Abstract
Pancreatic cystic lesions (PCLs) are increasingly being identified because of the widespread use of high-resolution abdominal imaging. These cysts encompass a spectrum from malignant disease to benign lesions, and therefore, accurate diagnosis is crucial to determine the best management strategy, either surgical resection or surveillance. However, the current standard of diagnosis is not accurate enough due to limitations of imaging and tissue sampling techniques, which entail the risk of unnecessary burdensome surgery for benign lesions or missed opportunities of prophylactic surgery for potentially malignant PCLs. In the last decade, endoscopic innovations based on endoscopic ultrasonography (EUS) imaging have emerged, aiming to overcome the present limitations. These new EUS-based technologies are contrast harmonic EUS, needle-based confocal endomicroscopy, through-the-needle cystoscopy and through-the needle intracystic biopsy. Here, we present a comprehensive and critical review of these emerging endoscopic tools for the diagnosis of PCLs, with a special emphasis on feasibility, safety and diagnostic performance.
Keywords: Intraductal papillary mucinous neoplasm, Pancreatic cystic lesions, Endoscopic ultrasonography, Confocal endomicroscopy, Mucinous cystadenoma, Through-the-needle cystoscopy, Serous cystadenoma, Through-the-needle forceps biopsy, Contrast harmonic endoscopic ultrasonography
Core tip: This paper provides a focused update on emerging endoscopic technologies for improving the diagnosis and prediction of the malignant potential of pancreatic cystic lesions. Basic principles, diagnostic performance, safety and limitations are critically reviewed.
INTRODUCTION
Pancreatic cystic lesions (PCLs), initially thought to be rare, have become an incidental finding increasingly identified because of technological advances and the widespread use of high-resolution abdominal imaging. It is estimated that approximately 3% and 20% of patients undergoing abdominal computed tomography (CT) and magnetic resonance imaging (MRI), respectively, present a PCL[1-2]. Among neoplastic cysts, certain subtypes, basically mucinous cysts, entail a risk of present or future malignancy. Other neoplastic cysts, such as serous cystadenomas (SCAs), are considered benign cysts without potential of malignancy. These two types of neoplastic cysts are sometimes indistinguishable, and therefore, the awareness of possible malignant potential may lead physicians to refer these patients to surgical resection. Despite improvements in pancreatic surgery, considerable morbidity and mortality still occur in 18%-38% and 0.2%-2% of patients who undergo surgery because of PCLs[3-6]. Accurate assessment of malignant potential is therefore of the utmost importance to avoid unnecessary surgery for benign cysts while considering appropriate surveillance for low-risk lesions and surgical treatment for malignant and high-risk cysts.
The initial step of the diagnostic approach to PCLs usually relies on radiological imaging focusing on size and morphological features. Once a PCL has been identified, most commonly by CT, an MRI is recommended due to its higher ability to evaluate nodules and to depict a communication between the cyst and the main pancreatic duct. Owing to the frequent lack of specific radiological features of many PCLs, the overall accuracy of CT and MRI remains low, ranging from 23% to 93%[7-16]. Endoscopic ultrasonography (EUS) further characterizes PCLs and performs better than CT or MRI in assessing the morphology of small cysts and in depicting nodules in mucinous cysts, but EUS imaging alone also shows inadequate accuracy in the range of 40%-94%[17-23]. A major advantage of EUS is the ability to safely obtain cyst fluid for biochemical and cytological analysis. However, the scant cellularity of the cyst fluid accounts for the low diagnostic yield of cytology. Although the cyst fluid carcinoembryonic antigen (CEA) level has been proven to be more accurate than cytology or EUS morphology alone, the reported sensitivity of CEA and cytology for mucinous lesions in a recent meta-analysis do not exceed 63% and 54%, respectively[24].
All the above limitations have led to the recent updated International, AGA and European guidelines based on predictors of malignancy, which have been shown to be far from providing reliable differentiation between the various PCLs, and recommendations provided in these guidelines are based on low-grade evidence[25-27]. Moreover, the Fukuoka International Consensus Guideline, restricted their recommendations to branch-duct IPMNs that are diagnosed easily in a vast majority of cases (multiple cysts, communication with the main pancreatic duct)[28]. The Fukuoka guidelines were evaluated in a prospective study yielding a high negative predictive value (NPV) of 94% for malignancy but a low positive predictive value (PPV) of approximately 38%, frequently prompting unnecessary surgery[29]. Efforts to overcome current limitations have boosted the research in this area. Molecular analysis of DNA-based biomarkers in cyst fluid has been described with promising results[30]. Genomics, miRNA, proteomics and metabolomics in cyst fluid seem to be promising, but validation studies are pending. In addition to molecular testing, endoscopic innovations based on EUS imaging have emerged in the last decade and they are more easily available than the omics technologies though with a longer learning curve. Although not all of these EUS-based innovations have been validated, they warrant a thorough analysis to evaluate their diagnostic performance and potential impact as a part of the diagnostic workflow of PCLs.
In this article, we aim to review the evolving role of emergent EUS-based technologies-contrast harmonic enhanced imaging, needle-based confocal endomicroscopy, through-the-needle cystoscopy, and through-the-needle intracystic biopsy-in the clinical diagnosis of PCLs, with a critical focus on feasibility, safety and diagnostic performance. Novel approaches to cystic fluid analysis, such as omics technologies and other biomarkers, are beyond of the scope of this review.
A literature search was performed for all available studies concerning the EUS diagnosis of PCLs in PubMed and Embase databases. The following search domains (including closely related words) were used: “pancreatic cysts” in combination with “contrast harmonic EUS” or “contrast enhanced EUS” or “needle confocal endomicroscopy” or “cystoscopy” or “intracystic biopsy”. The search was limited to papers published in English until December 2017. Titles were then screened for suitability, and the full-text papers were retrieved. A hand-search of the references listed in the articles accessed was also performed to identify other relevant original studies. Both retrospective and prospective studies reporting data on the feasibility, diagnostic performance and safety of the above referred procedures in patients with PCLs were considered for inclusion. Indications, technical details, performance outcomes, impact on final diagnosis and management, complications and mortality were extracted and further discussed.
CONTRAST-HARMONIC ENHANCED ENDOSCOPIC ULTRASOUND
Because perfusion patterns on CT or MRI explorations allow the characterization of focal lesions, EUS has recently incorporated the use of ultrasound contrast agents (UCAs) to depict blood flow in small vessels. Available UCAs consist of microbubbles composed of an inert gas encapsulated by a shell[31]. Gases are compressible, and when exposed to an ultrasound wave, microbubbles alternatively compress under positive pressure and expand under negative pressure, producing a backscattered acoustic signal with harmonic components[31-32]. These harmonic components are higher than those obtained from tissue and may be selectively detected and reproduced on the ultrasound image for displaying the microvascularity pattern[31]. Not until recently, when new UCAs, broadband EUS transducers and contrast-specific software programs became available, was contrast harmonic EUS (CH-EUS) feasible for the first time, allowing the discrimination between tissue and contrast signals. Second-generation UCAs, which contain a soluble gas, unlike air-filled first-generation agents, are commonly used for CH-EUS. They have a resistant but more flexible and longer lasting shell, making possible the use of low acoustic power (a low mechanical index) and continuous real-time assessment[31-35].
Several steps must be followed to perform CH-EUS[31]. After fundamental B-mode exploration of the target area, a dual screen is displayed, simultaneously showing the CH-EUS image and the conventional B-mode image. Next, optimal parameters, notably, a low MI, should be selected on the ultrasound platform. The UCA is then injected intravenously slowly through a large-gauge intravenous catheter of 16G-18G in order to avoid breaking microbubbles. Finally, the venous catheter must be flushed with saline to clear out persistent microbubbles in the vein. After intravenous injection of microbubbles, it takes 10-20 s to observe the arrival of the contrast agent. The arterial phase lasts 30-45 s, during which the enhancement increases progressively. After the arterial phase, there is a progressive washout of the contrast, and the venous phase persists from 30 s to 120 s.
Clinical outcomes: Review of the literature
Among the 71 articles retrieved from PubMed and Embase databases using the terms “pancreatic cysts” and “contrast harmonic EUS”, only seven were suitable for further review[36-42]. All of the studies but one were retrospective, and the majority was devoted to the diagnosis of mural nodules and/or malignancy in intraductal pancreatic mucinous neoplasms (IPMNs). Only three articles addressed the issue of the differential diagnosis of PCLs. Selected articles are summarized in Table 1.
Table 1.
Contrast harmonic enhanced endoscopic ultrasound in pancreatic cystic lesions
| Authors | Study | n | Main outcomes | Complications |
| Yamashita et al[39], 2013 | P | 17 | Differential diagnosis between mural nodules and mucus clots: CH-EUS: Sen 100%, Spe 80%, PPV 92%, NPV 100%, A 94% CT and Doppler-EUS: Sen 41% and 0% respectively | 0 |
| Hocke et al[36], 2014 | R | 125 | Differential diagnosis between non-neoplastic cysts and PCNs. Hyperenhancement: 100% PCNs Hypoenhancement: 94% non-neoplastic cysts (PCs and dysontogenic cysts) CH-EUS superior to EUS in differential diagnosis between PCNs and non-neoplastic cysts (aP < 0.001) | 0 |
| Harima et al[41], 2015 | R | 30 | Performance for diagnosing mural nodules CT: Sen 71%, Spe 100%, PPV 100%, NPV 90%, A 92% EUS: Sen 72%, Spe 61%, PPV 50%, NPV 100%, A 72% CH-EUS: Sen 100%, Spe 97%, PPV 93%, NPV 100%, A 98% | 0 |
| Fujita et al[40], 2016 | R | 50 | Sensitivity for diagnosing mural nodules: CT: 86% vs MRI 71% vs EUS 100% EUS was not able to distinguish mural nodules from mucus clots CH-EUS correctly differentiated mural nodules from mucus clots in all cases | 0 |
| Fusaroli et al[37], 2016 | R | 76 | Differential diagnosis between non-neoplastic cysts and PCNs and between benign and malignant cysts. Hyperenhancement: 86% SCAs and 89% mucinous cysts (P = ns) Hypoenhancement: 90% PCs (bP < 0.000004 vs SCAs and cP < 0.000005 vs mucinous cysts) Hyperenhanced solid components : 100% malignant cysts Non- hype-enhanced solid components: 100% benign cysts | 0 |
| Kamata et al[38], 2016 | R | 70 | Mural nodule as a sign of mucinous cyst EUS vs CH-EUS: Sen 85% vs 79%, Spe 46% vs 96%, A 73% vs 84% (P = 0.057) Mural nodule as a sign of malignancy EUS vs CH-EUS: Sen 97% vs 97%, Spe 40% vs 75%, A 64% vs 84% (dP = 0.0001) | 0 |
| Yamamoto et al[42], 2016 | R | 30 | Quantitative CH-EUS in IPMNs Echo intensity change and echo intensity reduction rate, and nodule/parenchyma contrast ratio significantly higher in HGD/invasive carcinoma (eP < 0.05) Microvessel density in mural nodule Significantly higher in HGD/invasive carcinoma (fP < 0.002) Significant correlation between echo intensity change and microvessel density (gP < 0.001) | 0 |
P: Prospective; R: Retrospective; CT: Computed tomography; MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography; CH-EUS: Contrast harmonic endoscopic ultrasonography; Sen: Sensitivity; Spe: Specificity; PPV: Positive predictive value; NPV: Negative predictive value; A: Accuracy; PCNs: Pancreatic cystic neoplasms; IPMN: Intraductal papillary mucinous neoplasm; HGD: High grade dysplasia.
