Abstract
Background:
Rotator cuff tears are the leading cause of shoulder pain and disability. However, the diagnosis of a rotator cuff tear based on patient characteristics, symptoms, and physical examination findings remains a challenge because of a lack of data. Moreover, data on the predictive ability of a combination of these characteristics and tests are not available from a large cohort of patients. Consequently, clinicians rely on expensive imaging, such as magnetic resonance imaging (MRI), to make a diagnosis.
Purpose:
To model patient characteristics, symptoms, and physical examination findings that predict a rotator cuff tear. We present a nomogram based on our predictive model that can be used in patients with shoulder pain to determine the probability of the diagnosis of a rotator cuff tear without the need for imaging.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
We recruited patients from outpatient clinics who were ≥45 years of age and who had shoulder pain of at least 4 weeks’ duration. A rotator cuff tear was diagnosed based on expert clinical impression and the presence/absence of a tear on a blinded review of MRI. Ultimately, 301 patients were included in the analysis.
Results:
A total of 123 patients (41%) had rotator cuff tears, and 178 patients (59%) did not. The predictors of the diagnosis of a rotator cuff tear included external rotation strength ratio of the affected versus unaffected shoulder (odds ratio [OR], 1.20 [95% CI, 1.08-1.34]), male sex (OR, 1.98 [95% CI, 1.10-3.56]), positive lift-off test result (OR, 4.33 [95% CI, 1.46-12.86]), and positive Jobe test result (OR, 9.19 [95% CI, 4.69-17.99]). A nomogram based on these predictor variables was plotted.
Conclusion:
Presented is a model that can accurately predict the diagnosis of a rotator cuff tear with satisfactory discrimination and calibration based on 4 variables: sex, lift-off test, Jobe test, and external rotation strength ratio. Data from this study can be used to aid in the diagnosis of a rotator cuff tear in day-to-day clinical practice in outpatient settings without the need for expensive imaging such as MRI.
Keywords: rotator cuff tears, diagnostic accuracy, predictive modeling
In the United States, shoulder symptoms accounted for an estimated 10.7 million ambulatory care visits to physician offices in 2013.10 The prevalence of shoulder pain in the population ranges from 14% to 34%.2,8,46,50,55,56 Rotator cuff disorders are the underlying issue in 65% to 70% of patients with shoulder pain,11,57 and they accounted for 272,148 surgeries in the United States in 2006.12,27 Recent reports have highlighted the importance of patient symptoms and shoulder examination results in the management of shoulder pain.7 However, the diagnosis of a rotator cuff tear based on patient characteristics, symptoms, and physical examination findings remains a challenge.30 The lack of data on this issue is well documented, and a need for the synthesis of such data has been expressed by leading experts.22,42 As such, there is a heavy reliance on expensive imaging such as magnetic resonance imaging (MRI) to make a diagnosis of a rotator cuff tear.
There are several “special” shoulder physical examinations described for the diagnosis of rotator cuff tears. Data on the diagnostic accuracy of individual special shoulder tests for rotator cuff tears are variable28 and are mostly available from single-site/single-provider studies or retrospective chart reviews.4,25,31,38,39,47,63,64 Several of these studies assessed patient populations undergoing rotator cuff surgery,6,16,17,40,49 which creates a spectrum bias, thus limiting the inferences that can be made to the larger population of patients with rotator cuff tears, most of whom do not undergo surgery. To the best of our knowledge, data from patient characteristics, symptoms, and physical examinations have not been used to build a robust, diagnostic predictive model in a large cohort for use in clinical practice.
In a large cohort of patients with shoulder pain, we modeled patient characteristics, symptoms, and physical examination findings that predict a symptomatic rotator cuff tear. We present a nomogram based on our predictive model that can be used in patients with shoulder pain to determine the probability of the diagnosis of a rotator cuff tear without the need for imaging.
Methods
Patient Population
We recruited a cohort of 390 patients with shoulder pain and/or limitation in range of motion lasting at least 4 weeks and who completed baseline history questionnaires. These patients were recruited from 4 sports medicine/shoulder clinics (3 academic and 1 community) between February 2011 and June 2015. Other inclusion criteria were patients aged ≥45 years because a diagnostic dilemma of shoulder pain is most common in this age group. Patients provided informed consent, and the study was approved by our institutional review board. Exclusion criteria were a current shoulder fracture of the affected shoulder, history of index shoulder surgery, and active cervical radiculopathy. Patients were asked if they had neck pain radiating to the shoulder to elicit cervical radiculopathy. Patients missing information on the degree of clinical certainty of a rotator cuff tear (n = 4), those found to be ineligible after enrollment (n = 1), and those missing physical examination findings (n = 19) were excluded from the analysis.
History and Shoulder Pain/Function Assessment
The structured shoulder and general health questionnaire assessed patient demographics; comorbidities; symptoms; smoking habits; prior treatments, including physical therapy and corticosteroid injections; and occupational history. Patients were asked about their medication use, including acetaminophen, nonsteroidal anti-inflammatory drugs, glucosamine, and narcotics for shoulder pain in the past 2 weeks. Patients also completed the Shoulder Pain and Disability Index (SPADI),51 a standardized 13-item questionnaire. The SPADI has a pain scale (5 items) and a disability scale (8 items) that elicit information on pain and functional limitations with activities of daily living. The composite SPADI score ranges from 0 to 100, with higher scores reflecting worse pain and function.
