Abstract
Traumatic brain injury (TBI) is a significant cause of morbidity in military Veterans and Service Members. While most individuals recover fully from mild injuries within weeks, some continue to experience symptoms including headaches, disrupted sleep, and other cognitive, behavioral or physical symptoms. Diffusion magnetic resonance imaging (dMRI) shows promise in identifying areas of structural disruption and predicting outcomes. Although some studies suggest widespread structural disruption after brain injury, dMRI studies of military brain injury have yielded mixed results so far, perhaps due to the subtlety of mild injury, individual differences in injury location, severity and mechanism, and comorbidity with other disorders such as post-traumatic stress disorder (PTSD), depression, and substance abuse. We present preliminary dMRI results from the ENIGMA (Enhancing Neuroimaging Genetics through Meta-Analysis) military brain injury working group. We found higher fractional anisotropy (FA) in participants with a history of TBI. Understanding the injury and recovery process, along with factors that influence these, will lead to improved diagnosis and treatment.
Keywords: traumatic brain injury, military, diffusion MRI, blast, ENIGMA
1. INTRODUCTION
Traumatic brain injury (TBI) is one of the most common injuries affecting members of the United States military, and armed services members across the world. For years, TBI was underestimated and considered an “invisible injury” – but it is now recognized as a major source of morbidity in Veterans and Active Duty Service Members (ADSM). Most military injuries are classified as “mild”, but injuries can affect combat readiness in the immediate post-injury phase, and can also lead to long-term cognitive impairments and adverse health consequences.
Mild injuries can be difficult to identify, because the effects on the brain can be subtle, and they also vary across individuals. Diffusion MRI (dMRI) has emerged as a more sensitive type of brain imaging than other traditional modalities in the TBI field, and as such has recently been applied to study brain injury. There have been only a few studies using dMRI in military brain injury, and those that have been conducted have found mixed results. One study reported lower fractional anisotropy (FA; a marker of tissue microstructure that depends on myelin organization) after TBI in the cerebral peduncles, cingulate, and orbitofrontal cortex [1]. Other dMRI-derived measures include MD (mean diffusivity) and RD (radial diffusivity), elevations in which can suggest demyelination, and AD (axial diffusivity), which can indicate axonal injury if decreased. Importantly, these abnormalities persist for at least a year post-injury, and in some cases several years [2]. Other studies reported no significant differences in service members who had sustained a brain injury [3-5].
In deployment-related TBI, there is the added question of blast-related vs. impact injury, and how these two types of injury compare. The blast waves created by explosive devices that have become increasingly common in modern military conflicts can cause diffuse damage throughout the brain. The mechanics of blast-related injury differ from those of impact injury and as such, may result in a different recovery profile [6]. Importantly, blast-related injury most often occurs in the context of concomitant blunt injury in combat situations. How blast-related and impact injuries differ is not well understood, but clarifying this will be an essential step in developing more effective treatments.
Given the small effect sizes and heterogeneity in imaging measures in chronic mild TBI, larger sample sizes are necessary to reliably identify common disruptions post-injury. The ENIGMA consortium (Enhancing Neuroimaging Genetics through Meta-Analysis; http://enigma.ini.usc.edu) has recently published the largest collection of neuroimaging studies to date of schizophrenia, major depressive disorder, bipolar disorder, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), among 18 disorders in total, using harmonized protocols and metaanalysis to assess their effects on the brain [7]. The data in these studies come from separately collected samples that were then processed and analyzed in a harmonized manner, and meta-analyzed. We recently started an ENIGMA brain injury group, with a sub-group dedicated to military brain injury. Our goal is to identify imaging biomarkers of brain injury and recovery, and to understand factors that affect these processes. We hope our results will help develop more targeted treatments and to reduce the morbidity of TBI.