Hocke et al[36] performed CH-EUS in 125 patients with PCLs. Contrast enhancement of cyst walls, septa and nodules was observed in all PCNs, including mucinous cysts, cystic adenocarcinomas, SCAs and cystic neuroendocrine neoplasms (NENs), but in only 6% of nonneoplastic cystic lesions (PCs and dysontogenic cysts). Further supporting these results, in another study by Fusaroli et al[37], of 76 patients with PCLs, most SCAs were hyper-enhanced during CH-EUS, without a significant difference (86% vs 89%, P = NS), when in fact, 90% of pseudocysts showed hypoenhancement (P = 0.000004 vs serous cysts and P = 0.000005 vs mucinous cysts). In addition, Kamata et al[38] reported that CH-EUS did not add any advantage to EUS for differentiating mucinous and nonmucinous cysts when the presence of mural nodules was considered a sign of mucinous cysts (sensitivity, 79% vs 85%; specificity, 96% vs 46%; accuracy, 73% vs 84%, respectively, P = 0.057).
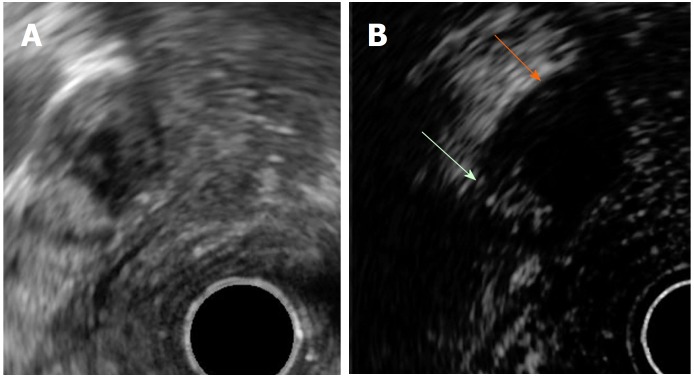
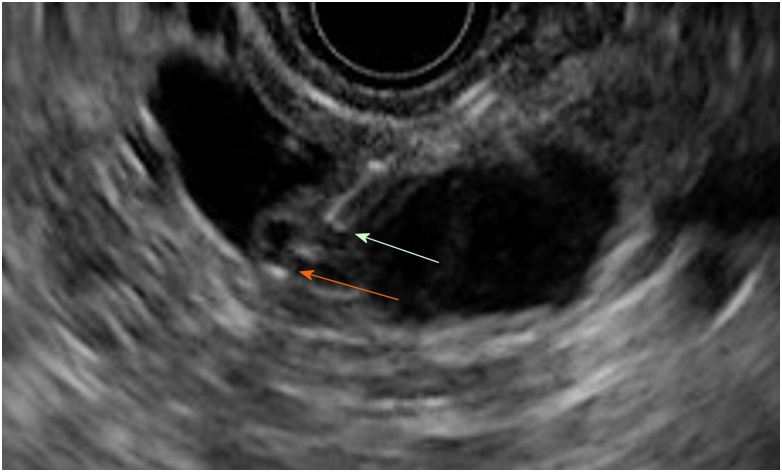
Yamashita et al[39] used CT, color Doppler EUS and CH-EUS to prospectively study 17 patients with mural nodules in branch duct type IPMN (BD-IPMN) detected by EUS before being referred for surgery. After pathological analysis, 75% of mural nodules corresponded to adenocarcinomas, and 25% corresponded to adenomas. Compared with surgical specimens, CH-EUS depicted vascularity in all pathologically confirmed nodules and in one case with mucous clots (sensitivity, 100%; specificity, 80%; PPV, 92%; NPV, 100%; and accuracy, 94%). Moreover, the sensitivity of CT and color Doppler-EUS was only 41% and 0%, respectively. Comparable results were found in later studies. Fujita et al[40] observed that CT, MRI, and EUS detected mural nodules histologically confirmed in 86%, 71% and 100% of cases. Although EUS was highly sensitive, it was not able to distinguish mucous clots from mural nodules that were correctly classified in all cases after assessing the vascular pattern by CH-EUS (Figure 1). CH-EUS was also shown to be more accurate than CT or EUS in diagnosing mural nodules in the study by Harima et al[41] (accuracy of 98%, 72% and 92%, respectively).
Figure 1.
Mural nodule and mucus in branch duct type intraductal pancreatic mucinous neoplasms. A: EUS B mode image. B: Contrast harmonic EUS image. Microbubbles in a mural nodule (green arrow). No bubbles in a mucus clot (orange arrow). EUS: Endoscopic ultrasonography.
Fusaroli et al[37] observed that all hyper-enhanced solid components during CH-EUS turned out to be malignant, whereas nonenhanced ones were either mucous clots or internal debris. Nevertheless, other authors found it difficult to discriminate between adenomas or adenocarcinomas in BD-IPMN based on the vascular pattern. Only one study evaluated the accuracy of quantitative CH-EUS for differentiating between low-grade dysplasia (LGD) or intermediate-grade dysplasia and high-grade dysplasia (HGD) or invasive carcinoma. In this study, Yamamoto et al[42] retrospectively analyzed the time-intensity curve in 30 patients with resected IPMNs who underwent CH-EUS. The analyzed parameters were the echo intensity change and the echo intensity reduction rate of the mural nodule and the nodule/parenchyma contrast ratio. All of the parameters were significantly higher in the HGD/invasive group (P < 0.05), with the nodule/parenchyma contrast ratio being the most accurate parameter (accuracy, 93%). Moreover, a positive linear correlation was observed between the echo intensity change in the mural nodule and the microvessel density in pathologic specimens (r = 0.803, P < 0.001).
No mortality or CH-EUS-related adverse events were reported in any study.
NEEDLE-BASED CONFOCAL LASER ENDOMICROSCOPY
Needle-based confocal laser endomicroscopy (nCLE) is an emergent endoscopic modality that enables imaging of a target tissue at a subcellular level of resolution, providing real-time in vivo optical biopsy. For CLE imaging, a low-power laser is used to illuminate the tissue. The laser beam is focused on a plane of interest, and the reflected light from the tissue is filtered and transformed into an electrical signal by a detection system and finally translated into grayscale images by a computer system[43,44]. The final result consists of images with very high spatial resolution and magnification of the focal plane examined within the tissue. Because confocal imaging relies on reflected fluorescent light, intravenous injection of a fluorescent dye, most commonly sodium fluorescein, is required. Fluorescein acts as a contrast agent highlighting blood vessels and tissue architecture[43-46].
Recent advances have allowed the incorporation of CLE technology into a miniprobe of 0.85 mm (AQ-Flex) that can be passed through a 19-gauge (19G) EUS needle. This probe is provided with 10.000 optical fibers and has a field of view of 325 μm, 3.5 μm of lateral resolution and 40-70 μm of confocal depth[46].
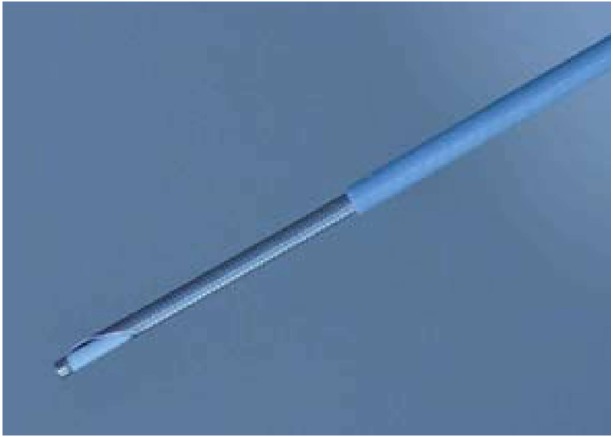
Before starting the procedure, a 19G EUS needle is preloaded with the AQ-Flex probe that should be inserted until 2 mm of the probe is positioned beyond the needle tip (Figure 2). At this moment, the probe is fixed to the inlet of the needle channel by a locking system. After identifying the cyst, a single pass with the preloaded 19G EUS needle is performed, and the needle is advanced under EUS guidance until the needle tip contacts the cyst wall. Immediately after, 2.5-5 mL of 10% fluorescein is injected; nCLE imaging begins, during which gentle apposition of the probe to the cyst wall is pursued. The elevator, endoscope dials and torquing are useful for imaging in a fanning technique[43]. Because images are obtained at a rate of 12 frames/s, video-recording is always performed for 2-5 min and further reviewed with a dedicated software program. At the end of the procedure, the probe is withdrawn, and the cyst fluid is aspirated as per standard practice. Antibiotic prophylaxis is systematically administered[47].
Figure 2.
Needle-based confocal laser endomicroscopy probe in a 19G needle.
Clinical outcomes: Review of the literature
A literature search in PubMed and Embase databases identified 24 articles reporting on nCLE in PCLs. Only 11 of these articles were deemed eligible and consisted of 7 prospective and 4 retrospective studies (Table 2)[48-58]. Most of them were focused on feasibility, safety and performance in differentiating mucinous from nonmucinous cysts or in the differential diagnosis among the several types of PCLs. Three studies aimed to externally validate the nCLE criteria, and one study performed an ex vivo validation of the in vivo nCLE criteria.
Table 2.
