Abstract
BACKGROUND
Platelet counts of less than 150,000 per cubic millimeter during uncomplicated pregnancies are described as gestational thrombocytopenia if no alternative cause is identified. Platelet counts may be even lower in women with pregnancy-related complications. However, the occurrence and severity of thrombocytopenia throughout pregnancy are not defined.
METHODS
We evaluated platelet counts throughout pregnancy in women who delivered at Oklahoma University Medical Center between 2011 and 2014. These platelet counts were compared with those of nonpregnant women who were included in the National Health and Nutrition Examination Survey from 1999 through 2012.
RESULTS
Among the 15,723 deliveries that occurred during the study period, 7351 women had sufficient data for our analyses. Of these women, 4568 had uncomplicated pregnancies, 2586 had pregnancy-related complications, and 197 had preexisting disorders associated with thrombocytopenia. Among the women who had uncomplicated pregnancies, the mean platelet count in the first trimester (mean gestation, 8.7 weeks) was 251,000 per cubic millimeter, which was lower than the mean platelet count in the 8885 nonpregnant women (273,000 per cubic millimeter) (P<0.001). At the time of delivery, 9.9% of the women with uncomplicated pregnancies had a platelet count below 150,000 per cubic millimeter. During the course of the uncomplicated pregnancies and deliveries, only 45 women (1.0%) had a platelet count below 100,000 per cubic millimeter. Among the 12 women with uncomplicated pregnancies who had a platelet count below 80,000 per cubic millimeter, only 5 (0.1%, among whom the range of platelet counts was 62,000 to 78,000 per cubic millimeter; median, 65,000) were identified by medical record review as having no alternative cause for the thrombocytopenia. Platelet counts of less than 150,000 per cubic millimeter at the time of delivery were more common among women who had pregnancy-related complications than among women who had uncomplicated pregnancies (11.9% vs. 9.9%, P = 0.01). Throughout their pregnancies and deliveries, 59 women (2.3%) with pregnancy-related complications had a platelet count below 100,000 per cubic millimeter, and 31 (1.2%) had a platelet count below 80,000 per cubic millimeter.
CONCLUSIONS
Mean platelet counts decreased during pregnancy in all the women, beginning in the first trimester. In women who have a platelet count of less than 100,000 per cubic millimeter, a cause other than pregnancy or its complications should be considered. (Funded by the National Heart, Lung, and Blood Institute.)
Beginning in 1993, three large studies documented that 5 to 10% of women who had uncomplicated pregnancies had a platelet count of less than 150,000 per cubic millimeter at the time of delivery,1–3 which was described as gestational thrombocytopenia.4 The normal distribution of platelet counts at the time of delivery and the absence of health problems in the mother and infant suggested that gestational thrombocytopenia was the result of lower platelet counts that occur in all women during pregnancy.2,3,5,6 The current thinking is that platelet counts in all women begin to decrease in the mid-second to third trimester and continue to decrease until the time of delivery.4 However, our recent systematic review of published reports that describe platelet counts throughout uncomplicated pregnancies did not provide support for this concept.7 The number of published reports that we were able to identify was few, and their results were inconsistent.
Pregnancy-related complications, such as pre-eclampsia, may also cause thrombocytopenia.4,8–10 Therefore, it may be hypothesized that platelet counts in women who have pregnancy-related complications are lower than platelet counts in women who have uncomplicated pregnancies. In addition, thrombocytopenia in women who have preexisting disorders, such as immune thrombocytopenic purpura, may become more severe during pregnancy.4,11 To understand the course of platelet counts throughout pregnancy, we evaluated platelet counts in women who delivered at the Oklahoma University Medical Center between 2011 and 2014. Our objectives with respect to women who had uncomplicated pregnancies were to learn the course of platelet counts throughout pregnancy, the potential severity of gestational thrombocytopenia, and the risk for recurrence of gestational thrombocytopenia with a subsequent pregnancy. Our objective with respect to women who had complicated pregnancies was to determine whether there is a relationship between the identified complications and platelet counts. Our objective with respect to women who had preexisting disorders associated with thrombocytopenia was to learn whether their thrombocytopenia becomes more severe during pregnancy.
METHODS
STUDY POPULATIONS
We analyzed the platelet counts in women 15 to 44 years of age who delivered at Oklahoma University Medical Center between January 1, 2011, and August 19, 2014. Demographic data, platelet counts, medical-record numbers, and diagnosis codes identified from electronic medical records were combined into a single database. If a woman had multiple pregnancies during the study period, only the first uncomplicated pregnancy was included; if the woman had no uncomplicated pregnancies, the first complicated pregnancy was included. In our primary analyses, we included women who had a singleton pregnancy, whose duration of gestation at the time of delivery was recorded, and who had a platelet count measurement at the time of delivery and at least one additional platelet count measurement during their pregnancy. Pregnancy-related complications that were recorded as such were hypertension or diabetes before or during pregnancy, preeclampsia, HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome, preterm birth (defined as birth before 37 weeks of gestation), stillbirth, and placental abnormalities (e.g., placental abruption, placenta previa, or placenta accreta). Preexisting disorders that were considered to be associated with thrombocytopenia were recorded as immune thrombocytopenic purpura, systemic lupus erythematosus, human immunodeficiency virus infection, and hepatitis B or C. Women who did not have these pregnancy-related complications or preexisting disorders were considered to have had uncomplicated pregnancies even though they could have had other diagnoses that could be considered as complicating a pregnancy, such as a history of treated cancer. Data from women who had uncomplicated twin pregnancies were analyzed separately according to the same selection criteria, except that uncomplicated delivery was defined as birth at or after 34 weeks of gestation.
Data on nonpregnant women 15 to 44 years of age from the National Health and Nutrition Examination Survey (NHANES) from 1999 through 2012 were used for comparisons. We recorded each woman’s platelet count, race or ethnic group, and age. Women who reported having received a diagnosis of hypertension, diabetes, or cancer were excluded.