Physical Examination Protocol
Special Tests
Our standardized physical examination protocol has been previously published and was based on the original descriptions of the special shoulder tests.28,29 Briefly, shoulder special tests were performed by a physician/orthopaedic physician assistant trained in our research protocol. The research protocol was developed before the recruitment of patients. The 13 shoulder special tests that were performed included the lift-off test,17 passive lift-off test,16 belly-press test,16 belly-off sign,53 and bear hug test6 for the subscapularis; the external rotation lag sign at 0°,23 external rotation lag sign at 90°,23 Jobe test (empty can test),32,33 full can test,36 Neer sign,48 Hawkins-Kennedy sign,20 and drop arm test60 for the infraspinatus and supraspinatus; and the hornblower sign58 for the teres minor/infraspinatus. Good interrater and intrarater reliability have been reported for the performance of many of these tests.9,15,34,43
Strength Testing
Strength testing was performed using a handheld dynamometer in abduction, external rotation, and internal rotation by trained research assistants. Both the affected and contralateral shoulders were assessed, and a mean of 2 consecutive measurements that were at least 10 seconds apart was used in our analysis. Our detailed protocol for standardized strength testing has been previously described.29,45 Strength testing using a dynamometer has good intrarater and interrater reliability.21 We used a ratio of the affected shoulder strength versus the contralateral shoulder strength in our analysis.
Diagnostic Imaging
Shoulder MRI scans were read in a blinded fashion by consensus of 2 shoulder experts (L.D.H. and N.B.J. or J.E.K. and N.B.J.). Although this was a pragmatic cohort with no specific requirements for MRI, most patients underwent MRI on a 1.5-T or 3.0-T magnet with a dedicated shoulder coil. The following sequences were usually obtained: coronal oblique fast spin echo (FSE) proton density–weighted images, coronal oblique FSE short tau inversion recovery (STIR) images, sagittal FSE proton density– or T2-weighted images with fat suppression, sagittal FSE T1-weighted images, axial T1-weighted images, and axial T2-weighted gradient echo images. Scans were read at least 2 months after the clinical encounter. Our previous work has shown good interrater and intrarater reliability for these MRI readings as compared with those of a musculoskeletal radiologist. Kappa values ranged from 0.75 to 0.90 for tear presence, tear size, and tear thickness.26 MRI features that were assessed in a standardized manner included tear thickness, tear size in the longitudinal and transverse planes, fatty infiltration of the rotator cuff muscles, and rotator cuff muscle atrophy. Criteria for each of these measurements have been previously described26 and follow standard radiology methodology.
Diagnosis of Rotator Cuff Tears (Reference Standard)
Prior literature has shown structural evidence for rotator cuff tears even in asymptomatic patients.44,54,61,62 Moreover, a rotator cuff tear is a clinical syndrome, and a case definition simply based on imaging findings is incomplete and clinically inaccurate. Our study was designed to account for this issue because an accurate case definition is paramount for our results to be valid. In addition to our standardized protocol for assessing the structural presence of a rotator cuff tear on MRI, a fellowship-trained shoulder or sports medicine attending physician performed an independent clinical assessment (by history and physical examination). The attending physician then rated the degree of certainty that the patient’s symptoms were clinically attributable to a rotator cuff tear on a scale ranging from 0 (certainly not a tear) to 100 (certainly a tear). If the degree of certainty was marked as ≥50 and a tear was documented on the blinded MRI review, the patient was considered to have a clinical diagnosis of a rotator cuff tear. If the degree of certainty was marked as <50, the patient was considered not to have a clinical diagnosis of a rotator cuff tear.
In our analysis, we excluded 65 patients who had a degree of certainty of ≥50 but (1) who did not undergo MRI because it was not clinically indicated/ordered (n = 31) or (2) whose MRI did not show a structural deficit indicating a rotator cuff tear (n = 34). Thus, 301 patients were included in our final analysis for this study, termed the Rotator Cuff Outcomes Workgroup (ROW). Patients with a negative MRI finding but a degree of certainty of ≥50 were excluded because the sensitivity of MRI in partial-thickness rotator cuff tears is 64%.13 Thus, it was possible that a structural deficit in the case of a partial-thickness tear was not detected by MRI, which would lead to the misclassification of such patients. This strict definition of a rotator cuff tear ensured that a patient diagnosed as having a tear in our study indeed had a tear.
Statistical Analysis
We followed the methodology described by Harrell19 for creating our predictive model. Among 115 individual and composite variables, 41 variables were selected a priori by clinical judgment as potential predictors. With 123 patients classified as having a rotator cuff tear in our cohort, our goal was to reduce our predictor set to include no more than 12 (123/10) degrees of freedom. A hierarchical cluster analysis based on the Spearman correlation of our initial 41 variables was conducted for an independent review by 2 shoulder-trained clinicians (N.B.J. and J.E.K.) to choose, among highly correlated variables, a relatively independent variable set that would have significant predictive power. Among the 9 variables agreed upon by the 2 independent reviewers, a separate hierarchical cluster analysis and redundancy analysis were conducted. The highest pairwise correlation was <0.1, and the greatest R 2 value with which each variable could be predicted from all the others was 0.184. Nonlinearity of the covariates overall was assessed, and the P value to reject the hypothesis of linearity was not rejected (P = .413). Consequently, our full model was based on 9 variables with 10 degrees of freedom selected without using our primary response.