Needle-based confocal laser endomicroscopy in pancreatic cystic lesions
| Authors | Study | n | Main outcomes | Complications |
| Konda et al[48], 2011 | P | 16 | 94% Technical success (feasibility study) | 12% post-procedure pancreatitis |
| Konda et al[49], 2013 | P | 66 | Stage 1: Description of visualized structures (n = 26) with histological correlation Stage 2: Performance assessment of defined criteria (n = 31): Villous pattern: Sen 59%, Spe 100%, PPV 100%, NPV 50%, A 71% for PCNs Significant association with PCNs (aP = 0.004) | 3% post-procedure pancreatitis 4.5% intracystic self-limited bleeding |
| Nakai et al[50], 2015 | P | 30 | Villous pattern in 18 patients with highly certain diagnosis: Sen 80%, Spe 100%, PPV 100%, NPV 80%, A 89% for mucinous cysts Significant association with mucinous cysts (bP = 0.001) | 7% post-procedure (cystoscopy followed by nCLE) pancreatitis |
| Napoléon et al[51], 2015 | P | 31 | Superficial vascular network: Sen 69%, Spe 100%, PPV 100%, NPV 82%, A 87% for SCAs | 3% post-procedure pancreatitis |
| Napoléon et al[52], 2016 | R | 31 | Step 1: Description of nCLE patterns for mucinous cysts, PCs and cystic NENs with histological correlation Step 2: Retrospective external validation of nCLE criteria Accuracy 94% for mucinous cysts (90% IPMN - 90% MCA) - 87% SCA - 87% PCs Substantial global IOA: Perfect PC, almost perfect SCA, moderate IPMN, fair MCA | |
| Kadayifci et al[53], 2017 | P | 20 | nCLE performance for mucinous cysts: Sen 66% -Spe 100% -A 80% | 0 complications |
| Krishna et al[54], 2017 | P | 10 | Reproducibility of the in vivo nCLE criteria in ex vivo specimens | |
| Napoléon et al[55], in press | P | 209 | Diagnostic yield 91% in 78 patients with non-communicating cysts and pathological diagnosis: Sen 95%, Spe 100% - PPV 100% - NPV 98% - A 99% for SCAs Sen 95%, Spe 100% - PPV 100% - NPV 94% - A 97% for mucinous cysts Sen 100%, Spe 95% - PPV 70% - NPV 100% - A 96% for NENs Sen 96%, Spe 95% - PPV 98% - NPV 91% - A R96% for premalignant cysts | 1.3% post-procedure pancreatitis |
| Karia et al[56], 2016 | R | 15 | IOA poor to fair for all nCLE variables | |
| Krishna et al[57], 2016 | R | 49 | nCLE performance on 26 patients with definitive diagnosis (23 with pathological diagnosis): Sen 94%, Spe 82% - PPV 88% - NPV 92% - A 89% for mucinous cysts IOA and IOR: Substantial for all nCLE criteria | 6.1% post-procedure pancreatitis |
| Krishna et al[58], 2017 | R | 29 | nCLE performance on 29 patients with definitive diagnosis (23 with pathological diagnosis): Sen 95%, Spe 94% - A 95% for mucinous cysts Sen 99%, Spe 98% - A 98% for SCAs Sen 99%, Spe 98% - A 98% for NENs IOA and IOR: Almost perfect for mucinous cysts and SCAs |
P: Prospective; R: Retrospective; Sen: Sensitivity; Spe: Specificity; PPV: Positive predictive value; NPV: Negative predictive value; A: Accuracy; PCNs: Pancreatic cystic neoplasms; PC: Pseudocyst; MCA: Mucinous cystadenoma; SCA: Serous cystadenoma; IPMN: Intraductal papillary mucinous neoplasm; NENs: Neuroendocrine neoplasm; IOA: Interobserver agreement; IOR: Intraobserver reliability.
The first series was reported in 2011 by Konda et al[48] and was a feasibility study of 16 cysts and 2 solid masses of the pancreas. The nCLE procedure was feasible in 15 of 16 cysts, although the technical challenges described in 6 of them were related to the transduodenal approach, the post loading technique (the insertion of the CLE probe after positioning the EUS needle inside the lesion) and the longer length of the metallic tip at the distal end of the probe. Complications occurred in two patients, both of whom developed pancreatitis requiring hospitalization. This study was followed by a larger multicenter study (in vivo nCLE Study in the Pancreas with Endosonography of Cystic Tumors, INSPECT) that was reported by the same group and that aimed to evaluate the diagnostic potential and safety of nCLE in the differential diagnosis of PCLs in 66 patients[49]. A consensus description of visualized structures on 26 patients was achieved, and the correlation between histology and nCLE was investigated during the first stage of the study. Then, the performance of nCLE criteria to identify PCNs, including mucinous cystadenoma (MCA), IPMN or adenocarcinoma, was assessed in 31 additional patients. The presence of villous structures was highly specific (100%) but provided low sensitivity, at 59%, and it was the only specific finding having a significant association with PCNs (P = 0.004). Post procedure pancreatitis occurred in 3% of cases: one patient experienced transient abdominal pain, and three cases of intracystic bleeding were observed and spontaneously solved.
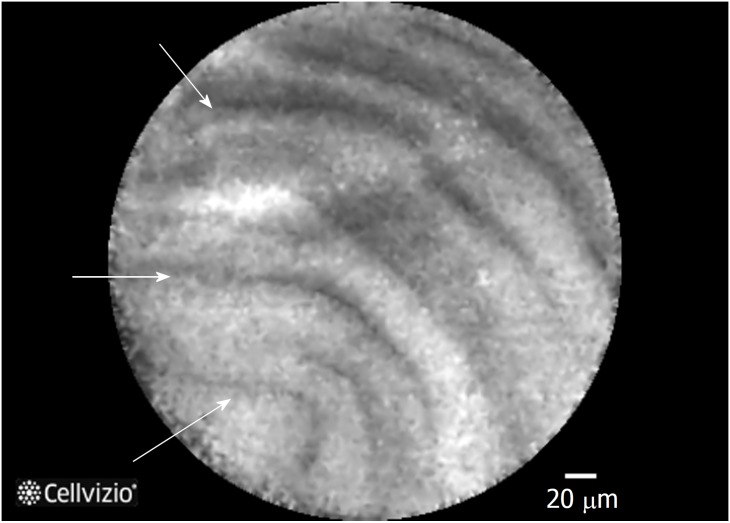
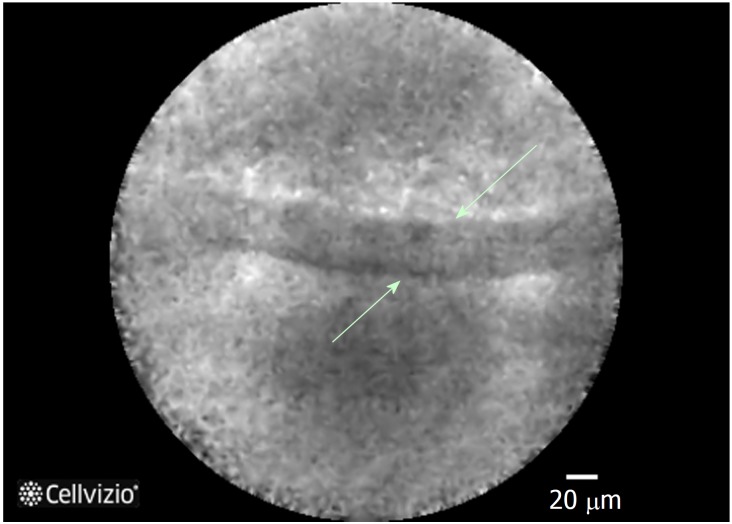
The DETECT trial (Diagnosis of Pancreatic Cysts: Endoscopic Ultrasound, Through-the-Needle Confocal Laser Endomicroscopy and Cystoscopy Trial) was designed to evaluate the diagnostic yield of cystoscopy followed by nCLE in 30 patients[50]. A highly certain diagnosis was possible in 18 of these patients based on the clinical presentation, other image findings, fluid analysis and cytology. In these patients, a papillary projection (Figure 3) and/or a dark ring on nCLE, corresponding to the villous pattern previously reported by Konda, was associated with mucinous cysts (P = 0.001) with 80% sensitivity, 100% specificity, 100% PPV, 80% NPV and 89% accuracy. Two patients (7%) developed post procedure pancreatitis.
Figure 3.
Needle-based confocal laser endomicroscopy image of an intraductal pancreatic mucinous neoplasms displaying multiple papillary projections.
