Abstract
Background:
Costs related to diabetic foot ulcer (DFU) care are greater than $1 billion annually and rising. We sought to describe the impact of diabetes mellitus (DM) on foot ulcer admissions in the United States, and to investigate potential explanations for rising hospital costs.
Methods:
The Nationwide Inpatient Sample (2005–2010) was queried using International Classification of Diseases, 9th Revision (ICD-9) codes for a primary diagnosis of foot ulceration. Multivariable analyses were used to compare outcomes and per-admission costs among patients with foot ulceration and DM versus non-DM.
Results:
In total, 962,496 foot ulcer patients were admitted over the study period. The overall rate of admissions was relatively stable over time, but the ratio of DM versus non-DM admissions increased significantly (2005: 10.2 vs. 2010: 12.7; P < 0.001). Neuropathy and infection accounted for 90% of DFU admissions, while peripheral vascular disease accounted for most non-DM admissions. Admissions related to infection rose significantly among DM patients (2005: 39,682 vs. 2010: 51,660; P < 0.001), but remained stable among non-DM patients. Overall, DM accounted for 83% and 96% of all major and minor amputations related to foot ulcers, respectively, and significantly increased cost of care (DM: $1.38 vs. non-DM: $0.13 billion/year; P < 0.001). Hospital costs per DFU admission were significantly higher for patients with infection compared with all other causes ($11,290 vs. $8,145; P < 0.001).
Conclusions:
Diabetes increases the incidence of foot ulcer admissions by 11-fold, accounting for more than 80% of all amputations and increasing hospital costs more than 10-fold over the 5 years. The majority of these costs are related to the treatment of infected foot ulcers. Education initiatives and early prevention strategies through outpatient multidisciplinary care targeted at high-risk populations are essential to preventing further increases in what is already a substantial economic burden.
INTRODUCTION
The prevalence of diabetes mellitus is increasing annually across the United States. The number of hospital discharges associated with diabetes has increased from 4.6 million in 2001 to 5.5 million in 2009.1 As a result, costs associated with diabetes care are also rising. In 2012, the direct medical costs associated with diabetes were $176 billion, which is 2.3 times higher than healthcare costs associated with care of nondiabetic patients.2
Approximately 33% of diabetes-related costs have been linked to the treatment of foot ulcers,3 the majority of which are related to inpatient hospital admissions.4 Hospital inpatient care accounts for at least 50% of the national diabetes cost burden overall,5 and hospital charges and costs related to diabetic foot ulcers specifically have increased significantly over the past 5 years.6 Interestingly, hospital admissions for diabetic foot ulcers were relatively stable between 2003 and 2007, ranging from 112,000 to 115,000 admissions per year.7 In addition, the rate of lower extremity amputation among patients with diabetes is stable or even decreasing; the estimated lower extremity amputation rate among diabetic patients was 3.1/10,000 admissions in 2001 compared with 2.2/10,000 admissions in 2009.8 Therefore it is currently unclear why hospital costs associated with diabetic foot ulcer care is increasing.
In this study, we sought to describe the impact of diabetes on foot ulcer admissions in the United States, including the etiology, incidence of major and minor lower extremity amputations, and to investigate potential explanations for rising hospital costs among patients with foot ulcers and diabetes compared with those with foot ulcers and no diabetes.
METHODS
Study Design
Data were obtained from the Healthcare Cost and Utilization Project’s (HCUP) Nationwide Inpatient Sample (NIS). We performed a retrospective analysis of all patients aged 18 to 99 years, admitted with a primary diagnosis of foot ulceration (ICD-9 codes 440.23, 707.14–707.15) between January 1, 2005 and December 31, 2010. Patients admitted for trauma, acute limb ischemia, compartment syndrome, fasciotomy, pressure ulcers, venous hypertension, or gestational diabetes, as well as those with missing amputation data and/or cost, were excluded. This study was approved by the Johns Hopkins Institutional Review Board.
Variables pertaining to patient demographics (age, sex, race), insurance status (private, government, uninsured), median household income (stratified by quartile), admission status (elective versus urgent), and hospital characteristics (teaching status, bed size, geographic location, and urban versus rural location) were abstracted from the database. Charlson comorbidity scores were calculated for each patient using the International Classification of Diseases Program for Injury Categorization program.9
Statistical Analysis
For the purposes of analysis, patients were stratified into 2 groups: those with diabetes versus those without. We first described trends in foot ulcer admissions over time (2005–2010), and then based on limb pathology and diabetes status. Patients admitted with a primary diagnosis of foot ulceration were identified as having diabetes versus no diabetes using ICD-9 codes. Similarly, foot ulcer admissions were stratified by admission related to infection (cellulitis, abscess, osteomyelitis, and/or inpatient use of intravenous antibiotics), neuropathy, peripheral vascular disease (PVD), and gangrene based on ICD-9 diagnosis codes. Patients with more than one limb pathology diagnosis were coded as such; as a result, the prevalence of each diagnosis is presented as a proportion. Admission numbers are provided as actual values (not weighted values). A full summary of the ICD-9 diagnosis codes used in this study is provided in Supplementary Table 1.
