Abstract
Background
There is increased focus among policymakers on improving value for heart failure (HF) care, given its rising prevalence and associated financial burden in the United States. However, little is known about the relationship between payments and mortality for a 30-day episode of HF care.
Objectives
To examine the association of 30-day payments for an episode of HF care with patient outcomes.
Methods
Using Medicare claims data for all fee-for-service beneficiaries hospitalized for HF between July 1st, 2011 and June 30th, 2014, we examined the association between 30-day Medicare payments – beginning with a hospital admission for HF and across multiple settings following discharge -and patient 30-day mortality using mixed-effect logistic regression models.
Results
We included 1,343,792 patients hospitalized for HF across 2,948 hospitals. Mean 30-day Medicare payments per beneficiary were $15,423 (standard deviation, $1,523). Overall observed mortality in the cohort was 11.3%. Higher 30-day payments were associated with lower 30-day mortality after adjustment for patient characteristics (OR per $1,000 increase in payments, 0.961; 95% CI 0.954–0.967). This relationship was slightly attenuated after accounting for hospital characteristics and HF volume, but remained significant (OR per $1,000 increase, 0.968; 95% CI, 0.962–0.975). Additional adjustment for potential mediating factors, including cardiac service capability and post-acute service use, did not significantly affect the relationship.
Conclusions
Higher 30-day episode payments were associated with lower 30-day mortality following a hospitalization for HF. This has implications for policies that incentivize reduction in payments without considering value. Further investigation is needed to understand the mechanisms that underlie this relationship.
Introduction
There is increased focus among policymakers on improving value for heart failure (HF) care, given the high and rising prevalence of HF and its associated financial burden in the United States (1). HF is the most common cause of hospitalization among Medicare beneficiaries and accounts for a large portion of total Medicare expenditures (2,3). However, mortality rates remain high, and improvements have slowed in recent years (4). To incent ongoing progress in both costs and outcomes of care, the Centers for Medicare and Medicaid Services (CMS), through the mandatory Hospital Value-based Purchasing (HVBP) program, financially rewards or penalizes hospitals based on performance on both mortality and payment measures for HF, as well as other common conditions (5).
As value-based and alternative payment models increasingly spur hospitals to both reduce costs and improve outcomes for HF, it is important to understand how payments for an episode of HF care are related to clinical outcomes. Prior studies have demonstrated significant variation in payments associated with HF hospitalizations in the US (6–8). However, little is known about whether higher payments are associated with better outcomes, which would at least potentially indicate high value, or whether higher payments are associated with worse outcomes, which would indicate poor value. The relationship is unclear, in part, because little is known about how higher payments might translate into actual care delivery. Higher payments may reflect the overuse of low-value resources or utilization of unnecessary post-acute care, which would not have a positive effect on outcomes. Alternatively, high payments may be driven by the use of resources and services that actually improve quality of care and survival. Given that for hospitals participating in HVBP, episode payment metrics together with 30-day mortality metrics account for one-half of a total score used by CMS to evaluate performance (and determine financial rewards or penalties), understanding the relationship between these measures for an episode of HF care is increasingly important and policy-relevant (5).
Therefore, in this study, we aimed to answer several questions. First, how do hospitals whose HF patients incur high 30-day Medicare episode payments, reflecting both hospital-based and outpatient care in the immediate post-discharge time frame, differ from those with low episode payments? Second, are higher 30-day episode payments for HF care, beginning with a hospital admission for HF and across multiple care settings following discharge, associated with lower mortality rates? And if so, to what extent do differences in hospital characteristics, cardiac service capability, and post-acute service use explain the association?
Methods
Patient Cohort
Eligible patients were fee-for-service Medicare beneficiaries over the age of 65 hospitalized at an acute-care hospital for HF based on principal discharge diagnosis codes from the International Classification of Diseases, Ninth Revision from July 1st, 2011 through June 30th, 2014. Patient characteristics included age, sex, and comorbidities that were defined based on a validated administrative claims model used to profile hospital 30-day mortality measures for HF (9). We applied inclusion criteria previously used by CMS for HF mortality rate measures. For patients with more than one HF admission across the three-year period, only one randomly selected episode of care was included (7,9,10).