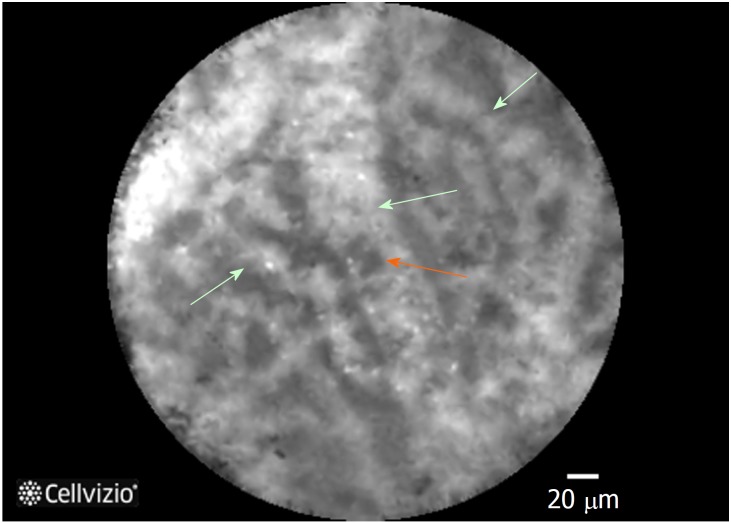
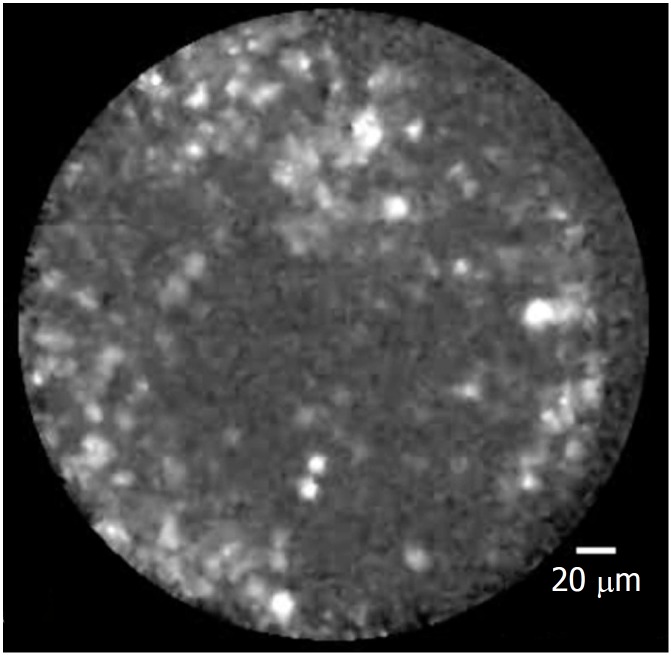
After the above initial experiences, Napoléon and colleagues described new nCLE criteria based on histological correlation in two consecutive studies[51-52]. In the first one, a criterion for in vivo diagnosis of SCA was defined and consensually identified as a superficial vascular network (Figure 4). The presence of small and regular structures circulating inside the opacified channels during nCLE suggested the vascular nature of these channels, which was confirmed by histological assessment of surgical specimens (Figure 5). This vascular network was demonstrated to be at a superficial depth of 50-70 μm and, therefore, at the reach of the nCLE probe. Moreover, SCA was the only PCL that featured this pattern among 31 patients with PCLs of unknown diagnosis. The sensitivity, specificity, PPV, NPV and accuracy of this criterion for diagnosing SCA were 69%, 100%, 100%, 82% and 87%, respectively. Only one patient suffered mild acute pancreatitis (3%). In a second study (CONTACT 1), the same authors identified three other nCLE criteria that included a thick gray line for mucinous neoplasms (Figure 6), a field of bright particles for PCs (Figure 7) and black neoplastic clusters with white fibrous areas for NENs. In this case, the histological correlation was the epithelial border, a mix of inflammatory cells and neoplastic cell proliferation with several forms of architectural organization respectively. In the retrospective validation, four external and blinded reviewers evaluated the diagnostic performance of these criteria. A conclusive diagnosis was achieved in 23 of 31 patients (74%). Overall, the accuracy of nCLE criteria was 94% for mucinous cysts, 87% for SCA and 87% for PC. Trends toward high specificity were also shown (> 90% for mucinous cysts and 100% for nonmucinous cysts). NENs were excluded from the external validation due to the small number in this series (n = 2). More recently, Krishna et al[54] have further confirmed the reproducibility of the in vivo nCLE criteria in ex vivo specimens of 10 patients with surgically resected PCLs.
Figure 4.
Needle-based confocal laser endomicroscopy image of the superficial vascular network pattern of a serous cystadenoma. Multiple interconnected vessels (green arrows). Red cells inside displayed as black structures (orange arrow).
Figure 5.
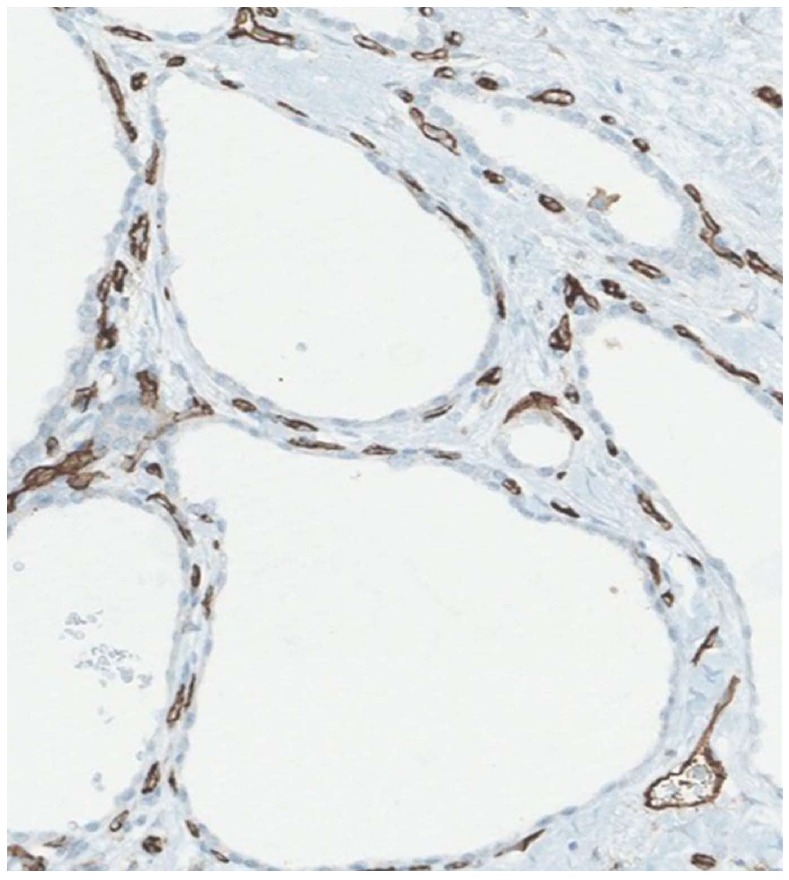
Staining with a vascular marker of serous cystadenomas histological specimen. Capillary necklace with subepithelial vessels showed in brown.
Figure 6.
Epithelial border image in a mucinous cystadenoma at needle-based confocal laser endomicroscopy.
Figure 7.
Heterogeneous sized grey and white particles in a pseudocyst at needle-based confocal laser endomicroscopy.
To overcome the limitations of the reduced number of patients and the lack of pathological confirmation in previous series, Napoléon et al[55] designed a larger multicenter and prospective study (CONTACT 2) whose results are now available (submitted). Among 209 enrolled patients with a noncommunicating solitary cyst, 78 patients with a final diagnosis proven by surgical histopathology or cytopathological analysis of cyst fluid by EUS fine needle aspiration (EUS-FNA) were included in the final results. The overall diagnostic yield of nCLE was 91%, and the sensitivity and specificity for the main types of PCLs were higher than 95%. Perfect specificity (100%) was observed for diagnosing SCA and premalignant mucinous cysts. Furthermore, the nCLE area under the curve was significantly higher than that of CEA dosage for differentiating mucinous from nonmucinous cysts (P < 0.01) and higher than that of EUS morphology in differentiating between premalignant and benign PCLs (P < 0.05). However, nCLE criteria were not highly specific for NENs and PCs. NEN criteria were also observed in one cystic solid pseudopapillary neoplasia (CSPPN), one cystic lymphoma and 1 PC. Additionally, one mucinous lesion and one SCA exhibited PC criteria. Acute pancreatitis occurred only in 1.3% of patients. Although the impact of nCLE on patient management was not evaluated, it is noteworthy that in 29% of patients with a previous inconclusive EUS-FNA, nCLE was conclusive in 91% of cases and 100% accurate.
The first reports on interobserver agreement (IOA) yielded diverging results[51,56]. In the first one (CONTACT 1), four external reviewers assessed the IOA of the nCLE criteria in 31 cases[51]. The diagnostic accuracy for mucinous cysts was 94%, and the global IOA was rated as substantial (k = 0.72, 95%CI: 0.52-0.87). A later validation study reported low diagnostic accuracy for the type of PCL (46%), with an IOA ranging from poor to fair for all nCLE variables[56]. However, careful interpretation of these results is advised due to limitations such as poor image quality and short duration of video capture, which may have accounted for the poor results, and other methodological issues such as the lack of intraobserver reliability and few patients with a histological gold-standard diagnosis. More recently, two other studies aimed to validate nCLE criteria. One investigation consisted of a retrospective analysis at a single center[57,58]. nCLE videos from 26 patients (23 with pathological diagnosis) were reviewed by 6 blinded nCLE-naïve observers[57]. Substantial IOA and IOR were achieved for differentiating mucinous from nonmucinous cysts (k = 0.67, 95%CI: 0.57-0.77 and k = 0.78 ± 0.13, respectively) and for detecting all nCLE criteria. These results were further corroborated by an international external interobserver and intraobserver study[58]. In 29 patients, the overall accuracy of nCLE for the diagnosis of mucinous cysts was 95%, with an almost perfect IOA and IOR among six expert endosonographers with nCLE experience (k = 0.81, 95%CI: 0.71-0.90 and k = 0.86 ± 0.11, respectively). Furthermore, nCLE was 98% accurate in diagnosing SCA and the IOA and IOR for recognizing the fern pattern (previously defined as superficial vascular network) were also almost perfect (k = 0.83, 95%CI: 0.73-0.92 and k = 0.85 ± 0.11, respectively).
THROUGH-THE-NEEDLE CYSTOSCOPY
Through-the-needle cystoscopy is a procedure that allows direct assessment of the cyst content as well as the inner cyst wall by means of single-operator cholangioscopy fiberoptic probe (Spyglass®, Boston Scientific, Natick, Mass, United States). The probe has 6000-pixel optic bundles, a 300 cm working length and a diameter of 0.77 mm. It provides a 70-degree field of view and has a 2-7 mm focal length[43,50]. The cystic cavity is accessed under EUS guidance with a 19G EUS needle. Before starting the procedure, the needle stylet is removed, and the fiberoptic probe is preloaded through the 19G needle and prefitted with the advancement of the probe 2 mm beyond the needle tip. Then, the probe is withdrawn 2-3 mm inside the needle, and once inside the cyst, the probe is advanced again to the prefitted position. Prophylactic antibiotics are always given, and cystoscopy images may be recorded for further review[50].
Clinical outcomes: Review of the literature
Of the 8 references retrieved, only 3 suitable articles were identified[50,59-60]. The first one reported on two patients who underwent through-the-needle cystoscopy followed by biliary forceps biopsy[59]. In both cases, it was possible to rule out a pseudocyst because a flat normal mucosa was visualized lining the inner cyst wall. In addition, cystoscopy enabled a better delineation of mural nodules and targeted biopsies of the selected suspicious areas. Severe acute pancreatitis occurred in one patient one month after the procedure. It is not possible to rule out a delayed procedure-related complication, although very unlikely.
In the prospective DETECT study, Nakai et al[50] performed through-the needle-cystoscopy followed by nCLE in 30 patients. The cyst content was evaluated for clarity, the presence of mucin or debris, and the smoothness, nodularity and vascularity of the cyst walls were assessed. The median image time of cystoscopy was 4 min, and 33% of the images were rated as fair or poor. The mucinous content was described as viscous and cloudy fluid. Typical findings and their clinical correlations were finger-like projections and a mucin cloud in IPMNs, smooth cyst walls with cloudy fluid in MCNs, and smooth cyst walls with prominent regular vessels in SCAs. However, the only significant association in 18 high-certainty diagnoses was observed between mucin on cystoscopy and mucinous cysts (P = 0.0004), with 90% sensitivity, 100% specificity, 100% PPV, 100% NPV and 94% accuracy. However, finger-like projections were identified in only two of the ten high-certainty mucinous lesions. When cystoscopy and nCLE were combined, the sensitivity increased from 90% to 100%. Post procedure pancreatitis was reported twice.
