Abstract
Objective/background:
Few adolescents report obtaining adequate amounts of sleep. Correlational studies have linked adolescent short sleep with driving crashes and sluggish cognitive tempo (SCT), a cluster of symptoms that include sluggishness and low persistence which are related to but distinct from inattention and sleepiness. The relationship between SCT and driving is understudied and no study has experimentally examined the relation between SCT and sleep. We examined the relationship between SCT and driving problems in a sample of chronically short-sleeping adolescents. We also examined whether experimentally extending sleep improved SCT and driving behaviors.
Participants/Methods:
Licensed 16–18-year-olds who regularly obtain 5–7 hours of sleep completed a 5-week at-home experimental protocol: a baseline week to determine typical sleep (TYP), followed in counterbalanced order by 2-week spans in which school-night bedtimes and rise times were (a) matched to TYP, or (b) modified to extend (EXT) time in bed by 1.5 hours/night. Sleep was monitored via actigraphy. Self- and parent-reported SCT and inattention, as well as self-report of driving problems, were obtained at baseline and following each condition. Of the 38 eligible participants who completed the baseline session, 24 completed all 5 weeks.
Results:
After controlling for inattention, only parent-reported SCT was significantly positively associated with self-report of purposeful driving violations at baseline. Adolescents reported less SCT during EXT than TYP. Also after controlling for inattention, participants who reported improvement in SCT demonstrated fewer driving problems during EXT than during TYP.
Conclusions:
Preliminary findings suggest that extending sleep in short-sleeping adolescents may help alleviate SCT symptoms and improve driving.
Keywords: sluggish cognitive tempo, inattention, chronic sleep deprivation, experimental sleep extension, automobile driving
1. Introduction
It is recommended that adolescents obtain 8–10 hours of sleep each night [1], though it is widely recognized that a large number of adolescents regularly fall short of this recommendation [2,3,4]. Moreover, shortened sleep duration in adolescence has been linked to a range of adverse outcomes [5]. One particularly concerning negative outcome associated with adolescent sleep deprivation is diminished driving ability [6]. Automobile crashes are a leading cause of adolescent deaths, and driving crashes occur often in short-sleeping adolescents [7,8]. This may be partially due to inattention resulting from sleep deprivation. In one study, adolescents whose attention worsened following experimental sleep restriction also showed less consistency in lateral vehicle control during driving simulation [9].
Sluggish cognitive tempo (SCT), characterized by symptoms such as daydreaming, slowed behavior/thinking, and confusion, may also play a role in the impact of sleep on driving. The study of SCT and its relation to attention-deficit/hyperactivity disorder (ADHD) has spanned over three decades, and it is established that SCT is associated with, but independent from, ADHD [10]. A recent meta-analysis on SCT concluded that there is “strong support for the internal validity of SCT” [10]. Further, while SCT correlates with sleep pathology and daytime sleepiness, it is distinct from both [10,11]. Studies examining whether SCT is associated with impairment beyond inattention are sorely needed [10]. Since driving demands SCT-relevant skills beyond basic attention, SCT may reflect a second mechanism by which insufficient sleep might affect adolescent driving.
This exploratory study examined the unique relationship between SCT and driving problems in a sample of adolescents who chronically sleep 5–7 hours on school nights. We examined whether experimental sleep extension reduced SCT and whether reduction in SCT was linked to improved driving. We hypothesized that sleep extension would mitigate SCT with an associated improvement in driving behaviors.
2. Method
The local IRB approved all study procedures. Adolescent informed assent and parental informed consent were obtained. Participants were healthy adolescents aged 16–18 years with a valid driver’s license who regularly obtained 5–7 hours of sleep on school nights (see Supplemental Table). Exclusionary criteria included: report of psychiatric or neurologic history, self-report or actigraphic evidence of <5 or >7 hours of typical sleep on school nights, medication use that affects sleep or alertness, symptoms of periodic limb movement disorder or obstructive sleep apnea, inflexible obligations that would not allow for bedtime shifts, and a body mass index >30.
