Abstract
Objective
Based on our recent studies the prevalence of polyclonal infection in tuberculosis clinical specimens is more than 50% in Tehran, Iran. With this background, Spoligotyping was performed on clinical specimens and their respective cultures, and we examined whether mixed infections interfere with the results or not.
Results
Based on the Spoligotyping pattern, among the fourteen patients, 57.1% had different genotypes in clinical samples and their respective cultures. These discrepant patterns were suggestive of polyclonal infections in clinical samples with possible overlapping Spoligotype patterns. We propose that in societies with high mixed infections (e.g. Iran), direct Spoligotyping on clinical samples can be controversial.
Keywords: Direct Spoligotyping, Tuberculosis, Polyclonal infection, MANU2 genotype
Introduction
Tuberculosis (TB) is still a major health problem all over the world. An essential tool in clinical microbiology and molecular epidemiology is genotyping of bacterial pathogens [1]. In many studies the researchers have used cultures for genotyping of Mycobacterium strains. But because of the slow growth of the bacteria in the culture medium, genotyping of samples from M. tuberculosis culture is also slowly [2]. Mycobacterium cultures can also be false negative, because some strains require more time to grow in culture [3]. Also, the growth of the various Mycobacterium lineages in the culture medium can be influenced by the expression of different genes in the pathways of metabolism of these lineages [4]. Therefore using a quicker method and using clinical samples directly for genotyping can be very crucial [5]. Several PCR-based methods have been used to study Mycobacterium genetic variation. The techniques include Spoligotyping and MIRU-VNTR typing [6]. In very few studies direct Spoligotyping on clinical specimens was performed [3].
One of the major issues with TB is mixed (polyclonal) infections, which is a person’s infection with several different genotypes of Mycobacterium [7]. MIRU-VNTR is the best and most widely used method for identifying mixed infections in TB [8]. Several studies have used MIRU-VNTR to diagnose mixed infections in clinical specimens and this method has been successful in detecting the mixed infections [9–11]. But a recent article suggests that mixed infections in clinical specimens can disrupt direct genotyping and challenge the Spoligotyping technique [3]. Multiple strain infections may cause false Spoligotypes that have been reported previously [5, 12].
The aim of the present study was comparing the direct and indirect Spoligotyping on clinical specimens and their respective cultures, respectively. We also examined whether mixed infections interfere with the results or not.
Main text
Methods
Sample collection and microscopy
This study was conducted between October 2017 and January 2018. Samples were from patients with definite diagnosis of pulmonary TB. Ethical reviews and informed consent approval were granted by the Ethical Committee of the Pasteur Institute of Iran. The written informed consent was obtained from all patients enrolled in the study. Study samples were included 14 clinical samples (11 smear positive and 3 smear negative). In our study, 12 clinical specimens including sputa and 2 samples were gastric juices. Clinical samples were classified by microscopy according to CDC guidelines [13].
Culture
Fourteen clinical specimens were decontaminated by N-acetyl-l-cysteine method and inoculated in Lowenstein–Jensen (LJ) medium.
DNA extraction from clinical samples and their respective cultures
For DNA extraction, the volume of clinical sample was 1.5 mL; after centrifugation, 500 μL of pellet was used. For their respective cultures single colony was selected and diluted in 500 μL TE buffer. After that, genomic DNA was extracted from clinical samples and their cultures with Proba-NK DNA extraction kit (DNA-Technology Company, Moscow, Russia) according to the manufacturer’s instructions. The DNA was stored at − 20 °C until used for molecular studies.
Spoligotyping on clinical samples and their respective cultures
Spoligotyping was performed in duplicate with a commercially available kit (Mapmygenome Genomics company, India) [14]. The PCR was performed on 10 ng purified chromosomal Mycobacterial DNA and 20 ng DNA extracts from clinical samples. M. tuberculosis H37Rv and M. bovis BCG (Pasteur strain) were used as control strains. Data analysis was performed by MIRU-VNTR plus [15, 16].