2. METHODS
2.1. Subjects and Image Acquisition
Participants were scanned and assessed via 5 different projects, for a total of 437 participants who reported history of at least one event consistent with TBI or concussion (TBI group) and 268 comparison participants who have never been diagnosed with TBI. Individual scan parameters can be found on the ENIMGA Military Brain Injury website (http://enigma.ini.usc.edu/enigma-tbi/). All cohorts included participants who were either United States Veterans or ADSM. One study included Vietnam-era Veterans, and the other four included Veterans or ADSM of the American military operations in Iraq or Afghanistan (Operation Iraqi Freedom/Operation Enduring Freedom/Operation New Dawn). The study of Vietnam Veterans included those with a history of moderate-severe TBI, while those of OIF/OEF/OND Veterans and ADSM included only mild TBI. This study included participants from the “Department of Defense (DoD) Alzheimer’s Disease Neuroimaging Initiative” (ADNI; Brain Aging in Vietnam War Veterans), “Chronic Effects of Neurotrauma Consortium” (CENC), “A Longitudinal Study of Chronic TBI in OEF/OIF/OND Veterans and Service Members” (CETBI), “Imaging Support of Study of Cognitive Rehabilitation Effectiveness in Mild Traumatic Brain Injury” (iSCORE), and the “Mid-Atlantic MIRECC Sample” projects. Demographics for each project can be seen in Table 1. All sites processed dMRI brain scans locally with a standard protocol based on TBSS (tract-based spatial statistics) in Freesurfer 5.0 or later [8] (http://enigma.usc.edu). FA, MD, RD, and AD were calculated and FA images were used to register data to the ENIGMA-DTI FA template [9]. Each subject’s FA values were then projected onto the ENIGMA-DTI FA skeleton; corresponding voxels from diffusion scans were also extracted. Measures were averaged across the entire skeleton, and within each of 5 midline, and 19 bilaterally averaged white matter (WM) regions of interest (ROIs) from the Johns Hopkins University (JHU) atlas, some of which partially overlap. Preprocessing included automated and visual quality control of the data, and exclusion of outliers. An overview of the method can be seen in Figure 1.
Table 1.
Demographics of sites included in meta-analysis.
M/F=male/female ratio, age column lists average (range).
| Site | N TBI | N controls | M/F | Age |
|---|---|---|---|---|
| DoD ADNI | 64 | 71 | 134/1 | 69.3 (61.4-83.2) |
| CENC | 209 | 44 | 213/40 | 39.8 (22-69) |
| CETBI | 65 | 16 | 73/8 | 34.7 (23.1-53.9) |
| ISCORE | 31 | 71 | 89/13 | 35.9 (19-51) |
| Duke | 68 | 66 | 109/25 | 39.6 (23-67) |
Figure 1.
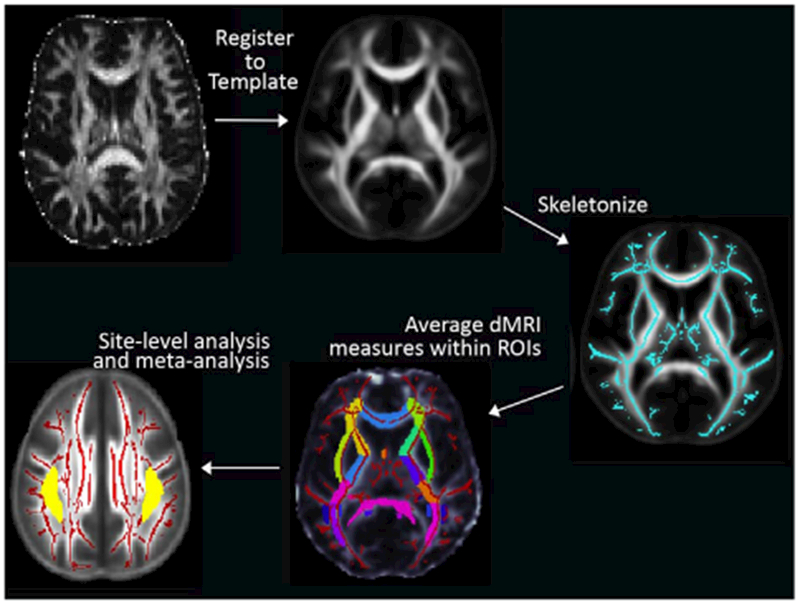
ENIGMA dMRI processing and meta-analysis. Regions with significant differences are shown in the bottom left in yellow.
