Abstract
Background:
Schistosoma mansoni is a major public health problem. Different studies reported unidentified sites in Ethiopia with variable prevalence and intensity, but there is no report from this study area.
Objective:
To assess the clinico-epidemiology, malacology, risk factors, and community awareness of S. mansoni in Haradenaba and Dertoramis kebeles in the Bedeno district, eastern Ethiopia.
Methods:
A cross-sectional study was conducted among 1011 study participants in 413 systematically selected households from Haradenaba and Dertoramis kebeles from 30 June 2016 to 30 July 2017. Data were collected by using pretested, structured questionnaires, clinical examinations, and stool examinations. Stool samples were processed by the Kato-Katz method and examined microscopically. Snails were collected by scooping from water contact points. Data were analyzed using SPSS, version 16 statistical software.
Result:
The overall prevalence of S. mansoni was 35.7%. Heavy-intensity infection was detected in 8.9% of the study participants. Results included: participants who were unaware about the possible source of infection (adjusted odds ratio: 2.95; 95% confidence interval: 1.25, 7.95), modes of transmission (adjusted odds ratio: 5.51; 95% confidence interval: 3.52, 12.51), prevention (adjusted odds ratio: 4.01; 95% confidence interval: 2.00, 8.75) about schistosomiasis/bilharziasis were more likely infected with S. mansoni than those who were aware. Participants who swim or bathe in the river were more likely infected with S. mansoni than those who do not (adjusted odds ratio: 6.41; 95% confidence interval: 3.15, 11.25). Biomphalaria pfeifferi snails were collected from all water bodies in Haradenaba and Dertoramis, but they did not shed schistosome cercaria in the laboratory.
Conclusion:
S. mansoni infection is found in high magnitude in these study areas, despite not being previously reported. A majority of the study participants had low awareness about the source of infection, mode of transmission, and prevention methods of schistosomiasis. Efforts should be made to improve community awareness about transmission and prevention of schistosomiasis.
Keywords: Clinico-epidemiology, malacology, community awareness, Schistosoma mansoni, Bedeno district, Ethiopia
Introduction
Schistosomiasis is caused by Schistosoma species.1,2 In Ethiopia, schistosomiasis is caused by both Schistosoma mansoni and Schistosoma haematobium species. S. mansoni is the leading cause of schistosomiasis. Low water temperature, the presence of snails’ intermediate host, and the absence of safe water supply and emergence of water development might contribute to distribution of schistosomiasis in Ethiopia.3,4 Transmission occurs when an infected person defecates or urinates eggs of the parasite near water bodies.5 Water resource development projects in tropical areas, especially the construction of dam and irrigation system, often create favorable conditions for increasing the transmission potential of schistosomiasis.3,6,7 In addition, the absence of a safe water supply, sanitary facilities, affordable anti-schistosomal drug, a lack of community awareness about schistosomiasis, and population movement to endemic communities puts the population at risk of infection.4
In Africa, more than 130,000 people die per year because of intestinal schistosomiasis.8,9 The disease remains one of most neglected tropical diseases.1 In endemic areas, children are the carriers of acute schistosomiasis. However, adult populations are carries of the chronic form of the disease like periportal fibrosis, hepatomegaly, splenomegaly, portal hypertension, and hematemesis.10,11
There are no published reports in community awareness and the prevalence of schistosomal-induced hepatomegaly/splenomegaly in the study area. Even though, a number of cases of intestinal schistosomiasis were reported from different health institutions in Eastern Hararghe. Therefore, this study assessed the clinico-epidemiology, malacology, and community awareness of S. mansoni in Haradenaba and Dertoramis kebeles in the Bedeno district, eastern Ethiopia.
Methods
Study area design and period
A community-based cross-sectional study was conducted in two selected kebeles in Bedeno district, Eastern Hararghe from 30 June 2016–30 July 2017. Eastern Hararghe is in the Oromia region, which has 22 districts.12
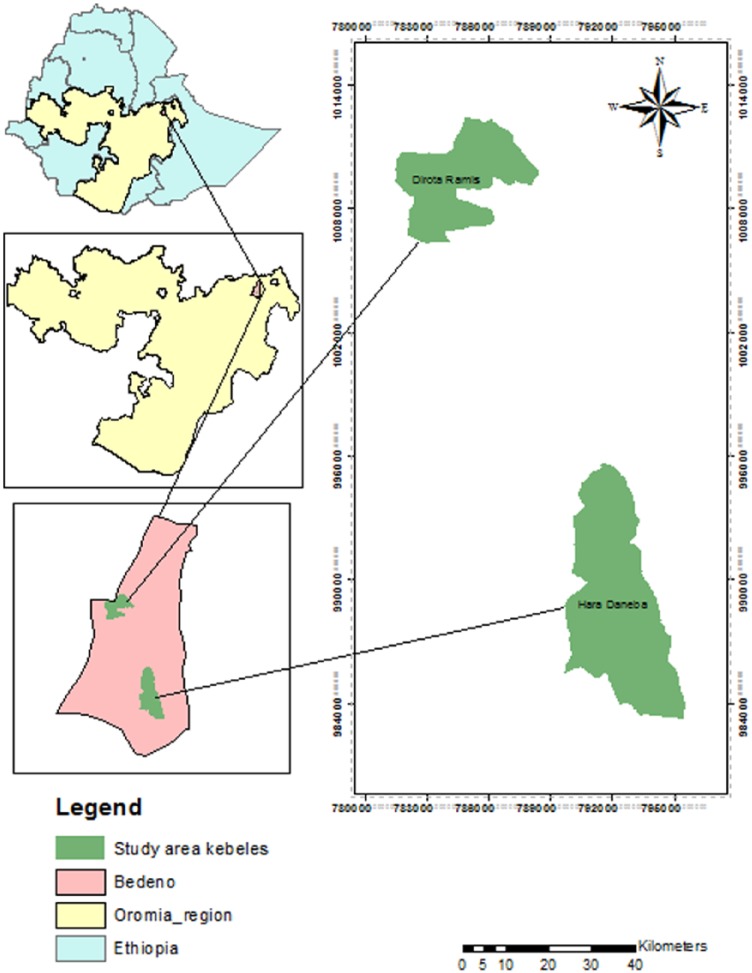
Bedeno district is one of the districts in Eastern Hararghe zone of Oromia regional state with a total population of 296,362; 40 kebeles; and 61,742 households. The altitude of this study area ranges from 1200 to 3100 m above sea level. This study was conducted in two selected kebeles namely Haradenaba and Dertoramis (Figure 1), which has water bodies used by community for different purpose and suspected to have intestinal schistosomiasis. According to the Eastern Hararghe zonal administration office, in a total of 6382 and 6242 people live in Haradenaba and Dertoramis kebeles in 2013/14, respectively. A total of 1276 and 1248 households live in Haradenaba and Dertoramis kebeles, respectively.13
Figure 1.