Results
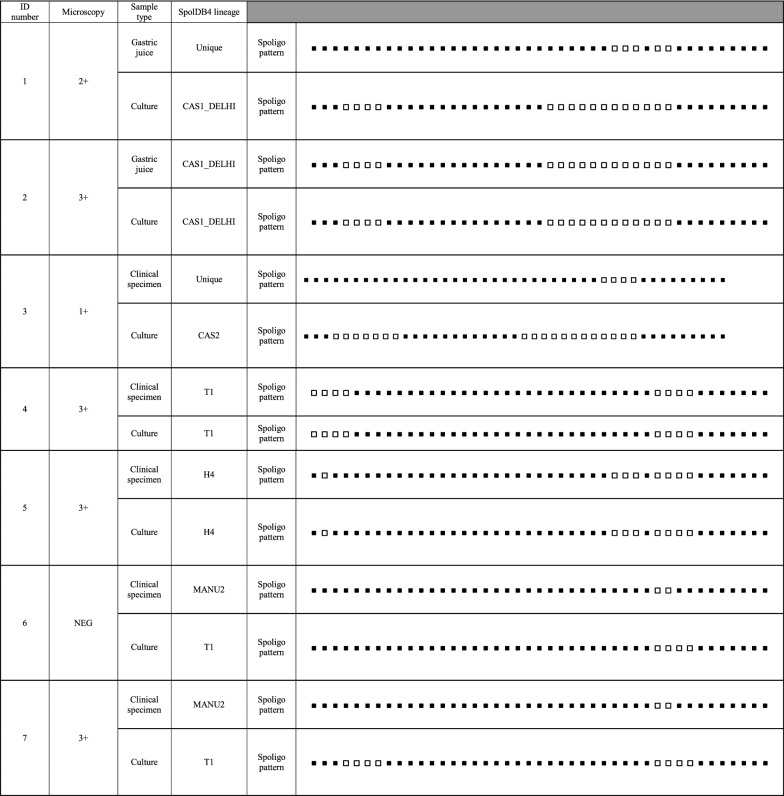
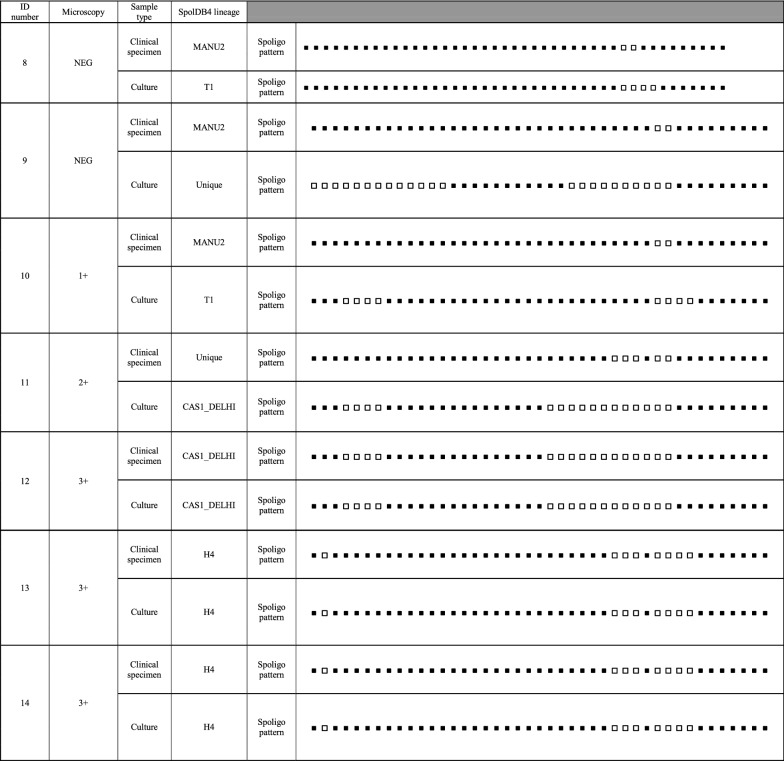
Based on the Spoligotyping pattern, among the fourteen patients, 57.1% (8/14) had different genotypes on clinical samples and their respective cultures. Direct and indirect Spoligotyping yielded the patterns in 100% (14/14) of the specimens and their respective cultures. Microscopy was negative in 3 sediments after decontamination. Of these, all of them was successful in direct Spoligotyping. In our study, 42.86% at Spoligotype had similarity between clinical samples and culture. According to SpolDB4 Lineage, among the 14 clinical samples, five (35.7%) belonged to MANU2 genotype which had the highest proportion in the genotype of clinical specimens. In clinical samples, other strains were classified into families included three strains (21.42%) from the H4 family, two (14.29%) from the CAS1-DELHI, one (7.14%) from the T1 family and three (3/14; 21.4%) strains were Unique.