PLATELET COUNTS
Platelet counts were measured with standard electronic equipment maintained in laboratories certified by the Clinical Laboratory Improvement Amendments program and were categorized according to the following time periods: first trimester of pregnancy, 0 to 13 weeks of gestation; second trimester, 14 to 27 weeks; third trimester, 28 to 42 weeks (excluding the time within 48 hours before delivery); delivery; and postpartum period (defined as 4 to 12 weeks after delivery). To determine the course of platelet counts throughout pregnancy, at the time of delivery, and during the postpartum period, we selected only one platelet count measurement from each time point for each woman: the first platelet count measurement during each trimester and the postpartum period and the platelet count measurement preceding and closest to the time of delivery. To identify the lowest platelet counts throughout pregnancy and at the time of delivery, we reviewed all the platelet counts that had been measured during pregnancy up to the time of delivery. To search for potential alternative causes of platelet counts less than 80,000 per cubic millimeter in women who had uncomplicated pregnancies, we reviewed the woman’s entire set of medical records from Oklahoma University Medical Center.
STATISTICAL ANALYSIS
To determine whether platelet counts changed significantly during gestation, whether they differed significantly among races or ethnic groups or age groups, and whether the rate of decrease during pregnancy differed significantly between women who had uncomplicated pregnancies and women who had pregnancy-related complications or preexisting disorders, we constructed linear mixed models to account for women who had repeated platelet count measurements. To compare postpartum platelet counts with platelet counts at the time of delivery, we used a paired t-test. We calculated the number and percentage of women with pregnancy-related complications who had a platelet count of less than 150,000 per cubic millimeter, less than 100,000 per cubic millimeter, and less than 80,000 per cubic millimeter and compared them, using chi-square tests, with the corresponding numbers and percentages of women with uncomplicated pregnancies. For the analysis of the NHANES data, we used the sampling weights provided by NHANES to account for the complex survey design, which included oversampling of some populations, and to account for cases in which participants either did not respond to the survey or did not complete all aspects of the survey.12,13 To compare the platelet counts of the pregnant women with those of the nonpregnant women from NHANES, we calculated weighted mean platelet counts for all the nonpregnant women overall and also separately for each subgroup of nonpregnant women defined according to race or ethnic group and age. This stratified analysis accounted for any differences in platelet counts on the basis of race or ethnic group or age between the nonpregnant women from NHANES and the pregnant women. After obtaining weighted estimates for the data from the women from NHANES, we used Student’s t-test to compare the platelet counts in the pregnant women with those in the nonpregnant women. Platelet counts at the time of delivery in the women who had singleton pregnancies and in the women who had twin pregnancies were compared with the use of Student’s t-test. To determine the risk in women of having a platelet count of less than 150,000 per cubic millimeter in a subsequent pregnancy if they had had a platelet count of less than 150,000 per cubic millimeter in a previous pregnancy, we calculated a risk ratio and 95% confidence interval. All the analyses were performed with the use of SAS software, version 9.4 (SAS Institute).
RESULTS
OVERVIEW OF STUDY POPULATION
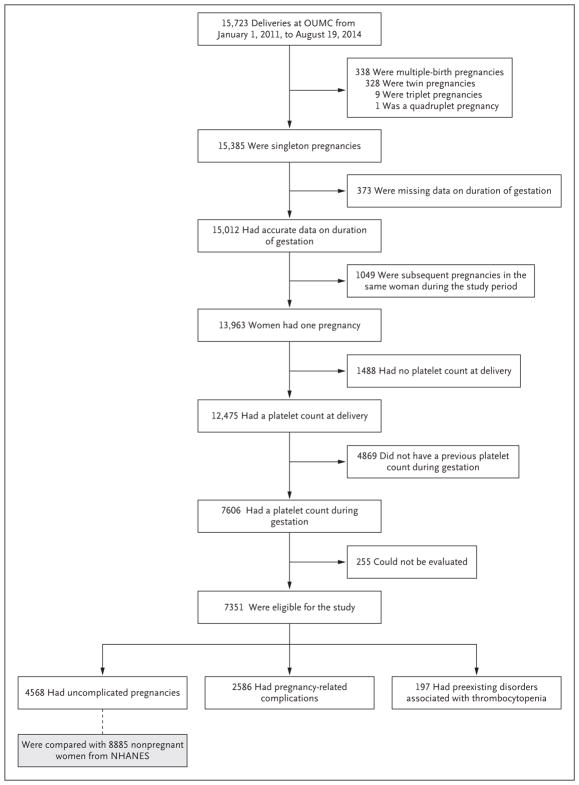
Among the 15,723 deliveries that occurred during our study period, 7351 women had sufficient data for our analyses. Of these women, 4568 had an uncomplicated pregnancy, 2586 had a pregnancy-related complication, and 197 had a pre-existing disorder associated with thrombocytopenia (Fig. 1). The data from the women who had uncomplicated pregnancies were compared with the data from 8885 nonpregnant women from the NHANES database. The characteristics of these women are provided in Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org.
Figure 1. Selection of Women for Analysis of Platelet Counts during Singleton Pregnancies.
Among all 15,723 deliveries that occurred at Oklahoma University Medical Center (OUMC) between January 1, 2011, and August 19, 2014, a total of 7351 women who had a platelet count measurement at the time of delivery and at least one platelet count measurement during their pregnancy were selected for inclusion in our study. The 255 women who could not be evaluated and were therefore deemed to be ineligible included 141 women who reported illicit-drug use, 113 women who had received treatment with glucocorticoids for an indication other than a pregnancy-related complication or a pre-existing disorder, and 1 woman who had thrombotic thrombocytopenic purpura. Data from the 328 women who had twin pregnancies were analyzed separately. NHANES denotes National Health and Nutrition Examination Survey.