Map of the study area.
Study population
For the prevalence and intensity of S. mansoni study, all individuals with 5 years of age or older, living in 413 households were included. However, for the community awareness assessment of S. mansoni, individuals in the selected households with age greater or equals to 18 were included. Individuals who had taken treatment for schistosomiasis a month prior to the survey were excluded. Children less than 5 years of age were also excluded because he or she might not develop hepatomegaly and splenomegaly in the early age even in the presence of the worm.
Sample size and sampling techniques
The sample size was determined using a single proportion formula by considering the prevalence of 42.9% of S. mansoni from a study conducted in Jimma,14 using a 10% non-response rate. The final sample size for this study was 413 households. The 413 households divided for the two kebeles were based on the number of households (209 for Haradenaba and 204 for Dertoramis). The households were selected by systematic sampling techniques using kebeles house number as the sampling frame.
Method of data collection
Data was collected by:
Face-to-face interview
Socio-demographic characteristics, residence, knowledge about the causative agent of the disease, transmission, prevention and control, water sources, swimming and fishing habits, and other information were obtained through interviews using pretested structured questioners by trained nurses.
Clinical examination
Clinical examination of each study participant was done by Health officers to assess both acute and chronic conditions related to schistosomiasis like pallor, jaundice, fever, splenic/liver enlargement, superficial abdominal collateral veins and others.
Laboratory examination
Freshly passed stool specimens were collected by using a clean plastic container during visit of selected households. It was then processed using Kato-Katz methods.15 Two Kato-Katz slides were prepared at the field from each participants and one of them was examined using microscopy at field for immediate treatment of positive individuals. Then, all the slides were stored in a slide box and transported to the Haramaya University department of medical laboratory science laboratory for microscopic examination and quantification of the egg of S. mansoni. The average of two Kato-Katz slides egg counts were converted into number of eggs per gram (EPG) of stool. The intensity infection classified based on EPG as heavy (>399 EPG), moderate (100–399 EPG), and light (1–99 EPG) according to guidelines developed by Montresor et al.16
Malacological studies
Survey sites were selected on the basis of preliminary field observations and discussing with study participants on water contact points where people consistently go to collect water, wash clothes, bath, and swim or play. Snails were collected by scooping water bodies for 30 min on each site by an experienced snail collector wearing boots and heavy duty gloves to prevent infection. The collected snails were placed in wide-mouthed glass bottles filled with water and vegetation from the same habitat and put inside a cooler container with ice to avoid overheating during transportation.17 Then, they were transported to Aklilu Lemma Institutes of Pathobiology (ALIPB), Addis Ababa University. At ALIPB, the snails were examined for trematode infection (cercariae shedding) by transferring each snail to the shedding vial and exposing them to electric light for about 2 h. The time of cercariae shedding was carefully selected to coincide with the early peak shedding time (mid-day). The shedding vial was examined for the presence of cercariae under a dissecting microscope and identified to the genus level using tail morphology.18
Data analysis
Data were entered and cleaned using EPI Data software and analyzed using SPSS statistical package (version 16 SPSS Inc., Chicago, IL, USA). Geometric means of intensities of S. mansoni of EPG were reported in the table. The prevalence of S. mansoni was determined as proportion-positive individuals during stool examination. Chi-square, Crude (CORs) and adjusted odds ratios (AORs) were used to test the association between prevalence of S. mansoni infection with different possible risk factors. The prevalence of hepatomegaly and/or splenomegaly was determined by a positive finding in the clinical examination. Chi-square, CORs, and AORs were used to test the association between prevalence of development of hepatomegaly and/or splenomegaly with different possible risk factors. To show the magnitude difference in both prevalence and intensity of infection 95% confidence interval (CI) was used. A p value less than 0.05 was considered as statistical factor.
Data quality assurance
To maintain the quality of the data, structured and pretested questionnaires were used to collect information. Training was given to all data collectors and supervisors for 2 days. Each questionnaire was checked daily for completeness. In addition, supervision was conducted in each data collection site. Standard operational procedures were used for stool collection and examination.
Result
Socio-demographic characteristics of study participants
A total of 1011 study participants were included in this study. The majority of the study participants were female (59.1%). The mean age of the study participants was 22.65 with standard deviation ± 1.43 and range of 5–72 years. Almost all of the study participants were Muslim (99.7%) in religion and farmers (54.2%) in their occupation. In total, 439 (43.4%) and 322 (31.8%) of the study participants were enrolled in pre-school and could not read and write, respectively (Table 1).
Table 1.
Socio-demographic characteristics of study participants recruited from the community, Bedeno District, eastern Ethiopia, 2017 (n = 1011).
