Abstract
Current approaches to the measurement of hearing aid benefit typically use clinical or laboratory-based speech perception tests or retrospective self-report surveys. However, when assessing hearing aid outcomes in adults with mild hearing impairment, the traditional outcome measures may not be sufficiently sensitive. An alternative to these techniques are approaches that capture data about real-world experiences as they are experienced, such as ecological momentary assessment. This single-subject experimental design pilot study investigated the feasibility of using ecological momentary assessment in assessing whether hearing aids make a difference to the real-world listening experiences of adults with mild hearing impairment. Ten participants with an average age of 70 years and no previous amplification experience answered survey questions on their listening experiences over a 4-week period (1 week without hearing aids, 2 weeks with hearing aids, and 1 week without hearing aids). A total of 860 surveys were collected. Participants reported significantly better speech understanding and less listening effort during the 2-week trial with hearing aids compared to baseline conditions. In addition, they reported that they were significantly less hampered by their hearing difficulties and had greater enjoyment of listening events with wearing hearing aids. Individual variation in hearing aid benefit was evident. This pilot study showed that ecological momentary assessment has potential to quantify self-reported aided benefit for individuals with mild hearing impairment fitted with hearing aids. This research also highlighted that a real-world approach is needed to explore individualized outcomes and provide different insights to standardized questionnaires.
Keywords: ecological momentary assessment, hearing impairment, hearing aids, older adults
Introduction
Measuring hearing aid (HA) outcomes is an important aspect of delivering quality audiological care and ascertaining the benefits and costs of intervention options (Humes, Ahlstrom, Bratt, & Peek, 2009; Saunders, Chisolm, & Abrams, 2005). Current approaches to the measurement of HA benefit typically take the form of clinical or laboratory-based speech perception tests or retrospective self-report surveys of experiences outside the clinic. However, both have limitations and may not be considered appropriately reflective of performance in the real world (Barker, MacKenzie, Elliott, & de Lusignan, 2015; Best, Keidser, Buchholz, & Freeston, 2013).
In particular, when assessing HA outcomes in adults with mild hearing impairment (HI), traditional outcome measures may not be sufficiently able to detect change and hence are insufficiently sensitive for this clinical population. A recent systematized review concluded that speech perception tests in quiet or in noise showed only a moderate correlation, at best, with self-reported hearing difficulties for adults with mild HI (Timmer, Hickson, & Launer, 2015). Equally, some self-report measures may lack sufficient sensitivity or specificity for this population. Salonen, Johansson, Karjalainen, Vahlberg, and Isoaho (2011) and Sindhusake et al. (2001) reported a weaker relationship between mild HI and self-reported hearing difficulty than with greater degrees of impairment, using the popular screening version of the Hearing Handicap Inventory for the Elderly (HHIE-S; Lichtenstein, Bess, & Logan, 1988). Questionnaires used to assess the impact on quality of life show a similar lack of sensitivity. Chia et al. (2007) found no significant difference in health-related quality of life for participants with mild, bilateral HI when compared to similar older adults with no, or unilateral, HI. The measure used in their study was the 36-Item Short-Form Health Survey (SF-36; Ware & Sherbourne, 1992), a generic measure of health functional status. The SF-36 may be not be sufficiently sensitive to hearing-related quality of life, particularly in the case of mild HI or when using a small participant sample size (Hickson et al., 2008).
An alternative to using self-report outcome measures that require individuals to reflect on and generalize past experiences are techniques that capture data about real-world experiences as they are lived, such as ecological momentary assessment (EMA) or experiential sampling (Shiffman, Stone, & Hufford, 2008). This approach was utilized by the authors in a previous study to investigate the hearing difficulties encountered in real-world situations by adults with mild HI (Timmer, Hickson, & Launer, 2017a). The participants were 29 adults with a mean age of 69 years and mild HI, defined as average hearing loss at .5, 1, 2, and 4 kHz between 20 and 40 dB HL in both ears (this definition of mild HI is also utilized for this study). Participants answered a self-report questionnaire on a smartphone, triggered based on defined time, event, or user criteria. The self-report questionnaire included questions about the intended listening activity, characteristics of the acoustic environment, and three questions which together gave an indication of the participant’s self-rated hearing performance on a 5-point response scale. The three questions were as follows: “On average, how much speech did you understand during the listening event?” “On average, how much effort did you have to put in to listen effectively?” and “How much have your hearing difficulties affected what you wanted to do during the listening event?” In parallel, selected parameters about the sound environment were also logged in a hearing device, to allow comparisons between the objective sound environment and subjective ratings of participants’ listening experiences in those environments. All participants also completed the full version of the HHIE (Ventry & Weinstein, 1982) before and after the EMA data collection period to check for reactivity, which is the potential for behaviors or experiences to be influenced by the act of observing them (Stone & Shiffman, 2002).
The findings from this previous EMA study demonstrated that in 91% of the 962 speech-listening surveys collected, speech understanding was rated as either “75%” or “100%,” and in only 9% of listening events, speech understanding was rated as “0%,” “25%,” or “50%” (Timmer, 2017). However, although the participants self-reported very good or excellent speech understanding in their common listening events, they also rated the events as needing relatively more effort to reach that level. It can therefore be deduced that the provision of HAs to this population may not result in significant change in self-reported speech understanding but may improve other dimensions such as the effort required to hear effectively.
The previous EMA study also showed considerable variation in self-reported disability as measured by the HHIE, and in self-reported hearing performance, as measured by the EMA surveys, among this clinical population. In acknowledging the variation across participants with mild HI in terms of self-reported hearing, a single-subject experimental design (SSED) was chosen for this study. In SSED, also called single-case design, the effects of intervention on performance are examined over time using continuous assessment, with the individual participant acting as his or her own control (Kazdin, 1982, p. 104).
The SSED chosen incorporated a three-phase or ABA design: an observation or baseline phase, the intervention phase (the provision of HAs), and a final withdrawal phase. Many SSED studies include a second intervention phase and are therefore labeled as an ABAB design, with the A denoting a baseline and B an intervention phase (Kazdin, 2016; Tate, Perdices, McDonald, Togher, & Rosenkoetter, 2014). As this ABAB design may place undue burden on the participant and involves a high number of repeated assessments, other single-subject study designs have also emerged (Byiers, Reichle, & Symons, 2012). Nevertheless, to ensure that causal relationships can be assessed and internal validity is not at risk, a single-subject design should incorporate at least three phases (Kazdin, 1982, p. 119).
A small number of SSED studies have been conducted in hearing research. For example, Glista, Scollie, and Sulkers (2012) used an ABA design when investigating acclimatization to frequency-lowering HAs with six children between 11 and 18 years. Twenty years earlier, Gatehouse (1992) used an SSED in which one ear acted as control and the other as test ear to investigate acclimatization to monaural HA fitting with four participants. Desjardins (2016) also used an ABA SSED with six participants between 54 and 64 years to examine changes in cognitive performance before and after HA use. Finally, Palmer, Adams, Bourgeois, Durrant, and Rossi (1999) used an SSED to show the benefits of HA provision on problem behaviors in eight individuals with Alzheimer’s disease. Unfortunately, this last study used an AB design which, although sometimes necessary due to ethical reasons, does not allow a robust conclusion as to whether the change in behavior was due to the intervention.
Although EMA can yield valuable aggregate or group data, the technique lends itself to gaining in-depth information regarding individual differences and in detecting intervention effects (Moskowitz & Young, 2006). While EMA has been shown to be feasible with older adults with mild HI (Timmer et al., 2017a), to the authors’ knowledge, it has not been utilized to measure HA benefit following the provision of amplification. As yet, it is unknown if the approach is sufficiently sensitive to detect these changes, particularly for adults with mild HI.