The incidence of major and minor amputations was then compared between patients with foot ulcers and diabetes versus those with foot ulcers and no diabetes using both univariable and multivariable logistic regression analyses. Covariates in the multivariable model included age, sex, race, income quartile, payer status, year of admission, hospital location by US census region, hospital location by urban/rural location, hospital teaching status, elective versus nonelective admission, Charlson comorbidity index, concurrent gangrene, concurrent infection, endovascular revascularization, and open revascularization.
Finally, we report hospital costs associated with foot ulcer admissions. Cost of care per inpatient stay was calculated using hospital-specific cost-to-charge ratio provided by HCUP. The mean cost per inpatient admission among diabetics and nondiabetics with foot ulcers was compared after adjusting for age, sex, race, income quartile, payer status, year of admission, hospital bed size, hospital location by US census region, hospital location by urban/rural location, hospital teaching status, emergency/elective admission, Charlson comorbidity score categories, endovascular revascularization, open revascularization, minor amputation, type of co-occurring lower limb pathology, and length of stay. All dollar values reported were adjusted for inflation and are presented in 2010 US dollars.10
All analyses were performed using Stata version 12.0 (StataCorp, College Station, TX) with significance set at P < 0.05.
RESULTS
Temporal Trends in Foot Ulcer Admissions Over Time
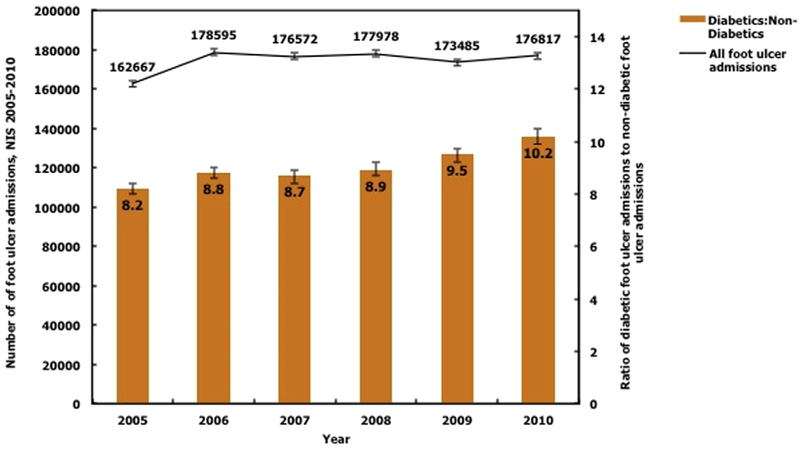
There were 962,496 foot ulcer admissions over the 6-year study period. Of these, 91.8% (n = 883,463) of admissions were among patients with diabetes, compared with 8.2% (n = 79,033) admissions among patients with no diabetes. The number of foot ulcer admissions in 2005 was 150,418 (95% confidence interval [CI] 148,755–152,082). The number of foot ulcer admissions increased to 165,277 (95% CI 163,537–167,016) in 2006 (P < 0.001), after which there were no significant variations in the number of admissions in subsequent years (all, P = nonsignificant [NS]). However, the ratio of diabetic to nondiabetic foot ulcer admissions increased significantly over time from 10.2 (95% CI 9.9–10.5) in 2005 to 12.7 (95% CI 12.4–13.0) in 2010 (Fig. 1). The overall ratio of foot ulcer admissions was significantly higher among patients with diabetes versus those without diabetes (11.2, 95% CI 10.8–11.5; P < 0.001).
Fig. 1.
Temporal trends in the number of foot ulcer admissions and the ratio of diabetic to nondiabetic foot ulcer admissions from 2005 to 2010. There were 962,496 foot ulcer admissions over the 6-year study period. The overall number of foot ulcer admissions was relatively stable between 2005 and 2010, but the ratio of diabetic to nondiabetic foot ulcer admissions increased significantly over time from 10.2 in 2005 to 12.7 in 2010 (P < 0.001).
Patient Demographics
The baseline characteristics of patients admitted with a primary hospital diagnosis of foot ulcer between 2005 and 2010 are listed in Table I. Patients admitted with foot ulceration and diabetes were younger (64.8 ± 0.04 vs. 70.7 ± 0.13 years), and more frequently male (54.0% vs. 51.9%), black (18.2% vs. 11.6%), uninsured (5.5% vs. 3.5%), and among the lowest household income bracket (35.3% vs. 30.4%) compared with patients admitted with foot ulceration and no diabetes (all, P < 0.001). Diabetic foot ulcer patients were also sicker (Charlson comorbidity index > 3: 10.8% vs. 5.8%), more frequently admitted urgently/emergently (85.1% vs. 54.1%), and more frequently admitted to nonteaching hospitals (56.2% vs. 51.8%) than nondiabetics (all, P < 0.001).
Table I.