We used logistic regression to model the probability of a rotator cuff tear with our predictor set. The effect size from this model was the odds ratio, which estimated the increased odds of a rotator cuff tear diagnosis for a unit increase in a given covariate. To account for bias due to missing data, we used predictive mean matching, including variables previously deleted by clinical judgment but correlated to the predictor set, to create 20 inputed data sets for analysis. For each of these 20 data sets, a predictive model was generated, resulting in 20 sets of parameter values and variability estimates. These parameter sets were pooled using Rubin’s52 rules. Model validation and calibration were conducted using 500 bootstrap samples.
Seeking the most parsimonious predictive model (termed the final model), we used ordinary least squares to fit the full model–predicted values with all 9 variables, with backward elimination for each of the 20 imputation data sets. For each of these 20 models, variables were eliminated if they were not in the set of variables, ordered from largest to smallest contribution, with a cumulative R 2 value <0.95. Variables that presented in at least 10 models were retained in the final model for predicting a rotator cuff tear. Model validation of the subsequent 4-variable logistic regression was conducted as described above. A nomogram was also developed.
Results
Of the 301 patients in our cohort who were included in this analysis, 123 (41%) were diagnosed with a rotator cuff tear, and 178 patients (59%) did not have a tear (Table 1). Patients without tears had glenohumeral osteoarthritis, adhesive capsulitis, biceps lesions, impingement syndrome (without a tear), labral tears, and acromioclavicular osteoarthritis as their diagnosis. The mean age for those with a tear was 61.6 ± 8.7 years compared with 59.2 ± 9.0 years for those without a tear. The dominant shoulder was affected in a majority of patients with (68%) and without (54%) a tear. The median SPADI score was lower in patients without a tear versus those with a tear (40 vs 50, respectively).
TABLE 1.
Baseline Characteristics of the ROW Cohort by the Presence of Rotator Cuff Tearsa
| Rotator Cuff Tear (n = 123) | No Rotator Cuff Tear (n = 178) | |
|---|---|---|
| Sex | ||
| Female | 49 (40) | 95 (53) |
| Male | 74 (60) | 83 (47) |
| Age, y | ||
| 25th/50th (median)/75th percentiles | 54.0/63.0/66.9 | 51.3/58.6/66.6 |
| Mean ± SD | 61.6 ± 8.7 | 59.2 ± 9.0 |
| Dominant shoulder affected? | ||
| Yes | 84 (68) | 97 (54) |
| No | 35 (28) | 70 (39) |
| Missing | 4 (3) | 11 (6) |
| Daily shoulder use at work? | ||
| Heavy/moderate manual work | 35 (28) | 29 (16) |
| Light/no manual labor | 83 (67) | 139 (78) |
| Missing | 5 (4) | 10 (6) |
| Lift-off test | ||
| Positive | 18 (15) | 8 (4) |
| Negative | 76 (62) | 152 (85) |
| Unable to perform | 6 (5) | 5 (3) |
| Missing | 23 (19) | 13 (7) |
| Jobe test | ||
| Positive | 91 (74) | 57 (32) |
| Negative | 13 (11) | 116 (65) |
| Missing | 19 (15) | 5 (3) |
| Use of medication for shoulder pain/corticosteroid injection | ||
| Yes | 106 (86) | 125 (70) |
| No | 17 (14) | 53 (30) |
| External rotation strength ratiob | ||
| 25th/50th (median)/75th percentiles | 0.44/0.62/0.86 | 0.67/0.86/0.99 |
| Mean ± SD | 0.63 ± 0.30 | 0.85 ± 0.26 |
| SPADI score | ||
| 25th/50th (median)/75th percentiles | 34/50/69 | 24/40/58 |
| Mean ± SD | 51 ± 22 | 42 ± 23 |
aData are shown as n (%) unless otherwise indicated. ROW, Rotator Cuff Outcomes Workgroup; SPADI, Shoulder Pain and Disability Index.
bRatio of the affected versus contralateral shoulder.
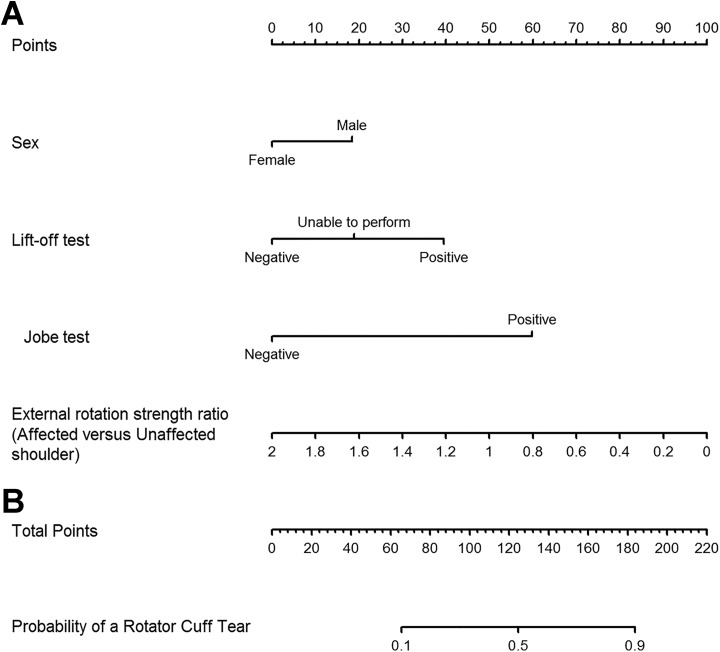
Our final model was derived using bootstrapped backward elimination of the full model variable fitted to the predicted values of the full model. The subsequent final model variable set was refit to the observed outcome. External rotation strength ratio, sex, lift-off test, and Jobe test constituted the final set of significant predictors of the diagnosis of a rotator cuff tear (Table 2 and Figure 1).