Thirty-Day Episode Payments for Heart Failure
Hospital-level risk-standardized payments for a 30-day episode of HF care (which from here on, will be referred to as episode payments) - a measure made publicly available by CMS on Hospital Compare - were used to characterize payments across a 30-day period beginning with a hospital admission for HF (7,8). Episode payments reflect variations in hospital practice patterns and resource utilization related to HF care and are calculated by summing total payments associated with a 30-day episode of HF care for each beneficiary, beginning with index admission and across multiple care settings, services, and supplies (i.e. inpatient, outpatient, skilled nursing facility, home health, physician/clinical laboratory/ambulance services, durable medical equipment). In addition to inpatient payments, post-acute payments are attributed to the hospital of index HF admission because care and discharge planning during a hospitalization influences subsequent expenditures across care settings. Geographic differences and policy adjustments (i.e. for costs of living, graduate medical education, and disproportionate share hospitals) in Medicare payment rates are accounted for. Additionally, episode payments are risk-adjusted for differences in patient characteristics and hospital case mix, and account for clustering of patients within hospitals. For patients transferred from one acute care hospital to another, total payments across 30 days are attributed to the first hospital where the patient was admitted (7). Hospitals in the Inpatient Prospective Payment System with too few HF cases (<25) were not included in the analysis. Hospital payment performance is assessed over a rolling three-year period; here, we used performance data representing July 1st, 2011 through June 30th, 2014, which were used in the HVBP program in fiscal year 2016 (7).
We used episode payments because they represent healthcare expenditures from a payer’s (Medicare’s) perspective, and reflect a hospital’s style of practice in terms of the level of utilization of resources and services by their HF patients – for example, some hospitals may tend to discharge more HF patients to institutional post-acute care than others, or to provide more post-discharge follow-up care. We focused on a thirty-day episode of HF care because CMS payment measures through HVBP do so, making this the most policy-relevant approach to assessing value. Episode payments were assessed on a hospital rather than patient level to examine the impact of a patient population being exposed to varying styles of care rather than an individual patient being exposed to more intense care, and to diminish the likelihood of patient-level confounding (11).
Hospital Characteristics
Hospital characteristics were obtained from the 2013 American Hospital Association annual survey, and included hospital size, census region, Joint Commission certification status, location (urban or rural), ownership (for-profit, private not-for profit, and public), teaching status (large teaching versus others), nurse-to-patient ratio, and cardiac service capability (percutaneous coronary intervention and coronary artery bypass graft surgery). Additionally, using Medicare inpatient data, we calculated fee-for-service HF volume as well as the proportion of HF patients discharged to a skilled nursing facility or with homecare services for each hospital.
Outcomes
The primary outcome was patient-level 30-day mortality, defined as all-cause deaths within 30 days of the date of admission.
Statistical Analysis
We classified 30-day HF episode payments into low- (<25th percentile), average- (25th–75th percentile), and high-spending (>75th percentile) for descriptive purposes, similar to prior studies (12–16). Bivariate analyses were performed to compare patient and hospital characteristics across episode payment categories, using the Mantel-Haenszel χ2 test for categorical variables and the Kruskal-Wallis test for continuous variables. To demonstrate geographic variability, we also mapped county-specific episode payments for HF care.
To evaluate the association between 30-day episode payments and 30-day patient-level mortality, we fit a mixed model with a logit link function and random hospital intercepts to model mortality as a function of 30-day HF episode payments ($1,000). We fit the model in the following sequence: 1) unadjusted 2) risk-adjusted for patient characteristics and comorbidities used by CMS to profile hospital 30-day mortality measures for HF (9), and 3) additionally adjusted for key hospital characteristics (ownership, major teaching hospital, urban vs. rural hospital, region, and nurse staffing) as well as HF volume. This allowed us to control for individual risk factors and institutional characteristics and make inferences at the patient level regarding the association of being exposed to different levels of 30-day payments for HF care and outcomes. Next, we explored potential mediating variables related to hospital payment including cardiac service capability and mean proportion of HF patients discharged to skilled nursing facility (SNF) or with homecare services.
We performed several additional analyses. First, we examined the relationship between CMS inpatient payments and patient mortality, to determine if this relationship paralleled our primary analysis. Second, we performed quantile regression to assess the nature of the relationship between episode payments and outcomes (17). This allowed us to understand whether the association between episode payments and patient risk of mortality differed across quantiles of mortality. Third, we conducted an iterative non-parametric bootstrapping analysis with a replacement that randomly selected hospitals from the CMS episode payment dataset with a sample size equal to total hospitals in the dataset. We then re-fit the mixed models described above. We repeated this process 1,000 times to obtain the distribution of odds ratios for the association between payments and outcomes. Finally, we also evaluated the relationship between 30-day episode payments and one year mortality following the index hospitalization.
Statistical tests were 2-sided at a significance level of 0.05. Analyses were performed using SAS version 9.4 64-bit (SAS Institute Inc., Cary, North Carolina).