During the school year, adolescent sleep was manipulated at home using a five-week experimental protocol, with office/assessment visits on the Friday afternoons of weeks 1, 3, and 5. Week 1 served as a baseline measure of sleep; teens were asked to follow normal their normal sleep patterns on school nights. Using a randomized-crossover design, adolescents participated in two sleep conditions, each lasting two weeks: Prescribed Typical Sleep (TYP), in which school-night bedtimes and rise times were matched to adolescents’ baseline sleep; versus Sleep Extension (EXT), in which the adolescent and his/her parent problem-solved ways to extend time in bed on school nights by 1.5 hrs (see Supplemental Table). On weekends, adolescents self-selected their sleep schedules, provided they did not shift sleep phase by >2 hours compared to school days.
Adherence to the protocol was monitored via actigraphy (Sleepwatch; Ambulatory Monitoring, Inc), and reviewed with parents and adolescents concurrently at each study visit. Here, we focused on weeknights within each condition.
SCT symptoms were measured using 14-item validated scales: the Sluggish Cognitive Tempo Scale [12] (parent-report) and Child Concentration Inventory [13] (self-report). Parent-report of ADHD inattention was assessed using 9 items on the validated Vanderbilt Rating Scale [14], with the wording modified slightly to allow adolescents to self-report [15]. Parents and adolescents rated symptoms for the “past five days” at the end of each condition.
Adolescents reported typical driving behavior (past 6 months) at baseline using the validated 50-item Driving Behavior Questionnaire (DBQ) [16]. This measure consists of three scales: violations (e.g., running red lights), dangerous errors (e.g., misjudging speed of oncoming vehicle), and silly errors/lapses (e.g., forgetting where car is parked). Changes in driving behavior were assessed following each sleep condition using a short-form of selected items. Based on the relationship between baseline SCT and DBQ (see Results), a short-form measure of 4 items assessing driving violations (speeding, “racing” other drivers, running red lights, and distracted driving) in the past 5 days was created. This short-form correlated moderately with the DBQ violations at baseline (r = .54, p = .004).
3. Results
Of 41 teens initially recruited, three were excluded prior to randomization due to ineligibility (e.g, obesity). The randomized 38 adolescents (63.2% female; Mage=16.82 years, SD=0.80, Mlicensed=1.32 months, SD=0.64) averaged 6.34 (SD=0.68) hours of weeknight sleep at baseline per actigraphy. Eleven did not complete the five-week protocol due to lack of interest or schedule conflicts, one was excluded from participation for being non-adherent to wearing the actigraph, and two did not adhere to the sleep condition instructions. The remaining 24 participants did not differ from non-completers on baseline demographics, SCT, driving behavior, or sleep duration.
In zero-order correlations, baseline parent-reported SCT correlated with self-reported DBQ violations (r=.36, p=.03), but not dangerous errors (r=.04, p=.81) or silly errors/lapses (r=.23, p=.18). Self-reported SCT correlated with all DBQ subscales (rs=.43-.52, ps ≤ .05). Parent-reported inattention was negatively, non-significantly, correlated with DBQ violations and was not significantly correlated with the remaining subscales. With the exception of a strong positive relationship with DBQ violations (r=.56, p=.000), self-reported inattention displayed similar relationships with the remaining DBQ scales as self-reported SCT. After controlling for inattention in partial correlations, parent-reported SCT was significantly positively correlated with violations (p=.01), but self-report of SCT symptoms was not significantly correlated with any baseline DBQ subscale (Table 1). Similarly, controlling for SCT rendered associations between inattention and subscales of the DBQ to non-significance with the following exceptions: parent-reported inattention remained negatively associated with DBQ violations and self-reported inattention remained positively associated with DBQ errors.
Table 1.