A big data study on HA use in adults with mild HI, based on a database of 8,489 bilateral fittings, showed that when individuals with mild HI are fitted with HAs, they use these as much as those with a moderate degree of HI (Timmer, Hickson, & Launer, 2017b). The outcome data were about HA use only and while there may be a link between use and benefit, they are different constructs and therefore should be measured separately (Cox, Gilmore, & Alexander, 1991; Dillon, James, & Ginis, 1997). In addition, there is a dearth of evidence about HA benefit for adults with a mild degree of HI specifically, as many studies combine participants with a mild and a moderate degree of HI (Timmer et al., 2015). A systematic review of HA benefit in adults with mild HI by Johnson, Danhauer, Ellis, and Jilla (2016) found only 10 papers that met the inclusion criteria based on quality of evidence and participants’ HI. The characteristics of the participants included in the systematic review showed large variations in terms of age, HA experience, and HA technology.
The Johnson et al. (2016) review defined HA benefit as dependent upon the wide range of outcome measures used in the studies and therefore the construct of benefit referred interchangeably to improvements in satisfaction, activity limitations, or participation restrictions. These dimensions are most often measured on self-report questionnaires such as the International Outcome Inventory for Hearing Aids (IOI-HA; Cox & Alexander, 2002). The IOI-HA is a 7-item questionnaire which surveys the HA outcome dimensions of use, benefit, residual activity limitations, satisfaction, residual participation restrictions, impact on others, and quality of life. Responses are scored 1 (poorest outcome) to 5 (best outcome), with a maximum total score of 35. Participants in this study were administered the IOI-HA to allow comparison of the EMA data to an outcome measure commonly used with adults fitted with HAs (e.g., Barker et al., 2015; Hickson, Clutterbuck, & Khan, 2010; Williams, Johnson, & Danhauer, 2009). The IOI-HA was chosen, as it encompasses the wide range of dimensions used to define “benefit” in the Johnson et al. (2016) review.
For the purposes of this study, HA benefit is defined as a (positive) difference comparing scores without HAs and during the use of HAs on four questions in the EMA survey. These questions, collectively referred to as hearing performance questions, were as follows: On average, how much speech did you understand during the listening event? On average, how much effort did you have to put in to listen effectively? Do you feel that any difficulty with your hearing negatively affected or hampered communication during this listening event? and Do you feel your hearing negatively affected your enjoyment of this listening event?
In summary, the research questions for this pilot study were twofold:
Can EMA be used to measure differences in performance with and without HAs in older adults with a mild HI?
Can HAs provide benefit for adults with a mild HI in daily life, as measured by EMA?
Method
In this pilot study, the SSED ABA design (1 week without HAs, 2 weeks with HAs, and 1 week without HAs) was applied over a 4-week period. This design allowed for equal amount of time for participants in both conditions, that is, 2 weeks without HAs (unaided) and 2 weeks with HAs (aided). It also allowed for data analysis to determine whether the differences in self-reported aided performance changed during the 2 weeks, perhaps due to acclimatization. Ethical approval was obtained from the University of Queensland Behavioural and Social Sciences Ethical Review Committee.
Participants
Ten participants (six males and four females) with acquired sensorineural mild HI participated in this study. The average age of the participants was 70 years, with a range of 57 to 81. The participant characteristics are shown in Table 1.
Table 1.
Participant Characteristics.
| Participant | Age (years) | Sex | Highest education level | Employment status | Main language | Smartphone ownership | Self-reported health statusa | Self- reported visiona | Length of hearing difficulties (years) | Self-reported confidence in managing HAsb | Attitude to HAsc |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 71 | Female | Postgraduate degree | Retired | English | Yes | Good | Fair | 2 | Quite a bit | 0 |
| 2 | 73 | Male | Trade qualification | Retired | English | Yes | Excellent | Excellent | 10 | Quite a bit | 2 |
| 3 | 75 | Female | Bachelor’s degree | Retired | English | Yes | Very good | Very good | 9 | Quite a bit | −3 |
| 4 | 65 | Male | Postgraduate degree | Employed, part-time | English | Yes | Very good | Very good | 17 | Quite a bit | −1 |
| 5 | 65 | Male | Bachelor’s degree | Retired | English | Yes | Very good | Excellent | 8 | Extremely | 1 |
| 6 | 81 | Female | High school | Retired | English | Yes | Very good | Very good | 15 | Somewhat | 1 |
| 7 | 71 | Female | Postgraduate degree | Retired | English | No | Fair | Fair | 7 | Quite a bit | 0 |
| 8 | 57 | Male | Postgraduate degree | Employed, full-time | English | Yes | Excellent | Excellent | 20 | Extremely | 2 |
| 9 | 72 | Male | Postgraduate degree | Retired | English | Yes | Good | Good | 6 | Quite a bit | 0 |
| 10 | 67 | Male | Postgraduate degree | Employed, part-time | English | Yes | Very good | Very good | 4 | Extremely | −2 |
Note. HAs = hearing aids.
aOn a scale of excellent, very good, good, fair, or poor. bOn a scale of extremely, quite a bit, somewhat, a little bit, or not at all. cResponse to the question “How would you rate your general attitude to hearing aids” on a scale of −5 (very negative) to +5 (very positive) (Meyer, Hickson, Lovelock, Lampert, & Khan, 2014).
The 10 participants were recruited from a previous EMA study (identified as Participants 1, 4, 5, 6, 8, 18, 20, 23, 25, and 29 in that study; Timmer et al., 2017a) and hence had some familiarity with the research equipment. Inclusion criteria for this study were that participants had no previous HA experience and were to have a mild HI, defined as average hearing loss at .5, 1, 2, and 4 kHz between 20 and 40 dB HL in both ears. The 4FAHL as well as the pure-tone averages at six frequencies (6FAHL) are shown in Table 2.
Table 2.
Participant Audiological Characteristics.
| N = 10 | Median (IQR) | |
|---|---|---|
| 4FAHL(dB HL) | BEA | 25.6 (21.3–30.6) |
| WEA | 30.6 (26.6–33.8) | |
| 6FAHL (dB HL) | BEA | 33.3 (30.2–40.6) |
| WEA | 40.4 (37.5–45.4) |
Note. 4FAHL = four-frequency average hearing loss, of air conduction thresholds at 0.5,1, 2, and 4 kHz; 6FAHL = six-frequency average hearing loss, of air conduction thresholds at 0.5,1, 2, 4, 6, and 8 kHz; BEA = better ear average; WEA = worse ear average; IQR = interquartile range.
Participants were selectively sampled from the previous study cohort; 5 participants were excluded as they owned HAs, and the remaining 24 participants were ranked from greatest self-reported hearing disability (based on their HHIE score and their self-reported hearing performance) to least self-reported hearing disability. The first approach was made to 15 participants from the previous cohort who had indicated willingness to be involved in another EMA study and had the highest self-reported hearing disability in that study. One of these had acquired HAs, one was ill, five were unavailable, and three could not commit to the 4-week data collection due to travel plans; therefore, five participants from this first approach agreed to participate. Subsequently, the next eight participants with the highest self-reported hearing disability were approached, one was unavailable, and two were ill, resulting in a further five participants. Therefore, a total of 23 potential participants were approached, yielding 10 actual participants.
The 10 participants were representative of the group of 29 participants included in the Timmer et al. (2017a) study. For example, the mean HHIE of the participants in this study was 18.8 and the mean posttrial HHIE score of all 29 in the Timmer et al. (2017a) study was 19.9. Similarly, the mean hearing performance score from the previous study for the 10 participants included in this study was 12.4 and of all 29 participants was 12.6.
All participants provided written informed consent at their first appointment and were reimbursed with an AUD50 (approximately USD39) gift voucher for their participation in the study at the last appointment.
EMA Survey
The complete EMA survey in this study contained up to 16 closed-ended questions about the listening activity, characteristics of the environment, and hearing performance (Table 3).
