled. Fifty patients were assigned to each treatment group. One patient in the hot compress plus tobramycin/dexamethasone group was subsequently excluded because the initial size of their chalazion was never recorded. The intention-to-treat (ITT) population included 149 patients (hot compress, n = 50; hot compress + tobramycin, n = 50; hot compress + tobramycin/dexamethasone, n = 49). Of all patients in the ITT population, 105 (70%) completed study follow-up. Fifteen patients (30%) in the hot compress group, eighteen patients (36%) in the hot compress plus tobramycin group, and eleven patients (22%) in the hot compress plus tobramycin/dexamethasone group were lost to follow-up (Figure 2).
Figure 2.

Patient enrollment flow diagram for randomized controlled trial assessing within-treatment efficacy of three conservative chalazion treatments: hot compress, hot compress plus tobramycin drops and ointment, and hot compress plus tobramycin/dexamethasone drops and ointment.
Given the large loss to follow-up, further demographic analyses were carried out to determine the validity of the randomization process. In the ITT population, there were no differences between the three treatment groups in regard to baseline demographics and lesion characteristics (Table 1). In the PP population, there were also no differences between the three treatment groups in regard to baseline demographics and lesion characteristics (Supplemental Table 1). Similarly, there were no differences between the three treatment groups when considering patients with incomplete follow-up alone (Supplemental Table 2) or when comparing patients who completed follow-up and who were lost to follow-up in each of the three treatment groups when analyzed by specific treatment group alone (Supplemental Table 3). Given these results, randomization was not thought to be compromised despite a large loss to follow-up. It was assumed that loss to follow-up is common for patients with this particular diagnosis, and that many patients may have felt it unnecessary to return for follow-up if their lesion(s) had completely resolved.
Table 1.
Baseline Demographic and Lesion Characteristics of Intention to Treat Population of Patients with One or Multiple Chalazia (each on a single eyelid) Treated with Hot Compress alone or with Tobramycin or Tobramycin/Dexamethasone Drops and Ointment
| Hot Compress | Tobramycin | Tobramycin/Dexamethasone | p-value [95% CI] | |
|---|---|---|---|---|
| Number of Patients | 50 | 50 | 49 | |
| Number of Eyelids | 63 | 74 | 61 | |
| Age (Range, ±SD) | 45.50 (20-81, ±15) | 46.42 (18-88, ±19) | 47.52 (19-87, ±17) | 0.83 [43.80-49.16] |
| Gender | ||||
| Male | 25 (50%) | 26 (52%) | 20 (40%) | 0.58 |
| Female | 25 (50%) | 24 (48%) | 30 (60%) | |
| Pre-visit Duration (months) | 3.55 (±6) | 2.88 (±3) | 5.72 (±13) | 0.11 [2.83-5.11] |
| Eyelid Location | ||||
| RUL | 23 (37%) | 24 (32%) | 14 (23%) | 0.63 |
| RLL | 10 (16%) | 9 (12%) | 10 (16%) | |
| LUL | 21 (33%) | 27 (37%) | 22 (36%) | |
| LLL | 9 (14%) | 14 (19%) | 15 (25%) | |
| Mean Initial Size (mm) | 6.05 (±3) | 6.16 (±3) | 6.38 (±3) | 0.78 [5.82-6.56] |
CI = confidence interval; RUL = right upper eyelid; RLL = right lower eyelid; LUL = left upper eyelid; LLL = left lower eyelid
Twenty-six patients were treated at McMaster University, one patient at University of Toronto, 72 at Mount Sinai Hospital, and 50 patients at Elmhurst Hospital. The per-protocol (PP) population included 105 patients (hot compress, n = 35; tobramycin, n = 32; tobramycin/dexamethasone, n = 38).
Efficacy
Primary endpoint
Complete resolution occurred in 36 (18%) lesions total, 13 (21%) lesions treated with hot compress alone, 12 (16%) lesions treated with hot compress plus tobramycin, and 11 (18%) lesions treated with hot compress plus tobramycin/dexamethasone. There was no statistically significant difference in complete resolution between the three groups (p = .78, Table 2). Results in the PP population were consistent with this finding (p = 0.74). In an analysis using generalized estimating equations to account for multiple lesions on separate eyelids in the same patient, there were also no significant differences in regard to the primary outcome of complete resolution (Supplemental Table 4). Pre-treatment duration of lesions that completely resolved ranged from 0.03 to 9.5 months, with 31/36 (86%) lesions resolving in 6 months or less. In a subset analysis with a statistical duration cut-off of 6 months, lesions that completely resolved had a statistically significant lower pre-treatment duration (1.5 months) compared to lesions that did not completely resolve (2.2 months) (p = .04).
