Abstract
Background:
Several attempts (radiographic and nonradiographic) have been made to measure the lumbar lordosis (LL), but the results differ substantially as investigators have used different parameters. Radiography is the gold standard, and the methods include lumbosacral angle (LSA), lumbosacral joint angle (LSJA), Cobb angle, and tangential radiologic assessment of LL (TRALL) angle. The traditional method, the Cobb technique, has a wide range of normal mean values, with a large standard deviation. Using a more reliable radiographic angle will hopefully simply and standardize LL measurement in the diagnosis, treatment, and follow-up of patients.
Aim:
To compare in normal individuals with fully developed LL the LSA, LSJA, TRALL, and Cobb angles, by determining (a) if any correlation exists between them and (b) the most reliable measures of LL, based on, least (i) number of measurement lines, (ii) range of values, (iii) mean, (iv) standard deviation, and (v) variance.
Materials and Methods:
The four angles were retrospectively measured in each supine lateral lumbosacral radiograph of 100 males and 100 females, aged 15 years and above. Data were analyzed with IBM SPSS Statistics 23.0 (NY, USA); P < 0.05 was considered statistically significant.
Results:
No correlation existed between the mean values of the four angles, and in each angle, there was no male-versus-female correlation. LSJA had the best reliability criteria for LL measurement.
Conclusion:
The mean LSA, LSJA, TRALL, and Cobb angles have no significant Pearson's correlation, and of the four angular measures of LL, LSJA was the most reliable.
Keywords: Comparison, correlation, lumbar lordosis, methods, radiography, reliability
INTRODUCTION
Lumbar lordosis (LL) is the curvature assumed by intact lumbar spine to compensate for the inclination of the sacrum, restore an upward spinal orientation, and consequently avoid a forward inclination.[1] It is anteriorly convex in the mid-sagittal plane.[2] This curve gives the lumbar spine certain resilience and helps protect it from compressive forces. If the spine were straight, compressive forces would be transferred through the vertebral bodies to the intervertebral discs (IVDs, the shock absorbers of the spine) alone. In the curved lumbar spine, some of the compressive force is taken by the anterior longitudinal ligaments.[3] The alteration of LL may cause low back pain (LBP) and disabilities, especially in adults. Although most patients might have mild and transient symptoms that decline within 6 weeks,[4] about 15%–45% will have chronic symptoms that persist beyond 3 months.[5] For this latter group, the impact on quality of life and economic implications is extensive.[6] The LL may be altered by congenital disabilities, trauma, and degenerative and inflammatory disorders; therefore, reliable measurements of this curve have relevance to the diagnosis and continuing care of patients with these disorders.[7]
Various attempts have been made to measure the LL; however, as investigators have used different parameters, the results differ substantially. Radiography is one such method, and a supine lateral lumbosacral spine radiograph accurately measures LL, and this radiographic method remains the gold standard.[8,9,10] Some of the radiographic angular measures of LL include lumbosacral angle (LSA),[11,12] lumbosacral joint angle (LSJA),[3,13] Cobb angle,[14] and tangential radiologic assessment of LL (TRALL) angle.[7] Other nonradiographic methods that have been used to quantify the LL include goniometry,[15] flexible rulers,[16] software method,[17] spinal mouse,[18] spinal pantograph,[19] inclinometer,[20] and magnetic resonance imaging (MRI).[21]
In the radiographic LL measurement, the traditional method is the Cobb method, which is effective for scoliosis, however, which may provide less reliable information for vertebral column changes measured in the sagittal plane.[14] Previous studies of LL in healthy adults and children with the Cobb method have demonstrated a wide range of normal mean LL values with a large standard deviation.[7,8,14,22,23,24,25,26,27,28] Furthermore, in children under 16 years of age, the Cobb angle showed the most variability when compared to TRALL angle, on the one hand,[7] and TRALL and LSA, on the other hand.[29]
A reliable radiographic angular measure of LL should not only be easy to measure but should also have a small range of values, small standard deviation, and small variance, when compared to the other radiographic methods. Previous studies have tended to compare Cobb angular measure with usually one and rarely two other angles.