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Sex | ||
| Male | 413 | 40.9 |
| Female | 598 | 59.1 |
| Age groups | ||
| 5–9 | 227 | 22.5 |
| 10–14 | 207 | 20.5 |
| 15–19 | 66 | 6.5 |
| 20–24 | 52 | 5.1 |
| 25–29 | 88 | 8.7 |
| 30–34 | 101 | 10.0 |
| 35–39 | 89 | 8.8 |
| 40–44 | 92 | 9.1 |
| 45–49 | 44 | 4.4 |
| 50–54 | 39 | 3.9 |
| >55 | 6 | 0.6 |
| Religion | ||
| Muslim | 1008 | 99.7 |
| Orthodox | 3 | 0.3 |
| Occupation | ||
| Under age | 439 | 43.4 |
| Farmer | 548 | 54.2 |
| Student | 10 | 1.0 |
| House wife | 14 | 1.4 |
| Educational status | ||
| Pre-school | 439 | 43.4 |
| Cannot read and write | 322 | 31.8 |
| Read and write only | 167 | 16.5 |
| Elementary school (1–8) | 66 | 6.5 |
| Secondary school and above | 17 | 1.7 |
| Name/address of residence | ||
| Haradenaba | 746 | 73.8 |
| Dertoramis | 265 | 26.2 |
Prevalence of S. mansoni
The prevalence of S. mansoni was 35.7%. Only 8.9% of the study participants had heavy intensity of infection (Table 2). The prevalence of S. mansoni was higher among males (31.5%); those in 18–24 (36.2%) and 50 or older (37.5%) years of age group; students (50%); those with primary school educational status (39.4%); and living in Haradenaba (36.4%). Regarding the other potential risk factors, the prevalence of S. mansoni was higher among those who swim or bathe on the river (46.1%), catch fish from the river (34.6%), fetch drinking water from the river (29.9 %), practicing open field defecation (31%), and have information about bilharziasis/schistosomiasis (31.2%) (Table 3).
Table 2.
Prevalence and intensity infection of S. mansoni among study participants recruited from the community, Bedeno District, eastern Ethiopia, 2017 (n = 1011).
| Variable | Frequency (%) |
|---|---|
| Microscopic examination result | |
| Positive | 361 (35.7) |
| Negative | 650 (64.3) |
| Intensity of infection | |
| Light (1–99 EPG) | 178 (49.3) |
| Moderate (100–399 EPG) | 151 (41.8) |
| Heavy (>399 EPG) | 32 (8.9) |
EPG: eggs per gram.
Table 3.
Awareness of adult study participants recruited from the community about intestinal schistosomiasis, Bedeno District, 2017 (n = 572).
| Variables | No. (%) | |
|---|---|---|
| Can bilharziasis affect all age group? | Yes | 57 (10) |
| No | 49 (8.6) | |
| I don’t know | 466 (81.4) | |
| What are the possible sources of infection of bilharziasis? | Water contact (water from river/lake and infected water snail) | 120 (21) |
| I don’t know | 452 (79) | |
| What are the possible modes of transmission for bilharziasis? | Water contact (swimming in river and fishing) | 78 (13.6) |
| I don’t know | 494 (86.4) | |
| The sign/symptoms of bilharzias | Abdominal pain | 71 (12.4) |
| Vomiting | 49 (8.6) | |
| I don’t know | 452 (79) | |
| Is bilharzias treatable? | Yes | 120 (21) |
| I don’t know | 452 (79) | |
| Is bilharzias preventable? | Yes | 120 (21) |
| I don’t know | 452 (79) | |
| What are the possible prevention methods of bilharzias? | Avoid swimming in nearby river/stream/lake | 120 (21) |
| I don’t know | 452 (79) | |
Community awareness about intestinal schistosomiasis
Most of the study participants have no awareness about age groups of people as risk to S. mansoni (81.4%), the possible sources of infection (79%), possible modes of transmission for bilharziasis (86.4%), signs and symptoms of bilharzias (79%), knowledge about treatment (79%), and prevention of bilharziasis (79%) (Table 3).
Sign and symptoms of the study participants
The presence of 17 signs and symptoms and their relation with prevalence S. mansoni were assessed using questionnaire and clinical examination. From the positive participants, 175 (48.5%) individuals had developed advanced chronic schistosomiasis. The prevalence of S. mansoni was significantly higher among those study participants with fatigue (40.9%) and bloody diarrhea (43.3%; p < 0.05). The prevalence S. mansoni was also higher among those without abdominal pain (40.7%), with headache (38.6%), wheezing sound (39.4%), wheezing sound, with hepatomegaly (38.4%), splenomegaly (41.5%), with ascetics (55.6%), without pallor (36%), jaundiced (38%), and superficial abdominal collateral veins (37.5%; p > 0.05) (Table 4).
Table 4.
Clinical features of the study participants for the last 2 weeks from the community, Bedeno district, eastern Ethiopia, 2017 (n = 1011).