Table 3.
EMA Survey.
| Question | Answer options |
|---|---|
| 1. A listening event is an occurrence in which you ACTIVELY listen to sounds (including speech and nonspeech sounds). Are you in the middle of the event? | □ Yes |
| □ No | |
| 1a. (If “No”) When did the event end? | □ Less than 1 hour ago |
| □ More than 1 hour ago1 | |
| 2. Were you listening to speech? | □ Yes |
| □ No | |
| 2a. (If “Yes”)—what were you listening to? | □ Conversation, three people or fewer |
| □ Conversation, four people or more | |
| □ Speech listening, live | |
| □ Speech listening, media | |
| □ Conversation on phone | |
| 2b. (If “No”)—what were you listening to? | □ Listening to nonspeech sound |
| □ Not actively listening | |
| 3. Where were you? | □ Outdoor/traffic |
| □ Indoor | |
| 3a. (If “Outdoor/traffic”) Please be more specific | □ Outdoor, moving traffic |
| □ Outdoor, no traffic | |
| 3b. (If “Indoor”) Please be more specific | □ Home, fewer than 10 people in the room |
| □ Other than home, fewer than 10 people in the room | |
| □ Crowd of people, more than 10 people | |
| 4. (If listening to speech) Were you familiar with the speaker(s)? | □ Unfamiliar |
| □ Somewhat unfamiliar | |
| □ Somewhat familiar | |
| □ Familiar | |
| 5. (If listening to speech) Could you see the speaker’s face? | □ No |
| □ Yes, but only sometimes | |
| □ Almost always | |
| 6. (If listening to speech) Where was the speaker most of the time? | □ Front |
| □ Side | |
| □ Back | |
| 7. On average, how noisy was it during the listening event? | □ Quiet |
| □ Somewhat noisy | |
| □ Noisy | |
| □ Very noisy | |
| 8. (If not quiet) Where was the noise most of the time? | □ Front |
| □ Side | |
| □ Back | |
| □ All around | |
| 9. (If indoor) Compared to an average living room, how large was the room? | □ Smaller |
| □ About average | |
| □ Larger | |
| 10. (If indoor) Was there carpeting? | □ Yes |
| □ No | |
| 11. (If listening to speech) On average, how much speech did you understand during the listening event? | □ 0% |
| □ 10% | |
| □ 20% | |
| □ 30% | |
| □ 40% | |
| □ 50% | |
| □ 60% | |
| □ 70% | |
| □ 80% | |
| □ 90% | |
| □ 100% | |
| 12. On average, how much effort did you have to put in to listen effectively? | □ No effort |
| □ Some effort | |
| □ Moderate effort | |
| □ Quite a bit of effort | |
| □ A lot of effort | |
| 13. Do you feel that any difficulty with your hearing negatively affected or hampered communication during this listening event? | □ Not at all |
| □ A little | |
| □ Moderately | |
| □ Quite a bit | |
| □ Very much | |
| 14. Do you feel your hearing negatively affected your enjoyment of this listening event? | □ Not at all |
| □ A little | |
| □ Moderately | |
| □ Quite a bit | |
| □ Very much | |
| 15. How important was it for you to hear well during the listening event? | □ Not important at all |
| □ A little | |
| □ Moderately | |
| □ Quite a bit | |
| □ Very important | |
| 16. Are you currently wearing hearing aids? | □ Yes |
| □ No |
The survey in this study was modified from the previous 17-question EMA study based on the findings and participants’ feedback (Timmer et al., 2017a). The changes to the survey incorporated in this study were mainly related to the hearing performance questions from the previous study:
Question 11 (On average, how much speech did you understand during the listening event?) was changed from a 5-point to 11-point Likert-type scale to increase the number of response options for this item.
Question 13 (“How much have your hearing difficulties affected what you wanted to do during the listening event”) was changed to “Do you feel that any difficulty with your hearing negatively affected or hampered communication during this listening event?” for greater clarity. This wording was adapted from the Self-Assessment of Communication (Schow & Nerbonne, 1982).
Question 14 (“Were you feeling happy during the listening event?”) was changed to “Do you feel your hearing negatively affected your enjoyment of this listening event?” in order to give greater clarity to the intent of the question.
The question “In general, could you tell where sounds were coming from right away?” was removed as localization was not a problem for this cohort.
Procedures
During the first appointment, demographic information was collected (see Table 1) and audiological assessment of each participant was conducted (see Table 2). Due to the time between data collection for the previous study and this study (between 8 and 15 months), bilateral air-conduction thresholds were retested and obtained at .5, 1, 2, 3, 4, 6, and 8 kHz, and bone-conduction thresholds were obtained at .5, 1, 2, and 4 kHz.
Participants were given the Motorola G smartphone with the MobEval app during the first appointment, shown how to trigger an EMA survey themselves, and completed one survey in the presence of the researcher at that time. Surveys were automatically triggered based on defined time criteria or manually triggered by the participant themselves. The time triggers were identical to those used in the previous EMA study (the first trigger at a random time between 8:30 and 10:00 a.m. with subsequent surveys triggered every 4 hours subsequently, until 7:00 p.m.). During the first appointment, instructions in managing the smartphone were given orally and in written form, and participants were reminded to complete at least three surveys per day. The surveys collected over the following 7 days formed the participants’ baseline.
During their second appointment 1 week later, participants were fitted with bilateral Phonak Bolero V-90 mini-behind-the-ear HAs, with a thin tube and open dome, clinically appropriate to their HI. All HAs were programmed to meet National Acoustic Laboratory-Non-Linear 2 prescription procedure targets (NAL-NL2; Keidser, Dillon, Flax, Ching, & Brewer, 2011). To verify the fitting, real-ear measurements using the Otometrics AURICAL FreeFit (Otometrics A/S, 2016) were obtained. Participants were seated at 0 degrees azimuth to the speaker at a distance of 100 cm. Insertion gain curves using the International Speech Test Signal (Holube, Fredelake, Vlaming, & Kollmeier, 2010) were obtained at 55, 65, and 80 dB SPL ensuring correct calibration for open fittings. All targets were matched within +5 dB for octave frequencies 250 to 4000 Hz for all participants at all levels.
Participants were then instructed in HA management and reminded to wear the HAs all day for the next 2 weeks, while continuing to complete at least three surveys per day. After the 2-week trial with HAs, which constituted the intervention phase, participants then continued 1 more week of surveys, without wearing the HAs. Participants were contacted by telephone or e-mail, according to their preference, to remind them to stop wearing the HAs after the intervention phase but to continue to complete at least three listening event surveys per day using the smartphone for 1 week to return participants to the prefitting baseline conditions.
During the third appointment, at the end of the 1-week withdrawal phase, participants were debriefed and completed a paper-and-pencil version of the IOI-HA (Cox & Alexander, 2002). While IOI-HA would normally be administered immediately following, or during, a HA trial, a 1-week delay in administration was necessary for practical reasons in this study.
The timeframe between the first and the second appointment was exactly 7 days for each of the 10 participants. The 2-week trial with HAs was 14 days for each participant, as they were reminded via e-mail or telephone to stop wearing the HA at that time point, and the third/final appointment was booked at the time of the first appointment and was 28 days from that date.
Data Analysis
Answers to the four hearing performance dimensions of speech understanding, effort required to listen effectively, hearing difficulties negatively effecting or hampering communication, and enjoyment of the listening events (Questions 11–14 of the listening event survey) were coded according to the number of response options and to ensure the highest scores showed the best self-rated performance. For Question 11 (“On average, how much speech did you understand during the listening event?”), if the participant responded 0% the question was scored a 0, if the response was “100%” it was scored 10. For Question 12 (“On average, how much effort did you have to put in to listen effectively?”), if the participant responded “a lot of effort” the question was scored 1, if the response was “no effort” it was scored 5. For Questions 13 and 14 (“Do you feel that any difficulty with your hearing negatively affected or hampered communication during this listening event?” and “Do you feel your hearing negatively affected your enjoyment of this listening event?,” respectively), if the participant responded “very much” the question was scored 1, and if they responded “not at all” the score was 5. The differences in mean scores on these questions over the three phases (baseline, intervention, and withdrawal) were calculated. In addition, individual data were analyzed.