In a retrospective study published last year, Chai et al[60] performed through-the-needle cystoscopy in 43 patients. Based on the blood vessel distribution, the presence of partitions or ridge-like structures and the presence of papilla-like structures, the characteristic findings of different PCLs were defined and then validated by surgical pathology, FNA or fluid cytology. The authors concluded that a tree-like branching pattern of blood vessels may suggest the diagnosis of SCA (specificity, 91%; sensitivity, 69%) and that intracystic papilla-like structures may be characteristic of mucinous cysts (specificity, 92%; sensitivity, 22%). No pancreatitis was observed, and only two patients presented mild abdominal post procedure pain.
THROUGH-THE-NEEDLE FORCEPS BIOPSY
The low sensitivity of EUS-FNA cytology because of relatively acellular samples makes appealing the possibility to obtain biopsies. The design of minibiopsy forceps has led to the development of a new EUS-FNA tissue acquisition technique. Moray® micro forceps (US Endoscopy, Ohio, United States) were designed for use in EUS procedures to enhance sampling from lesions that can occur within and outside the gastrointestinal tract, leading to a more definitive diagnosis (Figure 8). These forceps are 230 cm in length and have serrated jaws (jaw opening of 4.3 mm) and a spring sheath 0.8 mm in diameter, allowing use through a 19G EUS needle[43,61].
Figure 8.

Moray forceps.
Clinical outcomes: Review of the literature
No formal study was retrieved after searching PubMed and Embase for “pancreatic cyst” and “intracystic biopsy”. Only two pilot studies reporting on 2 cases each and four additional case reports were identified[59,61-65].
Through-the-needle intracystic biopsy was first described by Aparicio et al[59] in two patients. They used 0.8 mm endoscopic retrograde cholangiopancreatography biopsy forces followed by a 3-4 min observation with a fiberoptic probe to rule out immediate bleeding. In both cases, a mucinous-like cylindric epithelium without cellular atypia was observed. As stated above, one patient presented severe acute pancreatitis one month later. After this preliminary experience, six more cases were reported to undergo intracystic biopsy, enabling the correct diagnosis of 5 mucinous cysts (one of them with mild dysplasia) and one benign lymphoepithelial cyst without any complication[61-65].
DISCUSSION
PCLs remain a diagnostic and therapeutic challenge to clinicians. Several issues remain to be solved, notably, how to improve diagnosis and better predict malignant behavior. It has been reported that 36% of SCAs are treated with unnecessary surgery because of an uncertain diagnosis[66]. In the attempt to cover this need, several EUS-based tools have emerged recently and some experience is now available using these technologies in the diagnosis of PCLs.
On the grounds that CH-EUS has been proved to be accurate for the differential diagnosis of solid pancreatic masses, it was hypothesized that CH-EUS might also be helpful in PCLs, and some experience has been reported in the last five years[67-70]. Due to its high spatial resolution, CH-EUS may define the inner structure of cysts by depicting small septa or mural nodules that become echogenic during CH-EUS, whereas the intracystic content remains invisible (Figure 9). This modality may assist not only in the differential diagnosis but also in identifying malignancy risk features.
Figure 9.
Moray forceps inside a cyst. Green arrow: The tip of the 19G needle. Orange arrow: The tip of the Moray forceps grasping the cyst wall.
Current evidence suggests that CH-EUS is highly accurate for distinguishing nonneoplastic cysts (PCs and dysontogenic cysts) from neoplastic cysts because the former do not exhibit cystic wall vascularization. This feature prevents pointless and onerous surgery in this benign setting. However, a different scenario is observed among different neoplastic cysts whose biological behavior may be significantly different and where misinterpretations are common in CH-EUS. Benign SCAs, the most common nonmucinous cystic neoplasms, and potentially malignant mucinous cysts show undistinctive features on CH-EUS. Consequently CH-EUS cannot be used for the differential diagnosis of neoplastic cysts.
The presence of mural nodules is considered in the international consensus guidelines on IPMN management as a high-risk stigma and strongly supports surgical resection. Mural nodules may sometimes be too small for detection by CT or MRI. The high spatial resolution of EUS enables better identification in these cases. However, the performance of EUS is not enough to discriminate between mural nodules or mucous clots. Hyperenhancement of solid components during CH-EUS may differentiate mural nodules from mucous clots or debris. This step is essential to avoid unnecessary surgery and is included in the last guidelines[25]. Nodules in BD-IPMNs include not only malignant nodules but also benign adenomas that might be followed without surgery, but the preoperative differentiation between them does not seem possible with qualitative CH-EUS. Angiogenesis plays a key role in tumor growth and progression; in fact, neovascularization was reported to be crucial in the tumorigenesis of invasive IPMNs with a progressive increase in microvessel density from benign to malignant tissue[71]. According to this observation, preliminary experience with quantitative CH-EUS suggests that the analysis of echo intensity changes during CH-EUS may be an accurate method to discriminate between low/intermediate-grade dysplasia and high-grade dysplasia/invasive carcinoma. Further trials are necessary to confirm this interest.
When it comes to safety, CH-EUS exhibits an excellent safety profile with no adverse events in series reporting on PCLs. UCAs are the sole factor adding risk to conventional EUS. Concerns were raised after a study reporting on UCAs used for stress echocardiography, where 4 deaths and 190 serious adverse events were observed and associated with the use of UCAs[72]. Consequently, the Food and Drug Administration issued a black box warning regarding the use of UCAs in several pathologic cardiorespiratory states. Later experience in large cohorts of patients has shown that the rate of UCA-related serious adverse events is lower than 0.01%, with anaphylactoid reactions occurring in 1/10.000 cases[73-74].
More recent evidence confirms that nCLE is feasible during EUS-FNA and allows in vivo diagnosis of PCLs with high accuracy; nCLE criteria have been defined for IPMN, MCA, SCA, PC and cystic NEN with a proven histopathological correlation. Unlike CH-EUS, a perfect specificity of 100% has been confirmed with nCLE for benign SCA and for mucinous lesions. The superficial vascular network is exclusive to SCAs, allowing SCA diagnosis with high confidence, therefore preventing unnecessary surgical resection. Sensitivity of this pattern, although high, is not perfect, and epithelium denudation may account for the lack of a vascular pattern in oligocystic SCA. Specificity is also perfect for the overall group of mucinous lesions, but when they are further classified as either IPMN or MCA, the specific findings of papillae or epithelial borders, respectively, may both be present. Other times, papillae or epithelial borders cannot be visualized, and the explanation is the nonuniform distribution of papillae throughout the epithelium of IPMNs or modifications induced by inflammation in some MCAs. These inflammatory changes are also the reason why a field of bright, gray and black particles is not specific for PCs and may be found in other cystic tumors following infection or bleeding. Finally, the presence of dark spots of cell aggregates surrounded by gray areas of fibrosis and vessels, initially attributed to NENs, is not specific and may be present in other premalignant lesions, such as CSPPNs. However, due to the similar premalignant nature, the impact on clinical management of misdiagnosis between NENs and CSPPNs or between IPMNs and MCAs is of little importance.
The major concern related to nCLE is the risk of acute pancreatitis, which has ranged from 1.3% in the largest and most recent study to 12% in the first feasibility study. The use of Spyglass® (Boston Scientific, Natick, Mass, United States) for cystoscopy may also explain the second highest rate of pancreatitis in the DETECT study[50]. The average rate from the rest of the studies is 2.7%, which is comparable with that of the conventional EUS-FNA procedure[75]. Only one series reported intracystic bleeding in 3 patients (4.5%); however, no intervention was required, and they were solved spontaneously. Several factors that add to the risk of complications have been suggested, such as needle size, duration of the procedure and abrasion of the cyst lining with the needle tip. Some tips have been suggested during nCLE to maximize the procedure safety. The interposition of the main pancreatic duct should be avoided when selecting the puncture site to lower the risk of acute pancreatitis. Once inside the cyst, limited brushing of the cyst wall is recommended to avoid cystic bleeding and pancreatitis; instead, it is preferred to perform consecutive apposition between the probe and the cyst wall. Finally, the exploration should be stopped as soon as nCLE criteria are met, or after 6 min if no specific criteria are found, to minimize the risk of adverse events[43]. No study reported adverse events related to the injection of fluorescein, but severe allergic reactions are possible, although very uncommon (1/222000)[76]. Minor side effects, such as nausea, vomiting, mild epigastric pain, transient hypotension, injection site erythema or diffuse rash, have been reported in 1.4% of cases[77]. The learning curve for nCLE seems to have an important effect on the pancreatitis rate since one study reported three acute-pancreatitis cases among the first 25 patients and none in the successive 34 patients[58]. Technical challenges reported in initial feasibility studies are now overcome, and several tips have been suggested to avoid them (preloading of the nCLE probe, use of the most flexible needle). However, other limitations remain to be solved. The most important one is the limited surface of the cystic wall that is accessible to be scanned. Exploration is feasible over the area in front of the needle tip but less than 50% of the cystic surface is likely to be visualized. The second argued limitation is the high cost of the probe, which is considered a limiting step to implementing nCLE technology in routine practice. Nevertheless, a health economic evaluation carried out in France demonstrated that nCLE resulted in a reduction of 23% of surgical interventions[78]. This finding translated into a reduction in clinical costs of 13% in the public sector and 14% in the private sector. The improved diagnostic accuracy of nCLE reduces the number of false positives and false negatives, avoiding unnecessary surgical interventions and lifelong surveillance for benign cysts.
The heterogeneous distribution of neoplastic tissue in PCLs makes it reasonable to attempt to directly explore the inner cyst walls. Limited experience with through-the-needle cystoscopy has demonstrated the feasibility for direct visualization of cyst walls and has suggested that it may help to target biopsies to suspicious areas. Patterns at cystoscopy have been proposed for SCAs, MCNs and IPMNs but have not been validated yet. Like for nCLE, the main complication is acute pancreatitis, and therefore, limiting the time inside the cyst is strongly recommended. The greatest interest seems to be the ability to detect mucin clots that have a typical appearance on cystoscopy. Nevertheless, the performance of cystoscopy was not higher than the string test that is more simple and free of cost[50]. Beside the cost of the fiberoptic system, other limitations of cystoscopy in reported studies are mainly related to the suboptimal quality of images. Therefore, the real place of cystoscopy need to be established.