The aim of this study was to compare, in normal individuals with fully developed LL, the Cobb angle (the traditional angular measure of LL) with LSA, LSJA, and TRALL angle, which are three other angular measures of LL, and determine which is most reliable based on ease of measurement (i.e., no of measurement lines), least range of values, least mean, least standard deviation, and least variance. Using the most reliable angle will hopefully simply and standardize LL measurement in the diagnosis, treatment, and follow-up of patients.
MATERIALS AND METHODS
In this retrospective study of archival radiographs, the patients were merged for number (100 males and 100 females), sex (male and female), and age (16–72 years). In each radiograph, four radiographic angular measures of LL were measured; the angles were Cobb, LSA, LSJA, and TRALL. The radiographs were from the archives of a tertiary health institution in southeastern part of Nigeria, from 2000 to 2002. The study center normally does its lumbosacral radiographs in the lateral recumbent posture using standard radiographic imaging technique (for patient positioning and exposure).
The inclusion criteria were (a) age ≥15 years; this is to ensure that virtually all studied individuals have attained full LL development which occurs at spinal maturity;[30] and (b) normal radiographs with no associated vertebral pathology [Figure 1]. The exclusion criteria included patients <15 years of age or whose age and/or sex were not documented in the request form, radiographs that were of poor quality and/or showing any vertebral pathology.
Figure 1.

Normal lateral lumbosacral spine radiograph
A retrospective approach was used in this study to avoid the ethical issue of patient's irradiation, even though a prospective method using normal subjects would have been ideal. Even if some of the studied radiographs were those of patients who presented with back complaints, low back pain without any radiographically demonstrable vertebral pathology has been reported not to significantly affect the degree of normal LL.[31,32] Supine lateral films were studied because a supine lateral lumbosacral film accurately measures LL, and this radiographic method remains the gold standard.[8,9,10] Although erect radiographs would have been preferable due to some concern about posture and its possible effect on spine curvature, LL has been reported to be insignificantly different in the recumbent and upright positions;[33,34] in healthy individuals, the tone of the spinal muscles was thought to be sufficient to prevent such an increase in the upright position.[7] Demographic data and clinical information were retrieved from the filled out request forms, usually left in the film jackets. The author reviewed each individual's radiograph and measured the LL angle by (a) mounting the radiograph on a viewing screen with good illumination, (b) drawing measurement lines (using appropriate landmarks) with a 30-cm long transparent ruler and pencil, and (c) measuring the angles in degrees with a protractor.
Cobb angle was between perpendiculars from the superior endplate of L1 and the superior endplate of S1 [Figure 2a].[14] The LSA was between a horizontal line and a line through the plane of the superior margin of S1 [Figure 2b].[11,12] The LSJA was between a line through the inferior endplate of L5 and another through the superior endplate of S1 [Figure 2c].[3,14] The TRALL angle was measured as described by Chernukha et al. [Figure 2d].[7] Along the posterior vertebral bodies: (a) arc line (curved line from the superior end plate of L1 to the inferior end plate of S2) was drawn; (b) chord line (line connecting the superior end plate of L1 and the inferior end plate of S2) was drawn, and the greatest perpendicular distance between the arc line and the chord line was determined; and (c) from the point where the greatest perpendicular distance is touching the arc line, two lines were drawn, one to L1 (upper part of chord line) and the other to S2 (lower part of chord line); the intersection of these two lines is the TRALL angle.
Figure 2.
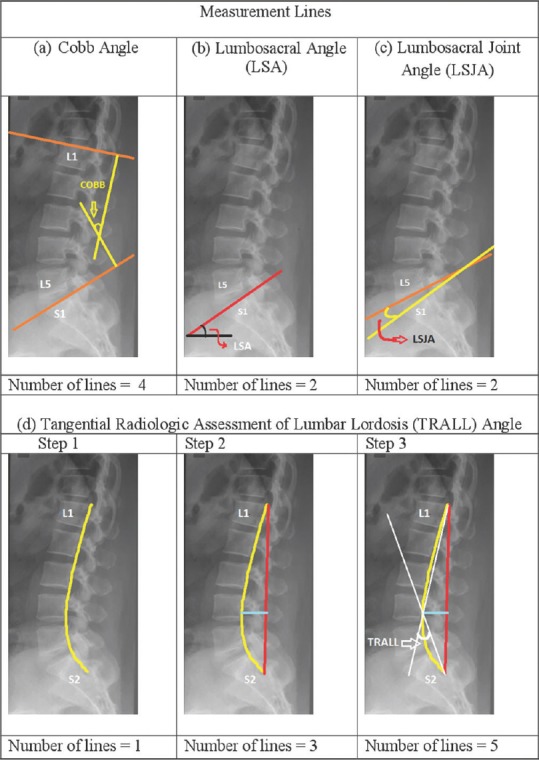
Lumbosacral angle, lumbosacral joint angle, Cobb, and tangential radiologic assessment of lumbar lordosis angles measurement lines in a normal lateral lumbosacral spine radiograph
Data were analyzed with IBM SPSS Statistics 23.0 (NY, USA); P < 0.05 was considered statistically significant. Some of the statistical methods employed included range of values, mean and standard deviation, variance, test of significance, and Pearson's correlation analysis.