TABLE 2.
Predictors of the Diagnosis of a Rotator Cuff Tear (Final Model)
| Odds Ratio (95% CI) | |
|---|---|
| External rotation strength ratio (affected vs contralateral shoulder) | 1.20 (1.08-1.34) |
| Sex (male vs female) | 1.98 (1.10-3.56) |
| Lift-off test (positive vs negative) | 4.33 (1.46-12.86) |
| Lift-off test (unable to perform vs negative) | 2.01 (0.46-8.75) |
| Jobe test (positive vs negative) | 9.19 (4.69-17.99) |
Figure 1.
Odds ratios with CIs for the probability of a rotator cuff tear (final model). The bars represent 90% (dark blue), 95% (light blue), and 99% (gray) CIs for the odds ratios.
A patient with a positive Jobe test result was 9.19 (95% CI, 4.69-17.99) times more likely to have a rotator cuff tear versus a patient with a negative test result. The lift-off test had an odds ratio of 4.33 (95% CI, 1.46-12.86) for a positive versus negative test finding. The full model with additional variables (age, SPADI score, affected shoulder, shoulder use at work, and use of medications/corticosteroid injection in addition to variables in the final model) is presented in the Appendix (Table A1 and Figures A1 and A3).
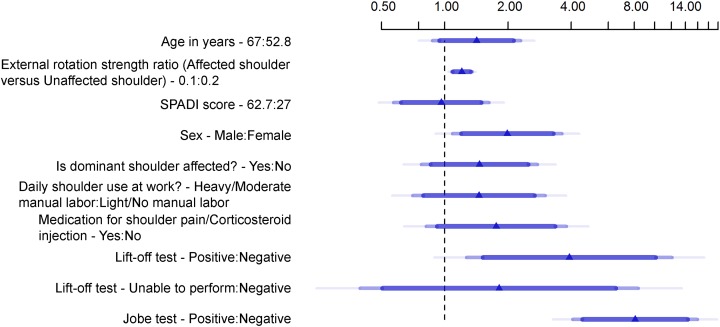
For ease of use in clinical settings, we plotted a nomogram with each of the significant variables in our final model (Figure 2A). The nomogram can be used to calculate the probability of a rotator cuff tear (Figure 2B). For instance, a male patient (20 points) with a positive lift-off test result (40 points), positive Jobe test result (∼60 points), and external rotation strength ratio of 1 (∼50 points) has a cumulative score of approximately 170 points and has a probability exceeding 80% for the diagnosis of a rotator cuff tear. We generated a table with various possible clinical scenarios and the corresponding probability of a rotator cuff tear (Table A2). A similar nomogram is also available for our full model, which includes additional variables (Figure A2).
Figure 2.
Nomogram to predict the probability of a rotator cuff tear (final model). (A) The values of a predictor variable for a patient are compared via a perpendicular line with the points scale. This is repeated for all variable values for a patient, and the total sum of points is calculated. (B) The total points value is then located on the total points scale, and the estimated probability of a rotator cuff tear for that patient is found by dropping a vertical line down to the probability line. SPADI, Shoulder Pain and Disability Index.
A calibration curve for our final model showed almost perfect overlap of predicted versus actual values (slope = 0.95) for the diagnosis of a rotator cuff tear (Figure 3). The corrected c-index for this model was 0.83. The van Houwelingen–Le Cessie heuristic shrinkage estimate was 0.956, suggesting that our final model would validate an independent data set only approximately 4.4% worse than our data set.
Figure 3.
Calibration curve for the fitted final model. Small vertical lines at the top of the graph denote the frequency of predicted probabilities for the patient set. The apparent line depicts the relationship between predicted and observed probabilities of a rotator cuff tear. The bias-corrected line compares predicted probabilities from a bootstrap-corrected model with observed probabilities. These lines are constructed using locally weighted smoothing. The ideal line of perfect agreement originates at the origin (0,0) with a slope of 1.
Discussion
The diagnostic dilemma of a rotator cuff tear in patients with shoulder pain is recognized by experts in the recent literature.22,42 In a large cohort of patients with shoulder pain, our results show that external rotation strength ratio, sex, lift-off test, and Jobe test were significant predictors of the diagnosis of a rotator cuff tear. We constructed a nomogram that can be used in clinical settings to predict the diagnosis of a rotator cuff tear in patients aged ≥45 years presenting with shoulder pain. Thus, data from our study fill a void and the unmet need of clinicians managing patients with shoulder pain in outpatient settings.