Characteristics of inpatients with a primary diagnosis of foot ulcers, 2005–2010
| Inpatients with foot ulcers (n = 962,496) |
P value | |||
|---|---|---|---|---|
| No diabetes |
Diabetes |
|||
| Population characteristics | n = 79,033 (8.2%)b | n = 883,463 (91.8%)b | ||
| Patient-level characteristics | ||||
| Age (years)a | 70.7 ± 0.13 | 64.8 ± 0.04 | <0.001 | |
| 18–39 | 4,199 (5.4) | 46,742 (5.4) | <0.001 | |
| 40–64 | 20,415 (26.2) | 374,509 (43.3) | ||
| >65 | 53,228 (68.4) | 444,610 (51.4) | ||
| Female | 37,968 (48.1) | 405,848 (46.0) | <0.001 | |
| Race | <0.001 | |||
| White | 46,103 (58.3) | 415,244 (47.0) | ||
| Black | 9,158 (11.6) | 160,373 (18.2) | ||
| Hispanic | 3,803 (4.8) | 99,825 (11.3) | ||
| Other | 2,236 (2.8) | 45,876 (5.2) | ||
| Not reported | 17,733 (22.4) | 162,145 (18.4) | ||
| Insurance status | <0.001 | |||
| Private | 10,482 (13.3) | 167,399 (19.0) | ||
| Government | 65,685 (83.2) | 665,287 (75.5) | ||
| Uninsured | 2,783 (3.5) | 49,100 (5.5) | ||
| Median household income quartile | <0.001 | |||
| Lowest quartile (Poorest) | 23,494 (30.4) | 302,912 (35.3) | ||
| 2nd quartile | 19,905 (25.8) | 223,271 (26.0) | ||
| 3rd quartile | 17,610 (22.9) | 183,271 (21.4) | ||
| Highest quartile (wealthiest) | 16,068 (20.9) | 147,951 (17.3) | ||
| Nonelective admission | 42,635 (54.1) | 750,396 (85.1) | <0.001 | |
| Charlson index > 3 | 4,593 (5.8) | 95,104 (10.8) | <0.001 | |
| Hospital-level characteristics | ||||
| Teaching hospital | 37,914 (48.2) | 384,703 (43.8) | <0.001 | |
| Hospital bed size | <0.001 | |||
| Small | 9,949 (12.6) | 120,816 (13.7) | ||
| Medium | 18,901 (24.0) | 223,489 (25.4) | ||
| Large | 49,883 (63.4) | 534,856 (60.8) | ||
| Urban hospital | 70,862 (90.0) | 762,846 (86.8) | <0.001 | |
Data are expressed as mean ± standard error of the mean.
Counts may not add up due to missing values.
Foot Ulcer Admissions Stratified by Limb Pathology
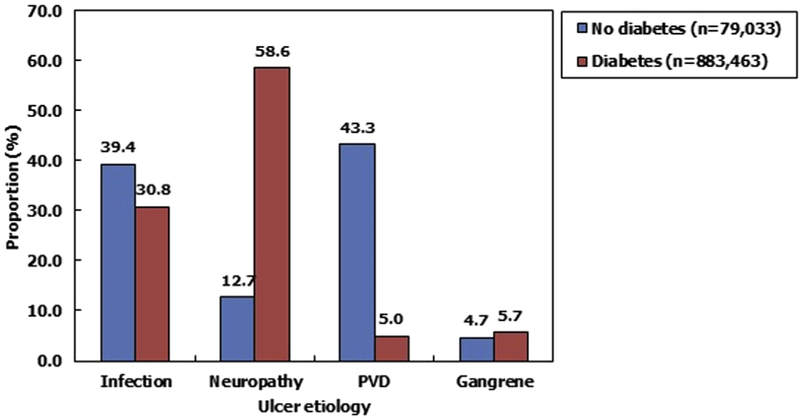
When stratified based on limb pathology, more than half (58.6%; n = 517,709) of foot ulcer admissions among diabetic patients were for simple neuropathic foot ulcers occurring in the absence of infection, PVD, or gangrene (Fig. 2). The second most common reason for foot ulcer admission among diabetic patients was infection, occurring in 30.8% (n = 272,107). Overall, neuropathy and infection accounted for 89.4% of all diabetic foot ulcer admissions. Isolated PVD (5.0%; n = 44,173) and gangrene (5.7%; n = 50,357) were rare.
Fig. 2.
Proportion of diabetic versus nondiabetic inpatients with foot ulcers stratified by limb pathology. More than half of foot ulcer admissions among diabetic patients were for simple neuropathic foot ulcers, followed by infection. In contrast, foot ulcer admissions among nondiabetic patients were most frequently related to PVD. Overall, infection accounted for 31.5% of all foot ulcer admissions (n = 303,246). Note: Numbers may add up to more than 100% because patients may have had >1 limb pathology diagnosis.
