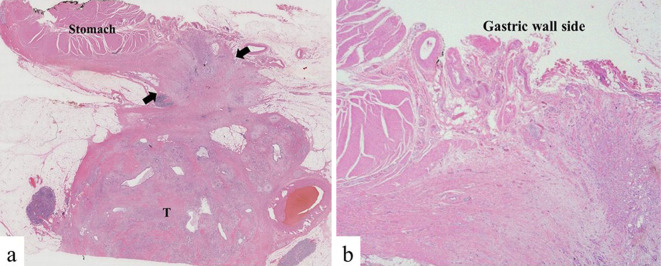
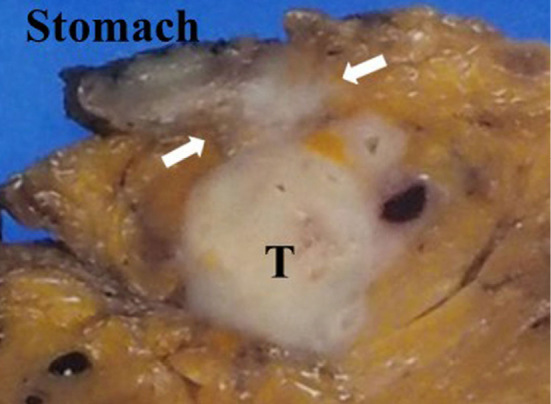
A 50-year-old man was referred to our hospital for the further evaluation of a pancreatic mass. Contrast-enhanced computed abdominal tomography (CE-CT) showed a 35-mm solid mass in the pancreatic body with soft tissue around the tumor extending to the celiac plexus. Endoscopic ultrasonography-guided fine needle aspiration (EUS-FNA) for the pancreatic mass was performed (21-G needle, 3 passes) via the trans-gastric approach, confirming the diagnosis of adenocarcinoma. CE-CT indicated celiac plexus invasion, and chemotherapy was administered for 8 months, during which the tumor size was reduced. However, CE-CT showed soft tissue density (arrow) between the stomach and pancreatic tumor (T) (Picture 1). EUS also showed soft tissue (arrow) from the stomach serosa (asterisk) to the pancreatic tumor (T) (Picture 2). Possible needle tract seeding was considered. We therefore planned distal pancreatectomy and partial stomach resection. The pathological findings of the resected specimen showed a pancreatic adenocarcinoma 25 mm in size (T) and fibrosis with cancer infiltration from the pancreatic body to the gastric wall (arrow) (Picture 3: gross specimen, Picture 4a: Hematoxylin and Eosin (H & E) staining loupe image, 4b: H & E staining×40).
Picure 1.
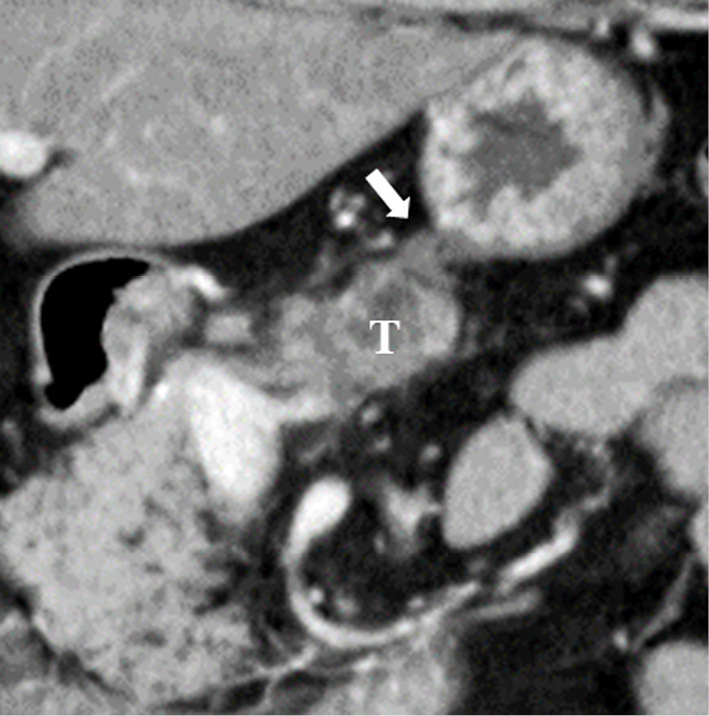
Picure 2.

Picure 3.
Picure 4.
The authors state that they have no Conflict of Interest (COI).