Table 2.
Primary Outcome, Secondary Outcome, and Patient Questionnaire Analysis in the 3 Treatment Groups
| Hot Compress | Tobramycin | Tobramycin/Dexamethasone | p-value [95% CI] | ||||||
|---|---|---|---|---|---|---|---|---|---|
| ITT | PP | ITT | PP | ITT | PP | ITT | PP | ||
| Number of Patients | 50 | 35 | 50 | 32 | 49 | 38 | |||
| Number of Eyelids | 63 | 44 | 74 | 53 | 61 | 44 | |||
| Complete Resolution at 4-6 weeks (%) | 13 (21%) | 13 (30%) | 12 (16%) | 12 (23%) | 11 (18%) | 11 (25%) | 0.78 | 0.74 | |
| Mean Size Difference (mm) | 1.20 (±3) | 1.72 (±4) | 1.69 (±3) | 2.36 (±3) | 1.54 (±3) | 2.14 (±3) | 0.61 [1.08-1.90] | 0.63 [1.55-2.63] | |
| Questionnaire Outcomes | Hot Compress Median (IQR) | Tobramycin Median (IQR) | Tobramycin/Dexamethasone Median (IQR) | ||||||
| ITT | PP | ITT | PP | ITT | PP | ITT | PP | ||
| Pre-Treatment Pain (Scale 0-10) | 0 (0, 0) | 0 (0, 0) | 0 (0, 1.5) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0.49 | 0.61 | |
| Post-Treatment Pain (Scale 0-10) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0.77 | 0.79 | |
| Pain Improvement (Scale 0-4) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0.78 | 0.87 | |
| Size Improvement (Scale 0-4) | 0 (0, 4) | 0 (0, 4) | 1 (0, 3.50) | 1 (0, 3.50) | 1 (0, 3.75) | 1 (0, 3.75) | 0.49 | 0.49 | |
CI = confidence interval; IQR = interquartile range
Secondary endpoints
There was also no significant difference between treatment groups in regard to the secondary outcome of mean size difference post-treatment on ANOVA (Table 2). Each of the three treatments resulted in a statistically significant decrease in chalazion size when analyzing treatments individually by paired t-tests: hot compress alone, p < 0.001 (95% CI, 4.03-5.67), hot compress plus tobramycin drops and ointment, p < 0.001 (95% CI, 3.81-5.12), and hot compress plus tobramycin/dexamethasone drops and ointment, p < 0.001, (95% CI, 3.94-5.72).
In regard to patient questionnaire data, patients who were lost to follow-up did not complete post-treatment questionnaires and were thus excluded from analysis of pain and size improvement data as outlined below. In total, 35 patients (44 lesions) treated with hot compress, 32 patients (53 lesions) treated with hot compress plus tobramycin, and 38 patients (44 lesions) treated with hot compress plus tobramycin/dexamethasone completed both pre and post treatment questionnaires for each of their chalazia and were included for statistical analysis. Patients in all three treatment groups most often experienced no pain before and after treatment and therefore recorded that they had no change in pain post-treatment when taking our survey. When rating their sense of size improvement after treatment, there was no significant difference in the response between groups, but patients treated with hot compresses alone more often rated their size improvement 0 (no change) compared to the hot compress plus either tobramycin or tobramycin/dexamethasone groups.
For lesions in the hot compress group, 59% were rated as having no change in size post-treatment, 7% as having 25% improvement, 2% as having 50% improvement, 2% as having 75% improvement, and 30% as having 100% improvement. For lesions in the tobramycin plus hot compress group, 40% were rated as having no change in size post-treatment, 15% as having 25% improvement, 11% as having 50% improvement, 9% as having 75% improvement, and 25% as having 100% improvement. For lesions in the tobramycin/dexamethasone plus hot compress group, 41% were rated as having no change in size post-treatment, 21% as having 25% improvement, 2% as having 50% improvement, 11% as having 75% improvement, and 25% as having 100% improvement. Overall, only 41% of lesions in the hot compress group were rated as having some form of improvement on the questionnaire, compared to 60% in the tobramycin plus hot compress group and 59% in the tobramycin/dexamethasone plus hot compress group.