Results
Study Population
Our study sample included 1,343,792 HF patients hospitalized from July 1st, 2011 through June 30th, 2014 across 2,948 hospitals with ≥ 25 eligible HF cases and episode payment information. Patient demographics were generally similar across low, average, and high episode payment hospital groups (eTable 1). Comorbidities, including the proportion of patients with a history of HF, coronary artery disease, prior myocardial infarction, stroke, and hypertension, were also similar across groups.
Thirty-day Payments
Thirty-day episode payments for HF care varied nearly two-fold across hospitals (10). Mean 30-day episode payments were $15,423, with a standard deviation of $1,523 (eFigure 1). Median 30-day episode payments per beneficiary were $13,732 in the low-payment group, $15,308 in the average-payment group, and $17,207 in the high-payment group (Table 1). There was evidence of geographic variation in 30-day episode payments for HF care across the United States (Figure 1)
Table 1.
Hospital Characteristics by 30-Day Episode Payment Categories
| Low (n=735) | Average (n=1476) | High (n=737) | P value | |
|---|---|---|---|---|
| 30-day HF spending, median $ (IQR) | 13,732 (13,268–14,019) | 15,308 (14,841–15,809) | 17,207 (16,713–17,853) | |
| Hospital size, median beds (IQR) | 95 (50–165) | 182 (99–310) | 260 (165–406) | <0.001 |
| Ownership, No. (%)a | 0.05 | |||
| For profit | 139 (19.0) | 261 (17.8) | 198 (26.9) | |
| Private nonprofit | 409 (56.0) | 1012 (68.9) | 490 (66.6) | |
| Public | 179 (24.5) | 195 (13.3) | 48 (6.5) | |
| Large teaching hospital, No. (%) | 22 (3.0) | 118 (8.0) | 103 (14.0) | 0.005 |
| JCAHO Accredited, No. (%) | 519 (70.6) | 1235 (83.7) | 648 (87.9) | <0.001 |
| Region, No. (%) b | <0.001 | |||
| Northeast | 86 (12.2) | 240 (16.5) | 145 (19.7) | |
| Midwest | 218 (31.0) | 247 (33.6) | 542 (37.3) | |
| South | 262 (37.3) | 467 (32.1) | 184 (25.0) | |
| West | 137 (19.5) | 205 (14.1) | 137 (21.6) | |
| Rural hospital, No. (%)* | 270 (36.9) | 461 (31.4) | 119 (16.2) | 0.27 |
| Nurses per 100 Patients, median (IQR) | 4.5 (3.7–5.7) | 4.3 (3.6–5.4) | 4.2 (3.3–5.0) | <0.001 |
| Medicare patients (%), median (IQR) | 49.4 (43.3–54.8) | 48.2 (42.4–54.0) | 46.2 (40.4–52.7) | <0.001 |
| Medicaid patients (%), median (IQR) | 17.9 (13.4–24.4) | 17.4 (13.0–22.4) | 18.0 (12.5–22.3) | <0.001 |
| Cardiac Services, No. (%) | ||||
| Cardiac surgery capable | 72 (9.8) | 581 (39.4) | 434 (58.9) | <0.001 |
| PCI capable | 160 (21.8) | 810 (54.9) | 514 (69.7) | <0.001 |
| HF Volume, median (IQR) | 50 (31–96) | 121 (64–211) | 178 (101–272) | <0.001 |
Abbreviations: HF, heart failure; JCAHO, joint commission accreditation; IQR, interquartile range; PCI, percutaneous coronary intervention
Variable missing for 13 hospitals
Variable missing for 56 hospitals
Figure 1.
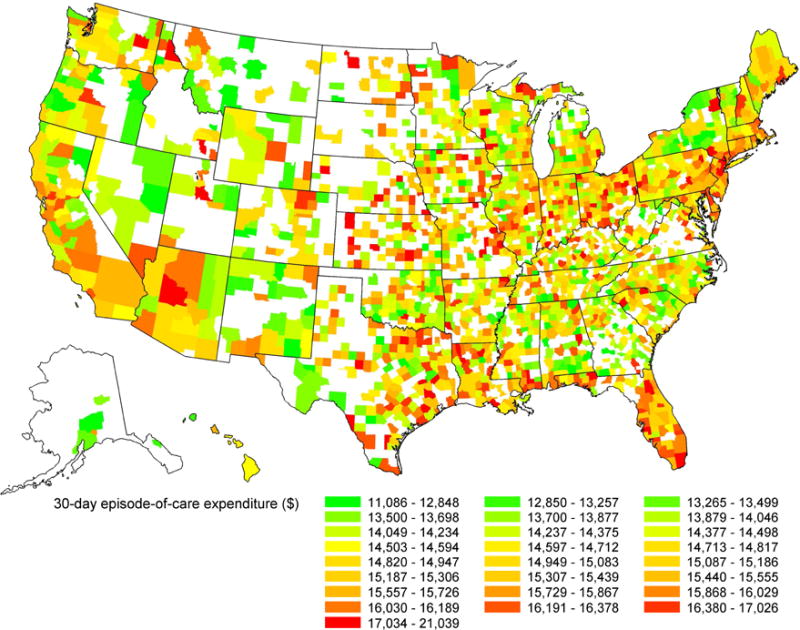
Geographic Variation in 30-day Episode Payments for Heart Failure Care
Hospital Structural Characteristics
Hospitals in the high 30-day episode payment group were larger, tended to be teaching hospitals, were more frequently Joint Commission accredited, were less likely to be public hospitals, and had lower nurse-staffing ratios, compared with hospitals in the average- and low-payment groups (Table 1). High episode payment hospitals also had greater median Medicare fee-for-service HF volume and were more likely to provide cardiac services including cardiac surgery and percutaneous coronary intervention (PCI).