WOMEN WITH UNCOMPLICATED PREGNANCIES
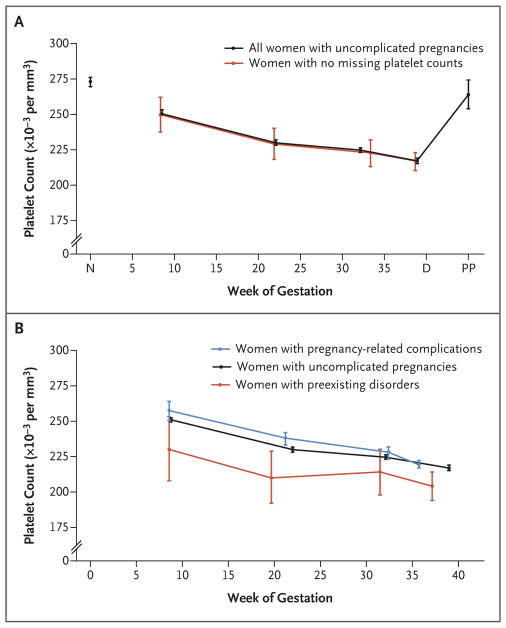
Among all 15,385 women who had singleton pregnancies, 9912 women had uncomplicated pregnancies. Of these women, 4568 (46.1%) had sufficient data for our analyses. The mean platelet counts in the women who had uncomplicated pregnancies and in the nonpregnant women are shown in Figure 2A and Table 1. The mean platelet count in the nonpregnant women was 273,000 per cubic millimeter. In the pregnant women, the platelet counts decreased significantly throughout pregnancy (P<0.001). The mean platelet count was 251,000 per cubic millimeter in the first trimester of pregnancy (mean gestation, 8.7 weeks), 230,000 per cubic millimeter in the second trimester (mean gestation, 22.0 weeks), 225,000 per cubic millimeter in the third trimester (mean gestation, 32.1 weeks), 217,000 per cubic millimeter at the time of delivery (mean gestation, 39.0 weeks), and 264,000 per cubic millimeter during the postpartum period (mean time after delivery, 7.1 weeks). The pregnant women had significantly lower mean platelet counts than the nonpregnant women during each trimester and at the time of delivery (P<0.001). The mean platelet count during the postpartum period did not differ significantly between the women with uncomplicated pregnancies and the nonpregnant women (P = 0.10). Among the 246 women with uncomplicated pregnancies who were assessed during the postpartum period, the mean platelet count was 17% lower at the time of delivery than during the postpartum period (218,000 vs. 264,000 per cubic millimeter).
Figure 2. Mean Platelet Counts over Time.
Panel A shows the mean platelet counts of the women who had uncomplicated pregnancies and of the nonpregnant women. I bars denote 95% confidence intervals. The mean platelet count in the 8885 nonpregnant women is designated by N on the x axis. The mean platelet counts of the 4568 women who had uncomplicated pregnancies are shown at each trimester (with the mean time of gestation when they were measured indicated on the x axis), at the time of delivery (designated by D on the x axis), and during the post-partum period (designated by PP on the x axis). The mean platelet counts of the 336 women with uncomplicated pregnancies who had platelet counts at each trimester and at the time of delivery are also shown in Panel A. The difference in the mean platelet count between the women who had no missing platelet counts and the 4232 women who had missing platelet counts during one or more trimesters was not significant (P = 0.79). Panel B shows the mean platelet counts of the women who had uncomplicated pregnancies, the women who had pregnancy-related complications, and the women who had preexisting disorders that were associated with thrombocytopenia. The platelet counts of all three groups of women decreased significantly throughout pregnancy (P<0.001). The mean platelet counts of the 2586 women who had pregnancy-related complications were higher than those of the 4568 women who had uncomplicated pregnancies during the first and second trimester (P<0.001) but were not significantly different during the third trimester (P = 0.38) or at the time of delivery (P = 0.09). The mean platelet counts of the 197 women who had preexisting disorders associated with thrombocytopenia were lower than those of the women who had uncomplicated pregnancies at all trimesters and at the time of delivery (P<0.03 for all comparisons).
Table 1.