In contrast, among nondiabetics almost half of all foot ulcer admissions were related to PVD (43.3%; n = 34,221), followed by infection (39.4%; n = 31,139). Simple neuropathic foot ulcers (12.7%; n = 10,037) and gangrene (4.7%; n = 3,715) were less common.
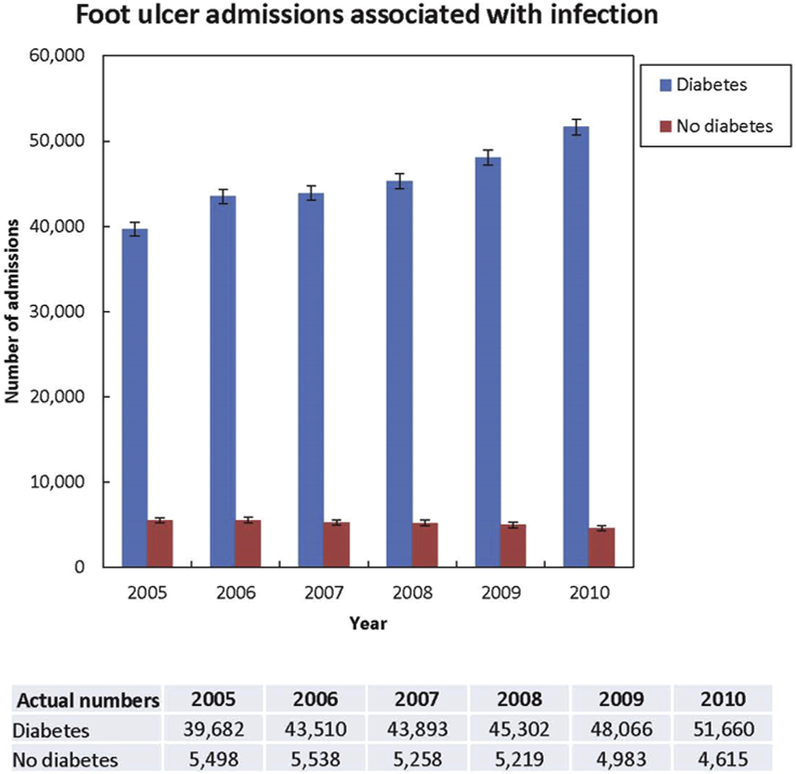
Overall, infection accounted for 31.5% of all foot ulcer admissions (n = 303,246). Admissions related to infection rose significantly among DM patients (2005: 39,682 vs. 2010: 51,660; P < 0.001), but remained stable among non-DM patients (P = NS; Fig. 3).
Fig. 3.
Trends in foot ulcer admissions related to infection over time for patients with diabetes versus no diabetes. Admissions related to infection rose significantly over time among DM patients (P < 0.001), but remained stable among non-DM patients (P = NS).
Effect of Diabetes on Incidence of Major and Minor Amputations for Foot Ulcers
Overall, there were 21,305 major amputations performed for foot ulcers over the 6-year study period. Of these, 17,669 major amputations occurred among diabetic patients, compared with 3,636 major amputations among nondiabetic patients. As such, diabetes accounted for 82.9% of all major amputations among patients admitted with a primary diagnosis of foot ulceration, while the nondiabetes group accounted for only 17.1% of all major amputations (P < 0.001). Of note, the overall proportion of diabetic foot ulcer patients requiring major amputation during hospital admission was only 2.0%, compared with 4.6% in the nondiabetic group (P < 0.001). When stratified by limb pathology (Table II), the proportion of diabetic patients requiring major amputation per admission was significantly lower for those patients presenting with simple neuropathic foot ulcers, PVD, and gangrene (P ≤ 0.003). There were no differences in major amputation rates per admission between diabetic and nondiabetic patients presenting with foot ulcers related to infection (P = 0.62).
Table II.
Proportion of major and minor amputation per admission among patients admitted with foot ulcers comparing diabetics with nondiabetics, stratified by limb pathology
| Major amputation (%) |
P value | Minor amputation (%) |
P value | |||
|---|---|---|---|---|---|---|
| Limb pathology | No diabetes | Diabetes | No diabetes | Diabetes | ||
| Overall | 4.6 | 2.0 | <0.001 | 5.2 | 11.6 | <0.001 |
| Infection | 3.7 | 4.3 | 0.013 | 7.4 | 28.9 | <0.001 |
| Neuropathy | 1.7 | 0.3 | <0.001 | 5.1 | 1.2 | <0.001 |
| PVD | 5.6 | 4.0 | <0.001 | 1.7 | 2.4 | 0.002 |
| Gangrene | 17.6 | 11.0 | <0.001 | 27.1 | 42.9 | <0.001 |
No diabetes, n = 79,033; diabetes, n = 883,463.