2.2. Statistics
TBI/control effect sizes were calculated within each site, and statistical results were pooled across sites to conduct a meta-analysis on the individual regression parameters, testing for group differences in the 4 dMRI measures averaged within each of the WM ROIs. Our primary model included age, sex, and educational level.
We also conducted exploratory analyses on the question of blast-related vs. impact TBI in sites that had that information available. Our primary analyses were conducted on FA measures, with MD, RD, and AD serving as post hoc tests. Results were corrected for multiple comparisons using a Bonferroni correction (p<0.05/25 = 0.002).
3. RESULTS
3.1. TBI vs. control
In the TBI vs. control comparisons, we found significant differences in just one ROI after correction for multiple comparisons:higher FA in the superior longitudinal fasciculus (SLF p=0.0013). The external capsule (EC) and posterior thalamic radiation (PTR) showed borderline effects. The effect sizes and 95% confidence intervals across ROIs can be seen in Figure 2. We found borderline differences (0.05>p>0.002) in MD and RD in the PTR, internal capsule, and sagittal striatum. The effect sizes for each site for the SLF result can be seen in Figure 3.
Figure 2.
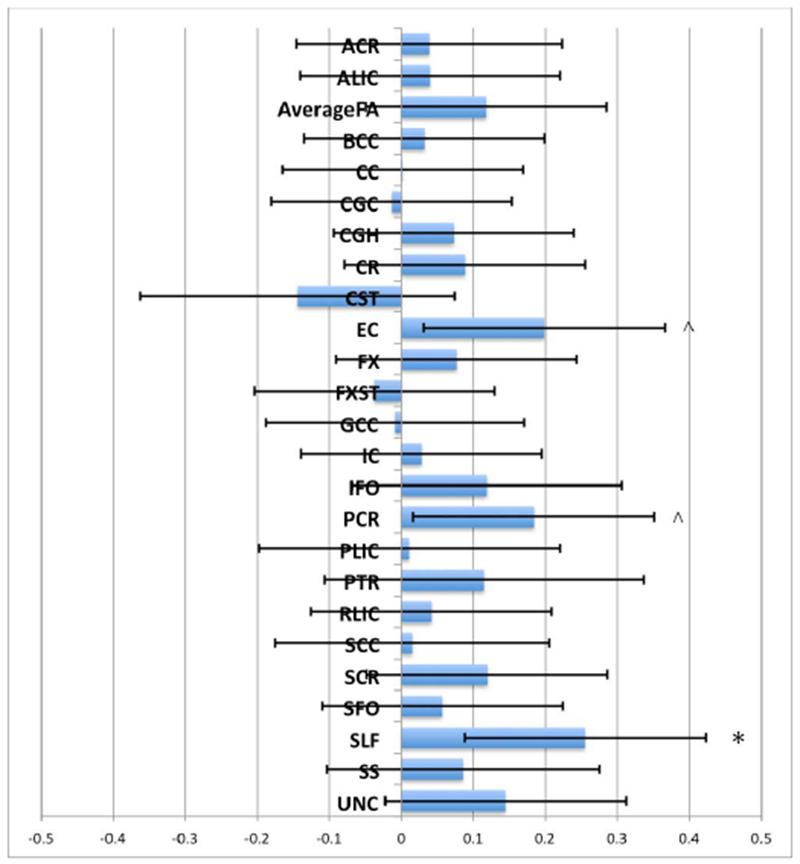
Effect sizes (Cohen’s d) for the case vs. control meta-analysis in all sites across ROIs. Bars show 95% CI.