A subset analysis comparing patients who were treatment naïve to those who had undergone prior conservative treatment for their chalazia was also conducted. Sixty patients (73 lesions) had never received treatment for their chalazia prior to enrollment in this study. In a subset analysis of these treatment naïve patients, complete resolution occurred in 13 (18%) lesions total, 8 (21%) treated with hot compresses alone, 2 (8%) treated with hot compresses plus tobramycin, and 3 (33%) treated with hot compresses plus tobramycin/dexamethasone (p = .19). Eighty-nine patients (125 lesions) had received prior treatment before enrollment in this study. Prior treatments included eyelid hygiene, hot compresses, topical antibiotics and/or steroids, oral antibiotics, or a combination of these options. In a subset analysis of these patients, complete resolution occurred in 23 (18%) lesions total, 5 (21%) treated with hot compresses alone, 10 (20%) treated with hot compresses plus tobramycin, and 8 (15%) treated with hot compresses plus tobramycin/dexamethasone (p = .76). There was no statistically significant difference in complete resolution rates between treatment naïve patients and those who had prior chalazia treatment (p = .92). There was also no difference in pre-treatment duration of chalazia between treatment naïve patients (2.9 months) and patients who had prior treatment (4.6 months) (p = .17).
Discussion
Past studies assessing the efficacy of chalazion treatments have all included invasive options such as I&C and TA injections and have not studied the efficacy of topical antibiotic and/or steroid drops and ointment (Wong et al. 2014, Simon et al.2005). This study is the first randomized trial that looks only at conservative methods of chalazion treatment. It is important to determine the within-treatment efficacy of each conservative treatment option, as these are considered first line in the management of chalazia (Gilchrist & Lee 2009). The findings from this randomized, multi-center clinical study demonstrate that complete resolution rates were low in each of the three treatment groups: hot compresses alone, hot compresses plus tobramycin drops and ointment, and hot compresses plus tobramycin/dexamethasone drops and ointment. The overall complete resolution rate for the study was only 18%, with a range from 16-21% depending on specific treatment group.
However, it is important to note that the 30% of patients who were lost to follow-up may not have returned to clinic because their lesions did completely resolve and they did not feel it was necessary to continue seeking care. If this was the case in our patient population, the overall complete resolution rate for the study may actually be as high as 48%, which is consistent with previous studies (Perry & Serniuk 1980). Similarly, resolution rates for each specific treatment group could be as high as 51% in the hot compress group, 52% in the hot compress plus tobramycin group, and 40% in the hot compress plus tobramycin/dexamethasone group. Each of the three treatment groups demonstrated a statistically significant difference in chalazion size change post-treatment. However, a statistically significant size change is not necessarily clinically relevant for patients who ideally would like complete resolution of their lesion(s).
These conclusions support the idea that all three of the studied conservative treatments are effective and should still be considered first line treatment options in the management of chalazia, especially for referring providers such as primary care and emergency department physicians, general ophthalmologists, and optometrists. However, we suggest that ophthalmologists consider advocating for surgical or more invasive therapy such as I&C or TA injections sooner in the course of these patients’ treatment if their chalazia have been present for a longer period of time prior to presentation. Past studies have suggested that physicians treat acute and chronic chalazia differently, but do not clarify their specific reasoning (Epstein & Putterman 1988). This implies knowledge in the medical community that chronic chalazia require more invasive treatment. In fact, one study found that patients with chalazia of duration greater than 8.5 months, lesions greater than 11.4 mm, and age greater than 35, were more likely to have chalazia with chronic suppurative granulomas on cytologic analysis, which were more likely to resolve by I&C than by TA or conservative therapies (Dhaliwal & Bhatia 2005). The few patients in our study who experienced complete resolution of their lesion(s) regardless of treatment group, on average had a shorter pre-treatment duration of their lesion(s) (2.4 months) compared to those without complete resolution (4.3 months).