On the other hand, among their respective cultures, T1 was the largest lineage (5/14; 35.7%) and other strains were classified into families included four strains (28.57%) from the CAS1-DELHI family, three (21.4%) from the H4 family, one (7.14%) from the CAS2 family and one (7.14%) strain was Unique. Interestingly, 62.5% (5/8) and 37.5% (3/8) of the samples with different genotypes in clinical samples and their respective cultures showed a genotype of MANU2 and Unique strains in their clinical sample, respectively. Additionally, 50% (4/8) and 37.5% (3/8) of the samples with different genotypes in clinical samples and their respective cultures showed Lineage 4 (SpolDB4 lineage T1) and Lineage 3 (SpolDB4 lineages CAS1-DELHI and CAS2) in their culture, respectively. All the Spoligotype patterns in clinical samples and their respective cultures from the 14 TB patients is summarized in Table 1.
Table 1.
Results of Spoligotyping of the clinical samples and their respective cultures from the 14 TB patients
Discussion
Our recent studies have shown that the rate of polyclonal infections in clinical specimens is more than 50 percent in our region [9–11]. With this background, Spoligotyping was performed on clinical specimens and their respective cultures, and interesting results were obtained.
The availability of all Spoligotype profiles in our study (100%) is higher than the 98.5% (196/199) found by Sanoussi et al., 90.9% (159/175) by Goyal et al., 49.1% (28/57) by Heyderman et al. on sputa and also higher than Suresh et al. and Zanden et al. on smears [3, 17–20]. These difference may due to DNA extraction methods from sputum [3]. Spoligotyping directly on clinical samples is very effective and time-saving as compared to indirect Spoligotyping on culture. It can also be used for samples that have been cultured negatively or contaminated [21, 22].
Of the 14 studied patients, 57.1% (8/14) had different genotypes on clinical samples and their respective cultures. These 8 samples with discrepant patterns were suggestive of mixed infections in clinical samples with possible overlapping Spoligotype patterns. Similar to our previous results, approximately 50% of mixed infections were observed in clinical specimens [9–11]. In the current study, 62.5% (5/8) of the samples with different genotypes in clinical samples and their respective cultures showed a genotype of MANU2 in their clinical samples. This could be another indication of the presence of mixed infections in these clinical specimens. In this regard, there are several studies that indicate that MANU2 genotype is rare in M.tb cultures in Iran. In none of these studies, the genotype MANU2 has been reported [23–30]. In addition, indirect Spoligotyping was performed by our group on 172 M.tb isolates, and in none of the strains, genotype MANU2 was observed (Unpublished data). Although two studies have suggested the presence of MANU2 in M.tb cultures in Iranian patients, but the percentage of this genotype in these two articles is very small in compare to our study (4.2 and 7.9% versus 35.7%) [31, 32].
On the other hand, Mozafari et al. worked on 1242 clinical samples in Iranian patients and MANU2 genotypes was detected in 25 cases [33]. This may indicate that in direct Spoligotyping, MANU2 is a result of mixed infections in clinical specimens in Iran. Albeit, it was not specific to this region; Lazzarini et al. suggested that MANU2 could be one of the five genotypes derived from mixed infections [34]. Also, the first evidence of the presence of the MANU lineages in Mozambique is the study of Viegas et al. who concluded that some of the MANU2 genotypes could be derived from a mixed infections of Beijing and T1 (or Beijing and T2) [35]. Additionally, in our study 37.5% (3/8) of the samples with different genotypes in clinical samples and their respective cultures showed a genotype of Unique strains in their clinical sample. This may indicate that the mixed infections can also occur in direct Spoligotyping as unique strains.
