Abstract
AIM
To study effects of orthokeratology (Ortho-k) on accommodation function in myopic children.
METHODS
A prospective, non-randomized, case-control study was performed from September to October 2016. Eighty-three children with myopia were divided into two groups. One group was treated with the rigid contact lens for overnight Ortho-k, and the other was treated with single-vision spectacle lens (SVL). Accommodation function were assessed by accommodative amplitude (AA), accommodative sensitivity (AS), accommodative lag (Lag), negative relative accommodation (NRA), and positive relative accommodation (PRA) before and 1, 3, 6 and 12mo after treated.
RESULTS
Totally 72 myopic children were finished the follow-up: 37 in Ortho-k group and 35 in SVL group. Wearing time had a significant effect on AA, AS, Lag, and NRA of myopic children in two groups (all P<0.05). Meanwhile, there was an interaction effect between wearing time and wearing types (FAA=5.3, FAS=45.5, FLag=7.0, FNRA=3.7, all P<0.05). However, the between-group difference of AA (F=0.1), AS (F=3.2), Lag (F=1.1), NRA (F=0.3), and PRA (F=0.1) showed no significance. AA, AS, NRA, Lag and PRA were improved significantly in Ortho-k group within 1 to 6mo after wearing.
CONCLUSION
Wearing Ortho-k can improve the accommodation function of myopic children, which might be one of the mechanisms for myopia control.
Keywords: orthokeratology, accommodation, myopia, children
INTRODUCTION
Orthokeratology (Ortho-k) is a rigid gas permeable (RGP) contact lens designed in an anti-geometric way, which can decrease ametropia by reshaping cornea[1]. Different regions and races like Iran[2], Switzerland[3], Russia[4], India[5], Singapore[6], and China[7] have extensively reported the good control effect of Ortho-k on myopia children. And its function of delaying the myopia progression has been verified. It has been widely used for myopic children among the world, especially in Asian countries where incidence of myopia is high. However, mechanism of these procedure remains unclear. It could be due to changes of refractive status around retinal[8]–[9], anterior chamber depth, and pupil size[10], etc.
Among these assumptions, accommodation function (AF) is an important factor that may affect the myopia progress. Many scholars have done related studies. Wu et al[11] noted that the accommodative lag (Lag) decreased when myopic patients were in the demand of high accommodation after wearing Ortho-k, which retard myopia progression. Zhu et al[12] had reported that juvenile myopia patients with low accommodative amplitude (AA) could obtain the better myopia control effect after two years of wearing Ortho-k. However, in a latest study, Felipe-Marquez et al[13] found no significant changes in AF after three months and three years. It shows that the conclusions of the above studies are not consistent. And all studies have no continuous accommodation data after wearing Ortho-k. As myopia incidence in the younger age is high, children are more often given Ortho-k. Will the wearing of Ortho-k affect the accommodation of children? How does the AF change?
We evaluated Ortho-k effects on AF in myopic children for one year with comparing to children using single-vision spectacle lens (SVL). AF included AA, accommodative sensitivity (AS), Lag, negative relative accommodation (NRA) and positive relative accommodation (PRA).
SUBJECTS AND METHODS
Subjects
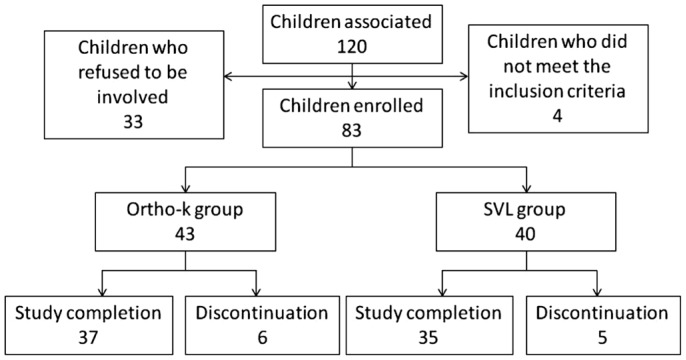
This is a prospective, non-randomized, and control study for one year. One hundred and twenty children received treatment in Shaanxi Institute of Ophthalmology from September to October 2016 were associated (Figure 1). Their parents had been told the advantages and disadvantages as well as possible complications after wearing Ortho-k and SVL in details. All children and their parents were informed the trial protocol, objectives, and procedures beforehand. The study was approved by the Ethics Committee of Xi'an Medical University and written consent was obtained from the children or their parents before study participation.