Several studies, including data from our cohort, have reported on the sensitivity and specificity of special tests in the diagnosis of rotator cuff tears.4–6,25,28,38,39,47,63 The limitations of prior studies are well described in the literature30 and include data from retrospective chart reviews, recruitment from a single institution/provider, and the use of either MRI or surgical findings as the “gold standard” for the diagnosis of a rotator cuff tear.4–6,25,38,39,47,63,64 The sole use of MRI or arthroscopic visualization for a rotator cuff tear diagnosis, without the inclusion of the clinical impression of an expert, is a major drawback. This methodology assumes that the diagnosis of a rotator cuff tear can be based only on structural findings. Asymptomatic rotator cuff tears documented on imaging are prevalent in approximately 40% of people aged >50 years, 54% of those aged >60 years, and 65% of those aged >70 years.44,54 Thus, the combination of imaging/surgical deficits and clinical findings is essential in making a diagnosis of the clinical syndrome of rotator cuff tear. Our study addresses this issue, although the clinical diagnosis of a rotator cuff tear, as in our study, is subjective. Prior studies that only recruited patients undergoing surgery create a disease spectrum bias because it is likely that patients with more severe disease undergo surgery. This patient population may not represent the majority of patients with rotator cuff tears, especially in primary care settings.
Our study found that in addition to a patient’s sex, the performance of simple physical maneuvers such as the lift-off test and Jobe test as well as the external rotation strength ratio can assist in the diagnosis of a rotator cuff tear. Strength measurements using a handheld dynamometer are easily performed in an office setting (although many practices including shoulder practices may not currently use them on a routine basis). External rotation predominantly measures force exerted by the infraspinatus. We used the ratio of strength of the affected versus contralateral shoulder to account for the variability in shoulder strength among patients by body weight, muscle mass, and sex.
The Jobe test32 or empty can test is performed by first assessing the deltoid with the arm in 90° of abduction and neutral rotation. The shoulder is then internally rotated and angled forward 30° so that the thumb is pointing to the floor. The test result is positive when manual muscle strength is weaker for the second maneuver as compared with the first. Prior studies have reported a sensitivity of 19% to 99%, specificity of 39% to 100%, and likelihood ratio of 0.6 to 2.7 for the Jobe test.4,25,37–39,47,64 Jain et al28 reported a sensitivity of 88% (95% CI, 80%-96%), specificity of 62% (95% CI, 53%-71%), and likelihood ratio of 2.30 (95% CI, 1.79-2.95) for the Jobe test. The Jobe test assesses the supraspinatus tendon, which functions as an abductor of the arm and is also the most commonly torn tendon of the rotator cuff.24 However, there is debate whether the Jobe test assesses exclusively the supraspinatus or multiple muscles. Most of the patients in our cohort had a supraspinatus tear, as would be the case in most clinical settings. Hence, our findings of a large effect size of the Jobe test are plausible. A recent meta-analysis also reported that the Jobe test had the highest pooled diagnostic odds ratio among physical examinations for diagnosing full-thickness rotator cuff tears.18
The lift-off test for subscapularis tears is based on the tendon’s function as an internal rotator. With the clinician’s assistance, the patient touches his or her lower back with the arm fully extended and internally rotated. If the test result is positive, the patient is unable to lift the dorsum of his or her hand off the back. In previous studies, the lift-off test had a sensitivity ranging from 6% to 79% and specificity ranging from 23% to 100% for the detection of subscapularis tears.5,25,38,39,64 A few patients in our cohort were unable to perform the lift-off test (likely because of pain/inability). Hence, we have reported positive lift-off test findings versus negative test findings and also results for those unable to perform the test versus those in whom the test results were negative. It should be noted that the lift-off test may be difficult to perform if the patient is limited in internal rotation movement due to pain.
Our study was performed in a specialty clinic setting. This study design was ideal and was chosen a priori because an accurate clinical diagnosis of a rotator cuff tear was an essential component of the “gold standard.” Reliance on a diagnosis by trained shoulder/sports physicians was the most accurate way to achieve this goal. An expert clinician’s impression has been used in prior studies of disease classification in which no gold standard exists, such as rheumatoid arthritis, spondyloarthropathy, fibromyalgia, spinal stenosis, and osteoarthritis.1,3,14,35,59 This broad clinical concept extends beyond musculoskeletal disorders and is embedded in the classification of acute coronary heart disease and congestive heart failure.41 However, clinical diagnosis is subjective and has a potential for bias.
We did not assess the role of a local anesthetic injection in the subacromial space to diagnose rotator cuff tears or impingement syndrome. Another limitation is the potential variability in the performance of physical examination maneuvers. However, good interrater and intrarater reliability have been reported for strength testing21 and special tests,9,15,34,43 and our protocols were standardized. Our study did not use ultrasound for the diagnosis of rotator cuff tears. MRI offers at least equally reliable information for the structural diagnosis of a rotator cuff tear. In some instances, especially in patients needing surgical intervention, MRI may be required, despite our algorithm showing a high probability of a rotator cuff tear. Our model also does not predict which patients may need surgery. We did not have the sample size to stratify our predictive models by tear thickness and tendon(s) involved. Few patients in our cohort had clinical suspicion of a tear with negative MRI findings or may have had a tear on MRI but were negative based on the clinical impression. This may have introduced a bias.
Conclusion
We present a model that can predict the diagnosis of a rotator cuff tear based on 4 variables—sex, lift-off test, Jobe test, and external rotation strength ratio—without the need for expensive imaging such as MRI. There may be situations, such as considerations for surgery, profound loss of strength, and major traumatic events leading to the current presentation, that may warrant MRI. Clinicians should use their judgment in these situations. Our model predicts the diagnosis of a rotator cuff tear accurately with satisfactory discrimination and calibration. This predictive model can be used by clinicians in the management of patients with shoulder pain when making the diagnosis of a rotator cuff tear and may possibly reduce the reliance on MRI.