Minor amputations were performed in 106,592 patients overall, including 102,482 minor amputations in diabetic patients and 4,110 amputations in nondiabetic patients. As such, diabetes accounted for 96.1% of all minor amputations among patients admitted with a primary diagnosis of foot ulceration, while the nondiabetes group accounted for only 3.9% of all minor amputations. The proportion of diabetic foot ulcer patients requiring minor amputation during hospital admission was 11.6%, compared with 5.2% in the nondiabetes group (P < 0.001). When stratified by limb pathology (Table II), the proportion of diabetic patients requiring minor amputation was higher in patients presenting with infection, gangrene, and PVD (all, P < 0.001). Diabetic patients with simple neuropathic foot ulcers had lower minor amputation rates than nondiabetic patients (1.2% vs. 5.1%; P < 0.001).
Multivariable analysis controlling for patient- and hospital-level factors demonstrated that diabetic foot ulcer patients had a significantly lower risk of major amputation per hospital admission overall compared with nondiabetic foot ulcer patients (odds ratio [OR] 0.70, 95% CI 0.64–0.77), but a significantly higher risk of minor amputation (OR 3.27, 95% CI 3.02–3.55; P < 0.001) (Table III). The risk of major amputation for foot ulcers related to infection was also lower for diabetic versus nondiabetic patients during a given hospital admission (OR 0.84, 95% CI 0.72–0.98; P = 0.05), whereas the risk of minor amputation was significantly higher in the infected diabetic population (OR 4.58, 95% CI 4.10–5.11; P < 0.001).
Table III.
Multivariablea analysis assessing major and minor amputation rates per admission comparing diabetics with nondiabetics, stratified by type of limb pathology
| Amputation (0 = nondiabetics, 1 = diabetics) |
Major amputation |
Minor amputation |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Overall | 0.70 | 0.64–0.77 | <0.001 | 3.27 | 3.02–3.55 | <0.001 |
| Infection | 0.84 | 0.72–0.98 | 0.045 | 4.58 | 4.10–5.11 | <0.001 |
| Neuropathy | 0.68 | 0.46–0.99 | 0.030 | 0.64 | 0.50–0.83 | <0.001 |
| PVD | 0.65 | 0.56–0.77 | <0.001 | 1.61 | 1.27–2.02 | <0.001 |
| Gangrene | 0.78 | 0.62–0.97 | 0.026 | 3.45 | 2.91–4.09 | <0.001 |
Multivariable logistic regression controlling for age, sex, race, insurance status, income quartile, elective admission, Charlson comorbidity score, type of limb pathology, hospital location by US census region, urban versus rural assignment, teaching status, year of admission, any open or endovascular revascularization during the same hospitalization.
Effect of Diabetes on Hospital Costs among Patients Admitted with Foot Ulcers
The overall mean adjusted cost of care for diabetic foot ulcers was $9,397 (95% CI 9,350–9,445) per admission (Table IV). Given the sample size of 883,463 diabetic foot ulcer patients, the overall cost incurred throughout the study period was $8.30 billion (95% CI 8.26–8.34 billion). Averaged over 6-year study period (2005–2010), the cost of diabetic foot ulcer care is estimated to be $1.38 billion per year.
Table IV.
Comparing mean cost for inpatient care per admission among diabetics and nondiabetics with foot ulcers
| Adjusteda cost per admission (in 2010 US dollars) |
No diabetes ($) |
Diabetes ($) |
P value |
|---|---|---|---|
| Average cost (95% CI) | Average cost (95% CI) | ||
| Overall | |||
| Unadjusted | 13,566 (13,335–13,798) | 8,842 (8,788–8,896) | <0.001 |
| Adjusted | 9,794 (9,675–9,913) | 9,397 (9,350–9,445) | <0.001 |
| Overall | |||
| No amputation | 8,838 (8,726–8,950) | 8,465 (8,417–8,513) | <0.001 |
| Minor amputation | 13,668 (12,954–14,382) | 14,270 (14,115–14,425) | 0.110 |
| Major amputation | 18,876 (17,735–20,018) | 18,877 (18,381–19,373) | 1.000 |
| Infection | |||
| No amputation | 11,476 (11,23–11,708) | 11,301 (11,199–11,403) | 0.159 |
| Minor amputation | 13,376 (12,348–14,403) | 12,989 (12,841–13,138) | 0.458 |
| Major amputation | 18,830 (16,512–21,148) | 19,101 (18,417–19,785) | 0.826 |
|
| |||
| Among diabetics | Average cost, $ (95% CI) |
||
| No amputation | Minor amputation | Major amputation | |
|
| |||
| Overall | 8,651 (8,601–8,700) | 9,955 (9,851–10,059) | 11,765 (11,473–12,057) |
| Infection | 11,290 (11,194–11,385) | 12,407 (12,265–12,548) | 15,158 (14,659–15,657) |
All pairwise combinations have P < 0.001.
Adjusted for age, sex, race, income quartile, payer status, year of admission, hospital bed size, hospital location by US census region, hospital location by urban/rural location, hospital teaching status, emergency/elective surgery, Charlson comorbidity score categories, endovascular revascularization, open revascularization, minor amputation, type of co-occurring lower limb pathology, and length of stay.