Zero-order and partial correlations between symptoms and self-reported driving problems at baseline
| Parent-Report SCT | Self-Report SCT | Parent-Report Inattention | Self-Report Inattention | |||||
|---|---|---|---|---|---|---|---|---|
| Zero-order | Partial | Zero-order | Partial | Zero-order | Partial | Zero-order | Partial | |
| Violations | .36* | .42* | .43** | .29 | −.25 | −.34* | .34* | .09 |
| Dangerous errors | .04 | .04 | .52** | .24 | .04 | .03 | .56** | .34* |
| Silly errors | .23 | .20 | .52** | .29 | .17 | .14 | .50** | .25 |
Note. SCT partial correlations control for inattention symptoms at baseline and inattention partial correlations control for SCT symptoms at baseline.
p < .05,
p < .01
Parents of adolescents who completed and adhered to the experimental protocol noted little change in SCT symptoms across conditions (t =0.87, p=.40), but the adolescents themselves reported fewer symptoms during EXT than TYP (t=3.25, p=.004; Cohen’s d=.71). Two SCT groups were created using median split of self-reported SCT: No Improvement and Improvement. Repeated measures analysis of covariance tested the effects of sleep condition on the short-form violations, with SCT group as the between subjects factor, covarying for inattention. The Sleep×SCT group interaction was significant [F(1, 21)=5.75, p=.03; η2p=.22]. The SCT Improvement group reported fewer driving violations during EXT than during TYP sleep (F=4.97, p= .04, η2p = .19). The SCT No Improvement group’s driving violations were not significantly different across sleep conditions (F=2.42, p=.14, η2p =.10, Figure 1).
Fig. 1.
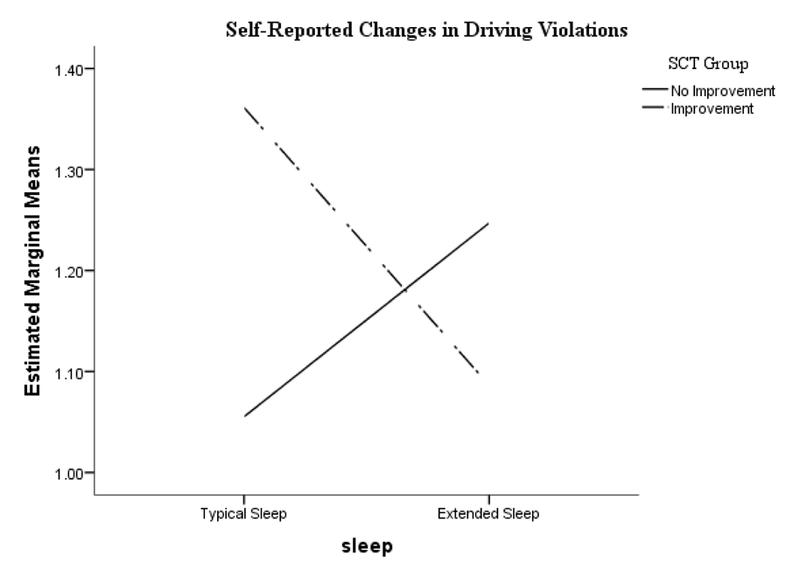
Results of follow-up test on the sleep condition × interaction. SCT Improvement group reported less driving violations during Extended Sleep than during Typical Sleep (p=.037). The SCT No Improvement group did not significant changes in violations as a function of sleep condition (p=.135).
4. Discussion
This is the first study to examine the impact of sleep extension on SCT in a sample of chronically short-sleeping adolescents. SCT symptoms – at least as experienced by the adolescents themselves – appear to be modified by extending sleep. This suggests that prior correlational links between SCT and sleep [10] may reflect true cause-effect relationships. Although SCT symptoms are distinct from sleepiness [10,17], lengthening sleep may alleviate SCT symptoms. SCT symptoms changed only by self-report. It has been argued that SCT may be an internal state, thus self-report may be especially important [10], though this is only the third study to date to include youth’s own report of their SCT symptoms [11,18].