Through-the-needle intracystic biopsy has been suggested to be a feasible technique for tissue acquisition in one series and several case reports. It allows histological diagnosis including the grade of dysplasia, although the retrieved samples are small. However, the processing of the samples is not always easy. Because of the small-sized specimens, they sometimes disintegrate during fixation in formalin. In addition, lesions such as mural nodules may not be targetable by the stiff 19G EUS-FNA, especially those located in the uncinate process. Finally, concerns remain about the risk of bleeding following through-the-needle forceps biopsy, similarly to brush cytology, even if no cases of bleeding have been reported. Formal studies in larger series are required to validate the results of this new technique and to confirm its safety.
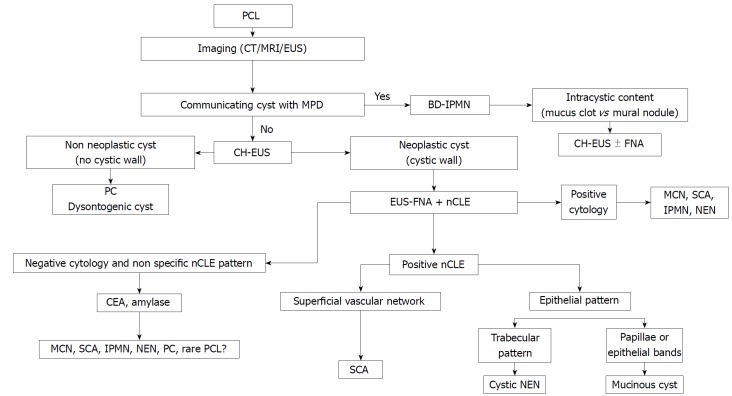
In summary, CH-EUS seems to be a safe and complementary tool to EUS-FNA for the assessment of PCLs. CH-EUS is especially accurate in differentiating nonneoplastic cysts from PCNs and mural nodules from mucus clots. Moreover, the recent International Association of Pancreatology and the European guidelines have recommended CH-EUS for further evaluation of mural nodules in IPMN and PCN respectively. Larger and prospective studies are required to confirm the role of quantitative CH-EUS in the differential diagnosis between malignant and benign mucinous neoplasms. EUS nCLE is a minimally invasive tool with remarkable potential for diagnosing PCLS. Future research should also address new nCLE criteria associated with the grade of dysplasia or cancer, the additional clinical value of combining nCLE with the current standard of PCLs diagnosis and the cost-effectiveness of nCLE during the initial EUS-FNA or after inconclusive results of EUS-FNA. Meanwhile, and based on available evidence at present, excluding cost-effectiveness, we propose an algorithm of diagnosis for PCLs (Figure 10). Through-the-needle cystoscopy and biopsy must be evaluated in formal studies in larger series to validate their results and to confirm their safety before integrating them in the diagnostic flowchart of PCLs.
Figure 10.
Diagnostic algorithm integrating new endoscopic ultrasonography-based technologies. PCL: Pancreatic cystic lesión; PC: Pseudocyst; MPD: Main pancreatic cyst; BD-IPMN: Branch duct intraductal pancreatic mucinous neoplasm; MCN: Mucinous cystic neoplasm; SCA: Serous cystadenoma; NEN: Neuroendocrine tumour; CT: Computed tomography, MRI: Magnetic resonance imaging; EUS: Endoscopic ultrasonography; CH-EUS: Contrast harmonic enhanced EUS; EUS-FNA: EUS guided fine needle aspiration; nCLE: Needle-based confocal endomicroscopy.
CONCLUSION
PCLs are increasingly identified on imaging, but their characterization remains challenging due to limitations of the current endoscopic and imaging techniques. In this article, we presented a comprehensive review about emerging endoscopic tools for the diagnosis of PCLs. Among them, through-the-needle cystoscopy and biopsy still have the lowest amounts of available evidence, with the most extensive experience reported for CH-EUS and nCLE. Both modalities have been demonstrated to provide valuable information for the decision-making process and to be supplementary techniques to EUS-FNA. Limitations for their widespread implementation are their elevated cost and learning curve. Future studies should address their clinical impact on patient management, the optimal timing for their application in the diagnostic work flow of PCLs and their cost-effectiveness. Through-the-needle cystoscopy and intracystic biopsy must be further evaluated in formal and larger trials. Moreover, because a combination of these new techniques may further improve our ability to diagnose PCLs, multi-arm trials incorporating these new technologies and emergent molecular markers would be of most value to determine the best diagnostic approach.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Spain
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
Conflict-of-interest statement: María-Victoria Alvarez-Sánchez has no conflicts of interest or financial ties to disclose. Bertrand Napoléon received educational fees from Boston Scientific SA and Mauna Kea Technologies.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 29, 2018
First decision: April 27, 2018
Article in press: June 16, 2018
P- Reviewer: Andrianello S, De Lisi S, Fusaroli P, Kitamura K, Liu QD S- Editor: Wang XJ L- Editor: A E- Editor: Yin SY
Contributor Information
María-Victoria Alvarez-Sánchez, Instituto de Investigación Sanitaria Galicia Sur, Complejo Hospitalario Universitario de Pontevedra, Pontevedra 36003, Spain. victoria.alvarez.sanchez@hotmail.com.
Bertrand Napoléon, Department of Gastroenterology, Ramsay Générale de Santé Private Hospital Jean Mermoz, Lyon 69008, France.
References
- 1.Laffan TA, Horton KM, Klein AP, Berlanstein B, Siegelman SS, Kawamoto S, Johnson PT, Fishman EK, Hruban RH. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008;191:802–807. doi: 10.2214/AJR.07.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee KS, Sekhar A, Rofsky NM, Pedrosa I. Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol. 2010;105:2079–2084. doi: 10.1038/ajg.2010.122. [DOI] [PubMed] [Google Scholar]
- 3.Ferrone CR, Correa-Gallego C, Warshaw AL, Brugge WR, Forcione DG, Thayer SP, Fernández-del Castillo C. Current trends in pancreatic cystic neoplasms. Arch Surg. 2009;144:448–454. doi: 10.1001/archsurg.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Valsangkar NP, Morales-Oyarvide V, Thayer SP, Ferrone CR, Wargo JA, Warshaw AL, Fernández-del Castillo C. 851 resected cystic tumors of the pancreas: a 33-year experience at the Massachusetts General Hospital. Surgery. 2012;152:S4–S12. doi: 10.1016/j.surg.2012.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salvia R, Fernández-del Castillo C, Bassi C, Thayer SP, Falconi M, Mantovani W, Pederzoli P, Warshaw AL. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004;239:678–685; discussion 685-687. doi: 10.1097/01.sla.0000124386.54496.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sohn TA, Yeo CJ, Cameron JL, Hruban RH, Fukushima N, Campbell KA, Lillemoe KD. Intraductal papillary mucinous neoplasms of the pancreas: an updated experience. Ann Surg. 2004;239:788–797; discussion 797-799. doi: 10.1097/01.sla.0000128306.90650.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Procacci C, Biasiutti C, Carbognin G, Accordini S, Bicego E, Guarise A, Spoto E, Andreis IA, De Marco R, Megibow AJ. Characterization of cystic tumors of the pancreas: CT accuracy. J Comput Assist Tomogr. 1999;23:906–912. doi: 10.1097/00004728-199911000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Curry CA, Eng J, Horton KM, Urban B, Siegelman S, Kuszyk BS, Fishman EK. CT of primary cystic pancreatic neoplasms: can CT be used for patient triage and treatment? AJR Am J Roentgenol. 2000;175:99–103. doi: 10.2214/ajr.175.1.1750099. [DOI] [PubMed] [Google Scholar]
- 9.Visser BC, Yeh BM, Qayyum A, Way LW, McCulloch CE, Coakley FV. Characterization of cystic pancreatic masses: relative accuracy of CT and MRI. AJR Am J Roentgenol. 2007;189:648–656. doi: 10.2214/AJR.07.2365. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhari VV, Raman SS, Vuong NL, Zimmerman P, Farrell J, Reber H, Sayre J, Lu DS. Pancreatic cystic lesions: discrimination accuracy based on clinical data and high resolution CT features. J Comput Assist Tomogr. 2007;31:860–867. doi: 10.1097/RCT.0b013e318039b277. [DOI] [PubMed] [Google Scholar]
- 11.Lu X, Zhang S, Ma C, Peng C, Lv Y, Zou X. The diagnostic value of EUS in pancreatic cystic neoplasms compared with CT and MRI. Endosc Ultrasound. 2015;4:324–329. doi: 10.4103/2303-9027.170425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sahani DV, Sainani NI, Blake MA, Crippa S, Mino-Kenudson M, del-Castillo CF. Prospective evaluation of reader performance on MDCT in characterization of cystic pancreatic lesions and prediction of cyst biologic aggressiveness. AJR Am J Roentgenol. 2011;197:W53–W61. doi: 10.2214/AJR.10.5866. [DOI] [PubMed] [Google Scholar]
- 13.Sainani NI, Saokar A, Deshpande V, Fernández-del Castillo C, Hahn P, Sahani DV. Comparative performance of MDCT and MRI with MR cholangiopancreatography in characterizing small pancreatic cysts. AJR Am J Roentgenol. 2009;193:722–731. doi: 10.2214/AJR.08.1253. [DOI] [PubMed] [Google Scholar]
- 14.de Jong K, van Hooft JE, Nio CY, Gouma DJ, Dijkgraaf MG, Bruno MJ, Fockens P. Accuracy of preoperative workup in a prospective series of surgically resected cystic pancreatic lesions. Scand J Gastroenterol. 2012;47:1056–1063. doi: 10.3109/00365521.2012.674970. [DOI] [PubMed] [Google Scholar]