The overall mean adjusted cost of care for nondiabetic foot ulcers was $9,794 (95% CI 9,675–9,913) per admission (Table IV). Given the sample size of 79,033 non-diabetic foot ulcer patients, the overall cost incurred throughout the study period was $0.77 billion (95% CI 0.76–0.78 billion). Averaged over the 6-year study period (2005–2010), the cost of nondiabetic foot ulcer care is estimated to be $0.13 billion per year.
Among those patients admitted with infected foot ulcers, there were no differences comparing costs for diabetic versus nondiabetic patients regardless of whether an amputation was performed (all, P = NS; Table IV). However, among diabetic patients admitted with foot ulceration, hospital costs per admission were significantly higher for patients with infection ($11,290, 95% CI $11,194–11,385) compared with other causes ($8,145, 95% CI $8,096–8,196) (P < 0.0001).
DISCUSSION
The prevalence of diabetes and diabetes-related morbidity is rising. Based on data from the Centers for Disease Control (CDC), the US population in 2010 was 308,745,538.11 Assuming a diabetes prevalence of 8.3%,12 approximately 25,625,880 Americans are currently affected by diabetes. Similarly, hospital costs are rising.6,13,14 Specifically, diabetic foot ulcer care costs the Medicare system approximately $1.5 billion per year,4 ranging anywhere from $3,000 to $108,000 per ulcer depending on the extent and management of disease.15 Understanding the effect of diabetes on foot ulcer admissions, treatment, and hospital costs, it is essential to developing health interventions in this population.
In this study, we sought to describe the impact of diabetes on foot ulcer admissions in the United States, including the temporal trends, etiology, incidence of major and minor lower extremity amputations, and to investigate potential explanations for rising hospital costs among patients with diabetic foot ulcers. Our data demonstrate that the rate of foot ulcer admissions over time was relatively stable overall between 2006 and 2010, but that the ratio of diabetic versus nondiabetic foot ulcer admissions increased significantly over time. Overall, the ratio of foot ulcer admissions was 11 times higher in patients with diabetes compared with those without, totaling nearly 150,000 admissions per year. When stratified based on limb pathology, nearly one-third of foot ulcer admissions among diabetic patients were for infection, which is a preventable condition in many cases.16 Neuropathy and PVD were also common in the diabetes and nondiabetes groups, respectively.
These findings are somewhat surprising in the context of published CDC data demonstrating that hospital admissions for diabetic foot ulcers have been relatively stable between 2003 and 2007.7 However, our study examines trends in diabetic foot ulcer admissions over a longer period of time (2006–2010). We report a marked change in the proportion of patients with diabetic versus nondiabetic foot ulcers between 2008 and 2010 from 10.9 to 12.7, respectively, indicating that increasing diabetic foot ulcer admissions is a contemporary trend that deserves acknowledgment. Interestingly, the proportion of major amputations per foot ulcer admission was lower in diabetic compared with nondiabetic patients in our study, but the minor amputation rates were higher. It is well documented that, overall, diabetic patients are more likely to undergo major amputation than nondiabetic patients.17,18 Consistent with this notion, diabetes accounted for 83% and 96% of major and minor amputations related to foot ulcers in our study, respectively. Therefore, it appears as though diabetic foot ulcer patients are more likely to be admitted for minor amputations and other attempts at limb salvage compared with their nondiabetic counterparts. This assumption is supported by prior work demonstrating that diabetes-related foot ulcer admissions are associated with increasing attempts at limb salvage in recent years.6 For example, we have previously shown that the rate of endovascular revascularizations and minor amputations among diabetic foot ulcer patients have significantly increased in the past 5 years, while major amputation rates remain stable.6
Unfortunately, it appears that these attempts at limb salvage might not be sufficient. According to the CDC, approximately 73,000 nontraumatic lower limb amputations were performed in adults with diabetes in 2010, accounting for about 60% of all major amputations.2 Based on these data, the risk of major amputation is estimated to be 1.5 times higher in patients with diabetes compared with those without. However, diabetes accounted for 83% of all major amputations in our study, compared with 17% in nondiabetics. These data suggest that the risk of major amputation among patients specifically admitted with a primary diagnosis of foot ulceration is 5 times higher in patients with diabetes compared with those without. As a result, the presence of diabetes and foot ulcer combined appears to increase the risk of major amputation by 3.2-fold per patient overall, despite a lower per-admission risk.
The high rate of amputations associated with diabetic foot ulcers has substantial financial implications. In general, medical costs for diabetes in 2012 were $176 billion, which was 2.3 times higher than medical costs related to no diabetes,2 and costs associated with the treatment of diabetic foot ulcers are increasing significantly over time.6 In this study, we found that the cost of diabetic foot ulcer care is estimated to be $1.38 billion per year, compared with $0.13 billion per year in nondiabetic foot ulcer patients. As a result, the presence of diabetes appears to increase the cost of foot ulcer care by 10-fold. Although the adjusted hospital costs per foot ulcer admission were actually lower among diabetic versus nondiabetic patients, diabetic patients with foot ulcers have a hospital readmission rates as high as 34%.19 This suggests that a need for multiple admissions over time is likely the driving force behind rising costs in diabetes care. As such, the per-patient costs for treatment of foot ulcers are likely substantially higher among the diabetic population, especially given the increased risk of minor amputations in this group.