This study was also the first to explore the relation between SCT and driving behaviors. SCT as reported by parents and adolescents was moderately to strongly correlated with several aspects of driving, but most of these associations were no longer significant after covarying ADHD inattention. Of note, ADHD inattention was also no longer associated with most driving domains after controlling for SCT. Although distinct constructs, SCT and inattention are strongly correlated [10]. It appears that controlling for the influence of the other often washes out the associations SCT and inattention each have with driving, though our sample size was small and may have contributed to the lack of unique effects found. However, SCT and inattention exhibited differential relationships with deliberate violations: SCT was uniquely positively associated with deliberate violations, whereas ADHD inattention was uniquely negatively associated with deliberate violations, suggesting that SCT may play a unique role in this aspect of adolescent driving. Given the positive association between DBQ violations with observable crash-related driving variables such as speed, the relationship between SCT and DBQ violations is notable [19]. It is also notable that the association between SCT and DBQ violations was a cross-rater relationship (parent-self, respectively) suggesting that this finding is not likely due to shared method variance. As noted above, we also note that we may have lacked statistical power to detect other unique effects for either SCT or ADHD inattention.
Sleep extension mitigated DBQ violations scores suggesting that changes in SCT could result in meaningful changes in driving behaviors known to increase crash risk. Sleep extension had the greatest effect on driving violations amongst adolescents who reported improvements in SCT, even when controlling for changes in attention. If replicated, this finding would be consistent with the notion that individuals vary in vulnerability/resilience relative to short sleep. Adolescents who show the greatest decline in attention after experimental sleep restriction also show the greatest decline in performance in driving simulation [9]; adolescents for whom sleep affects SCT the most may similarly be most vulnerable to driving violations when inadequately rested. Our findings are specific to a sample of adolescents experiencing chronic short-sleep on school nights. Although this is a common phenomenon during adolescence, future studies should examine the impact of sleep restriction and extension on SCT symptoms and driving in a variety of samples and with a diverse set of outcomes (e.g., official driving records). Future studies should include validated, applied measures of changes in driving behaviors. Finally, although attrition did not appear systematic, about a quarter of our sample dropped-out mostly due to conflicts in obligations. Preliminary findings suggest that alleviating chronic sleep restriction could be an important avenue for improving symptoms of SCT and driving, but additional work is needed.
Supplementary Material
Highlights.
Sluggish cognitive tempo (SCT) is uniquely associated with adolescent driving violations.
Sleep extension (EXT) reduces self-reported SCT relative to typical short-sleep (TYP).
Adolescents with improved SCT symptoms reported fewer driving violations during EXT versus TYP.
Acknowledgements:
We would like to thank Catharine Whitacre, Shealan McAlister, Perry Catlin, and Patrick Nalepka for their assistance executing this project. Funding was provided by a grant from the State of Ohio Emergency Medical Services. Dr. Garner reports grants from T32HT1002 National Research Service Award, during the conduct of the study. Dr. Becker is supported by award number K23MH108603 from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
REFERENCES
- 1.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, … & Kheirandish-Gozal L (2015). National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health, 1(4), 233–243. [DOI] [PubMed] [Google Scholar]
- 2.Gradisar M, Gardner G, & Dohnt H (2011). Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Medicine, 12(2), 110–118. [DOI] [PubMed] [Google Scholar]
- 3.Hysing M, Pallesen S, Stormark KM, Lundervold AJ, & Sivertsen B (2013). Sleep patterns and insomnia among adolescents: a population‐based study. Journal of Sleep Research, 22(5), 549–556. [DOI] [PubMed] [Google Scholar]