Platelet Counts during Pregnancy and in Nonpregnant Women.*
| Variable | Women with Uncomplicated Singleton Pregnancies | Nonpregnant Women | ||||
|---|---|---|---|---|---|---|
| First Trimester | Second Trimester | Third Trimester | Delivery | Postpartum Period | ||
| Overall | ||||||
|
| ||||||
| No. of women who could be evaluated | 2306 | 2553 | 2254 | 4568 | 246 | 8885 |
|
| ||||||
| Platelet count — ×10−3 per cubic millimeter | ||||||
|
| ||||||
| Mean (95% CI) | 251 (249–253) | 230 (228–232) | 225 (223–226) | 217 (215–219) | 264 (254–274) | 273 (269–276) |
|
| ||||||
| Range | 99–937 | 31–670 | 57–505 | 63–552 | 91–575 | 11–999 |
|
| ||||||
| Race or ethnic group | ||||||
|
| ||||||
| Mean platelet count (95% CI) — ×10−3 per cubic millimeter | ||||||
|
| ||||||
| Black, non-Hispanic | 263 (257–268) | 235 (231–240) | 223 (218–228) | 222 (218–226) | 288 (282–294) | |
|
| ||||||
| Hispanic | 249 (244–255) | 227 (223–232) | 223 (218–228) | 210 (206–214) | 274 (269–279) | |
|
| ||||||
| White, non-Hispanic | 247 (244–249) | 227 (224–229) | 223 (220–225) | 216 (213–218) | 273 (268–277) | |
|
| ||||||
| Age range | ||||||
|
| ||||||
| Mean platelet count (95% CI) — ×10−3 per cubic millimeter | ||||||
|
| ||||||
| 15 to 19 yr | 256 (249–263) | 238 (232–243) | 235 (228–242) | 223 (218–229) | 280 (274–285) | |
|
| ||||||
| 20 to 34 yr | 251 (248–253) | 229 (227–231) | 224 (222–226) | 217 (215–219) | 272 (268–277) | |
|
| ||||||
| 35 to 44 yr | 247 (241–253) | 229 (223–235) | 222 (214–227) | 211 (206–216) | 273 (267–278) | |
|
| ||||||
| Women with Uncomplicated Twin Pregnancies | ||||||
|
| ||||||
| Overall | ||||||
|
| ||||||
| No. of women who could be evaluated | 34 | 37 | 42 | 67 | ||
|
| ||||||
| Mean platelet count (95% CI) — ×10−3 per cubic millimeter | 240 (220–259) | 221 (206–237) | 217 (190–244) | 202 (183–221) | ||
|
| ||||||
| Women with Complicated Pregnancies | ||||||
|
| ||||||
| Complications related to pregnancy | ||||||
|
| ||||||
| No. of women who could be evaluated | 1082 | 1324 | 1664 | 2586 | ||
|
| ||||||
| Platelet count — ×10−3 per cubic millimeter | ||||||
|
| ||||||
| Mean (95% CI) | 258 (253–264) | 238 (233–242) | 228 (224–232) | 219 (217–222) | ||
|
| ||||||
| Range | 58–528 | 102–711 | 70–613 | 32–506 | ||
|
| ||||||
| Pregnant Women with Preexisting Disorders | ||||||
|
| ||||||
| Disorders associated with thrombocytopenia | ||||||
|
| ||||||
| No. of women who could be evaluated | 85 | 120 | 140 | 197 | ||
|
| ||||||
| Platelet count — ×10−3 per cubic millimeter | ||||||
|
| ||||||
| Mean (95% CI) | 230 (208–253) | 210 (192–229) | 214 (198–230) | 204 (194–214) | ||
|
| ||||||
| Range | 60–454 | 29–378 | 4–411 | 24–435 | ||
Data on the mean platelet counts of nonpregnant women were obtained from the National Health and Nutrition Examination Survey (NHANES) database. CI denotes confidence interval.
The mean platelet counts in the nonpregnant women and in the women with uncomplicated pregnancies in the first trimester and at the time of delivery were normally distributed, except for a slight skew toward higher values in all three cases (Fig. 3, and Table S2 in the Supplementary Appendix). The mean platelet count at the time of delivery was higher in non-Hispanic black women than in non-Hispanic white women and Hispanic women (P<0.001) and was higher in younger women (15 to 19 years of age) than in older women (20 to 44 years of age) (P<0.001). These findings were similar to the differences in race or ethnic group and age reported among non-pregnant women in the United States14 (Table 1, and Figs. S1A and S1B in the Supplementary Appendix).
Figure 3. Platelet Count Distribution.
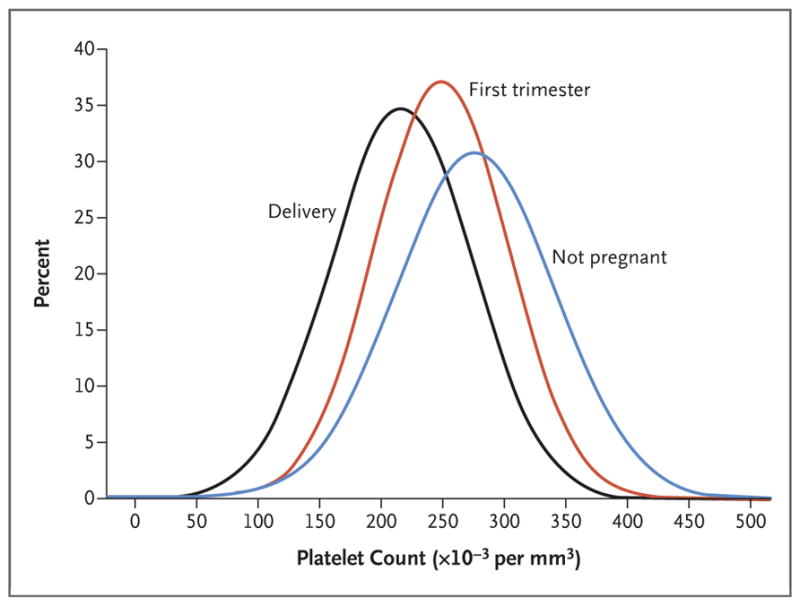
Shown are the distribution of the mean platelet counts of the nonpregnant women and the distribution of the mean platelet counts during the first trimester (mean gestation, 8.7 weeks) and at the time of delivery in the women who had uncomplicated pregnancies. The distributions of the mean platelet counts for all three curves were symmetric, with a slight skew toward higher platelet counts that was consistent across all three curves. The mean and median platelet count values for each of the three distribution curves differed by less than 3%. These analyses are presented in Table S2 in the Supplementary Appendix. Platelet counts measured during the postpartum period were not included in this figure because of the small sample size.
When we evaluated all 13,793 platelet count values measured during pregnancy and at the time of delivery in women with uncomplicated pregnancies (Fig. S2A in the Supplementary Appendix), we found that platelet counts of less than 150,000 per cubic millimeter occurred in 450 women (9.9%) at the time of delivery (Table 2). A total of 45 women (1.0%) had platelet counts below 100,000 per cubic millimeter during pregnancy, at the time of delivery, or both; 12 women had platelet counts below 80,000 per cubic millimeter during pregnancy, at the time of delivery, or both, but only 5 (0.1%) were identified by medical-record review as having no alternative cause for the thrombocytopenia. The alternative causes for the thrombocytopenia that were identified in the other 7 women were immune thrombocytopenic purpura (2 women), pseudothrombocytopenia due to in vitro platelet clumping (2 women), error in measurement of platelet count (2 women), and hereditary thrombocytopenia (1 woman). The platelet counts for these 12 women and the clinical data that supported their diagnoses are summarized in Table S3 in the Supplementary Appendix.