Figure 1. Flow chart showing particpants' recruitment.
Myopic children with the following conditions were enrolled, age from 8 to 15y; monocular spherical equivalent refractive error (SER) from -0.50 D to -6.00 D; monocular astigmatism form -0.25 D to -1.25 D; corneal flat K value form 39 D to 46 D; monocular best-corrected visual acuity of 0.0 logarithm of mininal angle resolution (logMAR) or better; wearing spectacle glasses before starting the trial; good compliance and follow-ups on time. Exclusion criteria: binocular SER>2 D; correction method replaced during the trial; presence of eye organic diseases; history of eye surgery or trauma; presence of abnormal eye position or eyeball movement.
All children completed the questionnaire, including age, gender, onset time of myopia and refraction of parents.
Orthokeratology
The American Euclid Ortho-k was used for the Ortho-k group, whose lens material is fluorosilicone acrylate (Boston XO, USA) with high oxygen permeability. And its oxygen permeability coefficient (Dk) is 100×10−11(cm2/s) (mL O2/mL·mm Hg). The lens diameter was set to 10.6 mm or 10.8 mm. All children will perform the standard trail wearing to a fittest lens state (good centralized positioning, movement degree of 1.5 to 2.5 mm, and ideal or acceptable fluorescence distribution). Each child and their parents had a detailed guidance on wearing methods and lens care. After receiving custom-made formal lens, all children were asked to wear it at least 8h per day for no less than 6d per week. Every children should cooperate for a follow-up study after wearing at 1d, 1wk, 1, 3, 6 and 12mo or return back anytime when any abnormal conditions episode. If a subject's monocular visual acuity was found less than 0.1 logMAR, he or she should replace lens. Visual acuity was measured with logMAR chart.
Single-vision Spectacle Lens
The material of SVL was aspherical blooming resin flake with refractive index of 1.56 or 1.6. The children wear it all day. If the optometry deviation of their former spectacle was within 0.50 D, the children still wear the old glasses. If there was a deviation over 0.50 D or worn glasses or deformed frames, the children change a new pair of glasses timely.
Accommodation Function Parameters
The baseline refractive status of both groups was obtained by optometry after cycloplegia with Mydrin-P. In addition to routine follow-ups, children needed to test their binocular AA, AS, Lag, NRA and PRA at month 1, 3, 6, and 12 after wearing. All AF were measured based on long-distance correction by the same examiner at 9 to 12 o'clock in the morning.
Accommodative amplitude
1) The examiner placed a pair of long-distance refractive correction lenses ahead of the children's eyes which were opened at the same time to measure binocular AA; 2) the children or the examiner held the visual acuity chart under a good lighting environment, then the subject looked at the one to two lines of visual target above his or her best vision and maintained to see a clear visual target; 3) the examiner moved the chart to the children slowly, and the children report immediately when the visual targets began to be blurred; 4) the linear distance which means the distance from the visual acuity chart to the subject's glasses/lens was measured. And this linear distance was near point (NP) distance. AA=1/s (‘s’ means accommodation of NP).
Accommodative sensitivity
The children watched a visual target above the best-corrected visual acuity which was placed at 40 cm distance away by using a ±2.00 D flipper on the basis of binocular long-distance correction. The children report whenever he or she could see the visual target clear after each flip. Then the examiner turned the flipper over and the subject reports again alternatively. The examiner counted the flipping times within one minute.
Accommodative lag
The examiner placed a ±0.50 D cross cylinder ahead of the children's eyes on the basis of long-distance correction by using a comprehensive refractometer. Then the negative axis of cross cylinder was fixed at 90° and the positive axis at 180°. After that, the children were asked to see the fused cross cylinder (FCC) test visual target through the cross cylinder. If the children reported to see the horizontal line more clear than the vertical line, it indicated the children have Lag. Accommodation should be made by adding positive lens with a +0.25 D lens one by one gradually before the children's eyes until the subject could see both line equally clear. If the children report the vertical line were more clearly, it indicated an advanced accommodation. Accommodation should be made by adding negative lens with a -0.25 D lens one by one gradually before the children's eyes until the subject could see both lines equally clear.
Negative relative accommodation and positive relative accommodation
The examiner used the comprehensive refractometer to make children watch the previous line of visual target for the best vision which is measured at 40 cm distance on the basis of binocular long-distance correction. NRA was measured firstly. By adding positive lens with a +0.25 D lens at one time before the children's eyes until the target was blur to the subject. And the total adding lens number recorded was the value of NRA. By removing all positive lens and adding negative lens ahead of the children's eyes with a -0.25 D lens at one time until the target was blur to the subject. And the final adding number of negative lens was the value of PRA.