| Sign/symptoms | Microscopic examination
result |
p value | ||
|---|---|---|---|---|
| Positive |
Negative |
|||
| Frequency (%) | Frequency (%) | |||
| Fever | Yes | 99 (35.4) | 181 (64.6) | 0.886 |
| No | 262 (35.8) | 469 (64.2) | ||
| Abdominal pain | Yes | 282 (34.5) | 535 (65.5) | 0.105 |
| No | 79 (40.7) | 115 (59.3) | ||
| Vomiting | Yes | 95 (35.3) | 174 (64.7) | 0.876 |
| No | 266 (35.8) | 476 (64.2) | ||
| Nausea | Yes | 165 (36.5) | 287 (63.5) | 0.634 |
| No | 196 (35.1) | 363 (64.9) | ||
| Fatigue/malaise | Yes | 175 (40.9) | 253 (59.1) | 0.003 |
| No | 186 (31.9) | 397 (68.1) | ||
| Bloody diarrhea | Yes | 129 (43.3) | 169 (56.7) | 0.001 |
| No | 232 (32.5) | 481 (67.5) | ||
| Headache | Yes | 170 (38.9) | 267 (61.1) | 0.064 |
| No | 191 (33.3) | 383 (66.7) | ||
| Rash/dermatitis | Yes | 40 (34.8) | 75 (65.2) | 0.826 |
| No | 321 (35.8) | 575 (64.2) | ||
| Wheezing | Yes | 13 (39.4) | 20 (60.6) | 0.653 |
| No | 348 (35.6) | 630 (64.4) | ||
| Splenomegaly | Yes | 73 (41.5) | 103 (58.5) | 0.079 |
| No | 288 (34.5) | 547 (65.5) | ||
| Hepatomegaly | Yes | 81 (38.4) | 130 (61.6) | 0.361 |
| No | 280 (35) | 520 (65) | ||
| Ascites | Yes | 15 (55.6) | 12 (44.4) | 0.029 |
| No | 346 (35.2) | 638 (64.8) | ||
| Hemoptysis | Yes | 1 (33.3) | 2 (66.7) | NA |
| No | 360 (35.7) | 648 (64.3) | ||
| Pallor | Yes | 18 (31.6) | 39 (68.4) | 0.503 |
| No | 343 (36) | 611 (64) | ||
| Jaundice | Yes | 27 (38) | 44 (62) | 0.672 |
| No | 334 (35.5) | 606 (64.5) | ||
| Superficial abdominal collateral veins | Yes | 24 (37.5) | 40 (62.5) | 0.757 |
| No | 337 (35.6) | 610 (64.4) | ||
Factors associated with the prevalence and intensity of S. mansoni
In bivariate analysis, educational status, kebeles residence, swimming or bathing in the river, washing clothes in the river, fetching water for drinking from the river, awareness about the possible source of infection of Bilharziasis, awareness about the possible modes of transmission for Bilharziasis, and awareness about the possible prevention methods of bilharzias were variables extracted as candidates for multivariate analysis (Tables 5 and 6).
Table 5.
Prevalence of S. mansoni with associated factors among adult study participants in Bedeno district, eastern Ethiopia, 2017 (n = 572).
| Variables | Positive no. (%) | Negative no. (%) | COR (95% confidence interval) | p valve | |
|---|---|---|---|---|---|
| Sex | Male | 63 (31.5) | 137 (68.5) | 1 | 0.73 |
| Female | 112 (30.1) | 260 (69.9) | 2.34 (1.305,3.51) | ||
| Age | 18–24 | 34 (36.2) | 60 (63.8) | 1 | 0.39 |
| 25–29 | 56 (32) | 119 (68) | 0.37 (0.122,1.00) | ||
| 30–34 | 29 (33.3) | 58 (66.7) | 0.60 (0.127,0.92) | ||
| 35–39 | 24 (21.6) | 87 (78.4) | 0.58 (0.17,1.39) | ||
| 40–44 | 10 (31.2) | 22 (68.8) | 1.00 (0.11,2.01) | ||
| 45–49 | 19 (29.2) | 46 (70.8) | 1.16 (0.37,3.61) | ||
| >50 | 3 (37.5) | 5 (62.5) | 1.16 (0.35,3.61) | ||
| Occupation | Farmer | 165 (30.1) | 383 (69.9) | 1 | 0.37 |
| Student | 5 (50) | 5 (50) | 1.17 (0.95,1.54) | ||
| House wife | 5 (35.7) | 9 (64.3) | 0.69 (0.45,0.98) | ||
| Educational status | Cannot read and write | 100 (31.1) | 222 (68.9) | 1 | 0.22 |
| Read and write only | 43 (25.7) | 124 (74.) | 1.0 (0.65,1.54) | ||
| Elementary school (1–8) | 26 (39.4) | 40 (60.6) | 1.4 (0.25,8.98) | ||
| Secondary school and above | 6 (35.3) | 11 (64.7) | 0.52 (0.15,1.25) | ||
| Residence of kebeles | Dertoramis | 14 (10.8) | 116 (89.2) | 1 | 0.001 |
| Haradenaba | 161 (36.4) | 281 (63.6) | 4.75 (2.64, 8.54) | ||
| Swim (bathing) in the river | Yes | 146 (46.1) | 171 (53.9) | 6.65 (4.26, 10.39) | 0.001 |
| No | 29(11.4) | 226 (88.6) | 1 | ||
| Catch fish from the river | Yes | 6 (37.5) | 10 (62.5) | 1 | 0.56 |
| No | 169 (30.4) | 387 (69.6) | 2.01 (0.90, 4.32) | ||
| Wash cloth in the river | Yes | 163 (34.9) | 304 (65.1) | 4.16 (2.21, 7.81) | 0.001 |
| No | 12 (11.4) | 93 (88.6) | 1 | ||
| Fetch water for drinking from the river | Yes | 165 (29.9) | 387 (70.1) | 1 | 0.08 |
| No | 10 (50) | 10 (50) | 2.4 (0.92, 7.24) | ||
| Where do you defecate your feaces? | Latrine | 82 (30.1) | 190 (69.9) | 1 | 0.75 |
| Open field | 93 (31) | 207 (69) | 1.01 (0.70, 1.70) | ||
| How frequent do you use (private latrine and public latrine)? | Always | 46 (28) | 118 (72) | 1 | 0.47 |
| Sometimes | 35 (33.3) | 70 (66.7) | 0.31 (0.21, 0.69) | ||
| Have you heard about bilharziasis? | Yes | 34 (28.3) | 86 (71.7) | 1 | 0.85 |
| No | 141 (31.2) | 311 (68.6) | 0.86 (0.67, 1.41) | ||
| Source of information | Health professions | 26 (25.5) | 76 (74.5) | 1 | 0.15 |
| Teacher | 8 (44.4) | 10 (55.6) | 1.00 (0.13, 6.85) | ||
COR: crude odds ratio.