Table 2.
Platelet Counts during Pregnancy and at the Time of Delivery.*
| Platelet count (per mm3), According to Type of Pregnancy | First Trimester | Second Trimester | Third Trimester | Delivery |
|---|---|---|---|---|
| number of women (percent) | ||||
| Women with uncomplicated pregnancies† | ||||
|
| ||||
| ≥150,000 | 2264 (98.2) | 2430 (95.2) | 2062 (91.5) | 4115 (90.1) |
|
| ||||
| 125,000–149,000 | 36 (1.6) | 89 (3.5) | 128 (5.7) | 293 (6.4) |
|
| ||||
| 100,000–124,000 | 5 (0.2) | 29 (1.1) | 48 (2.1) | 126 (2.7) |
|
| ||||
| 80,000–99,000 | 1 (<0.1) | 2 (0.1) | 12 (0.5) | 27 (0.6) |
|
| ||||
| 60,000–79,000 | 0 | 0 | 2 (0.1) | 4 (0.1) |
|
| ||||
| <60,000 | 0 | 0 | 0 | 0 |
|
| ||||
| Women with uncomplicated pregnancies, platelet counts <80,000 per cubic millimeter, and an alternative cause for thrombocytopenia† | ||||
|
| ||||
| 60,000–79,000 | 0 | 2 (0.1) | 1 (<0.1) | 3 (0.1) |
|
| ||||
| <60,000 | 0 | 1 (<0.1) | 1 (<0.1) | 0 |
|
| ||||
| Women with pregnancy-related complications‡ | ||||
|
| ||||
| ≥150,000 | 1060 (97.9) | 1264 (95.5) | 1506 (90.5) | 2279 (88.1) |
|
| ||||
| 125,000–149,000 | 18 (1.7) | 47 (3.5) | 99 (5.9) | 178 (6.9) |
|
| ||||
| 100,000–124,000 | 1 (0.1) | 10 (0.7) | 39 (2.3) | 82 (3.2) |
|
| ||||
| 80,000–99,000 | 1 (0.1) | 1 (0.1) | 13 (0.8) | 22 (0.9) |
|
| ||||
| 60,000–79,000 | 0 | 1 (0.1) | 6 (0.4) | 16 (0.6) |
|
| ||||
| <60,000 | 2 (0.2) | 1 (0.1) | 1 (0.1) | 9 (0.3) |
|
| ||||
| Women with preexisting disorders associated with thrombocytopenia§ | ||||
|
| ||||
| ≥150,000 | 73 (85.8) | 95 (79.2) | 105 (75.0) | 158 (80.2) |
|
| ||||
| 125,000–149,000 | 5 (5.9) | 3 (2.5) | 10 (7.1) | 12 (6.1) |
|
| ||||
| 100,000–124,000 | 2 (2.4) | 10 (8.3) | 6 (4.3) | 12 (6.1) |
|
| ||||
| 80,000–99,000 | 2 (2.4) | 4 (3.3) | 8 (5.7) | 7 (3.6) |
|
| ||||
| 60,000–79,000 | 0 | 3 (2.5) | 5 (3.6) | 2 (1.0) |
|
| ||||
| <60,000 | 3 (3.5) | 5 (4.2) | 6 (4.3) | 6 (3.0) |
The lowest platelet count for each woman during each trimester and at the time of delivery was determined from a search of all platelet counts that were measured throughout the index pregnancy up to the time of delivery (Fig. S2 in the Supplementary Appendix). Percentages may not sum to 100 because of rounding.
A total of 4568 women had uncomplicated pregnancies and were included in our analyses. At the time of delivery, 450 women (9.9%) with uncomplicated pregnancies had platelet counts of less than 150,000 per cubic millimeter. A total of 12 women had a platelet count of less than 80,000 per cubic millimeter. The medical records of these 12 women, including all platelet counts before and after the index pregnancy, were reviewed in their entirety to search for a cause of the thrombocytopenia. In 5 women (0.1%), who had platelet counts between 62,000 and 78,000 per cubic millimeter (median, 65,000), no cause was apparent; therefore, the low platelet count was attributed to gestational thrombocytopenia. One of these 5 women had a platelet count of 62,000 per cubic millimeter in her third trimester and 68,000 per cubic millimeter at the time of delivery. Among the other 7 women who had platelet counts between 31,000 and 75,000 per cubic millimeter (median, 64,000) during pregnancy or at the time of delivery, causes other than gestational thrombocytopenia were identified. One of these 7 women had platelet counts of 72,000 per cubic millimeter and 74,000 per cubic millimeter in her third trimester and 64,000 per cubic millimeter and 72,000 per cubic millimeter at the time of delivery.
A total of 2586 women had pregnancy-related complications and were included in our analyses. At the time of delivery, 11.9% (307 women) with pregnancy-related complications had platelet counts of less than 150,000 per cubic millimeter, a percentage that was significantly greater than that among the women with uncomplicated pregnancies (P = 0.01). However, the percentages of women with pregnancy-related complications who had platelet counts below 150,000 per cubic millimeter in the first, second, and third trimesters did not differ significantly from the percentages among women with uncomplicated pregnancies (P = 0.67 for the first trimester comparison, P = 0.69 for the second trimester comparison, and P = 0.29 for the third trimester comparison). A total of 31 women (1.2%) had platelet counts below 80,000 per cubic millimeter during pregnancy, at the time of delivery, or both.
A total of 197 women had preexisting disorders associated with thrombocytopenia and were included in our analyses. The mean platelet counts in the women with preexisting disorders associated with thrombocytopenia were lower than those in the women with uncomplicated pregnancies at all trimesters and at the time of delivery: P = 0.03 for the first trimester comparison, P = 0.003 for the second trimester comparison, P = 0.004 for the third trimester comparison, and P = 0.01 for the comparison at the time of delivery. A total of 17 women (8.6%) had platelet counts below 80,000 per cubic millimeter during pregnancy, at the time of delivery, or both.