Our results showed that of 14 TB patients, direct and indirect Spoligotyping were fully successful even for negative smear specimens. These contradict the results of Sanoussi et al. who failed for direct Spoligotyping for their negative smear specimens [3]. Additionally, in a same study 94.4% (135/143) of the Spoligotype levels and 96.5% (138/143) of the lineage level were similar between sputum samples and cultures. They had only two samples containing mixed infections in the sputum samples [3]. On the other hand, in our study, 42.86% at Spoligotype level and 42.86% at the lineage level had similarity between clinical samples and culture. This is due to the large number of mixed infections in sputum samples in our study.
In the current study, 100% of samples that had a different pattern in Spoligotyping between sputum specimens and their culture, contained inter-lineage discrepancies. This may indicate the presence of completely different strains in samples containing mixed infections. In another study, it was shown that MANU2 contains inter-lineage discrepancy of the Beijing and Euro-American strains (T1 and T2 sublineages) [35]. Similarly, in the study of Sanoussi et al. patterns of simultaneous presence of ancestral and modern lineages were observed in the sputum and culture [3].
Additionally, 50% and 37.5% of the samples with different genotypes in clinical samples and their respective cultures showed Lineage 4 (SpolDB4 lineage T1) and Lineage 3 (SpolDB4 lineages CAS1-DELHI and CAS2) in their culture, respectively. In this regard, it has previously been established that the lineage 4 has grown faster (in liquid medium) than the lineage 1 and the ancestral lineage [36]. Also, according to a study by Viegas et al. who considered MANU2 as a mixture of T1 and Beijing, in our study, T1 seems to have more chance of rising in cultures derived from clinical specimens with mixed infections [35].
In conclusion, direct Spoligotyping is very efficient in regions where mixed infections are low in their clinical specimens. On the other hand, in societies with high mixed infections (e.g. Iran) in clinical specimens, we recommend to rule out mixed infection by the MIRU-VNTR method in the first step and after that direct Spoligotyping can be performed more accurately.
Limitations
The present study must be confirmed by investigation on more clinal samples from TB patients.
Authors’ contributions
MKK wrote the manuscript. FV supervised the project and revised the manuscript. FV, SDS and AF designed the project. MKK, SH, HG and SK performed laboratory work. GF and MKK isolated the strains and contributed to laboratory work. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank all the personnel of Mycobacteriology and Pulmonary Research Department, Pasteur Institute of Iran for their assistance in this project.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analyzed during the current study could become available through the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by Ethical Committee of the Pasteur Institute of Iran (Tehran, Iran), under the Ethics Code of 927. The written informed consent was obtained from all patients enrolled in the study.
Funding
This work was supported by a Grant [Number 927] from Pasteur Institute of Iran.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- TB
tuberculosis
- Spoligotyping
Spacer-oligotyping
- MIRU-VNTR
mycobacterial interspersed repetitive unit-variable number tandem repeat
- LJ
Lowenstein–Jensen
Contributor Information
Mansour Kargarpour Kamakoli, Email: mansour_kargarpour@yahoo.com.
Sharareh Khanipour, Email: shararehkhanipour@yahoo.com.
Shima Hadifar, Email: shima_hadifar@yahoo.com.
Hasan Ghajavand, Email: hasan.ghajavand@yahoo.com.
Ghazaleh Farmanfarmaei, Email: gh.farmanfarmaei@gmail.com.
Abolfazl Fateh, Email: afateh2@gmail.com.
Seyed Davar Siadat, Email: d.siadat@gmail.com.
Farzam Vaziri, Phone: +982164112823, Email: farzam_vaziri@yahoo.com, Email: f_vaziri@pasteur.ac.ir.
References
- 1.Organization WHO: investing to overcome the global impact of neglected tropical diseases: third WHO report on neglected tropical diseases 2015. World Health Organization; 2015.