Hospital Resource Use and Discharge Patterns
Procedure and resource use during and immediately following hospitalization varied across episode payment groups (Table 2). Hospitals in the high 30-day episode payment group were more likely to perform cardiac catheterizations and coronary angiograms during initial hospitalization. Overall rates of revascularization were low, but high episode payment hospitals were also more likely to perform PCI and coronary artery bypass grafting surgery during initial inpatient stay. Patients cared for in high episode payment hospitals had longer mean lengths of stay and were less likely to be transferred to another institution. They were more likely to be discharged to a SNF or with homecare services. In addition, observed 30-day readmission rates were highest at average-payment institutions compared with low and high-payment institutions.
Table 2.
Resource Use, Procedure Use and Discharge Patterns by 30-Day Episode Payment Categories
| Low (n=166052) |
Average (n=699251) |
High (n=478489) |
P Value | |
|---|---|---|---|---|
| Observed 30-day mortality (%) | 11.6 | 11.4 | 11.0 | <0.001 |
| Observed 30-day readmission rates (%) | 21.6 | 23.9 | 22.6 | <0.001 |
| Length of Stay (mean days) | 4.6 | 5.1 | 5.7 | <0.001 |
| Cardiac Procedures (Initial Admission) | ||||
| Cardiac catheterization (%) | 2.3 | 4.6 | 6.4 | <0.001 |
| Coronary angiogram (%) | 2.2 | 4.5 | 6.0 | <0.001 |
| Percutaneous coronary intervention (%) | 0.3 | 0.7 | 1.2 | 0.002 |
| CABG (%) | 0.04 | 0.18 | 0.32 | 0.05 |
| Discharge Disposition | ||||
| Transferred Out (%) | 3.8 | 2.2 | 1.6 | <0.001 |
| Discharged home (%) | 45.7 | 41.2 | 38.9 | <0.001 |
| Homecare on discharge (%) | 20.9 | 23.8 | 24.3 | <0.001 |
| Discharged to SNF (%) | 19.2 | 21.7 | 22.5 | <0.001 |
Abbreviations: IQR, interquartile range; CABG, coronary artery bypass grafting; SNF, skilled nursing facility
Thirty-Day Payments and Patient Mortality
Observed mortality in the overall population was 11.3%. Greater 30-day episode payments were associated with lower 30-day mortality (unadjusted OR 0.975 for every $1,000 increase; 95% CI 0.969–0.982, p<0.001, Figure 2). This relationship became more pronounced following adjustment for patient characteristics (Table 3 and eTable 2: OR 0.961 per $1,000 increase; 95% CI 0.954–0.967, p<0.001). When both patient characteristics, hospital characteristics, and HF volume were accounted for, higher hospital episode payments remained associated with lower 30-day patient mortality (OR 0.968 per $1,000 increase, 95% CI 0.962–0.975, p=<0.001). Addition of variables that could potentially mediate the relationship between episode payments and outcomes, including cardiac service capability and discharge to SNF or homecare use, did not alter our findings (Table 3).
Figure 2.