Visual inspection is the most conventional approach to data analysis in SSED studies (Byiers et al., 2012). However, this method has been criticized for not being reliable in quantifying intervention effects and possibly leading to Type 1 errors (Beeson & Robey, 2006; Ottenbacher, 1986). Beeson and Robey (2006) showed calculations of effect size (ES) can identify quantifiable treatment effect in SSED studies, in particular with repeated measures of dimensions of interest across the baseline and intervention phases. This study utilized the same ES calculation, a variation on Cohen’s d statistic (Cohen, 1988), as proposed by Busk and Serlin (1992). As there is no universally accepted benchmarks for ES for HA provision, the within-subjects ES proposed in the meta-analysis on HA benefit with mild HI by Johnson et al. (2016) were used as benchmark; d ≥ 0.37, 0.93, and 1.47 for small, medium, and large effects, respectively.
Linear and mixed-effect models have been shown to be useful and valid for EMA data analysis (Hedeker, Mermelstein, & Demirtas, 2012). Therefore, data analysis was also conducted using mixed-effect modeling. The differences in hearing performance scores across the three conditions (baseline, intervention, and withdrawal) were analyzed using mixed-effect modeling. As the data collected were within-subject repeated measures, the participant was the fixed effect and the condition was the random effect.
A comparison of the IOI-HA data to normative data published by Cox, Alexander, and Beyer (2003) was made using independent samples t test analysis. All statistical analyses were conducted using Stata Version 13 (StataCorp, 2013).
Results
The total number of individuals listening event surveys completed over the 4-week data collection period was 860, with a mean of 86 (range = 63–113, SD = 13.94) per participant. The number of listening event surveys completed over the three conditions varied as expected, with 24.1 mean number of surveys completed by each participant during the baseline phase, 42.3 during the intervention, and 19.6 during the withdrawal phase being. As no significant differences were found between the listening event surveys from the first week and from the second week of the 2-week intervention phase (aided condition), data from both weeks of the intervention phase were used for data analysis.
Of all 860 listening events, 52% involved conversation with three or fewer people, 22% involved speech listening to media such as TV or radio, 15% involved conversation with four or more people, 6% were conversations on the telephone, 4% involved listening to live speech such as a presentation or a seminar, and 1% involved listening to nonspeech sounds such as music. The participants reported no problems in either the use of the research equipment or the management of the open-fit mini-behind-the-ear HAs.
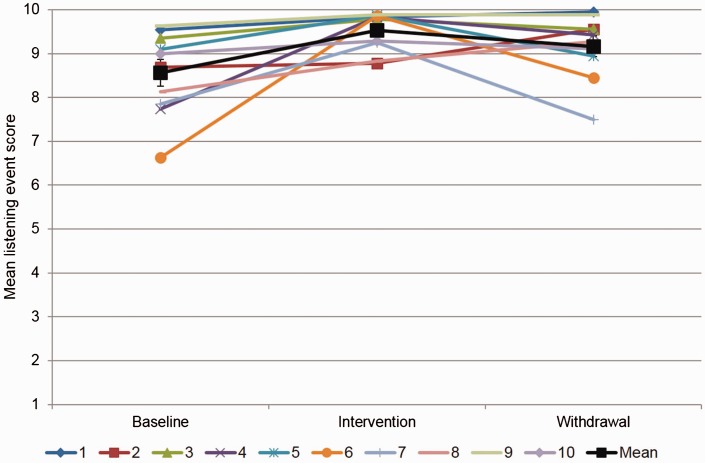
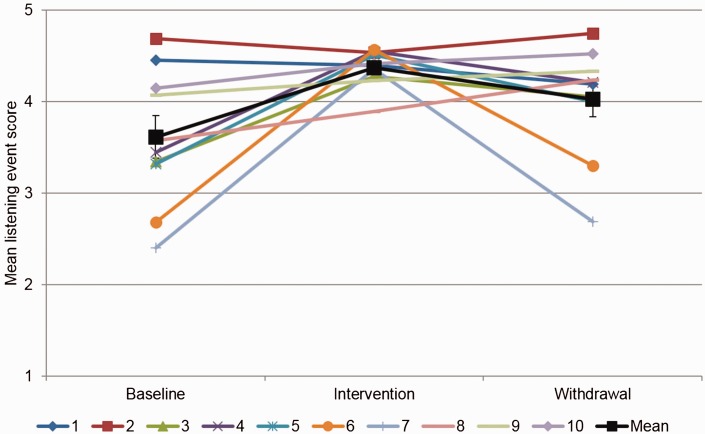
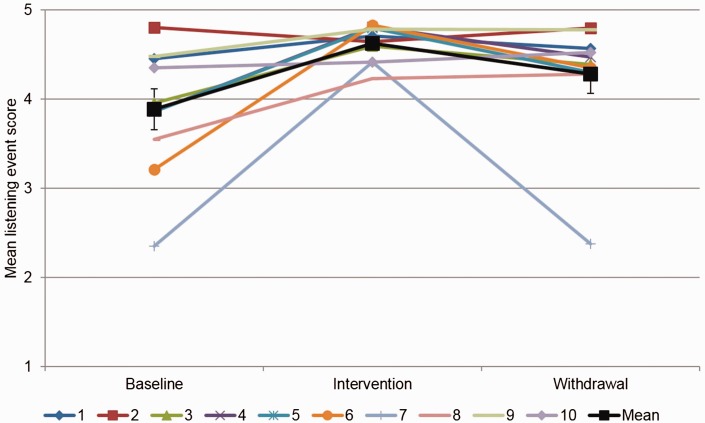
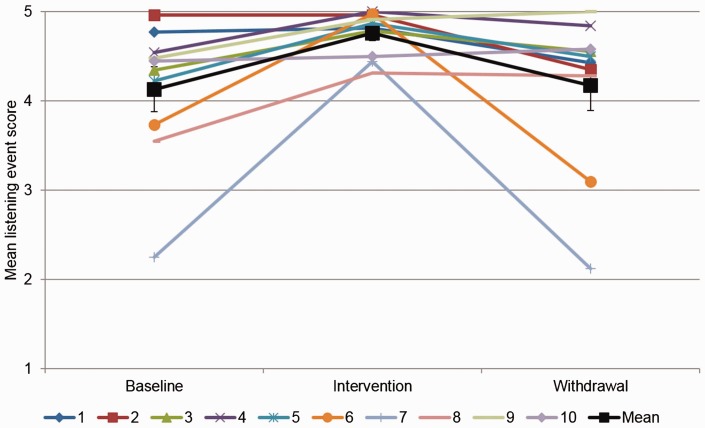
Figures 1 to 4 show the participant and group means for the baseline, intervention (2-week HA trial), and withdrawal (removal of HAs) phases, for the hearing performance dimensions of speech understanding, listening effort, hampered communication, and enjoyment of listening events. The error bars on the group mean show the standard error of the mean.
Figure 1.
Participant and group means of all individual listening event surveys answering the question “On average, how much speech did you understand during the listening event?”
Figure 2.
Participant and group means of all individual listening event surveys answering the question “On average, how much effort did you have to put in to listen effectively?”
Figure 3.
Participant and group means of all individual listening event surveys answering the question “Do you feel that any difficulty with your hearing negatively affected or hampered communication during this listening event?”
Figure 4.
Participant and group means of all individual listening event surveys answering the question “Do you feel your hearing negatively affected your enjoyment of this listening event?”