Figure 3.
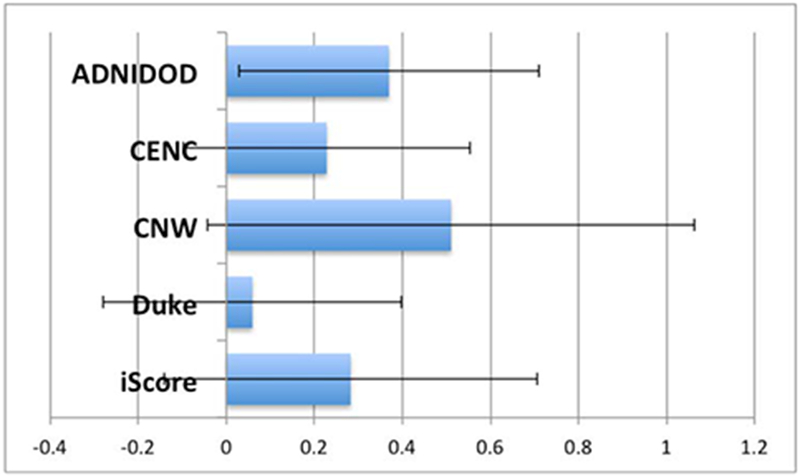
Effect sizes (Cohen’s d) for each site for the SLF result from the meta-analysis.
3.2. Blast-related vs. impact TBI
One project (CENC) had information on blast-related vs. impact TBI, with a total of 106 participants with blast-related TBI and 103 with impact TBI. This analysis was considered exploratory, as the use of this data was restricted to a single project in these preliminary analyses. We found borderline differences in the internal capsule, posterior thalamic radiation, fornix, corona radiata, and superior fronto-occipital fasciculus. We found borderline differences in FA and RD, with generally higher FA and lower RD in blast-related injury, with the exception of the fornix. These results can be seen in Figure 4.
Figure 4.
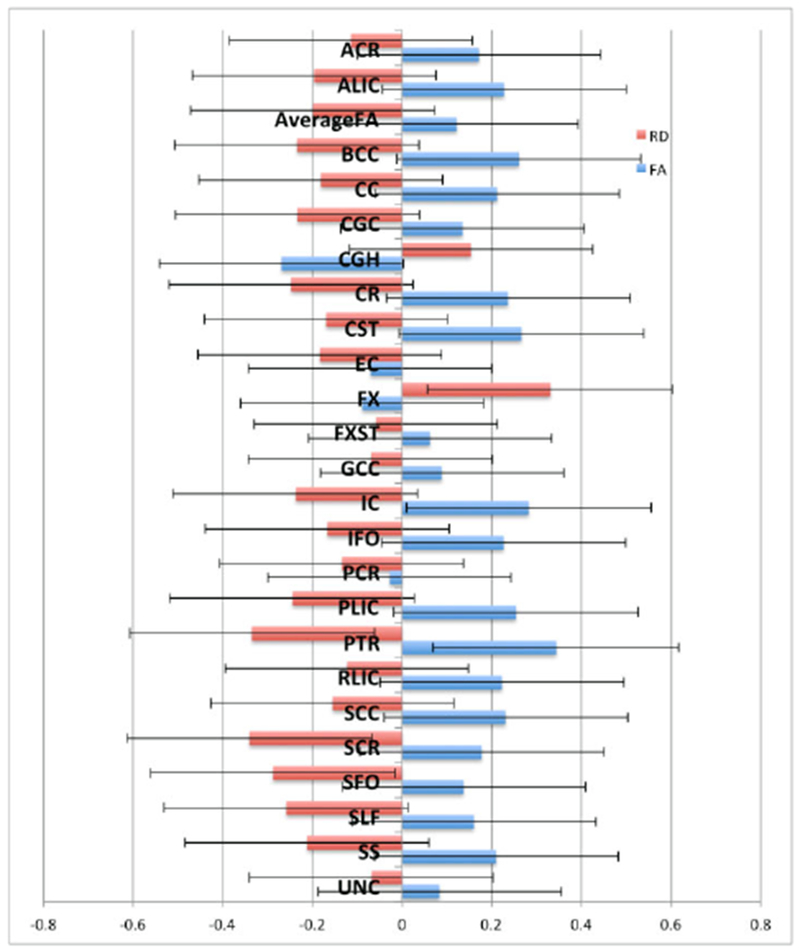
Effect sizes (Cohen’s d) for the blast vs. impact analysis in the CENC site across ROIs. Bars show 95% CI. Blue bars indicate FA effect sizes, red bars indicate RD effect sizes.