Over 80% of lesions that completely resolved had a pre-treatment duration of 6 months or less. A subset analysis of lesions present for 6 months or less demonstrated a significant difference between the pre-treatment duration of lesions that completely resolved (1.5 months on average) and those that did not completely resolve (2.2 months on average). Of all lesions that completely resolved, 24/36 (67%) had a pre-treatment duration of 2 months or less, versus 12/36 (33%) that had been present for more than 2 months. We suggest that ophthalmologists consider starting patients on a trial of conservative therapy versus invasive therapy based on pre-treatment duration. They may wish to treat chronic chalazia with an invasive intervention first, as conservative measures are unlikely to resolve a long-standing problem. Based on our results, we speculate that patients whose chalazion has been present for 2 months or less could be started on a trial of conservative treatment first, whereas those with lesions present greater than 2 months should undergo I&C or TA injection as first line treatment. Further studies are needed to elucidate the exact time cut-off at which to directly start with invasive therapy instead of a trial of conservative treatment. In addition to the fact that invasive therapies for chalazia have been found to be more effective in completely resolving lesions, starting with surgical options may also reduce patients’ exposure to antibiotics and/or steroids. Overuse of antibiotics contributes to antibiotic resistance, while overuse of steroids can cause increased intraocular pressure and steroid-induced glaucoma. Intraocular pressure post-treatment was not monitored in our study.
In regard to patient questionnaire data, patients who received prescription medication in the form of tobramycin or tobramycin/dexamethasone eye drops and ointment, rated their subjective sense of size improvement in their chalazion after treatment higher than patients who received hot compresses alone. This coincides with prior studies that have found that patients with high satisfaction rates are more likely to rate their health as excellent and more likely to have higher prescription drug expenditure than patients with low satisfaction rates (Fenton et al. 2012). Receiving and filling prescriptions from a physician influences patients’ treatment satisfaction which in turn may inform how patients view their own treatment success. Even though those treated with hot compresses had comparable size improvement to those treated with hot compresses plus antibiotic and/or steroid drops, patients who were given tobramycin or tobramycin/dexamethasone rated their treatment success higher.
There are several limitations to this study. Loss to follow-up was large across all three treatment groups, with an overall follow-up rate of only 70%. Despite a large loss to follow-up, no significant demographic differences were found between patients who completed follow-up and those who did not in each specific treatment group alone (Supplemental Tables 3). Based on these comparisons, randomization was not thought to be compromised and it was assumed that this particular diagnosis might naturally have a large loss to follow-up. Patients who experienced excellent results from their treatment might have found it unnecessary to return again and therefore their data was lost. In four phone conversations with patients who did not come to their follow up appointments, it was indicated that this was the case. Two of those phone calls were with patients in the hot compress plus tobramycin/dexamethasone group, one with a patient in the hot compress alone group, and one with a patient in the hot compress plus tobramycin group. Since the loss to follow up was largest in the hot compress with tobramycin group, it is possible that resolution was theoretically highest in this group and that these patients did not return for follow-up because their lesions resolved. The success rate for the three treatment groups may be higher than calculated due to this phenomenon.
It is also important to note that because our study patients had been referred to oculoplastics clinics by other physicians such as primary care and emergency department physicians, general ophthalmologists, and optometrists, there may be an inherent selection bias present that skews the results of this study. It can be assumed that once a patient is referred to a subspecialty level clinic, they have already been started on or failed prior treatments upon presentation to an oculoplastic surgeon. In this regard, many of our study patients may have been biased toward treatment failure upon enrollment, as 63% of the patients had undergone previous treatment of their chalazia with conservative options. Despite this, complete resolution rates did not significantly differ between patients who had prior treatment and those who were treatment naïve. Additionally, upon interview, many patients stated that they had not been treated prior, but had waited a long period of time to seek care because they thought their lesion(s) would resolve spontaneously. Thus, the average pre-treatment duration of lesions in each treatment group was most likely high due to the study including patients who had never sought care for long periods of time and patients who were referred to our subspecialty clinics after starting prior conservative treatments.
Finally, this study was only powered to observe within-treatment efficacy of each conservative treatment group rather than comparative efficacy between the groups. Further studies with a larger sample size are needed to assess comparative efficacy and to elucidate specific time-cutoffs for initiating conservative versus surgical therapy. It is also possible that some patients with unresolved chalazia in the study were initially misdiagnosed. It is common for other benign, premalignant, and malignant eyelid lesions to masquerade as chalazia. For this reason, it has been suggested that all chalazia be submitted for official diagnosis by histopathological exam (Ozdal et al. 2004). In our study, chalazion diagnosis was made clinically with no pathologic confirmation.
In summary, our study confirms that conservative treatments, including previously unstudied antibiotic and/or steroid eye drops and ointment, are all effective in completely resolving chalazia, and should remain the first line treatment options, particularly for referring providers. However, this study also suggests that ophthalmologists, particularly those in subspecialty clinics such as oculoplastics, could potentially use surgical or invasive therapy earlier on in the course of chalazion treatment or as the initial therapy in patients who present with long-standing lesions. Further studies are needed to determine the exact pre-treatment lesion duration requiring initial therapy with surgery rather than conservative therapy and the characteristics of chalazia that may be refractory to conservative treatment methods alone.