Following-up
Parents needed to confirm their wearing and caring methods at every follow-up and those who did not adhere to the standard experimental ways must be excluded.
Statistical Analysis
All data were analyzed by Statistical Product and Service Solutions 20.0 software (SPSS, IBM, USA). The comparison of accommodation functions between two groups was analyzed with repeated measures analysis of variance. Age and spherical equivalent at baseline were measured by t test. Enumeration data were measured by χ2 test. The statistical significance was indentified when P<0.05.
RESULTS
Among 83 children (Ortho-k group with 43, SVL group with 40), there were 11 children who did not complete the following-up for various reasons (7 children failure to taking reexaminations at required time, 2 subjects without cooperation of AF tests, 1 child lost contact after three-month follow-up, and 1 child gave up to continue wearing Ortho-k due to cracked lens). There were 72 children finally finished the study.
Basic Data of Completed Study Children
There was no significant difference between two groups in baseline data including age, gender and refractive status (Table 1).
Table 1. Baseline data of children in Ortho-k group and spectacle group.
| Groups | Case | Age (y) | Gender (Male/Female) | SER (diopter) |
| Ortho-k | 37 | 11.2±1.9 | 14/23 | -3.3±1.2 |
| SVL | 35 | 11.6±1.9 | 18/17 | -3.0±1.1 |
| t/χ2 | - | -0.8a | 1.3b | -1.1a |
| P | - | 0.4 | 0.2 | 0.3 |
Ortho-k: Otrthokeratology; SVL: Single-vision spectacle lens; SER: Spherical equivalent refractive error. at test for two independent samples; bχ2 test.
Accommodation Function Changes
The wearing time had a significant impact on AF of both groups except for PRA (FAA=5.6, P=0.00; FAS=59.0, P=0.00; FLag=8.3, P=0.00; FNRA=4.2, P=0.00; FPRA=0.6, P=0.70). Meanwhile, there was an interaction effect between wearing time and type (FAA=5.3, P=0.00; FAS=45.5, P=0.00; FLag=7.0, P=0.00; FNRA=3.7, P=0.00), that is, the different wearing type would have different variation trend in AA, AS, Lag and NRA. Besides, there were no significant changes in accommodative parameters between groups (FAA=0.1, P=0.70; FAS=3.2, P=0.08; FLag=1.1, P=0.30; FNRA=0.3, P=0.60; FPRA=0.1, P=0.80). The tendency chart showed that AA, AS and NRA in Ortho-k group increased as wearing time extended, yet an obvious decrease trend was occurred for Lag. The changing speed was fastest after wearing within one to six months. Then the speed was slowed down after 6mo (Table 2).
Table 2. Changes in AF during the 12-month treatment of children between Ortho-k group (n=37) and SVL group (n=35).
| AF | Groups | Baseline | 1mo | 3mo | 6mo | 12mo |
| AA (D) | Ortho-k | 14.2±1.8 | 14.3±1.8 | 14.5±1.9 | 14.6±1.8 | 14.6±1.9 |
| SVL | 14.3±2.0 | 14.3±2.0 | 14.3±2.0 | 14.3±2.0 | 14.3±2.1 | |
| AS (cpm) | Ortho-k | 8.9±1.8 | 9.3±2.0 | 9.9±2.0 | 10.2±2.1 | 10.2±1.9 |
| SVL | 8.8±1.9 | 8.9±1.8 | 9.0±1.7 | 8.9±1.7 | 9.0±1.8 | |
| Lag (D) | Ortho-k | 0.7±0.4 | 0.7±0.3 | 0.6±0.3 | 0.6±0.2 | 0.6±0.2 |
| SVL | 0.7±0.4 | 0.7±0.3 | 0.7±0.3 | 0.7±0.3 | 0.7±0.3 | |
| NRA (D) | Ortho-k | 1.8±0.4 | 1.8±0.5 | 1.9±0.5 | 1.9±0.5 | 1.9±0.4 |
| SVL | 1.8±0.5 | 1.8±0.5 | 1.8±0.5 | 1.8±0.4 | 1.8±0.4 | |
| PRA (D) | Ortho-k | -1.9±0.4 | -1.9±0.5 | -1.9±0.5 | -1.9±0.5 | -1.9±0.5 |
| SVL | -1.9±0.5 | -1.9±0.7 | -1.9±0.7 | -1.9±0.7 | -1.9±0.6 |
AF: Accommodation function; AA: Accommodative amplitude; AS: Accommodative sensitivity; Lag: Accommodative lag; NRA: Negative relative accommodation; PRA: Positive relative accommodation; Ortho-k: Orthokeratology; SVL: Single-vision spectacle lens; D: Diopter; cpm: Circle per minute.