Mixed-effect model analysis showed the effect of the data collection condition (the 1-week baseline phase without HAs, 2-week intervention phase with HAs, and the final 1-week withdrawal phase without HAs) had on the four hearing performance dimensions (see Table 4). The positive regression coefficients for the baseline versus intervention indicated that wearing a HA had a positive effect on each of the performance dimensions. Equally, all four hearing dimensions showed a negative regression coefficient for the intervention versus withdrawal comparisons, suggesting that when the participant stopped wearing the HA, hearing performance in the four dimensions decreased.
Table 4.
Results of Mixed Model Analysis of Condition on Dimensions of Hearing Performance.
| Hearing performance dimension | Condition | Regression coefficient | 95% CI | p value |
|---|---|---|---|---|
| Speech understanding | Intervention vs. Baseline | 0.90 | [0.65, 1.15] | <.01 |
| Withdrawal vs. Baseline | 0.56 | [0.15, 0.98] | <.01 | |
| Withdrawal vs. Intervention | −0.33 | [−0.59, −0.07] | .01 | |
| Listening effort | Intervention vs. Baseline | 0.71 | [0.56, 0.86] | <.01 |
| Withdrawal vs. Baseline | 0.40 | [0.19, 0.60] | <.01 | |
| Withdrawal vs. Intervention | −0.31 | [−0.47, −0.16] | <.01 | |
| Hampered communication | Intervention vs. Baseline | 0.71 | [0.57, 0.85] | <.01 |
| Withdrawal vs. Baseline | 0.40 | [0.18, 0.61] | <.01 | |
| Withdrawal vs. Intervention | −0.31 | [−0.46, −0.16] | <.01 | |
| Enjoyment | Intervention vs. Baseline | 0.61 | [0.44, 0.77] | <.01 |
| Withdrawal vs. Baseline | 0.05 | [−0.22, 0.32] | NS | |
| Withdrawal vs. Intervention | −0.56 | [−0.73, −0.39] | <.01 |
Note. 95% CI = 95% confidence interval; NS = not significant.
The participants’ self-rated hearing performance did not return to the baseline levels during the withdrawal phase, with the exception of enjoyment of listening events.
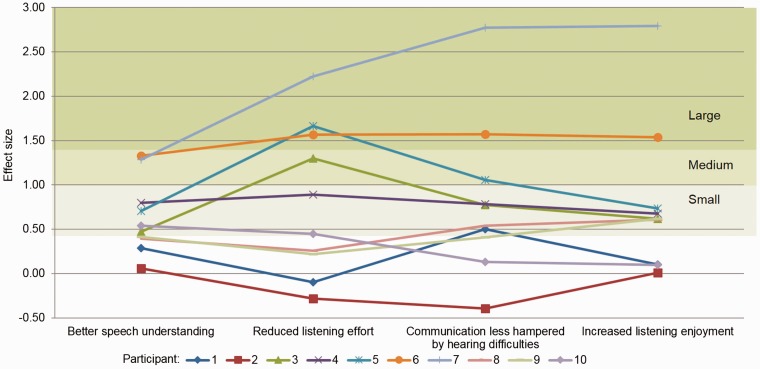
Mean ES was calculated using the 658 baseline and intervention listening event surveys collected from the 10 participants. The use of HAs during the intervention phase showed an ES of d = 0.63 (95% confidence intervals [CIs] = 0.37–0.88) on speech understanding, a mean ES of d = 0.82 (95% CIs = 0.30–1.34) on reducing listening effort, a mean ES of d = 0.81 (95% CIs = 0.28–1.35) on reducing how hearing difficulty hampered communication, and a mean ES of d = 0.78 (95% CIs = 0.26–1.29) on increasing enjoyment of listening events, using the modified Cohen’s d ES calculation. Overall ES on the four communication dimensions was d = 0.76 (95% CIs = 0.37–1.20), although individual participant variations in ES were evident and are shown in Figure 5.
Figure 5.
Individual ES on four hearing performance dimensions for all 10 participants. The shaded areas labeled small, medium, and large correspond to the ES benchmarks from Johnson et al. (2016).
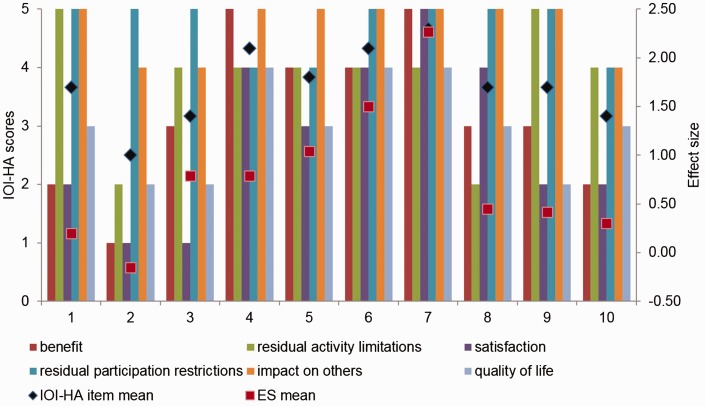
Figure 6 shows the individual IOI-HA scores for each participant and their mean IOI-HA scores as well as their overall HA ES calculated from their individual ES for speech understanding, effort, hampered communication, and enjoyment (Questions 11–14 on the EMA survey). As all participants reported using the HAs every day during the 2-week trial for more than 8 hours/day, the IOI-HA question regarding HA use is not shown and was excluded from the mean calculation. Mean total IOI-HA outcome scores for the participants ranged from 2.5 (out of 5) for Participant 2 to 4.7 for Participant 7.
Figure 6.
Individual IOI-HA question scores, mean IOI-HA score for Items 2 to 7 and mean ES on four hearing performance dimensions, for each participant, n = 10. IOI-HA = International Outcome Inventory for Hearing Aids; ES = effect size.
Calculating the group means for individual IOI-HA questions (Table 5), the lowest group mean was 2.8 (out of 5) for the dimension of satisfaction (measured by the question “Are HAs worth the trouble?”), and the highest group means were 4.7 for the dimensions of residual participation restrictions (“With HAs, how much did hearing difficulties affect things you can do?”) and impact on others (“With HAs, how much do you think others were bothered by your hearing difficulties?”).
Table 5.
Group Mean and SD for All IOI-HA Items for Participants in This Study, n = 10, and Normative Group Mean and SD for Individuals Who Report Mild or Moderate Hearing Difficulties, n = 71, From Cox et al. (2003).
| This study |
Cox et al.
(2003)
|
|||
|---|---|---|---|---|
| IOI-HA Item | Mean | SD | Mean | SD |
| HA usea | 5.00 | 0.00 | 3.73 | 1.17 |
| Benefit | 3.20 | 1.32 | 3.39 | 0.98 |
| Residual activity limitation | 3.80 | 1.03 | 3.40 | 0.95 |
| Satisfaction | 2.80 | 1.40 | 3.20 | 1.21 |
| Residual participation restrictiona | 4.70 | 0.48 | 3.57 | 1.13 |
| Impact on othersa | 4.70 | 0.48 | 3.79 | 1.13 |
| Quality of life | 3.00 | 0.82 | 3.19 | 0.93 |
Note. SD = standard deviation; IOI-HA = International Outcome Inventory for Hearing Aids.
aSignificant difference between mean in this study compared to normative data, p < .01.
Table 5 also shows the group normative mean reported by Cox et al. (2003). Using independent samples t test analysis, HA use was significantly higher in this study, t(79) = 9.15, p < .01, reflecting the instructions to participants to wear the HAs all day, every day. Participants in this study reported statistically significant better outcomes in terms of residual participant restrictions, t(79) = 5.56, p < .01, and impact on others, t(79) = 4.48, p < .01, compared to the normative data. Other differences between the IOI-HA item means in this study and the normative data were not statistically significant. This may be reflective of the clinical population of this study (mild HI only) compared to the greater range of HI in the Cox et al. (2003) study.