- 2.Oelemann MC, Diel R, Vatin V, Haas W, Rüsch-Gerdes S, Locht C, Niemann S, Supply P. Assessment of an optimized mycobacterial interspersed repetitive-unit-variable-number tandem-repeat typing system combined with spoligotyping for population-based molecular epidemiology studies of tuberculosis. J Clin Microbiol. 2007;45:691–697. doi: 10.1128/JCM.01393-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanoussi CD, Affolabi D, Rigouts L, Anagonou S, de Jong B. Genotypic characterization directly applied to sputum improves the detection of Mycobacterium africanum West African 1, under-represented in positive cultures. PLOS Neglected Trop Dis. 2017;11:e0005900. doi: 10.1371/journal.pntd.0005900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ofori-Anyinam B, Dolganov G, Van T, Davis JL, Walter ND, Garcia BJ, Voskuil M, Fissette K, Diels M, Driesen M. Significant under expression of the DosR regulon in M. tuberculosis complex lineage 6 in sputum. Tuberculosis. 2017;104:58–64. doi: 10.1016/j.tube.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mokrousov I, Valcheva V, Sovhozova N, Aldashev A, Rastogi N, Isakova J. Penitentiary population of Mycobacterium tuberculosis in Kyrgyzstan: exceptionally high prevalence of the Beijing genotype and its Russia-specific subtype. Infect Genet Evol. 2009;9:1400–1405. doi: 10.1016/j.meegid.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 6.Pang Y, Zhou Y, Wang S, Lu J, Lu B, He G, Wang L, Zhao Y. A novel method based on high resolution melting (HRM) analysis for MIRU-VNTR genotyping of Mycobacterium tuberculosis. J Microbiol Methods. 2011;86:291–297. doi: 10.1016/j.mimet.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Balmer O, Tanner M. Prevalence and implications of multiple-strain infections. Lancet Infect Dis. 2011;11:868–878. doi: 10.1016/S1473-3099(11)70241-9. [DOI] [PubMed] [Google Scholar]
- 8.Cohen T, van Helden PD, Wilson D, Colijn C, McLaughlin MM, Abubakar I, Warren RM. Mixed-strain Mycobacterium tuberculosis infections and the implications for tuberculosis treatment and control. Clin Microbiol Rev. 2012;25:708–719. doi: 10.1128/CMR.00021-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamakoli MK, Sadegh HR, Farmanfarmaei G, Masoumi M, Fateh A, Javadi G, Jamnani FR, Vaziri F, Siadat SD. Evaluation of the impact of polyclonal infection and heteroresistance on treatment of tuberculosis patients. Sci Rep. 2017;7:41410. doi: 10.1038/srep41410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadegh H, Kamakoli MK, Farmanfarmaei G, Masoumi M, Abdolrahimi F, Fateh A, Ebrahimzadeh N, Jamnani FR, Vaziri F, Siadat SD. Pros and cons of direct genotyping on tuberculosis clinical samples. Microb Pathog. 2017;103:135–138. doi: 10.1016/j.micpath.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 11.Farmanfarmaei G, Kamakoli MK, Sadegh HR, Masoumi M, Abdolrahimi F, Fateh A, Ebrahimzadeh N, Javadi G, Jamnani FR, Vaziri F, Siadat SD. Bias in detection of Mycobacterium tuberculosis polyclonal infection: use clinical samples or cultures? Mol Cell Probes. 2017;33:1–3. doi: 10.1016/j.mcp.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 12.Shamputa IC, Rigouts L, Eyongeta LA, El Aila NA, Van Deun A, Salim AH, Willery E, Locht C, Supply P, Portaels F. Genotypic and phenotypic heterogeneity among Mycobacterium tuberculosis isolates from pulmonary tuberculosis patients. J Clin Microbiol. 2004;42:5528–5536. doi: 10.1128/JCM.42.12.5528-5536.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Thoracic Society Diagnostic standards and classification of tuberculosis in adults and children. Am J Respir Crit Care Med. 2000;161:1376–1395. doi: 10.1164/ajrccm.161.4.16141. [DOI] [PubMed] [Google Scholar]
- 14.Kamerbeek J, Schouls L, Kolk A, Van Agterveld M, Van Soolingen D, Kuijper S, Bunschoten A, Molhuizen H, Shaw R, Goyal M. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. 1997;35:907–914. doi: 10.1128/jcm.35.4.907-914.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allix-Béguec C, Harmsen D, Weniger T, Supply P, Niemann S. Evaluation and strategy for use of MIRU-VNTRplus, a multifunctional database for online analysis of genotyping data and phylogenetic identification of Mycobacterium tuberculosis complex isolates. J Clin Microbiol. 2008;46:2692–2699. doi: 10.1128/JCM.00540-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MIRU-VNTRplus. http://www.miru-vntrplus.org/MIRU/index.faces. Accessed 1 Jan 2018.