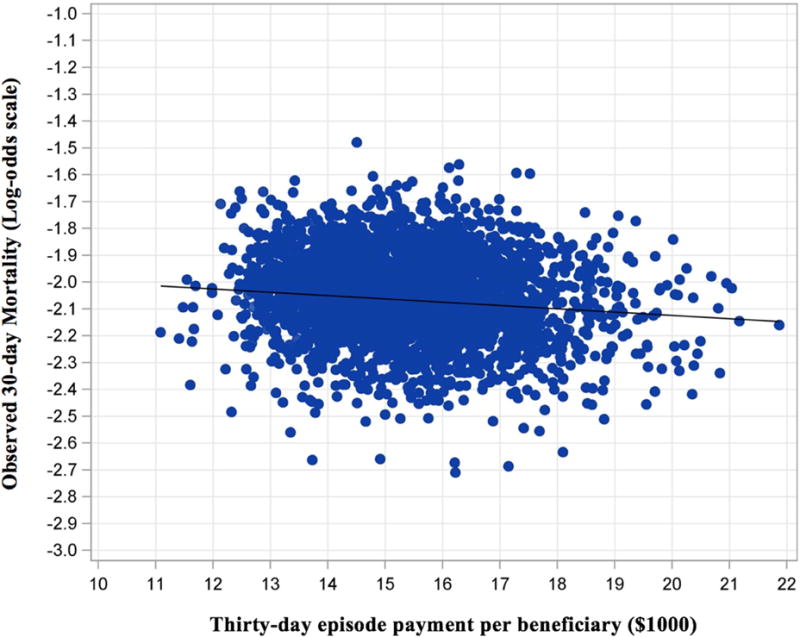
30-Day Episode Payments and Patient 30-day Mortality
Table 3.
Unadjusted and Multivariate Adjusted Odds of 30-Day Mortality for Every $1000 Increase in 30-Day Episode Payments
| Model | Odds Ratio (per $1000 increase) | 95% Confidence Interval |
|---|---|---|
| A | 0.975 | 0.969 – 0.982 |
| B | 0.961 | 0.954 – 0.967 |
| C | 0.972 | 0.966 – 0.979 |
| D | 0.968 | 0.962 – 0.975 |
| E | 0.969 | 0.962 – 0.977 |
| F | 0.969 | 0.962 – 0.976 |
A. Unadjusted
B. Adjusted for patient characteristics
C. Adjusted for patient and hospital characteristics
D. Adjusted for patient and hospital characteristics, and HF volume
E. Adjusted for patient/hospital characteristics, HF volume, and cardiac service capability
F. Adjusted for patient/hospital characteristics, HF volume, cardiac service capability and discharge disposition (SNF and home healthcare)
p<0.001 for all models
Additional Analyses
We found that the association between CMS inpatient payments and patient mortality was similar to our main analysis (eTable 3). We also examined whether the observed relationship between 30-day episode payments and mortality was consistent across all quantile levels of patient 30-day mortality. We found a predominately linear relationship across the distribution, though the association between episode payments and mortality was larger at higher quantiles of mortality (eFigure 2). Our iterative bootstrapping simulation demonstrated that the distribution of the odds ratios of the association between payments and outcomes remained significant (eFigure 3). Finally, we found that higher 30-day episode payments following a HF hospitalization were also associated with lower one year mortality (eTable 4).
Discussion
In this study of Medicare payments and mortality rates among beneficiaries hospitalized for HF, we found that higher Medicare payments for a 30-day episode of HF care, which included both inpatient and post-acute care payments across multiple settings, were associated with lower 30-day mortality even after accounting for patient case-mix. Overall, patients admitted for HF to hospitals with 30-day payments one standard deviation ($1523) above the mean, compared with hospitals one standard deviation below the mean, had an associated ≈1.3% lower mortality. This association was attenuated, but remained significant, after adjusting for key hospital characteristics and HF volume. Variation in hospital cardiac service capability and post-acute care use did not mediate the association between spending and outcomes. Collectively, our findings should not necessarily be interpreted as causal in nature, but rather, shed light on value and provide insight regarding HF care in the context of CMS episode-based payment models, particularly given the continued evolution of HVBP and ongoing uncertainty around cardiac bundled payment models (18).
There has been a broad interest among policymakers in improving the value of HF care, given the high and rising prevalence of HF and its associated financial burden. This interest is reflected in the addition of HF-specific spending measures, determined by Medicare payments made to hospitals, to the HVBP, as well as through alternate payment models (1,19). However, hospital characteristics associated with higher longitudinal payments are not accounted for in CMS payment models, leaving certain institutions susceptible to penalties, even if they provide high-quality care. In fact, early evidence from the HVBP demonstrates that some hospital types that tend to have better outcomes, including major teaching hospitals (20,21), often have high payments, as in our study, and consequently are more likely to be penalized (22). Conversely, some low-payment institutions that also provide low-quality care receive financial rewards (22). Whether or not the HVBP program truly incents value, then, is unclear.