APPENDIX
Figure A1.
Odds ratios with CIs for the probability of a rotator cuff tear (full model). The bars represent 90% (dark blue), 95% (light blue), and 99% (gray) CIs for the odds ratios. SPADI, Shoulder Pain and Disability Index.
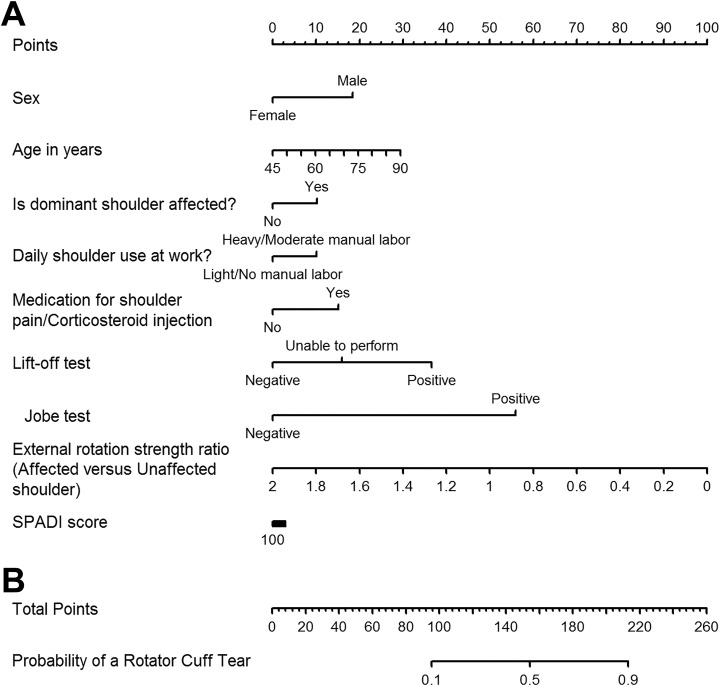
Figure A2.
Nomogram to predict the probability of a rotator cuff tear (full model). (A) The values of a predictor variable for a patient are compared via a perpendicular line with the points scale. This is repeated for all variable values for a patient, and the total sum of points is calculated. (B) The total points value is then located on the total points scale, and the estimated probability of a rotator cuff tear for that patient is found by dropping a vertical line down to the probability line. SPADI, Shoulder Pain and Disability Index.
Figure A3.
Calibration curve for the fitted full model. Small vertical lines at the top of the graph denote the frequency of predicted probabilities for the patient set. The apparent line depicts the relationship between predicted and observed probabilities of a rotator cuff tear. The bias-corrected line compares predicted probabilities from a bootstrap-corrected model with observed probabilities. These lines are constructed using locally weighted smoothing. The ideal line of perfect agreement originates at the origin (0,0) with a slope of 1.
TABLE A1.
Predictors of the Diagnosis of a Rotator Cuff Tear (Full Model)a
| Odds Ratio (95% CI) | |
|---|---|
| Age | 1.02 (0.99-1.06) |
| External rotation strength ratio (affected vs contralateral shoulder) | 1.21 (1.08-1.35) |
| SPADI score | 1.00 (0.98-1.01) |
| Sex (male vs female) | 1.98 (1.09-3.61) |
| Dominant shoulder affected? (yes vs no) | 1.46 (0.77-2.76) |
| Daily shoulder use at work? (heavy/moderate manual labor vs light/no manual labor) | 1.45 (0.70-3.01) |
| Use of medication for shoulder pain/corticosteroid injection (yes vs no) | 1.76 (0.81-3.80) |
| Lift-off test (positive vs negative) | 3.92 (1.27-12.10) |
| Lift-off test (unable to perform vs negative) | 1.81 (0.40-8.33) |
| Jobe test (positive vs negative) | 8.06 (4.06-15.99) |
aSPADI, Shoulder Pain and Disability Index.
TABLE A2.
Probability of a Rotator Cuff Tear for Selected Values of Predictive Variables
| Probability | ||||||
|---|---|---|---|---|---|---|
| 5.0% | 9.4% | 18.4% | 28.6% | 32.4% | 96.9% | |
| External rotation strength ratioa | 1.1 | 1.1 | 1.1 | 0.0 | 1.1 | 0.0 |
| Male sex | (–) | (+) | (–) | (–) | (–) | (+) |
| Positive lift-off test result | (–) | (–) | (+) | (–) | (–) | (+) |
| Positive Jobe test result | (–) | (–) | (–) | (–) | (+) | (+) |
aLow effect value for external rotation strength ratio set at 1.1 to elicit a probability of a rotator cuff tear at 5.0%.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by a Clinical and Translational Science Award (No. UL1TR000445) from the National Center for Advancing Translational Sciences. N.B.J. has grants/grants pending from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grants 1K23AR059199 and 1U34AR069201). L.D.H. has received educational support from Arthrex and Ethicon.
Ethical approval for this study was obtained from Partners HealthCare and Vanderbilt University.