- 17.Goyal M, Lawn S, Afful B, Acheampong J, Griffin G, Shaw R. Spoligotyping in molecular epidemiology of tuberculosis in Ghana. J Infect. 1999;38:171–175. doi: 10.1016/S0163-4453(99)90246-3. [DOI] [PubMed] [Google Scholar]
- 18.Heyderman R, Goyal M, Roberts P, Ushewokunze S, Zizhou S, Marshall B, Makombe R, Van Embden J, Mason P, Shaw R. Pulmonary tuberculosis in Harare, Zimbabwe: analysis by spoligotyping. Thorax. 1998;53:346–350. doi: 10.1136/thx.53.5.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suresh N, Arora J, Pant H, Rana T, Singh UB. Spoligotyping of Mycobacterium tuberculosis DNA from Archival Ziehl–Neelsen-stained sputum smears. J Microbiol Methods. 2007;68:291–295. doi: 10.1016/j.mimet.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 20.Van Der Zanden A, Te Koppele-Vije E, Bhanu NV, Van Soolingen D, Schouls L. Use of DNA extracts from Ziehl–Neelsen-stained slides for molecular detection of rifampin resistance and spoligotyping of Mycobacterium tuberculosis. J Clin Microbiol. 2003;41:1101–1108. doi: 10.1128/JCM.41.3.1101-1108.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gehre F, Antonio M, Faïhun F, Odoun M, Uwizeye C, de Rijk P, de Jong BC, Affolabi D. The first phylogeographic population structure and analysis of transmission dynamics of M. africanum West African 1—combining molecular data from Benin, Nigeria and Sierra Leone. PLoS ONE. 2013;8:e77000. doi: 10.1371/journal.pone.0077000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koro FK, Simo YK, Piam FF, Noeske J, Gutierrez C, Kuaban C, Eyangoh SI. Population dynamics of tuberculous Bacilli in Cameroon as assessed by spoligotyping. J Clin Microbiol. 2013;51:299–302. doi: 10.1128/JCM.01196-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Velayati AA, Masjedi MR, Farnia P, Tabarsi P, Ghanavi J, ZiaZarifi AH, Hoffner SE. Emergence of new forms of totally drug-resistant tuberculosis bacilli: super extensively drug-resistant tuberculosis or totally drug-resistant strains in Iran. Chest. 2009;136:420–425. doi: 10.1378/chest.08-2427. [DOI] [PubMed] [Google Scholar]
- 24.Doustdar F, Khosravi AD, Farnia P, Bahrmand AR, Masjedi MR, Velayati AA. Mutations in rpoB gene and genotypes of rifampin resistant Mycobacterium tuberculosis isolates in Iran. Tanaffos. 2008;7:11–17. [Google Scholar]
- 25.Ravansalar H, Tadayon K, Mosavari N, Derakhshan M, Ghazvini K. Genetic diversity of Mycobacterium tuberculosis complex isolated from patients in the Northeast of Iran by MIRU-VNTR and spoligotyping. Jundishapur J Microbiol. 2017;10(4):e39568. [Google Scholar]
- 26.Rezaei F, Haeili M, Mohajeri P, Shahraki AH, Fooladi AAI, Zahednamazi F, Feizabadi MM. Frequency of mutational changes in the embB among the ethambutol-resistant strains of Mycobacterium tuberculosis in Iran. J Infect Dev Ctries. 2016;10:363–368. doi: 10.3855/jidc.7215. [DOI] [PubMed] [Google Scholar]
- 27.Velayati AA, Farnia P, Mirsaeidi M, Reza Masjedi M. The most prevalent Mycobacterium tuberculosis superfamilies among Iranian and Afghan TB cases. Scand J Infect Dis. 2006;38:463–468. doi: 10.1080/00365540500504117. [DOI] [PubMed] [Google Scholar]