Table 6.
Awareness of adult study participants recruited from the community about intestinal schistosomiasis, Bedeno district, 2017 (n = 572).
| Microscopic examination
result |
|||||
|---|---|---|---|---|---|
| Variables | Positive no. (%) | Negative no. (%) | COR (95% CI) | p valve | |
| Can bilharziasis affect all age group? | Yes | 11 (19.3) | 46 (80.7) | 1 | 0.452 |
| No | 15 (30.6) | 34 (69.4) | 0.187 (0.091, 2.001) | ||
| I don’t know | 149 (32) | 317 (68) | 1.116 (0.578, 3.212) | ||
| What are the possible sources of infection of bilharziasis? | Water contact (water from river/lake and infected water snail) | 15 (12.5) | 105 (87.5) | 1 | 0.001 |
| I don’t know | 160 (35.4) | 292 (64.6) | 3.836 (2.16, 6.812) | ||
| What are the possible modes of transmission for bilharziasis? | Water contact (swimming in river and fishing) | 10 (12.8) | 68 (87.2) | 1 | 0.001 |
| I don’t know | 165 (33.4) | 329 (66.6) | 5.822 (2.476, 13.690) | ||
| The sign/symptoms of bilharzias | Abdominal pain | 19 (26.8) | 52 (73.2) | 1 | 0.874 |
| Vomiting | 15 (30.6) | 34 (69.4) | 1.057 (0.428, 3.249) | ||
| I don’t know | 141 (31.2) | 311 (68.8) | 1.401 (0.912, 4.813) | ||
| Is bilharzias treatable? | Yes | 34 (28.3) | 86 (71.7) | 1 | 0.912 |
| I don’t know | 141 (31.2) | 311 (68.8) | 1.280 (0.858, 4.247) | ||
| The type of treatment | Modern | 34 (28.3) | 86 (71.7) | ||
| Is bilharzias preventable? | Yes | 34 (28.3) | 86 (71.7) | 1 | 0.526 |
| I don’t know | 141 (31.2) | 311 (68.8) | 1.001 (0.125, 3.405) | ||
| What are the possible prevent methods of bilharzias? | Avoid swimming in nearby river/stream/lake | 14 (11.7) | 106 (88.3) | 1 | 0.021 |
| I don’t know | 161 (35.6) | 291 (64.4) | 4.8512 (1.612, 9.781) | ||
COR: crude odds ratio.
Participants who were unaware about the possible source of infection for bilharziasis were almost three times more likely to get infected with S. mansoni than those who know about it (AOR: 2.95; 95 % CI: 1.25, 7.95). Those participants who do not know about the possible modes of transmission for bilharziasis were more than five times more likely to get infected with S. mansoni than those who were aware of the possible modes of transmission (AOR: 5.51; 95% CI: 3.52, 12.51). Participants who were unaware about the possible prevention of bilharziasis were almost four times more likely to get infected with S. mansoni than those who know about it (AOR: 4.01; 95 CI: 2.00, 8.75). Participants who washed their clothes in the river were almost four times more likely to get infected with S. mansoni than those who do not (AOR: 3.92; 95 CI: 2.10, 8.12). Those participants who live in Haradenaba kebele were almost five times more likely to get infected with S. mansoni than those who live in Dertoramis (AOR: 4.57; 95% CI: 2.42, 9.43). Those participants who swim or bathe in the river were more than six times more likely infected with S. mansoni than those who do not (AOR: 6.41; 95% CI: 3.15, 11.25; Table 7).
Table 7.
Factors associated with prevalence of S. mansoni among adult study participants in Bedeno district, eastern Ethiopia, 2017 (n = 572).
| Characteristics | Positive no. (%) | Negative no. (%) | AOR (95% confidence interval) | p valve | |
|---|---|---|---|---|---|
| What are the possible sources of infection of bilharziasis? | I don’t know | 160 (35.4) | 292 (64.6) | 2.951 (1.25, 7.951) | |
| Water contact (water from river/lake and infected water snail) | 15 (12.5) | 105 (87.5) | 1 | ||
| What are the possible modes of transmission for bilharziasis? | I don’t know | 165 (33.4) | 329 (66.6) | 5.512 (3.521, 12.510) | |
| Water contact (swimming in river and fishing) | 10 (12.8) | 68 (87.2) | 1 | ||
| What are the possible prevent methods of bilharzias? | I don’t know | 161 (35.6) | 291 (64.4) | 4.01 (2.002, 8.7512) | 0.021 |
| Avoid swimming in nearby river/stream/lake | 14 (11.7) | 106 (88.3) | 1 | ||
| Wash cloth in the river | Yes | 163 (34.9) | 304 (65.1) | 3.915 (2.101, 8.124 | |
| No | 12 (11.4) | 93 (88.6) | 1 | ||
| Residence of kebeles | Haradenaba | 161 (36.4) | 281 (63.6) | 4.572 (2.424, 9.415) | |
| Dertoramis | 14 (10.8) | 116 (89.2) | 1 | ||
| Swim (bathing) in the river | Yes | 146 (46.1) | 171 (53.9) | 6.412 (3.145, 11.245) | |
| No | 29 (11.4) | 226 (88.6) | 1 | ||
AOR: adjusted odds ratio.