A total of 67 women had uncomplicated twin pregnancies and had at least one recorded platelet count during pregnancy; these women had lower platelet counts in all three trimesters and at the time of delivery than the women who had uncomplicated singleton pregnancies, but the difference at the time of delivery was not significant (P = 0.07) (Table 1, and Fig. S1C in the Supplementary Appendix). When all the women with uncomplicated singleton or twin pregnancies who had a platelet count at the time of delivery (8051 women with singleton pregnancies and 93 with twin pregnancies) were evaluated, the mean platelet count in the women with twin pregnancies (197,000 per cubic millimeter; 95% confidence interval [CI], 182,000 to 212,000) was significantly lower than the count in the women with singleton pregnancies (214,000 per cubic millimeter; 95% CI, 213,000 to 215,000) (P = 0.03) at the time of delivery.
Among the 4568 women with uncomplicated pregnancies whom we evaluated, 529 had a subsequent uncomplicated singleton pregnancy during our period of analysis and had a recorded platelet count at the time of delivery. A total of 57 (10.8%) had had a platelet count below 150,000 per cubic millimeter at the time of delivery in their initial pregnancy. Of these 57 women, 36 (63.2%) had a platelet count below 150,000 per cubic millimeter at the time of delivery in their subsequent pregnancy. Of the 472 women who did not have a platelet count below 150,000 per cubic millimeter in their initial pregnancy, only 21 (4.4%) had a platelet count below 150,000 per cubic millimeter at the time of delivery in their subsequent pregnancy. Therefore, the risk of a platelet count below 150,000 per cubic millimeter was 14.2 (95% CI, 8.9 to 22.6) times as high among women who had had a count below 150,000 per cubic millimeter in a previous pregnancy as among women who had not.
WOMEN WITH PREGNANCY-RELATED COMPLICATIONS
Among all 15,385 women who had singleton pregnancies, 4760 women had pregnancy-related complications. Of these women, 2586 (54.3%) had sufficient data for our analyses (Fig. 1, and Table S4A in the Supplementary Appendix). In 764 women (29.5%), multiple complications (two to four) occurred. The platelet counts in the women who had pregnancy-related complications decreased significantly throughout pregnancy (P<0.001). The interaction between the mean platelet count in the women with uncomplicated pregnancies and the mean platelet count in the women with pregnancy-related complications was significant (P = 0.002), which indicated that the rates of decrease in platelet counts differed. The rate of decrease in platelet counts was similar in the two groups until the third trimester, when the decrease occurred at a greater rate in the women with pregnancy-related complications than in the women with uncomplicated pregnancies (Fig. 2B). When we evaluated all 10,296 platelet count values measured during pregnancy and at the time of delivery in women with pregnancy-related complications (Fig. S2B in the Supplementary Appendix), we found that platelet counts of less than 150,000 per cubic millimeter occurred in 307 women (11.9%) women at the time of delivery, a percentage that was significantly greater than that in the women who had uncomplicated pregnancies (P = 0.01) (Table 2). A total of 59 women (2.3%) had platelet counts below 100,000 per cubic millimeter and 31 women had platelet counts below 80,000 per cubic millimeter during pregnancy, at the time of delivery, or both, which represented a higher incidence of low platelet counts than the incidence among women who had uncomplicated pregnancies (P<0.001). A total of 7 of the 25 women (28.0%) who had HELLP syndrome had a platelet count of less than 80,000 per cubic millimeter (median, 61,000; range, 32,000 to 78,000). Among the women who had one of the other five pregnancy-related complications, 0 to 3.6% had platelet counts of less than 80,000 per cubic millimeter (Table S4A in the Supplementary Appendix).
WOMEN WITH PREEXISTING DISORDERS ASSOCIATED WITH THROMBOCYTOPENIA
Among all 15,385 women who had singleton pregnancies, 338 women had preexisting disorders that were associated with thrombocytopenia. Of these women, 197 (58.3%) had sufficient data for our analyses (Fig. 1, and Table S4B in the Supplementary Appendix). The mean platelet counts in these women decreased significantly throughout pregnancy (P<0.001) and were lower in all three trimesters and at the time of delivery than the mean platelet counts in the women who had uncomplicated pregnancies (P<0.04 for all comparisons). The interaction between the mean platelet counts in the women with preexisting disorders and the mean platelet counts in the women with uncomplicated pregnancies was not significant (P=0.07), which indicated that the rates of decrease in platelet counts did not differ significantly (Fig. 2B). When we analyzed all 970 platelet count values measured during pregnancy, at the time of delivery, or both (Fig. S2C in the Supplementary Appendix), we found that platelet counts of less than 150,000 per cubic millimeter occurred in 39 women (19.8%) at the time of delivery (Table 2); 17 women (8.6%) had platelet counts of less than 80,000 per cubic millimeter (median, 48,000; range, 4000 to 77,000). Platelet counts below 80,000 per cubic millimeter occurred in 13 of the 24 women (54.2%) who had immune thrombocytopenic purpura. Among women who had one of the other three disorders, 1.4 to 6.0% had platelet counts below 80,000 per cubic millimeter (Table S4B in the Supplementary Appendix).
DISCUSSION
Although gestational thrombocytopenia has been recognized for more than 25 years,1 the course of platelet counts throughout pregnancy and the potential severity of gestational thrombocytopenia have not been defined.4,7–9 Our data showed that among the women who had uncomplicated pregnancies, the decline in platelet counts began in the first trimester and continued throughout pregnancy, with the nadir occurring at the time of delivery, when 9.9% of the women had platelet counts of less than 150,000 per cubic millimeter. At a mean of 7.1 weeks after delivery, platelet counts in the women who had uncomplicated pregnancies recovered to the level of platelet counts in the nonpregnant women. Assuming that platelet counts measured in the women during the postpartum period were similar to their platelet counts before pregnancy, mean platelet counts decreased by an estimated 17% during pregnancy.