As hospitals are held financially accountable for both longitudinal spending and outcomes following a hospitalization for HF, it will be important to understand what resources and services actually improve quality of care. It is possible that hospitals receiving higher payments use diagnostic testing, invasive procedures, specialist care, and intensive care units more frequently, to the benefit of outcomes (23). Alternatively, factors not captured in our study, such as use of education and counseling services, interdisciplinary collaborative ambulatory care, and home monitoring services may result in higher payments, but better care quality (24–26). In addition, early and frequent outpatient follow-up and the type of outpatient care received following discharge (i.e. primary care provider vs. cardiologist vs. HF clinic), may have also mediated the observed relationship (24). Understanding these mechanisms will be essential to ensure that hospitals do not respond to payment programs, such as the HVBP, by reducing expenditures in a manner that is ultimately detrimental to patient care - a potential unintended consequence. Additionally, identifying low-value procedures, resources and services that are of little benefit to patient care will also be of equal importance as hospitals navigate where to reduce expenditures (27).
Our study found significant differences in institutional characteristics across low, average, and high episode payment groups. While controlling for these characteristics in our analysis only somewhat attenuated our findings, and do not necessarily account for heterogeneity in care delivered within hospitals, these patterns may shed light on potential underlying mechanisms. For example, high-payment hospitals were more likely to be large, teaching institutions. Prior studies have shown that admission for HF to major teaching hospitals, compared with nonteaching hospitals, is associated with lower 30-day mortality (20,21). Similarly, a greater proportion of high-payments hospitals were Joint Commission accredited, which has been linked to better performance on HF quality measures (28). HF volume and cardiac service capabilities also varied across hospital payment groups, which may reflect differences in institutional experience and expertise in caring for HF patients. Collectively, these patterns suggest that greater capacity and expertise may result in better outcomes for HF patients, albeit at higher costs.
We also found that beneficiaries at high-payment institutions had longer average lengths of stay, which may have resulted in patients being more clinically optimized at time of discharge. This kind of reasoning may also be supported by the Hospital Readmission Reduction Program - with its incentives to reduce readmission rates (29), the program may have helped counteract pressures for hospitals to discharge patients ever more quickly and encouraged greater care coordination. Notably, observed 30-day readmission rates were slightly higher in average-episode payment institutions compared to low and high payment groups. In addition, patients at high-payment institutions were more likely to be discharged to SNFs and/or with home health services. Though SNF utilization has been linked at the patient level with a higher risk of death, likely because it reflects greater severity of illness (30), the use of home health services as a supplemental support mechanism has been associated with lower mortality after HF hospitalization (31,32). We found that the use of these post-acute care services did not explain the relationship between higher payments and better outcomes, thus it is not clear whether such patterns necessarily reflect high-value HF care. This is consistent with prior work that has shown that greater high-intensity post-acute care use in higher-spending regions of the US is not associated with better quality care (33). As institutions have a greater financial stake in post-acute care for HF through shared-savings programs and episode-based payment models, they will be incentivized to ensure appropriate use of post-acute care services (34).
Prior investigations have focused on the association of inpatient spending with HF outcomes, though findings have been mixed. For example, a study of Medicare beneficiaries hospitalized in 2006 found that higher inpatient costs of care for HF were associated with lower mortality, while another found no relationship between risk-adjusted costs and HF outcomes (12,13). Two subsequent analyses in Medicare showed that higher hospital spending intensity was associated with better in-hospital HF outcomes. Both studies used an end-of-life expenditure index -spending on hospital and physician services provided in patients’ last year(s) of life – to assess spending intensity. This measure is informative for care intensity in general, but may not necessarily reflect condition-specific treatment decisions for patients not at the end of life (14,16,35,36). Our study is novel in that it examined payments over a longitudinal episode that included both inpatient and post-discharge care across multiple settings, which has greater relevance given the movement toward episode-based reimbursement. In addition, we evaluated HF-specific payments, rather than hospital costs, thus reflecting utilization beyond hospitals’ internal cost structure.
There are limitations of this study. Due to its observational nature, we are unable to make inferences about causation. We only examined Medicare patients over 65 years of age, and our findings may not generalize to other populations. Patients may have varied in ways that were not captured by the comorbidities coded in claims data; however, such unmeasured severity would have most likely biased our results towards the null. In addition, claims data does not capture clinical information (i.e. vitals signs, ejection fraction, biomarkers, cardiac medications) that is of relevance to a heart failure population. We did not account for socioeconomic determinants of health, because payment programs such as HVBP do not, though these factors do play an important role in HF outcomes (37). Thirty-day episode payments reflected aggregate data at the hospital level, which may be subject to ecological fallacy, though our outcome was evaluated at the patient level. We also lacked detailed clinical data and a decomposition of episode payment data with which to identify specific mechanisms by which higher payments improved outcomes -this represents an important area for future study. Though we defined value as the relationship between payments and outcomes, we were unable to characterize quality of life, which is an important consideration when evaluating value of care. Because our sample size was large, our interpretation of this analysis focused on the estimated effect sizes for the relationship between episode payments and outcomes, rather than the extent to which P values were significant.