- 15.Fisher WE, Hodges SE, Yagnik V, Morón FE, Wu MF, Hilsenbeck SG, Raijman IL, Brunicardi FC. Accuracy of CT in predicting malignant potential of cystic pancreatic neoplasms. HPB (Oxford) 2008;10:483–490. doi: 10.1080/13651820802291225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee HJ, Kim MJ, Choi JY, Hong HS, Kim KA. Relative accuracy of CT and MRI in the differentiation of benign from malignant pancreatic cystic lesions. Clin Radiol. 2011;66:315–321. doi: 10.1016/j.crad.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Brugge WR, Lewandrowski K, Lee-Lewandrowski E, Centeno BA, Szydlo T, Regan S, del Castillo CF, Warshaw AL. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004;126:1330–1336. doi: 10.1053/j.gastro.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 18.Sedlack R, Affi A, Vazquez-Sequeiros E, Norton ID, Clain JE, Wiersema MJ. Utility of EUS in the evaluation of cystic pancreatic lesions. Gastrointest Endosc. 2002;56:543–547. doi: 10.1067/mge.2002.128106. [DOI] [PubMed] [Google Scholar]
- 19.Stojanović N, Ruvidić R, Jovcić G, Mijović A. Drug-induced agranulocytosis: bone marrow granulocytic progenitor cells. Biomed Pharmacother. 1990;44:181–184. doi: 10.1016/0753-3322(90)90007-v. [DOI] [PubMed] [Google Scholar]
- 20.Pais SA, Attasaranya S, Leblanc JK, Sherman S, Schmidt CM, DeWitt J. Role of endoscopic ultrasound in the diagnosis of intraductal papillary mucinous neoplasms: correlation with surgical histopathology. Clin Gastroenterol Hepatol. 2007;5:489–495. doi: 10.1016/j.cgh.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Koito K, Namieno T, Nagakawa T, Shyonai T, Hirokawa N, Morita K. Solitary cystic tumor of the pancreas: EUS-pathologic correlation. Gastrointest Endosc. 1997;45:268–276. doi: 10.1016/s0016-5107(97)70269-4. [DOI] [PubMed] [Google Scholar]
- 22.Gerke H, Jaffe TA, Mitchell RM, Byrne MF, Stiffler HL, Branch MS, Baillie J, Jowell PS. Endoscopic ultrasound and computer tomography are inaccurate methods of classifying cystic pancreatic lesions. Dig Liver Dis. 2006;38:39–44. doi: 10.1016/j.dld.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad NA, Kochman ML, Brensinger C, Brugge WR, Faigel DO, Gress FG, Kimmey MB, Nickl NJ, Savides TJ, Wallace MB, et al. Interobserver agreement among endosonographers for the diagnosis of neoplastic versus non-neoplastic pancreatic cystic lesions. Gastrointest Endosc. 2003;58:59–64. doi: 10.1067/mge.2003.298. [DOI] [PubMed] [Google Scholar]
- 24.Thornton GD, McPhail MJ, Nayagam S, Hewitt MJ, Vlavianos P, Monahan KJ. Endoscopic ultrasound guided fine needle aspiration for the diagnosis of pancreatic cystic neoplasms: a meta-analysis. Pancreatology. 2013;13:48–57. doi: 10.1016/j.pan.2012.11.313. [DOI] [PubMed] [Google Scholar]
- 25.Takaori K. “Revisions of the International Consensus Fukuoka Guidelines for the Management of IPMN of the Pancreas”: Progress for twelve years. Pancreatology. 2017;17:645–646. doi: 10.1016/j.pan.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 26.Vege SS, Ziring B, Jain R, Moayyedi P; Clinical Guidelines Committee; American Gastroenterology Association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148:819–822; quize12-13. doi: 10.1053/j.gastro.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 27.European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67:789–804. doi: 10.1136/gutjnl-2018-316027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–197. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Robles EP, Maire F, Cros J, Vullierme MP, Rebours V, Sauvanet A, Aubert A, Dokmak S, Lévy P, Ruszniewski P. Accuracy of 2012 International Consensus Guidelines for the prediction of malignancy of branch-duct intraductal papillary mucinous neoplasms of the pancreas. United European Gastroenterol J. 2016;4:580–586. doi: 10.1177/2050640615623370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Springer S, Wang Y, Dal Molin M, Masica DL, Jiao Y, Kinde I, Blackford A, Raman SP, Wolfgang CL, Tomita T, et al. A combination of molecular markers and clinical features improve the classification of pancreatic cysts. Gastroenterology. 2015;149:1501–1510. doi: 10.1053/j.gastro.2015.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alvarez-Sánchez MV, Napoléon B. Contrast-enhanced harmonic endoscopic ultrasound imaging: basic principles, present situation and future perspectives. World J Gastroenterol. 2014;20:15549–15563. doi: 10.3748/wjg.v20.i42.15549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ignee A, Atkinson NS, Schuessler G, Dietrich CF. Ultrasound contrast agents. Endosc Ultrasound. 2016;5:355–362. doi: 10.4103/2303-9027.193594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kang ST, Yeh CK. Ultrasound microbubble contrast agents for diagnostic and therapeutic applications: current status and future design. Chang Gung Med J. 2012;35:125–139. doi: 10.4103/2319-4170.106159. [DOI] [PubMed] [Google Scholar]
- 34.Kitano M, Kudo M, Sakamoto H, Komaki T. Endoscopic ultrasonography and contrast-enhanced endoscopic ultrasonography. Pancreatology. 2011;11 Suppl 2:28–33. doi: 10.1159/000323493. [DOI] [PubMed] [Google Scholar]
- 35.Sanchez MV, Varadarajulu S, Napoleon B. EUS contrast agents: what is available, how do they work, and are they effective? Gastrointest Endosc. 2009;69:S71–S77. doi: 10.1016/j.gie.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 36.Hocke M, Cui XW, Domagk D, Ignee A, Dietrich CF. Pancreatic cystic lesions: The value of contrast-enhanced endoscopic ultrasound to influence the clinical pathway. Endosc Ultrasound. 2014;3:123–130. doi: 10.4103/2303-9027.131040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fusaroli P, Serrani M, De Giorgio R, D’Ercole MC, Ceroni L, Lisotti A, Caletti G. Contrast Harmonic-Endoscopic Ultrasound Is Useful to Identify Neoplastic Features of Pancreatic Cysts (With Videos) Pancreas. 2016;45:265–268. doi: 10.1097/MPA.0000000000000441. [DOI] [PubMed] [Google Scholar]
- 38.Kamata K, Kitano M, Omoto S, Kadosaka K, Miyata T, Yamao K, Imai H, Sakamoto H, Harwani Y, Chikugo T, et al. Contrast-enhanced harmonic endoscopic ultrasonography for differential diagnosis of pancreatic cysts. Endoscopy. 2016;48:35–41. doi: 10.1055/s-0034-1393564. [DOI] [PubMed] [Google Scholar]
- 39.Yamashita Y, Ueda K, Itonaga M, Yoshida T, Maeda H, Maekita T, Iguchi M, Tamai H, Ichinose M, Kato J. Usefulness of contrast-enhanced endoscopic sonography for discriminating mural nodules from mucous clots in intraductal papillary mucinous neoplasms: a single-center prospective study. J Ultrasound Med. 2013;32:61–68. doi: 10.7863/jum.2013.32.1.61. [DOI] [PubMed] [Google Scholar]
- 40.Fujita M, Itoi T, Ikeuchi N, Sofuni A, Tsuchiya T, Ishii K, Kamada K, Umeda J, Tanaka R, Tonozuka R, et al. Effectiveness of contrast-enhanced endoscopic ultrasound for detecting mural nodules in intraductal papillary mucinous neoplasm of the pancreas and for making therapeutic decisions. Endosc Ultrasound. 2016;5:377–383. doi: 10.4103/2303-9027.190927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harima H, Kaino S, Shinoda S, Kawano M, Suenaga S, Sakaida I. Differential diagnosis of benign and malignant branch duct intraductal papillary mucinous neoplasm using contrast-enhanced endoscopic ultrasonography. World J Gastroenterol. 2015;21:6252–6260. doi: 10.3748/wjg.v21.i20.6252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yamamoto N, Kato H, Tomoda T, Matsumoto K, Sakakihara I, Noma Y, Horiguchi S, Harada R, Tsutsumi K, Hori K, et al. Contrast-enhanced harmonic endoscopic ultrasonography with time-intensity curve analysis for intraductal papillary mucinous neoplasms of the pancreas. Endoscopy. 2016;48:26–34. doi: 10.1055/s-0034-1393563. [DOI] [PubMed] [Google Scholar]
- 43.Leung Ki EL, Napoleon B. Nuevas herramientas y recursos en la evaluación de quistes pancreáticos por ultrasonografía endoscópica.In: Fauze Maluf-Filho/Shyam Varadarajulu. Avances en ultrasonografía endoscópica. Clínicas iberoamericanas de gastroenterología y hepatología. 2018:51–68. [Google Scholar]
- 44.Nakai Y, Isayama H, Shinoura S, Iwashita T, Samarasena JB, Chang KJ, Koike K. Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases. Dig Endosc. 2014;26 Suppl 1:86–94. doi: 10.1111/den.12152. [DOI] [PubMed] [Google Scholar]
- 45.Giovannini M. Needle-based confocal laser endomicroscopy. Endosc Ultrasound. 2015;4:284–288. doi: 10.4103/2303-9027.170405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsujino T, Yan-Lin Huang J, Nakai Y, Samarasena JB, Lee JG, Chang KJ. In vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy. Best Pract Res Clin Gastroenterol. 2015;29:601–610. doi: 10.1016/j.bpg.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 47.Ştefănescu D, Pereira SP, Keane M, Săftoiu A. Needle-based confocal laser endomicroscopy in pancreatic cystic tumors assessment. Rom J Morphol Embryol. 2015;56:1263–1268. [PubMed] [Google Scholar]
- 48.Konda VJ, Aslanian HR, Wallace MB, Siddiqui UD, Hart J, Waxman I. First assessment of needle-based confocal laser endomicroscopy during EUS-FNA procedures of the pancreas (with videos) Gastrointest Endosc. 2011;74:1049–1060. doi: 10.1016/j.gie.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 49.Wefers H, Sies H. Generation of photoemissive species during quinone redox cycling. Biochem Pharmacol. 1986;35:22–24. doi: 10.1016/0006-2952(86)90548-4. [DOI] [PubMed] [Google Scholar]