Discussion
This pilot study aimed to answer two research questions: Can EMA be used to measure differences in performance with and without HAs in older adults with a mild HI and can HAs provide benefit for adults with a mild HI in daily life, as measured by EMA?
The results show that in this cohort of older adults with mild HI, EMA is able to measure differences in performance with and without HAs, on a number of hearing performance dimensions. Figures 1 to 4 indicate the participants scored their hearing performance on average significantly better with HAs compared to the baseline condition without HAs. On average, participants reported significantly better speech understanding and less listening effort during the 2-week trial with HAs. In addition, they reported that they were significantly less hampered by their hearing difficulties and had greater enjoyment of listening events when wearing HAs.
Comparison of the participants’ IOI-HA scores to their EMA data suggests that EMA as used in this study provided additional insight into HA outcomes for the individuals with mild HI beyond what was possible with the IOI-HA. The EMA methodology allowed numerous questions about listening events to be asked in real time and did not rely on the person with HI having to recall their experiences after they had occurred or to do so for generalized listening situations.
Although the two participants with the lowest and highest IOI-HA scores also showed the lowest and highest ES (Participants 2 and 7, Figure 6), the data from other participants were more variable. This was expected, as the nature of the questions in the IOI-HA are different to those incorporated in the EMA survey. For example, Participant 3 had the second lowest IOI-HA score in this cohort, suggesting that this participant gained little benefit from HAs. EMA for this participant indicated that they rated their speech understanding to be excellent, even during baseline and withdrawal (unaided) data collection phases (see Figure 1). However, EMA data for Participant 3 did indicate that the HAs significantly reduced listening effort in daily listening situations (Figure 2). The IOI-HA frames the dimension of benefit as “help in a situation where you most wanted to hear better” which is highly suggestive of a rating of speech understanding. Individuals with mild HI often rate their speech understanding as high and improvement may be limited due to a ceiling effect. HA benefit for these individuals may take the form of better enjoyment of the listening situation, or in the case of Participant 3, less effort required to hear effectively and this would not be reflected in outcome measures such as the IOI-HA.
From this pilot study, it is evident that the EMA approach has potential as a HA outcome measure for adults with mild HI, as it was able to detect change in self-rated hearing performance, thereby answering the first research question in the affirmative.
The second research question can also be answered in the affirmative; from the results seen in this study, HAs may provide benefit to adults with mild HI. The mixed-model analysis indicated that a short trial with HAs resulted in significantly improved speech understanding, less listening effort, hearing difficulties hampering communication less, and greater enjoyment of listening events for this cohort (Table 4). If HA benefit is quantified based on the ES benchmarks proposed by Johnson et al. (2016), the group mean ES of d = 0.76 with 95% CIs of 0.37 and 1.20 would suggest that the older adults with mild HI in this study showed a small to medium HA ES.
This study used the Johnson et al. (2016) ES benchmarks, as these were extracted from papers focused on HA benefit for adults with mild HI. However, the benchmarks were calculated from only five studies, of which some included participants with greater degrees of HI and did not report results for participants with only mild HI separately. A previous meta-analysis by Chisolm et al. (2007) focused on changes in health-related quality of life with HA provision and reported higher ES benchmarks of d ≥ 0.48, 1.21, and 1.95 for small, medium, and large effects, respectively. These were based on 15 papers (of 16 papers included in the review) that allowed calculation of ES. The mean within-subjects ES of 1.01 (with 95% CIs of 0.76 and 1.26) obtained using disease-specific outcomes suggested that HAs have a small to medium effect on quality of life. Those 15 studies included participants with a wide range of age and degree of HI, although the majority were first-time HA users. Future research on HA provision for adults with mild HI is required to further develop a within-subject HA ES for this clinical population.
EMA facilitated the exploration and quantification of both groups as well as individual HA benefits (Figure 5). Only Participant 2 reported no HA benefit when defined as a positive change in baseline versus intervention scores in hearing performance. One participant indicated benefit on three of four hearing performance dimensions and eight participants improved on all four dimensions. Figure 5 shows that HA benefit within this cohort varied individually; Participants 6 and 7, for example, had a medium to large ES from the provision of HAs while Participant 2 showed negative to no effect from the HAs. Using these ES calculations as criteria, a conclusion could be reached that Participant 2 may not be a candidate for continuing with HAs. Participant 1 showed a small ES only on the dimension of hearing difficulties hampering communication which would suggest the need to further explore the experiences with HAs with this participant.
Figures 1 to 4 and Table 4 show that during the withdrawal phase, when HAs were not worn following 2 weeks of HA experience, the participants’ self-rated hearing performance did not return to the baseline levels, with the exception of enjoyment of listening events. In the case of ratings of speech understanding, listening effort, and hearing difficulties hampering communication, the withdrawal mean performance scores were significantly higher than the baseline means. In other words, participants rated their hearing performance to be better during the withdrawal phase than the baseline phase, although they were not wearing HAs in both these conditions. This could be due to the 2-week trial with HAs and better awareness of their communication abilities with and without HAs. Alternatively, the trend may suggest a form of disability denial. An exploratory study by Arthur, Watts, Davies, Manchaiah, and Slater (2016) suggested that some participants may show disability denial when asked about their hearing, as a coping mechanism. By overrating their hearing performance in the last week of this study, the participants may have hoped to show that they function well without HAs. This could be expected particularly from the six participants who rated their attitude toward HAs as neutral or negative, although this was not evident from the data. For example, the participant with the lowest ES (Participant 2) had a positive attitude toward HAs while the participant with the highest ES (Participant 7) had a neutral attitude toward HAs. It would require a follow-up study with a larger sample size to determine the interaction between a participant’s attitude to HAs and their real-world hearing performance ratings or to further explore differences in participants’ real-world listening experiences in baseline versus withdrawal phases.
There are a number of limitations related to this study, the first due to its design as an SSED study. The findings may be clinically significant, but the degree to which they can be generalized to other individuals may be limited (Glista et al., 2012). The lack of randomization is another limitation; however, SSED studies can be designed to incorporate randomization and blinding and therefore reduce the chance of introducing bias (Byiers et al., 2012).
A second limitation relates to the pilot nature of this study. To the authors’ knowledge, this is the first study that used EMA to detect HA benefit and to compare EMA results to a commonly used, standardized questionnaire. However, the small cohort of 10 older adults had only a 2-week trial with HAs. In recognizing the limitations of this pilot study as well as its positive results, a longer study utilizing the EMA approach with a larger cohort is indicated. Care should be exercised, however, when designing such EMA research, as a long data collection period could lead to participant burden and hence reduced compliance. Rather than a continuous period, breaks in data collection could be introduced. A lengthier study period would also allow a stronger conclusion regarding the benefit of HAs for adults with mild HI. As the recent reviews of HA benefit for adults by Barker et al. (2015) and Ferguson et al. (2017) concluded, there is a need for more long-term outcome assessment of HA benefit. EMA data collection periods of, for example, 2 weeks every 6 months could be feasible to detect changes in HA benefit over a period of years. This would be particularly the case if the EMA app could be installed on participants’ own smartphones rather than needing to supply a dedicated EMA smartphone.
A user-friendly EMA app, available to be installed by the individual or their clinician, could facilitate EMA to move from a research to a clinical tool. Now that EMA has been found to be useful for the collection of HA benefit data, this information could be valuable to clinicians, in terms of candidacy for HAs or other intervention options. Participants in this study used the HAs for at least 8 hours per day because they were instructed to do so. In clinical practice, clients could similarly be asked to trial HAs in this way and to record their experiences using EMA. The degree of benefit from wearing HAs could then be quantified and used by both clinician and client as an indicator of candidature for ongoing HA use.