- 4.Maslowsky J, & Ozer EJ (2014). Developmental trends in sleep duration in adolescence and young adulthood: evidence from a national United States sample. Journal of Adolescent Health, 54(6), 691–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Becker SP, Langberg JM, & Byars KC (2015). Advancing a biopsychosocial and contextual model of sleep in adolescence: a review and introduction to the special issue. Journal of Youth and Adolescence, 44(2), 239–270. [DOI] [PubMed] [Google Scholar]
- 6.Martiniuk AL, Senserrick T, Lo S, Williamson A, Du W, Grunstein RR, … & Ivers RQ (2013). Sleep-deprived young drivers and the risk for crash: the DRIVE prospective cohort study. JAMA Pediatrics, 167, 647–655. doi: 10.1001/jamapediatrics.2013.1429 [DOI] [PubMed] [Google Scholar]
- 7.National Highway Traffic Safety Administration (NHTSA). (2011). Early estimate of motor vehicle traffic fatalities in 2010. Washington, DC: US Department of Transportation; Retrived from: http://wwwnrd.nhtsa.dot.gov/Pubs/811451.pdf [Google Scholar]
- 8.Pizza F, Contardi S, Antognini AB, Zagoraiou M, Borrotti M, Mostacci B, … & Cirignotta F (2010). Sleep quality and motor vehicle crashes in adolescents. Journal of Clinical Sleep Medicine, 6, 41–45. [PMC free article] [PubMed] [Google Scholar]
- 9.Garner AA, Miller MM, Field J, Noe O, Smith Z, & Beebe DW (2015). Impact of experimentally manipulated sleep on adolescent simulated driving. Sleep Medicine, 16, 796–799. doi: 10.1016/j.sleep.2015.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Becker SP, Leopold DR, Burns GL, Jarrett MA, Langberg JM, Marshall SA, … & Willcutt EG (2015). The internal, external, and diagnostic validity of sluggish cognitive tempo: A meta-analysis and critical review. Journal of the American Academy of Child & Adolescent Psychiatry, 55, 163–178. doi: 10.1016/j.jaac.2015.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becker SP, Garner AA, & Byars KC (2016). Sluggish cognitive tempo in children referred to a pediatric sleep disorders center: Examining possible overlap with sleep problems and associations with impairment. Journal of Psychiatric Research, 77, 116–124. doi: 10.1016/j.jpsychires.2016.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.10.Penny AM, Waschbusch DA, Klein RM, Corkum P, & Eskes G (2009). Developing a measure of sluggish cognitive tempo for children: Content validity, factor structure, and reliability. Psychological Assessment, 21, 380–389. doi: 10.1037/a0016600 [DOI] [PubMed] [Google Scholar]
- 13.Becker SP, Luebbe AM, & Joyce AM (2015). The Child Concentration Inventory (CCI): Initial validation of a child self-report measure of sluggish cognitive tempo. Psychological Assessment, 27, 1037–1052. doi: 10.1037/pas0000083 [DOI] [PubMed] [Google Scholar]
- 14.Wolraich ML, Lambert W, Doffing MA, Bickman L, Simmons T, & Worley K (2003). Psychometric properties of the Vanderbilt ADHD diagnostic parent rating scale in a referred population. Journal of Pediatric Psychology, 28, 559–568. doi: 10.1093/jpepsy/jsg046 [DOI] [PubMed] [Google Scholar]
- 15.Beebe DW, Fallone G, Godiwala N, Flanigan M, Martin D, Schaffner L, & Amin R (2008). Feasibility and behavioral effects of an at-home multi-night sleep restriction protocol for adolescents. Journal of Child Psychology and Psychiatry, 49, 915–933. doi: 10.1111/j.1469-7610.2008.01885.x [DOI] [PubMed] [Google Scholar]
- 16.Reason J, Manstead A, Stradling S, Baxter J, & Campbell K (1990). Errors and violations on the roads: A real distinction? Ergonomics, 33, 1315–1332. doi: 10.1080/00140139008925335 [DOI] [PubMed] [Google Scholar]
- 17.Becker SP, Luebbe AM, & Langberg JM (2014). Attention-deficit/hyperactivity disorder dimensions and sluggish cognitive tempo symptoms in relation to college students’ sleep functioning. Child Psychiatry & Human Development, 45, 675–685. doi: 10.1007/s10578-014-0436-8 [DOI] [PubMed] [Google Scholar]
- 18.Smith ZR, Becker SP, Garner AA, Rudolph CW, Molitor SJ, Oddo LE, & Langberg JM (2016). Evaluating the structure of sluggish cognitive tempo using confirmatory factor analytic and bifactor modeling with parent and youth ratings. Assessment, doi: 10.1177/1073191116653471. [DOI] [PubMed] [Google Scholar]
- 19.Zhao N, Mehler B, Reimer B, D’Ambrosio LA, Mehler A, & Coughlin JF (2012). Exploring relationship between the Driving Behavior Questionnaire and objective measures of highway driving behavior. In Transportation Research Board 91st Annual Meeting (No. 12–3621). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