mean±SD
DISCUSSION
Ortho-k and SVL are two most widely used correction methods for myopic children. Our study found that Ortho-k can improve AF faster and better. This is great significance to the improvement of the visual quality of myopic children.
Results showed that children in both groups have experienced a decrease in Lag and an increase in AA, AS, and NRA. Wearing Ortho-k can improved AF better than wearing SVL. Before treating with Ortho-k, myopic children's AA is less than the counted value by Hofstetter's formula[14]. While after wearing, their AA increases dramatically. This result consists with conclusions drew by Zhu et al[12]. They has followed subjects' AA who had worn Ortho-k for two years. Though these two studies are different in follow-up time and experimental method, Zhu et al[12] also found that wearing Ortho-k can improve AA. But, they compared data before and after two years' wearing only, and could not explicit more change details within this period for the lack of data. Wearing Ortho-k can overcome deficiencies of spectacle in correcting myopia, which might be the cause that helps Ortho-k improving AA. For example, there is an elimination of shrinkage effect for objective image caused by spectacle lens and a relieving of prism effect and lens effect caused by spectacle lens. It helps increasing accommodative need. With sustained amount of increasing accommodative need, it stimulates the progress in accommodative force and improves AA.
Felipe-Marquez et al[13], however, held a different view that there was no changes in AA after wearing Ortho-k. That might cause by the adult subjects chosen, yet our study chose children between age 8 to 15y who had more plasticity in AA than adults. The increase in AA means the decrease in accommodative lag. In this study, the Lag dropped from 0.74±0.36 to 0.59±0.24 D after wearing Ortho-k. Using the method of dynamic retinoscopy to measure the monocular value, Han et al[15] found the 0.29±0.07 D decrease in Lag after one year wearing. Although there are different research methods, the result is basically same. Also similar conclusions drew by Ren et al[16], who found a sharp decrease in Lag value after one year wearing in both low and moderate myopia groups. And such improvement was greater than that of spectacle group. Comparing with the Lag value under different accommodative stimuli, Huang et al[17] found that Lag would be declined under high accommodative stimuli (≥3 D), but remained unchanged under 2 D or lower accommodative stimuli. The Lag value while the children saw the visual target with 40 cm distance ahead of eyes (Lag value at the 2.5 D accommodative stimuli) was decreased in this study.
It might be caused by using different testing methods. The FCC was used in our study to measure Lag. However, Huang et al[17] measured it through an open-field infrared refractometer and then counted the data. In addition to changes in above accommodative parameters, AS and NRA of myopic children who wear Ortho-k were also increased significantly.
The improvement mechanisms of AF might be related to peripheral refraction and aberration distribution after wearing. It has been confirmed that Ortho-k can change peripheral retinal refraction from hyperopic defocus to myopic defocus, especially that in the horizontal direction[18]. Such change can improve retina, especially improve the imaging quality of peripheral retina so as to ensure visual signals that enter into or leave cerebral cortex more precise[19]. Thereby, the accuracy of accommodative response is improved and the Lag value is decreased. Another reason for the improvement of AF might be aberration changes of myopic children caused by Ortho-k, which in turn changes accommodative cues and eventually changes accommodative functions. Tarrant et al[20] using a counting method, put out a hypothesis that the increase of spherical aberration leads to the decrease of Lag after wearing Ortho-k. Later on, Gifford et al[21] found that spherical aberration was increased toward the positive direction after one week of Ortho-k wearing through clinical observation. By studying quantitative effects of Ortho-k on spherical aberration, Thibos et al[22] found that spherical aberration of subjects would be increased 4 to 8 times after one week of wearing, which further reduced demands for myopic accommodation and was conducive to improve the accuracy of accommodation system under a defocusing state. Hiraoka et al[23] did a similar research and found dramatic change of full-eye aberration for myopia people after wearing Ortho-k. This change helped people to capture spatial distance and depth of object faster and more accurately. Besides, it could shorten defocusing distances, which enabling retina to make a clearer image, further decreasing Lag value, and increasing AA and AS.