In summary, we found that in a cohort of Medicare beneficiaries hospitalized for HF across a three-year period, higher 30-day episode payments for HF care was associated with lower mortality. Emerging payment models seek to incentivize high value HF care, but our findings illustrate the challenges institutions may face in balancing expenditures and clinical outcomes as these models hold practitioners and hospitals financially accountable for both these elements of care. Further research is needed to identify interventions that improve outcomes, both during and following hospitalization, to ensure that hospitals continue to invest in procedures, services, and resources that improve survival, while cutting wasteful utilization.
Supplementary Material
Perspectives.
Competency in Systems-Based Practice
Higher 30-day payments following an admission for heart failure are associated with a lower likelihood of mortality at 30-days.
Translational Outlook
Our findings highlight the challenges institutions may face as they are increasingly held financially responsible for both payments and outcomes associated with an episode of HF care through value-based and alternative payment programs. Further research is needed to understand the mechanisms that mediate the relationship between higher payments and better outcomes.
Acknowledgments
Dr. Rishi K. Wadhera is supported by NIH Training Grant T32HL007604-32, Brigham and Women’s Hospital, Division of Cardiovascular Medicine and by the Jerome H. Grossman, MD Fellowship in Healthcare Delivery Policy at the Harvard Kennedy School’s Healthcare Policy Program. He previously served as a consultant for Sanofi and Regeneron. Dr. Karen E. Joynt receives research support from the National Heart, Lung, and Blood Institute (K23HL109177-03) and is a former employee of the US Department of Health and Human Services, where she continues work on a limited basis as a contractor. Dr. Robert W. Yeh receives research support from the National Heart, Lung and Blood Institute (K23HL118138) and the Richard A. and Susan F. Smith Center for Outcomes Research in Cardiology.
Abbreviations
- HF
Heart Failure
- CMS
Centers for Medicare and Medicaid Services
- HVBP
Hospital Value-Based Purchasing Program
- SNF
Skilled Nursing Facility
- PCI
Percutaneous Coronary Intervention
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: All other co-authors have no disclosures.
References
- 1.Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–19. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fitch K, Pelizzari P, Pyenson B. The High Cost of Heart Failure for the Medicare Population: An Actuarial Cost Analysis. Milliman. 2015 [Google Scholar]
- 3.Fitch K, Pelizzari PM, Pyenson B. Inpatient Utilization and Costs for Medicare Fee-for-Service Beneficiaries with Heart Failure. Am Health Drug Benefits. 2016;9:96–104. [PMC free article] [PubMed] [Google Scholar]
- 4.Joynt KE, Orav EJ, Zheng J, Jha AK. Public Reporting of Mortality Rates for Hospitalized Medicare Patients and Trends in Mortality for Reported Conditions. Ann Intern Med. 2016;165:153–60. doi: 10.7326/M15-1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hospital Value-Based Purchasing. Centers for Medicare and Medicaid Services; 2017. [Google Scholar]
- 6.Ziaeian B, Sharma PP, Yu TC, Johnson KW, Fonarow GC. Factors associated with variations in hospital expenditures for acute heart failure in the United States. Am Heart J. 2015;169:282–289 e15. doi: 10.1016/j.ahj.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.2015 Condition-Specific Measure Updates and Specifications Report Hospital-Level 30-Day Risk-Standardized Payment Measures. Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE), 2015.