References
- 1. Altman R, Asch E, Bloch D, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–1049. [DOI] [PubMed] [Google Scholar]
- 2. Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993;9(3):174–182. [DOI] [PubMed] [Google Scholar]
- 3. Arnett FC, Edworthy SM, Bloch DA, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–324. [DOI] [PubMed] [Google Scholar]
- 4. Bak K, Sorensen AK, Jorgensen U, et al. The value of clinical tests in acute full-thickness tears of the supraspinatus tendon: does a subacromial lidocaine injection help in the clinical diagnosis? A prospective study. Arthroscopy. 2010;26(6):734–742. [DOI] [PubMed] [Google Scholar]
- 5. Barth J, Audebert S, Toussaint B, et al. Diagnosis of subscapularis tendon tears: are available diagnostic tests pertinent for a positive diagnosis? Orthop Traumatol Surg Res. 2012;98(suppl 8):S178–S185. [DOI] [PubMed] [Google Scholar]
- 6. Barth JR, Burkhart SS, De Beer JF. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006;22(10):1076–1084. [DOI] [PubMed] [Google Scholar]
- 7. Beach H, Gordon P. Clinical examination of the shoulder. New Engl J Med. 2016;375(11):e24. [DOI] [PubMed] [Google Scholar]
- 8. Bergenudd H, Lindgarde F, Nilsson B, Petersson CJ. Shoulder pain in middle age: a study of prevalence and relation to occupational work load and psychosocial factors. Clin Orthop Relat Res. 1988;(231):234–238. [PubMed] [Google Scholar]
- 9. Cadogan A, Laslett M, Hing W, McNair P, Williams M. Interexaminer reliability of orthopaedic special tests used in the assessment of shoulder pain. Man Ther. 2011;16(2):131–135. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention/National Center for Health Statistics. National Ambulatory Medical Care Survey: 2013 state and national summary tables. Available at: https://www.cdc.gov/nchs/ahcd/web_tables.htm#2013. Accessed May 2, 2017.
- 11. Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis Rheum. 1991;34(6):766–769. [DOI] [PubMed] [Google Scholar]
- 12. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94(3):227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009;192(6):1701–1707. [DOI] [PubMed] [Google Scholar]
- 14. Dougados M, van der Linden S, Juhlin R, et al. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991;34(10):1218–1227. [DOI] [PubMed] [Google Scholar]
- 15. Dromerick AW, Kumar A, Volshteyn O, Edwards DF. Hemiplegic shoulder pain syndrome: interrater reliability of physical diagnosis signs. Arch Phys Med Rehabil. 2006;87(2):294–295. [DOI] [PubMed] [Google Scholar]
- 16. Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78(7):1015–1023. [DOI] [PubMed] [Google Scholar]
- 17. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle: clinical features in 16 cases. J Bone Joint Surg Br. 1991;73(3):389–394. [DOI] [PubMed] [Google Scholar]
- 18. Gismervik SO, Drogset JO, Granviken F, Ro M, Leivseth G. Physical examination tests of the shoulder: a systematic review and meta-analysis of diagnostic test performance. BMC Musculoskelet Disord. 2017;18(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. 2nd ed New York: Springer; 2015. [Google Scholar]
- 20. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8(3):151–158. [DOI] [PubMed] [Google Scholar]
- 21. Hayes K, Walton JR, Szomor ZL, Murrell GA. Reliability of 3 methods for assessing shoulder strength. J Shoulder Elbow Surg. 2002;11(1):33–39. [DOI] [PubMed] [Google Scholar]
- 22. Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease? The Rational Clinical Examination systematic review. JAMA. 2013;310(8):837–847. [DOI] [PubMed] [Google Scholar]
- 23. Hertel R, Ballmer FT, Lombert SM, Gerber C. Lag signs in the diagnosis of rotator cuff rupture. J Shoulder Elbow Surg. 1996;5(4):307–313. [DOI] [PubMed] [Google Scholar]
- 24. Hijioka A, Suzuki K, Nakamura T, Hojo T. Degenerative change and rotator cuff tears: an anatomical study in 160 shoulders of 80 cadavers. Arch Orthop Trauma Surg. 1993;112(2):61–64. [DOI] [PubMed] [Google Scholar]
- 25. Itoi E, Minagawa H, Yamamoto N, Seki N, Abe H. Are pain location and physical examinations useful in locating a tear site of the rotator cuff? Am J Sports Med. 2006;34(2):256–264. [DOI] [PubMed] [Google Scholar]
- 26. Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R. 2015;7(3):245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014;15(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jain NB, Luz J, Higgins LD, et al. The diagnostic accuracy of special tests for rotator cuff tear: the ROW cohort study. Am J Phys Med Rehabil. 2017;96(3):176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jain NB, Wilcox RB, 3rd, Katz JN, Higgins LD. Clinical examination of the rotator cuff. PM R. 2013;5(1):45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jain NB, Yamaguchi K. History and physical examination provide little guidance on diagnosis of rotator cuff tears. Evid Based Med. 2014;19(3):108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jia X, Petersen SA, Khosravi AH, Almareddi V, Pannirselvam V, McFarland EG. Examination of the shoulder: the past, the present, and the future. J Bone Joint Surg Am. 2009;91(suppl 6):10–18. [DOI] [PubMed] [Google Scholar]
- 32. Jobe FW, Jobe CM. Painful athletic injuries of the shoulder. Clin Orthop Relat Res. 1983;(173):117–124. [PubMed] [Google Scholar]
- 33. Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med. 1982;10(6):336–339. [DOI] [PubMed] [Google Scholar]