It is worth mentioning that time effect was positive according to the dynamic follow-up, that is, four parameters of AA, AS, Lag and NRA were constantly improved as the extension of wearing. This improvement reached a prominent level in the half a year of wearing, but slowed down after wearing for six months.
A two-year randomized clinical trial[7] carried out in Hong Kong has shown that optic axial length of myopia people was decreased 55%, 51%, 51%, and 41% respectively at month 6, 12, 18, and 24 after wearing Ortho-k, which indicating a declined trend in its control over optic axial elongation. This shows that improvement in AF is consistent with myopic control tendency by Ortho-k. Therefore, the conjecture goes that accommodation improvement may be an important mechanism for delaying optic axial length and controlling myopia by Ortho-k. When working in a close distance, the inaccuracy of accommodation will lead to the retinal hyperopia defocus, which accumulates to a bigger defocus. The accumulation effect might have a greater impact on children for their constantly exchange between close-distance and long-distance visual targets due to learning. While optic axial grows longer in order to counteract retinal hyperopia defocus, which leads to myopia occurrence and development. After wearing Ortho-k, the above parameters of subjects have been improved and the hyperopia refraction of peripheral retina has been reduced which enabling a more accurate visual experience. Sequentially, the optic axial length is restrained and the myopia progress is controllable.
Although this study has performed an overall and dynamic study on accommodative changes of subjects after wearing Ortho-k, limitations still exist as follows, the first one is short follow-up time. The further investigation about effects on AF should be made after wearing for a longer time as well about accommodation changes after stopping wearing. The second is that only one Ortho-k brand is used in this study. Due to enough brand coverage, the detailed comparison should be made over different designs and types of Ortho-k in the future study.
Acknowledgments
Foundation: Supported by Special Scientific Research Program of Shaanxi Provincial Education Department (No.17JK0662).
Conflicts of Interest: Yang Y, None; Wang L, None; Li P, None; Li J, None.
REFERENCES
- 1.Jessen GN. World wide summary of contact lens techniques. Am J Optom Arch Am Acad Optom. 1962;39:680–682. doi: 10.1097/00006324-196212000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Rajabi MT, Hosseini SS, Ghorbani Z, Nobahari F, Bazvand F, Doostdar A, Zarrinbakhsh P, Rajabi MB. Utility of orthokeratology contact lenses; efficacy of myopia correction and level of patient satisfaction in Iranian myopic/myope-astigmatic patients. J Curr Ophthalmol. 2015;27(3-4):99–102. doi: 10.1016/j.joco.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, Gutiérrez-Ortega R, Sugimoto K. Long-term efficacy of orthokeratology contact lens wear in controlling the progression of childhood myopia. Curr Eye Res. 2017;42(5):713–720. doi: 10.1080/02713683.2016.1221979. [DOI] [PubMed] [Google Scholar]
- 4.Tarutta EP, Verzhanskaya TY. Stabilizing effect of orthokeratology lenses (ten-year follow-up results) Vestn Oftalmol. 2017;133(1):49–54. doi: 10.17116/oftalma2017133149-54. [DOI] [PubMed] [Google Scholar]
- 5.Khan MA, Gupta A, Ahluwalia TS, Moulick PS, Gurunadh VS, Gupta S. A prospective interventional study of effect of accelerated orthokeratology on the corneal curvature and refraction among young adults with myopia. Med J Armed Forces India. 2016;72(2):125–130. doi: 10.1016/j.mjafi.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leo SW, Scientific Bureau of World Society of Paediatric Ophthalmology and Strabismus (WSPOS) Current approaches to myopia control. Curr Opin Ophthalmol. 2017;28(3):267–275. doi: 10.1097/ICU.0000000000000367. [DOI] [PubMed] [Google Scholar]
- 7.Cho P, Cheung SW. Retardation of myopia in Orthokeratology (ROMIO) study: a 2-year randomized clinical trial. Invest Ophthalmol Vis Sci. 2012;53(11):7077–7085. doi: 10.1167/iovs.12-10565. [DOI] [PubMed] [Google Scholar]