Similarly, reports of subjective hearing performance when unaided on dimensions such as speech understanding and reduced listening effort (dimensions where HAs have been shown to be able to provide benefit) could be used to determine whether an individual might benefit from HAs. Therefore, EMA could be used to determine possible candidacy in two ways: as an indicator of degree of self-reported difficulty in real life for those considering HA fitting and as an indicator of degree of HA benefit for those trialing HAs.
The use of EMA in research and clinical practice may reveal intraindividual differences in hearing performance beyond listening activity or acoustic environment. For example, investigation of an individual’s EMA surveys could reveal changes in hearing performance related to the time of the day. Furthermore, if patients were given insight into their individual EMA data, much like wearable activity tracking devices (wearables) do, it may encourage enhanced self-management. Chiauzzi, Rodarte, and DasMahapatra (2015) found that the use of wearables gave patients greater control in their health care, placed greater emphasis on a patient’s experience of their chronic health condition, and could potentially improve overall patient engagement.
From a clinical perspective, this study reiterates that a more real-world and patient-centered approach to defining HA outcomes is required than is currently occurring in practice. Figure 5 shows that for the 10 participants, the ES on speech understanding from wearing HAs was less than the benefit received on other hearing performance aspects for most participants. Therefore, if benefit is measured as improvement in speech understanding, as suggested, for example, in the “ease of communication” scale of the Abbreviated Profile of Hearing Aid Benefit (Cox & Alexander, 1995) or the “final ability” section of the Client Oriented Scale of Improvement (Dillon et al., 1997), the reported HA benefit from this cohort would be underestimated. Participant 5, for example, showed that HAs had a stronger effect on reducing listening effort than any of the other three hearing performance dimensions. Participant 8 showed a greater enjoyment of listening events when wearing HAs, but no effect on speech understanding. This study reiterates previous findings that a mild HI may have little bearing on speech understanding in common real-world listening events but greater impact on other aspects that affect daily communication (Eckert, Matthews, & Dubno, 2017; Timmer et al., 2015).
Conclusion
This study has shown that EMA has the potential to measure differences in self-rated hearing performance after the provision of HAs. Second, the study showed that as a whole, HAs may provide benefits to adults with mild HI, particularly when taking hearing performance as a concept beyond speech understanding alone. It also showed that these benefits are individual. The results indicate that a real-world approach to measuring HA outcomes is needed and that this could lead to improved understanding of the benefits of HAs for adults with mild HI.
Acknowledgment
The authors thank Yu-Hsiang Wu, of the University of Iowa, for his input and expertise in the field of ecological momentary assessment.
Note
If participant answers “more than 1 hour ago,” the app reminds them to please try to complete the survey within 1 hour after the event.
Declaration of Conflicting Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a PhD studentship for Barbra H. B. Timmer funded by Sonova AG, Stäfa, Switzerland.
References
- Arthur J., Watts T., Davies R., Manchaiah V., Slater J. (2016) An exploratory study identifying a possible response shift phenomena of the Glasgow Hearing Aid Benefit Profile. Audiology Research 6(2): 44–48. . doi: 10.4081/audiores.2016.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker F., MacKenzie E., Elliott L., de Lusignan S. (2015) Outcome measurement in adult auditory rehabilitation: A scoping review of measures used in randomized controlled trials. Ear and Hearing 36(5): 567–573. . doi: 10.1097/AUD.0000000000000167. [DOI] [PubMed] [Google Scholar]
- Beeson P. M., Robey R. R. (2006) Evaluating single-subject treatment research: Lessons learned from the aphasia literature. Neuropsychology Review 16(4): 161–169. . doi: 10.1007/s11065-006-9013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best V., Keidser G., Buchholz J. M., Freeston K. (2013) Psychometric effects of adding realism to a speech-in-noise test. The Journal of the Acoustical Society of America 133(5): 3379–3379. . doi: 10.1121/1.4805816. [Google Scholar]
- Busk P. L., Serlin R. (1992) Meta-analysis for single case research. In: Kratochwill T. R., Levin J. R. (eds) Single-case research design and analysis: New directions for psychology and education, Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Byiers B. J., Reichle J., Symons F. J. (2012) Single-subject experimental design for evidence-based practice. American Journal of Speech-Language Pathology 21(4): 397–414. . doi: 10.1044/1058-0360(2012/11-0036). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia E. M., Wang J. J., Rochtchina E., Cumming R. R., Newall P., Mitchell P. (2007) Hearing impairment and health-related quality of life: The Blue Mountains Hearing Study. Ear and Hearing 28(2): 187–195. . doi: 10.1097/AUD.0b013e31803126b6. [DOI] [PubMed] [Google Scholar]
- Chiauzzi E., Rodarte C., DasMahapatra P. (2015) Patient-centered activity monitoring in the self-management of chronic health conditions. BMC Medicine 13: 77 doi: 10.1186/s12916-015-0319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chisolm T. H., Johnson C. E., Danhauer J. L., Portz L. J., Abrams H. B., Lesner S., Newman C. W. (2007) A systematic review of health-related quality of life and hearing aids: Final report of the American Academy of Audiology task force on the health-related quality of life benefits of amplification in adults. Journal of the American Academy of Audiology 18(2): 151–183. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical power analysis for the behavioral sciences, Hillsdale, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Cox R. M., Alexander G. C. (1995) The abbreviated profile of hearing aid benefit. Ear and Hearing 16: 176–186. [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C. (2002) The International Outcome Inventory for Hearing Aids (IOI-HA): Psychometric properties of the English version. International Journal of Audiology 41(1): 30–35. [DOI] [PubMed] [Google Scholar]
- Cox R. M., Alexander G. C., Beyer C. M. (2003) Norms for the International Outcome Inventory for Hearing Aids. Journal of the American Academy of Audiology 14: 403–413. [PubMed] [Google Scholar]
- Cox R. M., Gilmore C., Alexander G. C. (1991) Comparison of two questionnaires for patient-assessed hearing aid benefit. Journal of the American Academy of Audiology 2: 134–145. [PubMed] [Google Scholar]
- Desjardins J. L. (2016) Analysis of performance on cognitive test measures before, during, and after 6 months of hearing aid use: A single-subject experimental design. American Journal of Audiology 25(2): 1–15. . doi: 10.1044/2016_Aja-15-0067. [DOI] [PubMed] [Google Scholar]
- Dillon H., James A., Ginis J. (1997) The Client Oriented Scale of Improvement (COSI) and its relationship to several other measures of benefit and satisfaction provided by hearing aids. Journal of the American Academy of Audiology 8(2): 27–43. [PubMed] [Google Scholar]
- Eckert M. A., Matthews L. J., Dubno J. R. (2017) Self-assessed hearing handicap in older adults with poorer-than-predicted speech recognition in noise. Journal of Speech, Language, and Hearing Research 60(1): 251–262. . doi: 10.1044/2016_JSLHR-H-16-0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson, M. A., Kitterick, P. T., Chong, L. Y., Edmondson-Jones, M., Barker, F., & Hoare, D. J. (2017). Hearing aids for mild to moderate hearing loss in adults. Cochrane Database of Systematic Reviews, (9). doi:10.1002/14651858.CD012023.pub2. [DOI] [PMC free article] [PubMed]