Malacological survey
Dam and its drainages in Haradenaba and river shades in Dertoramis kebeles were surveyed for S. mansoni intermediate hosts during the study period. During the survey, many people were observed laundering, swimming, and bathing in both areas. Physical characteristics of the water bodies showed that Haradenaba dam water was covered with large amounts of fallen leaves, weeds, algae, and decaying wood and turbid. It was stagnant and slow flowing during the summer season and fitted with drainages. On the contrary, Dertoramis river was large; fast flowing; clear; and lacked any vegetation, weeds, and algae. Scooping was done in 11 human water contact sites of the two kebeles.
Biomphalaria pfeifferi were collected from all water bodies and a large number of B. pfeifferi were collected from Haradenaba dam and dam drainages. Out of 74 B. pfeifferi snails (4–8 snails from each collection sites) were collected during the study period, 16 (21.7%) died during transportation, and the remaining 58 (78.3%) were not observed to shed schistosome cercaria in the laboratory. Other snail species such as Lymnaea natalensis was also collected from Haradenaba dam and Dertoramis river.
Discussion
The prevalence rate of 35.7% S. mansoni infection was reported for the first time from this study among people dwelling in Haradenaba and Dertoramis kebeles in Bedeno district, eastern Ethiopia. This finding was comparable with two surveys conducted among rural communities in Shesha Kekel, Wondo Genet district and Sille-Elgo area found in Gofa Zone in the Southern Nations and Nationalities Regional State, which reported a prevalence rate of 31.6%.19,20 This study showed a lower prevalence rate of S. mansoni infection compared with other surveys conducted among communities from different parts of Ethiopia; in Dudicha community found in Ziway Dugda, Bora district (43.2%), Kemise which is found in Oromia Nationality Administrative Zone of the Amhara Regional State (89.6%), Wondo Genet which is found in western Arsi in Oromia Regional State (59.9%), and Waja-Timuga which is found in southern Tigray, northern Ethiopia (73.9%).19–21 But higher prevalence rate of S. mansoni infection compared with other survey conducted among communities in Jimma town (26.3 %).14
The reason why the presently observed prevalence of S. mansoni was different from other studies might be due to the difference in water contact behavior of the communities (frequency of contact to infested water), ecological distribution of the intermediate host (snail), local endemicity of the parasite, sample size, altitude and the temperature (which is favorable for the development and survival of snail), and awareness of community about transmission and prevention of S. mansoni infection.
This finding reflects that only 8.9% of those infected were heavily infected, but most people are infected moderately and/or lightly. Similar findings were reported from studies conducted in Jimma town and Waja-Timuga, Sille-Elgo of Ethiopia and Rwanda.14,20–22
There were higher proportion of S. mansoni infected individuals (36.4%) observed in Haradenaba kebele compared to individuals living in Dertoramis kebele (10.8%). There is also difference in water contact sites between the two communities. For instance, a dam in Haradenaba kebele is the only source of water for drinking, washing clothes, and swimming/bathing of the community. The low prevalence of S. mansoni infection among communities in Dertoramis kebele may be attributed to the presence of piped water as an alternative water source. Other explanations might be due to the difference in altitude and the temperature, which is favorable for the development and survival of snail.
Schistosomiasis has been spread by contact with water that contains the larval parasites. But, water contact is not itself a way of exposure for schistosomiasis. Many aspects of water contact (such as the frequency or total duration of contact, how much of the body is exposed and when) may contribute to the likelihood of encountering infective cercariae.23,24 In this study, water contact activities such as swimming/bathing and washing clothes were significantly associated with higher positivity because in such activities the body was exposed for a longer period of time. But water contact activity such as fishing and fetching water for drinking was not significantly associated with higher positivity. This might be due to the fact that a few individuals were observed in Dertoramis kebeles involved in river fishing. In addition to this, communities of Dertoramis kebeles have alternative pipe water source mainly used for drinking.
In Ethiopia, many studies have been done on the prevalence of schistosomiasis with very little emphasis on community knowledge about the disease.19 In this study, more than two-thirds (79%) of the study subjects had never heard about schistosomiasis despite the endemicity of the disease in the study areas. Similar findings were reported from studies conducted in two endemic localities of Ethiopia.19 But a large majority; 91% respondents in Nampula province in Mozambique,25 92.90 % in Mwea division, Kirinyaga County,Kenya26 and 92.4% in ten rural districts in Yemen27 reported that they had heard about the disease. This difference might be due to the active schistosomiasis control project in schistosomiasis endemic areas and/or exposure of individuals about the disease through different media.
A total of 452 (79%) respondents did not mention any signs or symptoms of schistosomiasis. Among the respondents, only 12.4 % of them mentioned experiencing abdominal pain and 8.6 % mentioned vomiting. This is in line with previous studies from Mwea, Kirinyaga County, Kenya, which reported abdominal pain as the main sign and symptom.26 A low level of knowledge about sign and symptoms was also reported among the rural population in Yemen, in Mwea, Kirinyaga county, Kenya, urban settlement of Kenya.26–28 There was no significant difference in schistosomiasis infection between the participants who mentioned the above two symptoms of schistosomiasis and who did not mention any signs or symptoms. This could be attributed to the disease being frequently confused with other intestinal infections exhibiting similar symptoms, which is common among the targeted populations.