RESULTS
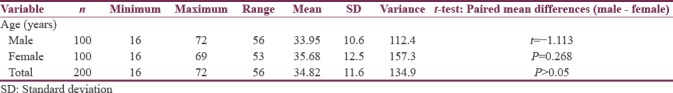
The age range of 200 individuals (100 males and 100 females) studied was 16–72 years; mean (standard deviation) was 34.8 (11.6) years and showed no significant gender difference (t = −1.113; P = 0.268) [Table 1].
Table 1.
Age variation by gender, and t-tests between genders
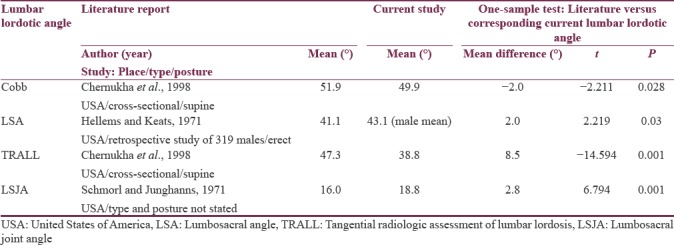
The mean (standard deviation) of the Cobb angle was 49.9° (12.8°); the male was 47.4° (10.7°) and the female 52.4° (14.2°). The gender difference was significant (t = −2.868, P = 0.005). The LSA, TRALL, and LSJA were 44.2° (10.0°), 38.8° (8.3°), and 18.8° (5.7°), respectively, and there was no significant gender difference in each angle [Table 2]. The four mean values compared favorably, though with some slight differences, with some corresponding literature values [Table 3].[3,7,35]
Table 2.
Lumbar lordotic angles variation by gender, and t-tests between genders
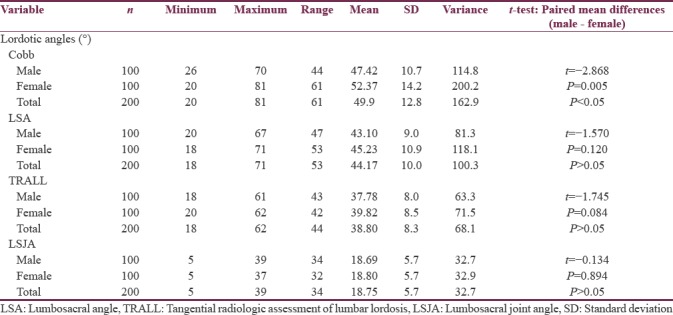
Table 3.
T-test of current mean lumbar lordotic angles with some corresponding literature values
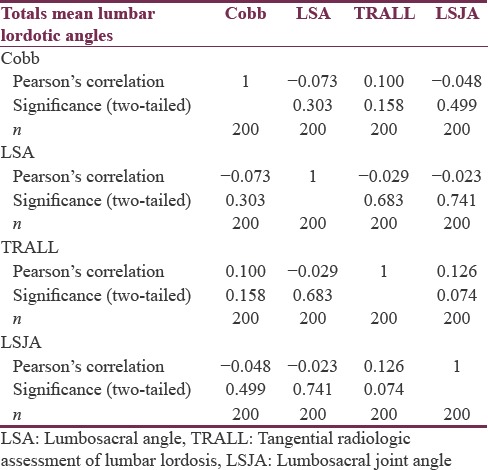
The mean of each angle showed no male-versus-female Pearson's correlation [Table 4] and all four angles showed no Pearson's correlation between their mean values [Table 5].