- Gatehouse S. (1992) The time course and magnitude of perceptual acclimatization to frequency responses: Evidence from monaural fitting of hearing aids. The Journal of the Acoustical Society of America 92: 1258–1269. [DOI] [PubMed] [Google Scholar]
- Glista D., Scollie S., Sulkers J. (2012) Perceptual acclimatization post nonlinear frequency compression hearing aid fitting in older children. Journal of Speech, Language, and Hearing Research 55(6): 1765–1787. . doi: 10.1044/1092-4388(2012/11-0163). [DOI] [PubMed] [Google Scholar]
- Hedeker D., Mermelstein R. J., Demirtas H. (2012) Modeling between- and within-subject variance in ecological momentary assessment (EMA) data using mixed-effects location scale models. Statistics in Medicine 31(27): doi:10.1002/sim.5338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickson L., Allen J., Beswick R., Fulton M., Wolf D., Worrall L., Scarinci N. (2008) Relationships between hearing disability, quality of life and wellbeing in older community-based Australians. The Australian and New Zealand Journal of Audiology 30(2): 99–111. [Google Scholar]
- Hickson L., Clutterbuck S., Khan A. (2010) Factors associated with hearing aid fitting outcomes on the IOI-HA. International Journal of Audiology 49: 586–595. . doi: 10.3109/14992021003777259. [DOI] [PubMed] [Google Scholar]
- Holube I., Fredelake S., Vlaming M., Kollmeier B. (2010) Development and analysis of an International Speech Test Signal (ISTS). International Journal of Audiology 49: 491–903. . doi: 10.3109/14992027.2010.506889. [DOI] [PubMed] [Google Scholar]
- Humes L. E., Ahlstrom J. B., Bratt G. W., Peek B. F. (2009) Studies of hearing-aid outcome measures in older adults: A comparison of technologies and an examination of individual differences. Seminars in Hearing 30(2): 112–128. . doi: 10.1055/s-0029-1215439. [Google Scholar]
- Johnson C. E., Danhauer J. L., Ellis B. B., Jilla A. M. (2016) Hearing aid benefit in patients with mild sensorineural hearing loss: A systematic review. Journal of the American Academy of Audiology 27(4): 293–310. . doi: 10.3766/jaaa.14076. [DOI] [PubMed] [Google Scholar]
- Kazdin A. E. (1982) Single-case research designs: Methods for clinical and applied settings, New York, NY: Oxford University Press. [Google Scholar]
- Kazdin A. E. (2016) Single-case experimental research designs. In: Kazdin A. E. (ed.) Methodological issues and strategies in clinical research, 4th ed Washington, DC: American Psychological Association, pp. 459–483. [Google Scholar]
- Keidser G., Dillon H., Flax M., Ching T., Brewer S. (2011) The NAL-NL2 prescription procedure. Hearing Research 1(1): 88–90. . doi: 10.4081/audiores.2011.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein M. J., Bess F. H., Logan S. A. (1988) Diagnostic performance of the hearing handicap inventory for the elderly (screening version) against differing definitions of hearing loss. Ear and Hearing 9(4): 208–211. [DOI] [PubMed] [Google Scholar]
- Meyer C., Hickson L., Lovelock K., Lampert M., Khan A. (2014) An investigation of factors that influence help-seeking for hearing impairment in older adults. International Journal of Audiology 53(Suppl 1): S3–S17. . doi: 10.3109/14992027.2013.839888. [DOI] [PubMed] [Google Scholar]
- Moskowitz D. S., Young S. N. (2006) Ecological momentary assessment: What it is and why it is a method of the future in clinical psychopharmacology. Journal of Psychiatry and Neuroscience 31(1): 13–20. [PMC free article] [PubMed] [Google Scholar]
- Otometrics A/S (2016) AURICAL FreeFit and the OTOsuite PMM and counseling and simulations modules: Reference manual, Taastrup, Denmark: Otometrics A/S. [Google Scholar]
- Ottenbacher K. J. (1986) Reliability and accuracy of visually analyzing graphed data from single-subject designs. American Journal of Occupational Therapy 40(7): 464–469. . doi: 10.5014/ajot.40.7.464. [DOI] [PubMed] [Google Scholar]
- Palmer C. V., Adams S. W., Bourgeois M., Durrant J., Rossi M. (1999) Reduction in caregiver-identified problem behaviors in patients with Alzheimer disease post-hearing-aid fitting. Journal of Speech, Language, and Hearing Research 42: 312–328. [DOI] [PubMed] [Google Scholar]
- Salonen J., Johansson R., Karjalainen S., Vahlberg T., Isoaho R. (2011) Relationship between self-reported hearing and measured hearing impairment in an elderly population in Finland. International Journal of Audiology 50(5): 297–302. . doi: 10.3109/14992027.2010.549517. [DOI] [PubMed] [Google Scholar]
- Saunders G. H., Chisolm T. H., Abrams H. B. (2005) Measuring hearing aid outcomes—not as easy as it seems. Journal of Rehabilitation Research and Development 42(4 Suppl 2): 157–168. [DOI] [PubMed] [Google Scholar]
- Schow, R. L., & Nerbonne, M. A. (1982). Communication screening profile: Use with elderly clients. Ear and Hearing, 3(3), 135–147. doi: 10.1097/00003446-198205000-00007. [DOI] [PubMed]
- Shiffman S., Stone A. A., Hufford M. R. (2008) Ecological momentary assessment. Annual Review of Clinical Psychology 4(1): 1–32. . doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Sindhusake D., Mitchell P., Smith W., Golding M., Newall P., Hartley D., Rubin G. (2001) Validation of self-reported hearing loss: The Blue Mountains Hearing Study. International Journal of Epidemiology 30(6): 1371–1378. [DOI] [PubMed] [Google Scholar]
- StataCorp (2013) Stata Statistical Software: Release 13, College Station, TX: StataCorp LP. [Google Scholar]
- Stone A. A., Shiffman S. (2002) Capturing momentary, self-report data: A proposal for reporting guidelines. Annals of Behavioral Medicine 24(3): 236–243. . doi: 10.1207/S15324796ABM2403_09. [DOI] [PubMed] [Google Scholar]
- Tate R. L., Perdices M., McDonald S., Togher L., Rosenkoetter U. (2014) The design, conduct and report of single-case research: Resources to improve the quality of the neurorehabilitation literature. Neuropsychological Rehabilitation 24(3–4): 315–331. . doi: 10.1080/09602011.2013.875043. [DOI] [PubMed] [Google Scholar]
- Timmer, B. H. B. (2017). Adults with mild hearing impairment: Measuring real-world hearing performance (PhD thesis). School of Health & Rehabilitation Sciences, The University of Queensland, Brisbane. doi: 10.14264/uql.2017.987.
- Timmer B. H. B., Hickson L., Launer S. (2015) Adults with mild hearing impairment: Are we meeting the challenge? International Journal of Audiology 54(11): 786–795. . doi: 10.3109/14992027.2015.1046504. [DOI] [PubMed] [Google Scholar]
- Timmer B. H. B., Hickson L., Launer S. (2017. a) Ecological momentary assessment: Feasibility, construct validity and future applications. American Journal of Audiology 26(3S): 436–442. . doi: 10.1044/2017_AJA-16-0126. [DOI] [PubMed] [Google Scholar]
- Timmer B. H. B., Hickson L., Launer S. (2017. b) Hearing aid use and mild hearing impairment: Learnings from big data. Journal of the American Academy of Audiology 28(8): 731–741. . doi: 10.3766/jaaa.16104. [DOI] [PubMed] [Google Scholar]
- Ventry I., Weinstein B. (1982) The hearing handicap inventory for the elderly: A new tool. Ear and Hearing 3(3): 128–134. [DOI] [PubMed] [Google Scholar]
- Ware J. E., Sherbourne C. D. (1992) The MOS 36-Item Short-Form Health Survey (SF-36): I. conceptual framework and item selection. Medical Care 30(6): 473–483. [PubMed] [Google Scholar]
- Williams V. A., Johnson C. E., Danhauer J. L. (2009) Hearing aid outcomes: Effects of gender and experience on patients’ use and satisfaction. Journal of the American Academy of Audiology 20(7): 422–432. . doi: 10.3766/jaaa.20.7.4. [DOI] [PubMed] [Google Scholar]