- 34. Johansson K, Ivarson S. Intra- and interexaminer reliability of four manual shoulder maneuvers used to identify subacromial pain. Man Ther. 2009;14(2):231–239. [DOI] [PubMed] [Google Scholar]
- 35. Katz JN, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis: diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38(9):1236–1241. [DOI] [PubMed] [Google Scholar]
- 36. Kelly BT, Kadrmas WR, Speer KP. Empty can versus full can exercise for rotator cuff rehabilitation: an electromyographic analysis. Orthop Trans. 1997;21:147–148. [Google Scholar]
- 37. Kim E, Jeong HJ, Lee KW, Song JS. Interpreting positive signs of the supraspinatus test in screening for torn rotator cuff. Acta Med Okayama. 2006;60(4):223–228. [DOI] [PubMed] [Google Scholar]
- 38. Kim HA, Kim SH, Seo YI. Ultrasonographic findings of painful shoulders and correlation between physical examination and ultrasonographic rotator cuff tear. Mod Rheumatol. 2007;17(3):213–219. [DOI] [PubMed] [Google Scholar]
- 39. Kim HA, Kim SH, Seo YI. Ultrasonographic findings of the shoulder in patients with rheumatoid arthritis and comparison with physical examination. J Korean Med Sci. 2007;22:660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. MacDonald PB, Clark P, Sutherland K. An analysis of the diagnostic accuracy of the Hawkins and Neer subacromial impingement signs. J Shoulder Elbow Surg. 2000;9(4):299–301. [DOI] [PubMed] [Google Scholar]
- 41. Marantz PR, Tobin JN, Wassertheil-Smoller S, et al. The relationship between left ventricular systolic function and congestive heart failure diagnosed by clinical criteria. Circulation. 1988;77(3):607–612. [DOI] [PubMed] [Google Scholar]
- 42. Matsen FA., 3rd Clinical practice: rotator-cuff failure. New Engl J Med. 2008;358(20):2138–2147. [DOI] [PubMed] [Google Scholar]
- 43. Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90(11):1898–1903. [DOI] [PubMed] [Google Scholar]
- 44. Milgrom C, Schaffler M, Gilbert S, van Holsbeeck M. Rotator-cuff changes in asymptomatic adults: the effect of age, hand dominance and gender. J Bone Joint Surg Br. 1995;77(2):296–298. [PubMed] [Google Scholar]
- 45. Miller JE, Higgins LD, Dong Y, et al. Association of strength measurement with rotator cuff tear in patients with shoulder pain: the Rotator Cuff Outcomes Workgroup Study. Am J Phys Med Rehabil. 2016;95(1):47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. BMJ. 2005;331(7525):1124–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Naredo E, Aguado P, De Miguel E, et al. Painful shoulder: comparison of physical examination and ultrasonographic findings. Ann Rheum Dis. 2002;61:132–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Neer CS., 2nd Impingement lesions. Clin Orthop Relat Res. 1983;(173):70–77. [PubMed] [Google Scholar]
- 49. Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Joint Surg Am. 2005;87(7):1446–1455. [DOI] [PubMed] [Google Scholar]
- 50. Pope DP, Croft PR, Pritchard CM, Macfarlane GJ, Silman AJ. The frequency of restricted range of movement in individuals with self-reported shoulder pain: results from a population-based survey. Br J Rheumatol. 1996;35(11):1137–1141. [DOI] [PubMed] [Google Scholar]
- 51. Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a Shoulder Pain and Disability Index. Arthritis Care Res. 1991;4(4):143–149. [PubMed] [Google Scholar]
- 52. Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley and Sons; 2004. [Google Scholar]
- 53. Scheibel M, Magosch P, Pritsch M, Lichtenberg S, Habermeyer P. The belly-off sign: a new clinical diagnostic sign for subscapularis lesions. Arthroscopy. 2005;21(10):1229–1235. [DOI] [PubMed] [Google Scholar]
- 54. Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB. Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am. 1995;77(1):10–15. [DOI] [PubMed] [Google Scholar]
- 55. Speed C. Shoulder pain. BMJ Clinical Evidence. 2006;2006:1107. [Google Scholar]
- 56. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57(11):649–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Vecchio P, Kavanagh R, Hazleman BL, King RH. Shoulder pain in a community-based rheumatology clinic. Br J Rheumatol. 1995;34(5):440–442. [DOI] [PubMed] [Google Scholar]
- 58. Walch G, Boulahia A, Calderone S, Robinson AH. The “dropping” and “hornblower’s” signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80(4):624–628. [DOI] [PubMed] [Google Scholar]
- 59. Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: report of the Multicenter Criteria Committee. Arthritis Rheum. 1990;33(2):160–172. [DOI] [PubMed] [Google Scholar]
- 60. Woodward TW, Best TM. The painful shoulder, part I: clinical evaluation. Am Fam Physician. 2000;61(10):3079–3088. [PubMed] [Google Scholar]
- 61. Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease: a comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88(8):1699–1704. [DOI] [PubMed] [Google Scholar]
- 62. Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg. 2001;10(3):199–203. [DOI] [PubMed] [Google Scholar]
- 63. Yoon JP, Chung SW, Kim SH, Oh JH. Diagnostic value of four clinical tests for the evaluation of subscapularis integrity. J Shoulder Elbow Surg. 2013;22(9):1186–1192. [DOI] [PubMed] [Google Scholar]
- 64. Yuen CK, Mok KL, Kan PG. The validity of 9 physical tests for full-thickness rotator cuff tears after primary anterior shoulder dislocation in ED patients. Am J Emerg Med. 2012;30(8):1522–1529. [DOI] [PubMed] [Google Scholar]