Table 4.
Paired samples correlations of the male-versus-female lumbar lordotic angles
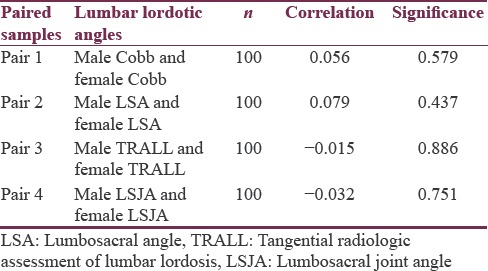
Table 5.
Totals mean lumbar lordotic angles correlations (i.e., bivariate correlation analysis with two-tailed test of significance)
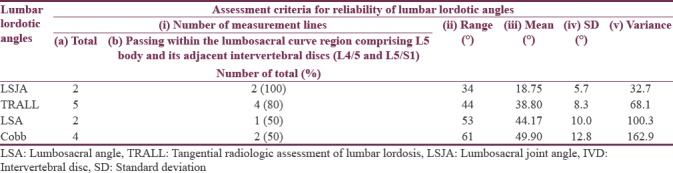
The assessment of reliability criteria for the four LL angles showed that the LSJA (apart from having the same least number of measurement lines with the LSA) had the least of each of the other four reliability criteria and was therefore the most reliable angular measure of LL [Table 6].
Table 6.
Summary of assessment criteria for reliability of lumbar lordotic angles
DISCUSSION
All the four LL mean angles obtained in this study compared favorably, though with some slight differences, with some literature values [Table 3].[3,7,35] This indicates that the values obtained in this study were most likely reliable. The four studied angles can therefore be more confidently compared to each other using the reliability criteria itemized in this study.
The reliability criteria for measuring the four LL angles showed that the LSJA (apart from having the same least number of measurement lines with the LSA) had the least of each of the other four reliability criteria (used in this study) and was therefore the most reliable angular measure of LL [Table 6]. It is therefore being recommended as a simple and standard radiographic angular measure of LL in the diagnosis, treatment, and follow-up of patients. Furthermore, the mean values of all the four studied angles (Cobb, LSA, TRALL, and LSJA) showed no Pearson's correlation [Table 5]; this implies that none of the four angles can be estimated from the measurement of another; each one intended for use must be measured. In other words, there is no way of converting the LL values of any of the angles to any of the others. There was also no male-versus-female correlation of the mean values in each of the four angles studied [Table 4].
Several investigators have shown that 50%–75% of the total LL between L1 and S1 was located at the bottom two motion segments made up of the IVD of L4/5, vertebral body of L5, and IVD of L5/S1 (lumbosacral transition).[36,37,38,39] The lumbosacral transition is normally at the level of L5/S1 and the IVD at this level is wedge shaped, with its anterior vertical height greater than the posterior.[30,40] The LSJA is the angle between a line through the inferior endplate of L5, and another through the superior endplate of S1;[3,13] its two measurement lines are therefore completely (i.e. 100%) located within the L5/S1 IVD space. This might largely account for why it was the most reliable angular measure of LL in comparison to LSA, Cobb and TRALL angles which have some of their measurement lines outside the bottom two motion segments (of the total LL between L1 and S1) made up of L5 body and its adjacent L4/5 and L5/S1 IVDs [Table 6].
After the LSJA, the next most reliable angular measures of LL were TRALL angle, followed by LSA; the Cobb angle was the least [Table 6]. The location of the measurement lines within or outside the lumbosacral curve region comprising the L5 body and its adjacent IVDs (L4/5 and L5/S1) might also largely account for this. Out of the five TRALL measurement lines, 4 (80%) passed within this region; the fifth line was further away. The LSA had 1 (50%) out of 2, and Cobb angle had 2 (50%) out of four measurement lines passing within this region. However, in the LSA, while the measurement line that did not pass within this region is fixed (does not move), those of the Cobb angle are mobile, and this might possibly explain why even though the LSA and Cobb angle have 50% of their measurement lines passing within this region, the Cobb angle was more variable than the LSA.