- 50.Nakai Y, Iwashita T, Park DH, Samarasena JB, Lee JG, Chang KJ. Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc. 2015;81:1204–1214. doi: 10.1016/j.gie.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 51.Napoléon B, Lemaistre AI, Pujol B, Caillol F, Lucidarme D, Bourdariat R, Morellon-Mialhe B, Fumex F, Lefort C, Lepilliez V, et al. A novel approach to the diagnosis of pancreatic serous cystadenoma: needle-based confocal laser endomicroscopy. Endoscopy. 2015;47:26–32. doi: 10.1055/s-0034-1390693. [DOI] [PubMed] [Google Scholar]
- 52.Napoleon B, Lemaistre AI, Pujol B, Caillol F, Lucidarme D, Bourdariat R, Morellon-Mialhe B, Fumex F, Lefort C, Lepilliez V, et al. In vivo characterization of pancreatic cystic lesions by needle-based confocal laser endomicroscopy (nCLE): proposition of a comprehensive nCLE classification confirmed by an external retrospective evaluation. Surg Endosc. 2016;30:2603–2612. doi: 10.1007/s00464-015-4510-5. [DOI] [PubMed] [Google Scholar]
- 53.Kadayifci A, Atar M, Basar O, Forcione DG, Brugge WR. Needle-Based Confocal Laser Endomicroscopy for Evaluation of Cystic Neoplasms of the Pancreas. Dig Dis Sci. 2017;62:1346–1353. doi: 10.1007/s10620-017-4521-2. [DOI] [PubMed] [Google Scholar]
- 54.Krishna SG, Modi RM, Kamboj AK, Swanson BJ, Hart PA, Dillhoff ME, Manilchuk A, Schmidt CR, Conwell DL. In vivo and ex vivo confocal endomicroscopy of pancreatic cystic lesions: A prospective study. World J Gastroenterol. 2017;23:3338–3348. doi: 10.3748/wjg.v23.i18.3338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Napoléon B, Palazzo M, Lemaistre AI, Caillol F, Palazzo L, Aubert A, Buscail L, Maire F, Mialhe-Morellon B, Pujol B, et al. Needle-based confocal laser endomicroscopy characterization of pancreatic cystic lesions with a definitive diagnoses: a prospective multicentre study. Endoscopy. 2017:In press. doi: 10.1055/a-0732-5356. [DOI] [PubMed] [Google Scholar]
- 56.Karia K, Waxman I, Konda VJ, Gress FG, Sethi A, Siddiqui UD, Sharaiha RZ, Kedia P, Jamal-Kabani A, Gaidhane M, et al. Needle-based confocal endomicroscopy for pancreatic cysts: the current agreement in interpretation. Gastrointest Endosc. 2016;83:924–927. doi: 10.1016/j.gie.2015.08.080. [DOI] [PubMed] [Google Scholar]
- 57.Krishna SG, Swanson B, Hart PA, El-Dika S, Walker JP, McCarthy ST, Malli A, Shah ZK, Conwell DL. Validation of diagnostic characteristics of needle based confocal laser endomicroscopy in differentiation of pancreatic cystic lesions. Endosc Int Open. 2016;4:E1124–E1135. doi: 10.1055/s-0042-116491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Krishna SG, Brugge WR, Dewitt JM, Kongkam P, Napoleon B, Robles-Medranda C, Tan D, El-Dika S, McCarthy S, Walker J, et al. Needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cystic lesions: an international external interobserver and intraobserver study (with videos) Gastrointest Endosc. 2017;86:644–654.e2. doi: 10.1016/j.gie.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 59.Aparicio JR, Martínez J, Niveiro M, Cabezas A, Ruiz F, De Madaria E, Casellas JA. Direct intracystic biopsy and pancreatic cystoscopy through a 19-gauge needle EUS (with videos) Gastrointest Endosc. 2010;72:1285–1288. doi: 10.1016/j.gie.2010.08.036. [DOI] [PubMed] [Google Scholar]
- 60.Chai N, Feng J, Guo Y, Li H, Ning B, Wang X, Wang Y, Wang Y, Zhai Y, Linghu E. Preliminary study of single-operator cholangioscopy for diagnosing pancreatic cystic lesions. Gastrointest Endosc. 2017;86:208–218. doi: 10.1016/j.gie.2017.01.038. [DOI] [PubMed] [Google Scholar]
- 61.Shakhatreh MH, Naini SR, Brijbassie AA, Grider DJ, Shen P, Yeaton P. Use of a novel through-the-needle biopsy forceps in endoscopic ultrasound. Endosc Int Open. 2016;4:E439–E442. doi: 10.1055/s-0042-101941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barresi L, Tarantino I, Ligresti D, Curcio G, Granata A, Traina M. A new tissue acquisition technique in pancreatic cystic neoplasm: endoscopic ultrasound-guided through-the-needle forceps biopsy. Endoscopy. 2015;47 Suppl 1:E297–E298. doi: 10.1055/s-0034-1392031. [DOI] [PubMed] [Google Scholar]
- 63.Pham KD, Engjom T, Gjelberg Kollesete H, Helgeland L. Diagnosis of a mucinous pancreatic cyst and resection of an intracystic nodule using a novel through-the-needle micro forceps. Endoscopy. 2016;48 Suppl 1:E125–E126. doi: 10.1055/s-0042-105437. [DOI] [PubMed] [Google Scholar]
- 64.Attili F, Pagliari D, Rimbas M, Inzani F, Brizi MG, Costamagna G, Larghi A. Endoscopic ultrasound-guided histological diagnosis of a mucinous non-neoplastic pancreatic cyst using a specially designed through-the-needle microforceps. Endoscopy. 2016;48 Suppl 1:E188–E189. doi: 10.1055/s-0042-108194. [DOI] [PubMed] [Google Scholar]
- 65.Huelsen A, Cooper C, Saad N, Gupta S. Endoscopic ultrasound-guided, through-the-needle forceps biopsy in the assessment of an incidental large pancreatic cystic lesion with prior inconclusive fine-needle aspiration. Endoscopy. 2017;49:E109–E110. doi: 10.1055/s-0043-100217. [DOI] [PubMed] [Google Scholar]
- 66.Jais B, Rebours V, Malleo G, Salvia R, Fontana M, Maggino L, Bassi C, Manfredi R, Moran R, Lennon AM, et al. Serous cystic neoplasm of the pancreas: a multinational study of 2622 patients under the auspices of the International Association of Pancreatology and European Pancreatic Club (European Study Group on Cystic Tumors of the Pancreas) Gut. 2016;65:305–312. doi: 10.1136/gutjnl-2015-309638. [DOI] [PubMed] [Google Scholar]
- 67.Kitano M, Kudo M, Yamao K, Takagi T, Sakamoto H, Komaki T, Kamata K, Imai H, Chiba Y, Okada M, et al. Characterization of small solid tumors in the pancreas: the value of contrast-enhanced harmonic endoscopic ultrasonography. Am J Gastroenterol. 2012;107:303–310. doi: 10.1038/ajg.2011.354. [DOI] [PubMed] [Google Scholar]
- 68.Napoleon B, Alvarez-Sanchez MV, Gincoul R, Pujol B, Lefort C, Lepilliez V, Labadie M, Souquet JC, Queneau PE, Scoazec JY, et al. Contrast-enhanced harmonic endoscopic ultrasound in solid lesions of the pancreas: results of a pilot study. Endoscopy. 2010;42:564–570. doi: 10.1055/s-0030-1255537. [DOI] [PubMed] [Google Scholar]
- 69.Gincul R, Palazzo M, Pujol B, Tubach F, Palazzo L, Lefort C, Fumex F, Lombard A, Ribeiro D, Fabre M, et al. Contrast-harmonic endoscopic ultrasound for the diagnosis of pancreatic adenocarcinoma: a prospective multicenter trial. Endoscopy. 2014;46:373–379. doi: 10.1055/s-0034-1364969. [DOI] [PubMed] [Google Scholar]
- 70.Omoto S, Takenaka M, Kitano M, Miyata T, Kamata K, Minaga K, Arizumi T, Yamao K, Imai H, Sakamoto H, et al. Characterization of Pancreatic Tumors with Quantitative Perfusion Analysis in Contrast-Enhanced Harmonic Endoscopic Ultrasonography. Oncology. 2017;93 Suppl 1:55–60. doi: 10.1159/000481231. [DOI] [PubMed] [Google Scholar]
- 71.Tachezy M, Reichelt U, Melenberg T, Gebauer F, Izbicki JR, Kaifi JT. Angiogenesis index CD105 (endoglin)/CD31 (PECAM-1) as a predictive factor for invasion and proliferation in intraductal papillary mucinous neoplasm (IPMN) of the pancreas. Histol Histopathol. 2010;25:1239–1246. doi: 10.14670/HH-25.1239. [DOI] [PubMed] [Google Scholar]
- 72.Main ML. Ultrasound contrast agent safety: from anecdote to evidence. JACC Cardiovasc Imaging. 2009;2:1057–1059. doi: 10.1016/j.jcmg.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 73.Szebeni J. Complement activation-related pseudoallergy: a new class of drug-induced acute immune toxicity. Toxicology. 2005;216:106–121. doi: 10.1016/j.tox.2005.07.023. [DOI] [PubMed] [Google Scholar]
- 74.Piscaglia F, Bolondi L; Italian Society for Ultrasound in Medicine and Biology (SIUMB) Study Group on Ultrasound Contrast Agents. The safety of Sonovue in abdominal applications: retrospective analysis of 23188 investigations. Ultrasound Med Biol. 2006;32:1369–1375. doi: 10.1016/j.ultrasmedbio.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 75.de Jong K, Poley JW, van Hooft JE, Visser M, Bruno MJ, Fockens P. Endoscopic ultrasound-guided fine-needle aspiration of pancreatic cystic lesions provides inadequate material for cytology and laboratory analysis: initial results from a prospective study. Endoscopy. 2011;43:585–590. doi: 10.1055/s-0030-1256440. [DOI] [PubMed] [Google Scholar]
- 76.Yannuzzi LA, Rohrer KT, Tindel LJ, Sobel RS, Costanza MA, Shields W, Zang E. Fluorescein angiography complication survey. Ophthalmology. 1986;93:611–617. doi: 10.1016/s0161-6420(86)33697-2. [DOI] [PubMed] [Google Scholar]
- 77.Wallace MB, Meining A, Canto MI, Fockens P, Miehlke S, Roesch T, Lightdale CJ, Pohl H, Carr-Locke D, Löhr M, et al. The safety of intravenous fluorescein for confocal laser endomicroscopy in the gastrointestinal tract. Aliment Pharmacol Ther. 2010;31:548–552. doi: 10.1111/j.1365-2036.2009.04207.x. [DOI] [PubMed] [Google Scholar]
- 78.Le Pen C, Palazzo L, Napoléon B. A health economic evaluation of needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cysts. Endosc Int Open. 2017;5:E987–E995. doi: 10.1055/s-0043-117947. [DOI] [PMC free article] [PubMed] [Google Scholar]