One strategy to reduce the costs associated with diabetic foot ulcers is through early identification and treatment before the ulcer reaches a stage that requires inpatient admission. Early referral to multidisciplinary diabetic foot clinics can decrease progression of disease,20 and limb salvage teams that address the prevention, surveillance, and management of foot ulcers can improve outcomes via a multidisciplinary approach.3,21–24 Deep infection and gangrene, specifically, are preventable with compliant outpatient foot ulcer care. Our data suggest that infection is the main driving force behind the hospital admission and health economic burden associated with diabetic foot ulcers. In addition, our data also suggest that patients with diabetic foot ulcers tended to be young black males of low socioeconomic status. These findings are consistent with prior studies demonstrating a higher risk of foot ulcers among disadvantaged populations,25,26 frequently due to recurrent infections of prior wounds site due to poor compliance with outpatient treatment.27 Therefore initiatives that target the identification of these high-risk patients that would benefit from foot ulcer screening and early intervention would be helpful. By preventing infection and minimizing the need for minor amputation among diabetic foot ulcer patients early in their disease course, we could potentially reduce the incidence of major amputations and ultimately the exorbitant hospital costs associated with diabetic foot ulcers.
The limitations of our study deserve discussion. We used data from the NIS that, like any administrative database, can suffer from administrative coding errors and missing data. As a result, it is possible that some of the diagnoses of foot ulceration that we identified using ICD-9 codes are not entirely representative of the disease state of interest. However, given that 962,496 foot ulcer patients were identified for analysis in this study, it is our hope that the effects of coding errors are minimized and the overall trends that we report are accurate. In addition, the NIS provides only per-admission information, so it is impossible to determine whether a patient has been admitted multiple times for the same diagnosis, or whether each admission represents a unique patient. Based on Agency for Healthcare Research and Quality (AHRQ) data reporting a 34% readmission rate among diabetes patients,19 we assume that many admissions represent repeat admissions for the same patient, which would explain why the per-admission major amputation rates are lower in the diabetes foot ulcer group even though it is well known that major amputation is significantly more common among diabetic patients overall.17,18 Future studies investigating the per-patient costs related to diabetic foot ulcer treatment would be helpful in delineating the precise economic burden of this disease.
In conclusion, the rate of foot ulcer admissions over time is increasing substantially among the diabetic population. The ratio of foot ulcer admissions is at least 11 times higher in patients with diabetes compared with those without, accounting for 83% and 96% of major and minor amputations, respectively. As a result, the national costs associated with diabetic foot ulcers have become astronomical, more than 10-fold that of the cost of nondiabetic foot ulcer care. Despite previous estimates that admissions for DFU were stable, these data suggest that efforts at limb salvage have resulted in a recent increase in hospital admissions and associated costs. The majority of these costs are related to the treatment of infected ulcers, which is often a preventable disease. Education initiatives and early prevention strategies with compliant outpatient multidisciplinary care targeted at high-risk populations are essential to preventing further increases in what is already a substantial economic burden.
Supplementary Material
Footnotes
SUPPLEMENTARY DATA
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.avsg.2015.11.025.
Disclosures: No competing interests declared. This work was completed without financial support.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). Number (in Thousands) of Hospital Discharges with Diabetes as Any-Listed Diagnosis, United States, 1988–2009. Available at: http://www.cdc.gov/diabetes/statistics/dmany/fig1.htm; 2009. Accessed 12 February, 2014.
- 2.Centers for Disease Control and Prevention (CDC). National Diabetes Statistic Report, 2014. Available at: http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf; 2014. Accessed 12 February, 2014.
- 3.Driver VR, Fabbi M, Lavery LA, et al. The costs of diabetic foot: the economic case for the limb salvage team. J Vasc Surg 2010;52:17S–22S. [DOI] [PubMed] [Google Scholar]
- 4.Harrington C, Zagari MJ, Corea J, et al. A cost analysis of diabetic lower-extremity ulcers. Diabetes Care 2000;23: 1333–8. [DOI] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008;31:596–615. [DOI] [PubMed] [Google Scholar]
- 6.Hicks CW, Selvarajah S, Mathioudakis N, et al. Trends and determinants of costs associated with the inpatient care of diabetic foot ulcers. J Vasc Surg 2014;60:1247–54. 1254.e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). Number (in Thousands) of Hospital Discharges with Peripheral Arterial Disease (PAD), Ulcer/Inflammation/Infection (ULCER), or Neuropathy as First-Listed Diagnosis and Diabetes as Any-Listed Diagnosis United States, 1988–2007. Available at: http://www.cdc.gov/diabetes/statistics/hosplea/diabetes_complications/fig1_number.htm; 2014. Accessed 12 February, 2014.