4. DISCUSSION
Here we present preliminary analyses from the ENIGMA Military Brain Injury working group on dMRI markers of traumatic brain injury. We completed a hybrid meta-analysis/multi-site study, in that data collection was planned and executed separately, but harmonized processing and analysis was used. Traditional meta-analyses do not include harmonization of data processing and analysis. While truly harmonized data collection across sites would certainly yield a more streamlined studied, using harmonized processing and analysis marks an improvement over traditional meta-analytic approaches. As to the issue of meta- vs. mega-analysis, prior studies from other ENIGMA working groups have found minimal differences in results from these two approaches [10]. We found significantly higher FA in the TBI group in the SLF, which was more pronounced on the right. Several other ROIs showed borderline effects in the same direction. Some studies of sports concussion have shown higher FA in the immediate post-injury period, which is often attributed to cytotoxic edema [11]. However, higher FA in concussed individuals can also be seen months post-injury [12, 13], when edema is less likely to be an issue – edema typically resolves within around 10 days and is more often seen in moderate-to-severe injuries. Another possibility is that higher FA after a mild injury is a marker of recovery. Some animal studies show that FA is higher in areas of fiber reorganization and remyelination [14, 15]. It could be that in moderate-severe injury, where we see lower FA, more macroscopic damage dominates dMRI measures, but in mild injury, in the absence of macroscopic damage, subtle indications of recovery may be detected. Finally, it is possible that elevated FA may represent a pathologic finding associated with gliosis or other deleterious alteration in tissue structure.
The finding of significantly higher FA in the SLF in the TBI group was consistent across 4 of 5 sites, although appeared to be driven primarily by the DoD ADNI cohort. This cohort is significantly older than the other four, included more severe injuries and the interval between injury and imaging was much longer (~40 years as opposed to months to several years), all of which could explain our finding more prominent differences in this cohort. Three of the four other cohorts also showed trends in the same direction however, which could suggest a dosing effect. Excluding DoD ADNI from meta-analyses, results were only borderline significant (left/right average p=0.026, right SLF p=0.016). Prior studies have shown altered dMRI measures in the SLF following TBI [16].
Within military brain injury, blast-related and impact injuries form two sub-categories, with different mechanics and potentially different injury and recovery profiles, though concomitant injury is common. We found some trend-level results that did not pass correction for multiple comparisons, but suggested that blast-related injury might be generally associated with higher FA than impact injury in some regions. These data came only from one cohort, though, so should be considered exploratory.
5. CONCLUSION
Here we present preliminary results from the newly formed ENIGMA Military Brain Injury working group. We found higher FA in the TBI group in our metaanalysis of 5 sites; this may indicate ongoing recovery processes. As a cross-sectional analysis however, we are not powered to examine recovery specifically. We also found trends towards higher FA in blast-related vs. impact TBI. ENIGMA Military Brain Injury will continue to add cohorts, which will give us more confidence in the reliability of our results. Identifying imaging biomarkers of brain injury in the military will help us better understand injury and recovery processes, and ultimately may assist in the assessment of more effective treatments.