Supplementary Material
Acknowledgments
The authors would like to acknowledge support from Research to Prevent Blindness, Inc., and the National Eye Institute (P30-EY026877).
Footnotes
None of the authors have any financial conflicts of interest to disclose.
References
- Ben Simon GJ, Huang L, Nakra T, Schwarcz RM, McCann JD, Goldberg RA. Intralesional triamcinolone acetonide injection for primary and recurrent chalazia: is it really effective? Ophthalmology. 2005;112:913–7. doi: 10.1016/j.ophtha.2004.11.037. [DOI] [PubMed] [Google Scholar]
- Ben Simon GJ, Rosen N, Rosner M, Spierer A. Intralesional triamcinolone acetonide injection versus incision and curettage for primary chalazia: a prospective, randomized study. Am J Ophthalmol. 2011;151:714–18. doi: 10.1016/j.ajo.2010.10.026. [DOI] [PubMed] [Google Scholar]
- Cottrell DG, Bosanquet RC, Fawcett IM. Chalazions: the frequency of spontaneous resolution. Br Med J (Clin Res Ed) 1983;287:1595. doi: 10.1136/bmj.287.6405.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhaliwal U, Bhatia A. A rationale for therapeutic decision-making in chalazia. Orbit. 2005;24:227–30. doi: 10.1080/01676830590946907. [DOI] [PubMed] [Google Scholar]
- Donaldson MJ, Gole GA. Amblyopia due to inflamed chalazion in a 13-month old infant. Clin Experiment Ophthalmol. 2005;33:332–3. doi: 10.1111/j.1442-9071.2005.00982.x. [DOI] [PubMed] [Google Scholar]
- Epstein GA, Putterman AM. Combined excision and drainage with intralesional corticosteroid injection in the treatment of chronic chalazia. Arch Ophthalmol. 1988;106:514–6. doi: 10.1001/archopht.1988.01060130560036. [DOI] [PubMed] [Google Scholar]
- Fenton JJ, Jerant AF, Bertakis KD, Franks P. The Cost of Satisfaction: A National Study of Patient Satisfaction, Health Care Utilization, Expenditures, and Mortality. Arch Int Med. 2012;172(5):405–411. doi: 10.1001/archinternmed.2011.1662. [DOI] [PubMed] [Google Scholar]
- Gilchrist H, Lee G. Management of chalazia in general practice. Aust Fam Physician. 2009;38:311–4. [PubMed] [Google Scholar]
- Goawalla A, Lee V. A prospective randomized treatment study comparing three treatment options for chalazia: triamcinolone acetonide injections, incision and curettage and treatment with hot compresses. Clin Experiment Ophthalmol. 2007;35:706–12. doi: 10.1111/j.1442-9071.2007.01617.x. [DOI] [PubMed] [Google Scholar]
- Ozdal PC, Codere F, Callejo S, Caissie AL, Burnier MN. Accuracy of the clinical diagnosis of chalazion. Eye (Lond) 2004;18:135–8. doi: 10.1038/sj.eye.6700603. [DOI] [PubMed] [Google Scholar]
- Perry HD, Serniuk RA. Conservative treatment of chalazia. Ophthalmology. 1980;87:218–21. doi: 10.1016/s0161-6420(80)35250-0. [DOI] [PubMed] [Google Scholar]
- Rumelt S, Rubin PA. Potential sources for orbital cellulitis. Int Ophthalmol Clin. 1996;36:207–21. doi: 10.1097/00004397-199603630-00019. [DOI] [PubMed] [Google Scholar]
- Unal M. Chalazion Treatment. Orbit. 2008;27:397–8. doi: 10.1080/01676830802623174. [DOI] [PubMed] [Google Scholar]
- Wong MY, Yau GS, Lee JW, Yuen CY. Intralesional triamcinolone acetonide injection for the treatment of primary chalazions. Int Ophthalmol. 2014;34:1049–53. doi: 10.1007/s10792-014-9904-1. [DOI] [PubMed] [Google Scholar]
- Yin Y, Gong L. The evaluation of meibomian gland function, morphology and related medical history in Asian adult blepharokeratoconjunctivitis patients. Acta Ophthalmol. 2017;95:634–8. doi: 10.1111/aos.13136. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