- 8.Centers for Disease Control and Prevention (CDC). Number (in Thousands) of Hospital Discharges for Nontraumatic Lower Extremity Amputation with Diabetes as a Listed Diagnosis, United States, 1988–2009. Available at: http://www.cdc.gov/diabetes/statistics/lea/fig1.htm; 2012. Accessed 12 February, 2014.
- 9.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores. Available at: http://ideas.repec.org/c/boc/bocode/s457028.html#biblio; 2010. Accessed 27 April, 2013.
- 10.Sahr RC. Consumer Price Index (CPI) Conversion Factors 1774 to Estimated 2022 to Convert to Dollars of 2010. Available at: http://oregonstate.edu/cla/polisci/sites/default/files/faculty-research/sahr/inflation-conversion/pdf/cv2010.pdf; 2013. Accessed 24 February, 2014.
- 11.Centers for Disease Control and Prevention (CDC). NVSS—National Vital Statistics System. Available at: http://www.cdc.gov/nchs/nvss.htm; 2014. Accessed 12 February, 2014.
- 12.Centers for Disease Control and Prevention (CDC). Diabetes Data & Trends. Available at: http://apps.nccd.cdc.gov/DDTSTRS/default.aspx. Accessed 16 December, 2013.
- 13.Chow I, Lemos EV, Einarson TR. Management and prevention of diabetic foot ulcers and infections: a health economic review. Pharmacoeconomics 2008;26:1019–35. [DOI] [PubMed] [Google Scholar]
- 14.McInnes AD. Diabetic foot disease in the United Kingdom: about time to put feet first. J Foot Ankle Res 2012;5:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavanagh P, Attinger C, Abbas Z, et al. Cost of treating diabetic foot ulcers in five different countries. Diabetes Metab Res Rev 2012;28:107–11. [DOI] [PubMed] [Google Scholar]
- 16.Boulton AJ, Kirsner RS, Vileikyte L. Clinical practice. Neuropathic diabetic foot ulcers. N Engl J Med 2004;351:48–55. [DOI] [PubMed] [Google Scholar]
- 17.Al-Thani H, El-Menyar A, Koshy V, et al. Implications of foot ulceration in hemodialysis patients: a 5-year observational study. J Diabetes Res 2014;2014:945075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cull DL, Manos G, Hartley MC, et al. An early validation of the Society for Vascular Surgery Lower Extremity Threatened Limb Classification System. J Vasc Surg 2014;60: 1535–41. [DOI] [PubMed] [Google Scholar]
- 19.Agency for Healthcare and Research Quality (AHRQ). Table 1. Annual Rate of Diabetic Foot Ulcer (DFU) and Any Readmissions Among Diabetic Medicare Parts A and B Fee-for-Service (FFS) Beneficiaries With DFU, 2006–2008, by Age, Gender, and Race 2007. Available at: http://www.effectivehealthcare.ahrq.gov/tasks/sites/ehc/assets/File/Data-Points_3_Diabetic-Foot-Ulcers-Amputations_Data_03-20111.pdf; 2007.
- 20.Williams DT, Majeed MU, Shingler G, et al. A diabetic foot service established by a department of vascular surgery: an observational study. Ann Vasc Surg 2012;26:700–6. [DOI] [PubMed] [Google Scholar]
- 21.Zayed H, Halawa M, Maillardet L, et al. Improving limb salvage rate in diabetic patients with critical leg ischaemia using a multidisciplinary approach. Int J Clin Pract 2009;63: 855–8. [DOI] [PubMed] [Google Scholar]
- 22.Driver VR, Madsen J, Goodman RA. Reducing amputation rates in patients with diabetes at a military medical center: the limb preservation service model. Diabetes Care 2005; 28:248–53. [DOI] [PubMed] [Google Scholar]
- 23.Driver VR, Goodman RA, Fabbi M, et al. The impact of a podiatric lead limb preservation team on disease outcomes and risk prediction in the diabetic lower extremity: a retrospective cohort study. J Am Podiatr Med Assoc 2010;100: 235–41. [DOI] [PubMed] [Google Scholar]
- 24.Conte MS. Diabetic revascularization: endovascular versus open bypass—do we have the answer? Semin Vasc Surg 2012;25:108–14. [DOI] [PubMed] [Google Scholar]
- 25.Amin L, Shah BR, Bierman AS, et al. Gender differences in the impact of poverty on health: disparities in risk of diabetes-related amputation. Diabet Med 2014;31:1410–7. [DOI] [PubMed] [Google Scholar]
- 26.Bruun C, Siersma V, Guassora AD, et al. Amputations and foot ulcers in patients newly diagnosed with type 2 diabetes mellitus and observed for 19 years. The role of age, gender and co-morbidity. Diabet Med 2013;30:964–72. [DOI] [PubMed] [Google Scholar]
- 27.Ang CL, Lim YJ. Recurrent admissions for diabetic foot complications. Malays Orthop J 2013;7:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.