The symmetric distribution of mean platelet counts seen in the nonpregnant women and also in the women with uncomplicated pregnancies in their first trimester and at the time of delivery suggests that the platelet counts of all women with uncomplicated pregnancies decrease at the same rate. The differences in the mean platelet count in the subgroups of women with uncomplicated pregnancies, which were defined according to race or ethnic group and age,14 were preserved throughout pregnancy, which also suggests that the platelet counts of all the women decreased at the same rate. Platelet counts in healthy women and men are genetically determined and exhibit little variation over time.15 Therefore, women whose platelet counts are at the low end of the normal range when they are not pregnant are more likely to have platelet counts that are below the normal range during pregnancy. This finding is consistent with the finding in our study that the risk of recurrent gestational thrombocytopenia was 14.2 times as high among women who had had previous gestational thrombocytopenia as among women who had not had previous gestational thrombocytopenia.
Multiple physiological changes during pregnancy may contribute to lower platelet counts. Dilution of platelets by the increased plasma volume that occurs during pregnancy16 is an apparent mechanism. In healthy, nonpregnant adult women, one third of all circulating platelets are transiently pooled within the low flow-rate circulation of the splenic sinusoids; an increased spleen size results in more pooling of the platelets and a lower platelet count.17 Therefore, the 50% increase in spleen size that occurs during pregnancy18 would also contribute to a lower platelet count. Because the placental circulation is similar to splenic circulation,19 platelets may also accumulate within the intervillous space of the placenta. The lower platelet counts observed in the women with twin pregnancies than in the women with singleton pregnancies could have been related to the larger placental size or the presence of two placentas, each of which is characteristic of twin pregnancies.20
Throughout pregnancy and at the time of delivery, platelet counts of less than 100,000 per cubic millimeter occurred in only 45 of the women (1.0%) who had uncomplicated pregnancies. Platelet counts of less than 80,000 per cubic millimeter for which an alternative cause was not identified occurred in only 5 women (0.1%), none of whom had a platelet count below 62,000 per cubic millimeter. An additional 7 women who had platelet counts of less than 80,000 per cubic millimeter had other causes for their thrombocytopenia. Platelet counts as low as 43,000 per cubic millimeter4,21 were reported previously in patients with gestational thrombocytopenia, but no information describing a search for an alternative cause was provided.21 Our data suggest that, for women with an uncomplicated pregnancy who have a platelet count of less than 100,000 per cubic millimeter, a cause of thrombocytopenia other than the pregnancy itself should be considered.
The mean platelet count decreased at a similar rate among women with pregnancy-related complications and those with uncomplicated pregnancies until the third trimester, when mean platelet counts decreased at a greater rate among women with pregnancy-related complications. At the time of delivery, 11.9% of the women with pregnancy-related complications had platelet counts of less than 150,000 per cubic millimeter, a percentage that was significantly greater than that in the women with uncomplicated pregnancies. A total of 59 women with pregnancy-related complications (2.3%) had platelet counts of less than 100,000 per cubic millimeter during pregnancy or at the time of delivery. The small difference between the percentage of women with complicated pregnancies who had a platelet count of less than 150,000 per cubic millimeter and the percentage of women with uncomplicated pregnancies who had a platelet count of less than 150,000 per cubic millimeter may be related to our criteria for pregnancy-related complications. We included women who had minor complications (e.g., hypertension or diabetes) who would not have been expected to have thrombocytopenia, because our primary aim in the designation of women with uncomplicated pregnancies was to avoid the inclusion of women who had any complications. We excluded women who did not have platelet count measurements during pregnancy and women who reported illicit-drug use; these women may have had minimal or no prenatal care and may have been at greater risk for complications. However, the frequencies of the pregnancy-related complications among these women were similar to U.S. population estimates.22–29 Therefore, our data may accurately reflect the platelet counts in women with these pregnancy-related complications.
Platelet counts in all women decrease throughout pregnancy, beginning in the first trimester. Severe thrombocytopenia is rare, even in women with pregnancy-related complications. In women with platelet counts below 100,000 per cubic millimeter who do not have preeclampsia or a preexisting disorder associated with thrombocytopenia, a cause other than pregnancy or its complications should be considered.