ACKNOWLEDGMENTS
Any opinions, findings, conclusions or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the views of the U.S. Government, the U.S. Department of Veterans Affairs, or the U.S. Department of Defense, and no official endorsement should be inferred. For a complete list of funding and acknowledgements, please see the ENIGMA Brain Injury website (http://enigma.ini.usc.edu/enigma-tbi/).
6. REFERENCES
- 1.Mac Donald CL, et al. : ‘Detection of blast-related traumatic brain injury in U.S. military personnel’, The New England journal of medicine, 2011, 364, (22), pp. 2091–2100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mac Donald C, et al. : ‘Cerebellar white matter abnormalities following primary blast injury in US military personnel’, PloS one, 2013, 8, (2), pp. e55823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davenport ND, et al. : ‘Diffuse and spatially variable white matter disruptions are associated with blast-related mild traumatic brain injury’, NeuroImage, 2012, 59, (3), pp. 2017–2024 [DOI] [PubMed] [Google Scholar]
- 4.Jorge RE, et al. : ‘White matter abnormalities in veterans with mild traumatic brain injury’, The American journal of psychiatry, 2012, 169, (12), pp. 1284–1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levin HS, et al. : ‘Diffusion tensor imaging of mild to moderate blast-related traumatic brain injury and its sequelae’, Journal of neurotrauma, 2010, 27, (4), pp. 683–694 [DOI] [PubMed] [Google Scholar]
- 6.Magnuson J, et al. : ‘Neuropathology of explosive blast traumatic brain injury’, Current neurology and neuroscience reports, 2012, 12, (5), pp. 570–579 [DOI] [PubMed] [Google Scholar]
- 7.Thompson PM, et al. : ‘ENIGMA and the individual: predicting factors that affect the brain in 35 countries worldwide’, NeuroImage, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith SM, et al. : ‘Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data’, NeuroImage, 2006, 31, (4), pp. 1487–1505 [DOI] [PubMed] [Google Scholar]
- 9.Kelly S, et al. : ‘White matter microstructural differences in 4,072 individuals with schizophrenia versus controls from 28 cohorts worldwide in the ENIGMA Schizophrenia DTI Working Group’, Molecular psychiatry, 2017, In Press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boedhoe PS, et al. : ‘Distinct Subcortical Volume Alterations in Pediatric and Adult OCD: A Worldwide Meta- and Mega-Analysis’, The American journal of psychiatry, 2017, 174 (1). pp. 60–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chu Z, et al. : ‘Voxel-Based Analysis of Diffusion Tensor Imaging in Mild Traumatic Brain Injury in Adolescents’, AJNR. American journal of neuroradiology, 2010, 31, (2), pp. 340–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borich M, et al. : ‘Combining whole-brain voxel-wise analysis with in vivo tractography of diffusion behavior after sports-related concussion in adolescents: a preliminary report’, Journal of neurotrauma, 2013, 30, (14), pp. 1243–1249 [DOI] [PubMed] [Google Scholar]
- 13.Mayer AR, et al. : ‘Diffusion abnormalities in pediatric mild traumatic brain injury’, Journal of Neuroscience, 2012, 32, (50), pp. 17961–17969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jiang Q, et al. : ‘MRI evaluation of white matter recovery after brain injury’, Stroke, 2010, 41, (10 Suppl), pp. S112–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Zijden JP, et al. : ‘Longitudinal in vivo MRI of alterations in perilesional tissue after transient ischemic stroke in rats’, Experimental neurology, 2008, 212, (1), pp. 207–212 [DOI] [PubMed] [Google Scholar]
- 16.Hulkower MB, et al. : ‘A Decade of DTI in Traumatic Brain Injury: 10 Years and 100 Articles Later’, AJNR. American journal of neuroradiology, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]