- 8.Li X, Friedman IB, Medow NB, Zhang C. Update on orthokeratology in managing progressive myopia in children: efficacy, mechanisms, and concerns. J Pediatr Ophthalmol Strabismus. 2017;54(3):142–148. doi: 10.3928/01913913-20170106-01. [DOI] [PubMed] [Google Scholar]
- 9.Yang X, Li Z, Zeng J. A review of the potential factors influencing myopia progression in children using orthokeratology. Asia Pac J Ophthalmol (Phila) 2016;5(6):429–433. doi: 10.1097/APO.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 10.Chen Z, Niu L, Xue F, Qu X, Zhou Z, Zhou X, Chu R. Impact of pupil diameter on axial growth in orthokeratology. Optom Vis Sci. 2012;89(11):1636–1640. doi: 10.1097/OPX.0b013e31826c1831. [DOI] [PubMed] [Google Scholar]
- 11.Wu C, Mao X, Lin H, Qu J. An investigation of the effects of wearing orthokeratology lenses on the magnitude of accommodative microfluctuations and accommodative lag. Chinese Journal of Optometry Ophthalmology and Visual science. 2013;15(2):75–78. [Google Scholar]
- 12.Zhu M, Feng H, Zhu J, Qu X. The impact of amplitude of accommodation on controlling the development of myopia in orthokeratology. Zhonghua Yan Ke Za Zhi. 2014;50(1):14–19. [PubMed] [Google Scholar]
- 13.Felipe-Marquez G, Nombela-Palomo M, Palomo-Álvarez C, Cacho I, Nieto-Bona A. Binocular function changes produced in response to overnight orthokeratology. Graefes Arch Clin Exp Ophthalmol. 2017;255(1):179–188. doi: 10.1007/s00417-016-3554-0. [DOI] [PubMed] [Google Scholar]
- 14.Hashemi H, Nabovati P, Khabazkhoob M, Yekta A, Emamian MH, Fotouhi A. Does Hofstetter's equation predict the real amplitude of accommodation in children? Clin Exp Optom. 2018;101(1):123–128. doi: 10.1111/cxo.12550. [DOI] [PubMed] [Google Scholar]
- 15.Han X, Xu D, Ge W, Wang Z, Li X, Liu W. A comparison of the effects of orthokeratology lens, medcall lens, and ordinary frame glasses on the accommodative response in myopic children. Eye Contact Lens. 2017 doi: 10.1097/ICL.0000000000000390. [DOI] [PubMed] [Google Scholar]
- 16.Ren Q, Yue H, Zhou Q. Effects of orthokeratology lenses on the magnitude of accommodative lag and accommodative convergence/accommodation. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2016;41(2):169–173. doi: 10.11817/j.issn.1672-7347.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Huang J, Qu X, Chen Z, Chu R. Comparison of accommodative lag in pre-adolescent myopes one year after wearing rigid gas permeable contact lenses, orthokeratology lenses or spectacles. Chinese Journal of Optometry Ophthalmology and Visual Science. 2010;12(1):33–36. [Google Scholar]
- 18.Queirós A, González-Méijome JM, Jorge J, Villa-Collar C, Gutiérrez AR. Peripheral refraction in myopic patients after orthokeratology. Optom Vis Sci. 2010;87(5):323–329. doi: 10.1097/OPX.0b013e3181d951f7. [DOI] [PubMed] [Google Scholar]
- 19.Gifford K, Gifford P, Hendicott PL, Schmid KL. Near binocular visual function in young adult orthokeratology versus soft contact lens wearers. Cont Lens Anterior Eye. 2017;40(3):184–189. doi: 10.1016/j.clae.2017.01.003. [DOI] [PubMed] [Google Scholar]
- 20.Tarrant J, Roorda A, Wildsoet CF. Determining the accommodative response from wavefront aberrations. J Vis. 2010;10(5):4. doi: 10.1167/10.5.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gifford P, Li M, Lu H, Miu J, Panjaya M, Swarbrick HA. Corneal versus ocular aberrations after overnight orthokeratology. Optom Vis Sci. 2013;90(5):439–447. doi: 10.1097/OPX.0b013e31828ec594. [DOI] [PubMed] [Google Scholar]
- 22.Thibos LN, Bradley A, Liu T, López-Gil N. Spherical aberration and the sign of defocus. Optom Vis Sci. 2013;90(11):1284–1291. doi: 10.1097/OPX.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 23.Hiraoka T, Kakita T, Okamoto F, Oshika T. Influence of ocular wavefront aberrations on axial length elongation in myopic children treated with overnight orthokeratology. Ophthalmology. 2015;122(1):93–100. doi: 10.1016/j.ophtha.2014.07.042. [DOI] [PubMed] [Google Scholar]