Supplementary Material
Acknowledgments
Supported in part by a grant (1K01HL135466-01) from the National Heart, Lung, and Blood Institute.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993;329:1463–6. doi: 10.1056/NEJM199311113292005. [DOI] [PubMed] [Google Scholar]
- 2.Boehlen F, Hohlfeld P, Extermann P, Perneger TV, de Moerloose P. Platelet count at term pregnancy: a reappraisal of the threshold. Obstet Gynecol. 2000;95:29–33. doi: 10.1016/s0029-7844(99)00537-2. [DOI] [PubMed] [Google Scholar]
- 3.Sainio S, Kekomäki R, Riikonen S, Teramo K. Maternal thrombocytopenia at term: a population-based study. Acta Obstet Gynecol Scand. 2000;79:744–9. [PubMed] [Google Scholar]
- 4.Practice bulletin no. 166: thrombocytopenia in pregnancy. Obstet Gynecol. 2016;128(3):e43–e53. doi: 10.1097/AOG.0000000000001641. [DOI] [PubMed] [Google Scholar]
- 5.Burrows RF, Kelton JG. Incidentally detected thrombocytopenia in healthy mothers and their infants. N Engl J Med. 1988;319:142–5. doi: 10.1056/NEJM198807213190304. [DOI] [PubMed] [Google Scholar]
- 6.Burrows RF, Kelton JG. Platelets and pregnancy. Curr Obstet Med. 1993;2:83–106. [Google Scholar]
- 7.Reese JA, Peck JD, McIntosh JJ, Vesely SK, George JN. Platelet counts in women with normal pregnancies: a systematic review. Am J Hematol. 2017;92:1224–32. doi: 10.1002/ajh.24829. [DOI] [PubMed] [Google Scholar]
- 8.Gernsheimer T, James AH, Stasi R. How I treat thrombocytopenia in pregnancy. Blood. 2013;121:38–47. doi: 10.1182/blood-2012-08-448944. [DOI] [PubMed] [Google Scholar]
- 9.Cines DB, Levine LD. Thrombocytopenia in pregnancy. Blood. 2017;130:2271–7. doi: 10.1182/blood-2017-05-781971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hypertension in pregnancy: report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–31. doi: 10.1097/01.AOG.0000437382.03963.88. [DOI] [PubMed] [Google Scholar]
- 11.Loustau V, Debouverie O, Canoui-Poitrine F, et al. Effect of pregnancy on the course of immune thrombocytopenia: a retrospective study of 118 pregnancies in 82 women. Br J Haematol. 2014;166:929–35. doi: 10.1111/bjh.12976. [DOI] [PubMed] [Google Scholar]
- 12.Curtin LR, Mohadjer LK, Dohrmann SM, et al. The National Health and Nutrition Examination Survey: sample design, 1999–2006. Vital Health Stat 2. 2012;155:1–39. [PubMed] [Google Scholar]
- 13.Curtin LR, Mohadjer LK, Dohrmann SM, et al. National Health and Nutrition Examination Survey: sample design, 2007–2010. Vital Health Stat 2. 2013;160:1–23. [PubMed] [Google Scholar]
- 14.Segal JB, Moliterno AR. Platelet counts differ by sex, ethnicity, and age in the United States. Ann Epidemiol. 2006;16:123–30. doi: 10.1016/j.annepidem.2005.06.052. [DOI] [PubMed] [Google Scholar]
- 15.Buckley MF, James JW, Brown DE, et al. A novel approach to the assessment of variations in the human platelet count. Thromb Haemost. 2000;83:480–4. [PubMed] [Google Scholar]
- 16.Abduljalil K, Furness P, Johnson TN, Rostami-Hodjegan A, Soltani H. Anatomical, physiological and metabolic changes with gestational age during normal pregnancy: a database for parameters required in physiologically based pharmacokinetic modelling. Clin Pharmacokinet. 2012;51:365–96. doi: 10.2165/11597440-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 17.Aster RH. Pooling of platelets in the spleen: role in the pathogenesis of “hypersplenic” thrombocytopenia. J Clin Invest. 1966;45:645–57. doi: 10.1172/JCI105380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maymon R, Strauss S, Vaknin Z, Weinraub Z, Herman A, Gayer G. Normal sonographic values of maternal spleen size throughout pregnancy. Ultrasound Med Biol. 2006;32:1827–31. doi: 10.1016/j.ultrasmedbio.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Jønsson V, Bock JE, Nielsen JB. Significance of plasma skimming and plasma volume expansion. J Appl Physiol (1985) 1992;72:2047–51. doi: 10.1152/jappl.1992.72.6.2047. [DOI] [PubMed] [Google Scholar]
- 20.Almog B, Shehata F, Aljabri S, Levin I, Shalom-Paz E, Shrim A. Placenta weight percentile curves for singleton and twins deliveries. Placenta. 2011;32:58–62. doi: 10.1016/j.placenta.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Burrows RF, Kelton JG. Thrombocytopenia at delivery: a prospective survey of 6715 deliveries. Am J Obstet Gynecol. 1990;162:731–4. doi: 10.1016/0002-9378(90)90996-k. [DOI] [PubMed] [Google Scholar]
- 22.Mogos MF, Salemi JL, Spooner KK, McFarlin BL, Salihu HH. Hypertensive disorders of pregnancy and postpartum readmission in the United States: national surveillance of the revolving door. J Hypertens. 2018;36:608–18. doi: 10.1097/HJH.0000000000001594. [DOI] [PubMed] [Google Scholar]
- 23.Haram K, Svendsen E, Abildgaard U. The HELLP syndrome: clinical issues and management: a review. BMC Pregnancy Childbirth. 2009;9:8–23. doi: 10.1186/1471-2393-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.ACOG practice bulletin no. 190: gestational diabetes mellitus. Obstet Gynecol. 2018;131(2):e49–e64. doi: 10.1097/AOG.0000000000002501. [DOI] [PubMed] [Google Scholar]
- 25.P ractice bulletin no. 171: management of preterm labor. Obstet Gynecol. 2016;128(4):e155–e164. doi: 10.1097/AOG.0000000000001711. [DOI] [PubMed] [Google Scholar]
- 26.A COG practice bulletin no. 102: management of stillbirth. Obstet Gynecol. 2009;113:748–61. doi: 10.1097/AOG.0b013e31819e9ee2. [DOI] [PubMed] [Google Scholar]
- 27.Ananth CV, Oyelese Y, Yeo L, Pradhan A, Vintzileos AM. Placental abruption in the United States, 1979 through 2001: temporal trends and potential determinants. Am J Obstet Gynecol. 2005;192:191–8. doi: 10.1016/j.ajog.2004.05.087. [DOI] [PubMed] [Google Scholar]
- 28.Frederiksen MC, Glassenberg R, Stika CS. Placenta previa: a 22-year analysis. Am J Obstet Gynecol. 1999;180:1432–7. doi: 10.1016/s0002-9378(99)70031-1. [DOI] [PubMed] [Google Scholar]
- 29.P ublications Committee, Society for Maternal-Fetal Medicine. Belfort MA. Placenta accreta. Am J Obstet Gynecol. 2010;203:430–9. doi: 10.1016/j.ajog.2010.09.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.