Infected individuals were significantly more likely to report the presence of bloody diarrhea and fatigue/malaise within 2 weeks preceding the interview. We also observed uninfected study participants identified by microscopic examination reported schistosomiasis-related symptoms. This may be a result of the fact that the disease can have a multitude of symptoms, most of which are non-specific. Through physical examination, hepatomegaly (0.2%), splenomegaly (0.17%), and ascites (0.02%) were identified. However, the value of clinical methods in describing the pathological sequelae induced by this parasite is limited.29,30 Ultrasonography is currently the diagnostic tool of choice for detecting pathologic conditions associated with S. mansoni such as liver fibrosis and enlargement and dilatation of the portal vein.31,32
This study revealed that a large majority of study participants do not know about the modes of transmission and prevention methods of schistosomiasis at 86.4% and 79%, respectively. Low level of knowledge about the source of infection, mode of transmission, and prevention methods of the disease were also reported from studies carried out in Ethiopia, Mozambique, Yemen, and Kenya.19,25–27
There was no significant difference in schistosomiasis infection between participants who heard about the disease and not. But there was significant difference in schistosomiasis infection between participants who had knowledge about the source of infection, the mode of transmission, and prevention methods. This indicated that those individuals who heard about the disease had limited knowledge about the source of infection, mode of transmission, and prevention methods of the disease. Studies carried out in Mozambique, Yemen, and Kenya reported poor awareness about the ways of transmission and preventive and control measures among the participants, although the majority of the respondents had heard about schistosomiasis.25–27
In this study, there was no cercarial shedding by B. pfeifferi snails at any of the sites of collection. As study indicated cercarial release from field-collected snails may be inhibited by a variety of contaminants and invertebrates harbored by the snails.33
Limitation
Ultrasonography, which provides sensitive and precise measurements of S. mansoni-associated pathologic changes such as liver fibrosis and enlargement and dilatation of the portal vein were not used because of budget scarcity.
Conclusion
Infection of S. mansoni is an important health problem in communities of these study sites which were not reported before. Even thought snails were not shade cercaria, the occurrence of infected human subjects with acute and chronic sequels of S. mansoni and the presence of intermediate snail host (B. pfeifferi), might confirm that S. mansoni is well established in these study sites. The finding of this study showed swimming/bathing and washing clothes in infected water sources are significant risk factors for acquiring S. mansoni infection, and majority of the people in the study areas had low awareness about schistosomiasis and its source of infection, mode of transmission, and prevention methods.
Efforts should be made to improve knowledge focused on causes, transmission, and prevention of schistosomiasis at the individual and community level. Interventions leading to reduction of water contact with dams/rivers, improved environmental sanitation in the dam/river catchments, provision of safe water supply, snail control, and targeted chemotherapy of the affected communities should be systematically planned to make control efforts achievable.
Although it is believed that increasing community awareness about schistosomiasis in such endemic areas through the provision of health education is a useful strategy, it may not be possible to avoid water contact activities and exposure of individuals to the parasite in the absence of an alternative water source. The community in Haradenaba has its water dam as the only source of water for drinking, washing clothes, and swimming/bathing. Thus, provision of alternative safe water source is highly recommended.
Acknowledgments
First, the authors would like to thank Haramaya University Research affairs for funding this research. We would like to express our deepest gratitude to the study participants, all individuals, and organizations that supported us in conducting this paper.
Footnotes
Author’s Note: J.M., F.W., Z.T., and H.M. designed the study; participated in data collection, analysis, interpretation, final write-up; drafted the manuscript; and critically revised the manuscript. All authors read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from Colleges of Health and Medical Sciences, Haramaya University, Institutional Health Research Ethical Review Committee.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The author(s) received financial support for conducting the research from Haramaya University.
Informed consent: Written informed consent was obtained from all adult participants before commencing data collection. Besides adults, children of parents/guardians who gave informed written consent and children who gave assent were included.
ORCID iD: Fitsum Weldegebreal  https://orcid.org/0000-0002-7867-1483
https://orcid.org/0000-0002-7867-1483
References
- 1. WHO. Strategy Development and Monitoring for Parasitic Diseases and Vector Control Team & UNICEF. Prevention and control of schistosomiasis and soil-transmitted helminthiasis: World Health Organization/Unicef joint statement. Geneva: World Health Organization, 2004. http://www.who.int/iris/handle/10665/68607. [Google Scholar]
- 2. Cheesbrough M. Medical laboratory manual for tropical countries, volume I. 2nd ed. Cambridge: Butterworth-Heinemann Ltd, 1987, pp. 321–341. [Google Scholar]
- 3. Alemayehu T, Ye-ebiyo Y, Ghebreyesus TA, et al. Malaria, schistosomiasis and intestinal helminths in relation to microdams in Tigray, northern Ethiopia. Parassitologia 1998; 40: 259–267. [PubMed] [Google Scholar]
- 4. Birrie H, Tedla S, Tilahun G, et al. Schistosomiasis and its distribution in Ethiopia and Eritrea. In: Birrie H, Tedla S, Jemaneh L. (eds) Schistosomiasis in Ethiopia and Eritrea. Addis Ababa, Ethiopia: Addis Ababa University, 1998, pp. 29–89. [Google Scholar]
- 5. Gryseels B, Polman K, Clerinx J, et al. Human schistosomiasis. Lancet 2006; 368: 1106–1118. [DOI] [PubMed] [Google Scholar]
- 6. Ofoezie IE. Human health and sustainable water resources development in Nigeria: schistosomiasis inartificial lakes. Nat Resour Forum 2002; 26: 150–160. [Google Scholar]
- 7. Nagi S, Chadeka EA, Sunahara T, et al. Risk factors and spatial distribution of Schistosoma mansoni infection among primary school children in Mbita district, western Kenya. PLoS Negl Trop Dis 2014; 8(8): e3190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fenwick A, Savioli L, Engels D, et al. Drugs for the control of parasitic diseases: current status and development in schistosomiasis. Trends Parasitol 2003; 19: 509–515. [DOI] [PubMed] [Google Scholar]
- 9. WHO. Ultrasound in schistosomiasis: a practical guide to the standard use of ultrasonography for assessment of schistosomiasis-related morbidity. Second international workshop. 2000, http://www.who.int/schistosomiasis/resources/tdr_str_sch_00.1/en/ (accessed January 2017).