- 8.Payment and Value of Care - Hospital. Hospital Compare Datasets. 2017. Center for Medicare and Medicaid Website: Center for Medicare and Medicaid Website. [Google Scholar]
- 9.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 10.Yale New Haven Health Services Corporation, Center for Outcomes Research and Evaluation for the Centers for Medicare and Medicaid Services. Baltimore: Centers for Medicare and Medicaid Services; 2015. 2015 Condition-specific measures updates and specifications report hospital-level: 30-day risk standardized mortality measures. [Google Scholar]
- 11.Cubanski J, Neuman T, Griffin S, Damico A. Medicare Spending at the End of Life: A Snapshot of Beneficiaries Who Died in 2014 and the Cost of Their Care. Kaiser Family Foundation: Kaiser Family Foundation; 2016. [Google Scholar]
- 12.Chen LM, Jha AK, Guterman S, Ridgway AB, Orav EJ, Epstein AM. Hospital cost of care, quality of care, and readmission rates: penny wise and pound foolish? Arch Intern Med. 2010;170:340–6. doi: 10.1001/archinternmed.2009.511. [DOI] [PubMed] [Google Scholar]
- 13.Jha AK, Orav EJ, Dobson A, Book RA, Epstein AM. Measuring efficiency: the association of hospital costs and quality of care. Health Aff (Millwood) 2009;28:897–906. doi: 10.1377/hlthaff.28.3.897. [DOI] [PubMed] [Google Scholar]
- 14.Romley JA, Jena AB, Goldman DP. Hospital spending and inpatient mortality: evidence from California: an observational study. Ann Intern Med. 2011;154:160–7. doi: 10.7326/0003-4819-154-3-201102010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romley JA, Jena AB, O’Leary JF, Goldman DP. Spending and mortality in US acute care hospitals. Am J Manag Care. 2013;19:e46–54. [PMC free article] [PubMed] [Google Scholar]
- 16.Stukel TA, Fisher ES, Alter DA, et al. Association of hospital spending intensity with mortality and readmission rates in Ontario hospitals. JAMA. 2012;307:1037–45. doi: 10.1001/jama.2012.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen CL. An Introduction to Quantile Regression and the QUANTREG Procedure. SAS Institute Inc; [Google Scholar]
- 18.Ellison A. CMS will cancel major bundled payment initiatives. Becker’s Hospital Review. 2017 [Google Scholar]
- 19.Bundled Payments for Care Improvement (BPCI) Initiative: General Information Centers for Medicare and Medicaid Services, 2017
- 20.Burke LG, Frakt AB, Khullar D, Orav EJ, Jha AK. Association Between Teaching Status and Mortality in US Hospitals. JAMA. 2017;317:2105–2113. doi: 10.1001/jama.2017.5702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shahian DM, Liu X, Meyer GS, Torchiana DF, Normand SL. Hospital teaching intensity and mortality for acute myocardial infarction, heart failure, and pneumonia. Med Care. 2014;52:38–46. doi: 10.1097/MLR.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 22.Das A, Norton EC, Miller DC, Ryan AM, Birkmeyer JD, Chen LM. Adding A Spending Metric To Medicare’s Value-Based Purchasing Program Rewarded Low-Quality Hospitals. Health Aff (Millwood) 2016;35:898–906. doi: 10.1377/hlthaff.2015.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnato AE, Chang CC, Farrell MH, Lave JR, Roberts MS, Angus DC. Is survival better at hospitals with higher “end-of-life” treatment intensity? Med Care. 2010;48:125–32. doi: 10.1097/MLR.0b013e3181c161e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–22. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 25.Jurgens CY, Goodlin S, Dolansky M, et al. Heart failure management in skilled nursing facilities: a scientific statement from the American Heart Association and the Heart Failure Society of America. Circ Heart Fail. 2015;8:655–87. doi: 10.1161/HHF.0000000000000005. [DOI] [PubMed] [Google Scholar]
- 26.Hindricks G, Taborsky M, Glikson M, et al. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet. 2014;384:583–90. doi: 10.1016/S0140-6736(14)61176-4. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring low-value care in Medicare. JAMA Intern Med. 2014;174:1067–76. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmaltz SP, Williams SC, Chassin MR, Loeb JM, Wachter RM. Hospital performance trends on national quality measures and the association with Joint Commission accreditation. J Hosp Med. 2011;6:454–61. doi: 10.1002/jhm.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Readmissions Reduction Program (HRRP) Centers for Medicare and Medicaid Services, 2016
- 30.Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feltner C, Jones CD, Cene CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med. 2014;160:774–84. doi: 10.7326/M14-0083. [DOI] [PubMed] [Google Scholar]
- 32.Jones CD, Bowles KH, Richard A, Boxer RS, Masoudi FA. High-Value Home Health Care for Patients With Heart Failure: An Opportunity to Optimize Transitions From Hospital to Home. Circ Cardiovasc Qual Outcomes. 2017;10 doi: 10.1161/CIRCOUTCOMES.117.003676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Newhouse JP, Garber AM. Geographic variation in health care spending in the United States: insights from an Institute of Medicine report. JAMA. 2013;310:1227–8. doi: 10.1001/jama.2013.278139. [DOI] [PubMed] [Google Scholar]
- 34.Mechanic R. Post-acute care–the next frontier for controlling Medicare spending. N Engl J Med. 2014;370:692–4. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
- 35.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138:288–98. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- 36.Doyle JJ., Jr Returns to Local-Area Healthcare Spending: Evidence from Health Shocks to Patients Far From Home. Am Econ J Appl Econ. 2011;3:221–243. doi: 10.1257/app.3.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Joynt KE, De Lew N, Sheingold SH, Conway PH, Goodrich K, Epstein AM. Should Medicare Value-Based Purchasing Take Social Risk into Account? N Engl J Med. 2017;376:510–513. doi: 10.1056/NEJMp1616278. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