- 28.Merza MA, Farnia P, Salih AM, Masjedi MR, Velayati AA. The most predominant spoligopatterns of Mycobacterium tuberculosis isolates among Iranian, Afghan-immigrant, Pakistani and Turkish tuberculosis patients: a comparative analysis. Chemotherapy. 2010;56:248–257. doi: 10.1159/000316846. [DOI] [PubMed] [Google Scholar]
- 29.Masjedi MR, Varahram M, Mirsaeidi M, Ahmadi M, Khazampour M, Tabarsi P, Baghei P, Marjane M, Bahadori M, Zarifi AZ. The recent-transmission of Mycobacterium tuberculosis strains among Iranian and Afghan relapse cases: a DNA-fingerprinting using RFLP and spoligotyping. BMC Infect Dis. 2008;8:109. doi: 10.1186/1471-2334-8-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farnia P, Masjedi MR, Mirsaeidi M, Mohammadi F, Jallaledin-Ghanavi, Vincent V, Bahadori M, Velayati AA. Prevalence of Haarlem I and Beijing types of Mycobacterium tuberculosis strains in Iranian and Afghan MDR-TB patients. J Infect. 2006;53:331–336. doi: 10.1016/j.jinf.2005.12.020. [DOI] [PubMed] [Google Scholar]
- 31.Feyisa SG, Haeili M, Zahednamazi F, Mosavari N, Taheri MM, Hamzehloo G, Zamani S, Feizabadi MM. Molecular characterization of Mycobacterium tuberculosis isolates from Tehran, Iran by restriction fragment length polymorphism analysis and spoligotyping. Rev Soc Bras Med Trop. 2016;49:204–210. doi: 10.1590/0037-8682-0405-2015. [DOI] [PubMed] [Google Scholar]
- 32.Zamani S, Haeili M, Nasiri MJ, Imani Fooladi AA, Javadpour S, Feizabadi MM. Genotyping of Mycobacterium tuberculosis isolates from Hormozgan province of Iran based on 15-locus MIRU-VNTR and spoligotyping. Int J Bacteriol. 2016;2016:1746470. doi: 10.1155/2016/7146470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mozafari M, Farnia P, Afraei M, Derakhshani-Nezhad Z, Masjedi MR, Velayati AA. Molecular diversity of Mycobacterium tuberculosis strains indifferent provinces of Iran. Iran J Microbiol. 2013;5:366. [PMC free article] [PubMed] [Google Scholar]
- 34.Lazzarini LCO, Rosenfeld J, Huard RC, Hill V, e Silva JRL, DeSalle R, Rastogi N, Ho JL. Mycobacterium tuberculosis spoligotypes that may derive from mixed strain infections are revealed by a novel computational approach. Infect Genet Evol. 2012;12:798–806. doi: 10.1016/j.meegid.2011.08.028. [DOI] [PubMed] [Google Scholar]
- 35.Viegas SO, Machado A, Groenheit R, Ghebremichael S, Pennhag A, Gudo PS, Cuna Z, Miotto P, Hill V, Marrufo T. Molecular diversity of Mycobacterium tuberculosis isolates from patients with pulmonary tuberculosis in Mozambique. BMC Microbiol. 2010;10:195. doi: 10.1186/1471-2180-10-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sarkar R, Lenders L, Wilkinson KA, Wilkinson RJ, Nicol MP. Modern lineages of Mycobacterium tuberculosis exhibit lineage-specific patterns of growth and cytokine induction in human monocyte-derived macrophages. PLoS ONE. 2012;7:e43170. doi: 10.1371/journal.pone.0043170. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study could become available through the corresponding author on reasonable request.