- 10. Vennervald BJ, Dunne DW. Morbidity in schistosomiasis: an update. Curr Opin Infect Dis 2004; 17(5): 439–447. [DOI] [PubMed] [Google Scholar]
- 11. Booth M, Vennervald BJ, Kabatereine NB, et al. Hepatosplenic morbidity in two neighboring communities in Uganda with high levels of Schistosoma mansoni infection but very different durations of residence. Trans R Soc Trop Med Hyg 2004; 98: 125–136. [DOI] [PubMed] [Google Scholar]
- 12. East Hararghe Zonal health office, Health office annual report. Unpublished, 2016. [Google Scholar]
- 13. East Hararghe Zonal administration office 2015/2016 report. Unpublished. [Google Scholar]
- 14. Mengistu M, Shimelis T, Torben W, et al. Human intestinal schistosomiasis in communities living near three rivers of Jimma town, south western Ethiopia. Ethiop J Health Sci 2011; 21(2): 111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Peters PA, El Alamy M, Warren KS, et al. Quick Kato smear for field quantification of Schistosoma mansoni eggs. Am J Trop Med Hyg 1980; 29: 217–219. [DOI] [PubMed] [Google Scholar]
- 16. Montresor A, Crompton DWT, Hall A, et al. Guidelines for the evaluation of soil-transmitted helminthiasis and schistosomiasis at community level: a guide for managers of control programmes / A. Montresor … [et al.]. Geneva: World Health Organization, 1998. [Google Scholar]
- 17. Jayawardena UA, Rajakaruna RS, Amerasinghe PH. Cercariae of trematodes in freshwater snails in three climatic zones in Sri Lanka. Cey J Sci 2010; 39(2): 95–108. [Google Scholar]
- 18. Frandsen F, Christensen NO. An introductory guide to the identification of cercariae from African fresh water snails with special reference to cercariea of trematode species of medical and veterinary importance. Acta Trop 1984; 41: 181–202. [PubMed] [Google Scholar]
- 19. Legesse M, Jones CR, Singh SK, et al. Community’s awareness about intestinal schistosomiasis and the prevalence of infection in two endemic localities of Ethiopia. Ethiop J Health Sci 2009; 19(2): 103–110. [Google Scholar]
- 20. Aemero M, Berhe N, Erko B. Status of Schistosoma mansoni prevalence and intensity of infection in geographically apart endemic localities of Ethiopia: a comparison. Ethiop J Health Sci 2014; 24(3): 189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abebe N, Erko B, Medhin G, et al. Clinico-epidemiological study of schistosomiasis mansoni in Waja-Timuga, district of Alamata, northern Ethiopia. Parasit Vectors 2014; 7: 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ruberanziza E, Mupfasoni D, Karibushi1 B, et al. A recent update of schistomiasis mansoni endemicity around Lake Rweru. Rwanda Med J 2010; 68(4): 6. [Google Scholar]
- 23. Bethony J, Williams JT, Kloos H, et al. Exposure to Schistosoma mansoni infection in a rural area in Brazil. II: household risk factors. Trop Med Int Health 2001; 6(2): 136–145. [DOI] [PubMed] [Google Scholar]
- 24. Burchard GD, Guissé-Sow F, Diop M, et al. Schistosoma mansoni infection in a recently exposed community in Senegal: lack of correlation between liver morphology in ultrasound and connective tissue metabolites in serum. Trop Med Int Health 1998; 3(3): 234–241. [DOI] [PubMed] [Google Scholar]
- 25. Rassi C, Kajungu D, Martin S, et al. Have you heard of schistosomiasis? Knowledge, attitudes and practices in Nampula province, Mozambique. PLoS Negl Trop Dis 2016; 10(3): e0004504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mwai J, Njenga S, Barasa M. Knowledge, attitude and practices in relation to prevention and control of schistosomiasis infection in Mwea Kirinyaga county, Kenya. BMC Public Health 2016; 16: 819. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 27. Sady H, Al-Mekhlafi HM, Atroosh WM, et al. Knowledge, attitude, and practices towards schistosomiasis among rural population in Yemen. Parasit Vectors 2015; 8: 436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Odhiambo GO, Musuva RM, Atuncha VO, et al. Low levels of awareness despite high prevalence of schistosomiasis among communities in Nyalenda informal settlement, Kisumu city, western Kenya. PLoS Negl Trop Dis 2014; 8(4): e2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Houston S, Munjoma M, Kanyimo K, et al. Use of ultrasound in a study of schistosomal periportal fibrosis in rural Zimbabwe. Acta Trop 1993; 53: 51–58. [DOI] [PubMed] [Google Scholar]
- 30. Doehring-Schwerdtfeger E, Kaiser C, Schlake J, et al. Ultrasound versus clinical examination as indication for Schistosoma mansoni associated morbidity in children. Trop Med Parasitol 1992; 43: 245–248. [PubMed] [Google Scholar]
- 31. Richter J, Hatz C, Häussinger D. Ultrasound in tropical and parasitic diseases. Lancet 2003; 362(9387): 900–902. [DOI] [PubMed] [Google Scholar]
- 32. Kabatereine NB, Kemijumbi J, Ouma JH, et al. Epidemiology and morbidity of Schistosoma mansoni infection in a fishing community along Lake Albert in Uganda. Trans R Soc Trop Med Hyg 2004; 98(12): 711–718. [DOI] [PubMed] [Google Scholar]
- 33. Opisa S, Odiere MR, Jura WG, et al. Malacological survey and geographical distribution of vector snails for schistosomiasis within informal settlements of Kisumu city, western Kenya. Parasit Vectors 2011; 4: 226–234. [DOI] [PMC free article] [PubMed] [Google Scholar]