In this study, the fact that the LSJA, in comparison to the LSA, TRALL, and Cobb angles, had the least range of values, least mean, least standard deviation, and least variance, suggests that the range of LL is indeed not as wide as it had been reported for long by many investigators.[8,23,24,25,38,41,42] It seems that it is the technique of quantifying the LL that is responsible for the reported wide variability of the LL range of values by many authors. A prospective or retrospective study of lateral lumbosacral spine magnetic resonance images is being suggested as further study; this has no ethical issue of patients’ exposure to ionizing radiation.
The possible limitation of this study is that it is not a prospective (standardized) study, but a retrospective (nonstandardized) study. This pitfall was reduced by merging the patients for number (100 males and 100 females), sex (male and female), age (16–72 years), and measuring all the four studied angles in each radiograph. However, in the study of LL in normal individuals, the retrospective approach has been reported to be a credible alternative to the prospective method.[8,34] It is noteworthy that in the radiographic imaging of lateral lumbosacral spine, there is global standard positioning for erect posture, on the one hand, and recumbent posture, on the other hand, irrespective of whether it is a prospective or retrospective study. Even if some of the studied radiographs were taken in the erect posture (though the study center routinely takes their lateral lumbar radiographs in the supine position), their small number would have rendered them statistically insignificant. Furthermore, some authors have shown that the LL is not significantly different in the erect and recumbent positions.[33,34] In healthy individuals, the tone of the spinal muscles was thought to be sufficient to prevent such an increase in the upright position.[7]
CONCLUSION
In normal patients, there is no significant Pearson's correlation between the mean LSA, LSJA, TRALL and Cobb LL angles, and of the four angles, LSJA is the most reliable angular measure of LL, followed by the TRALL angle, and then, the LSA; the Cobb angle was the least.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Skaf GS, Ayoub CM, Domloj NT, Turbay MJ, El-Zein C, Hourani MH, et al. Effect of age and lordotic angle on the level of lumbar disc herniation. Adv Orthop 2011. 2011 doi: 10.4061/2011/950576. 950576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bogduk N, Twomey LT. Clinical Anatomy of the Lumbar Spine. 2nd ed. New York: Churchill Livingstone; 1991. pp. 45–7. [Google Scholar]
- 3.Schmorl G, Junghanns H. 2nd American edition. New York: Grune and Stratton; 1971. The Human Spine in Health and Disease; p. 43. [Google Scholar]
- 4.Dillane JB, Fry J, Kalton G. Acute back syndrome – A study from general practice. Br Med J. 1966;2:82–4. doi: 10.1136/bmj.2.5505.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: Studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993;9:174–82. doi: 10.1097/00002508-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 6.van Tulder MW, Koes BW, Bouter LM. A cost-of-illness study of back pain in the Netherlands. Pain. 1995;62:233–40. doi: 10.1016/0304-3959(94)00272-G. [DOI] [PubMed] [Google Scholar]
- 7.Chernukha KV, Daffner RH, Reigel DH. Lumbar lordosis measurement. A new method versus Cobb technique. Spine (Phila Pa 1976) 1998;23:74–9. doi: 10.1097/00007632-199801010-00016. [DOI] [PubMed] [Google Scholar]
- 8.Fernand R, Fox DE. Evaluation of lumbar lordosis. A prospective and retrospective study. Spine (Phila Pa 1976) 1985;10:799–803. doi: 10.1097/00007632-198511000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Vrtovec T, Pernus F, Likar B. A review of methods for quantitative evaluation of spinal curvature. Eur Spine J. 2009;18:593–607. doi: 10.1007/s00586-009-0913-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salisbury PJ, Porter RW. Measurement of lumbar sagittal mobility. A comparison of methods. Spine (Phila Pa 1976) 1987;12:190–3. doi: 10.1097/00007632-198703000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Ferguson AB. Clinical and roentgen interpretation of lumbosacral spine. Radiology. 1934;22:548–58. [Google Scholar]
- 12.Ferguson AB. Roentgen Diagnosis of the Extremities and Spine. 2nd ed. New York: Paul B. Hoeber, Inc; 1949. pp. 382–3. [Google Scholar]
- 13.Wiltse LL, Winter RB. Terminology and measurement of spondylolisthesis. J Bone Joint Surg Am. 1983;65:768–72. [PubMed] [Google Scholar]
- 14.Cobb J. Outline for the study of scoliosis. Am Acad Orthop Surg Instr Course Lect. 1948;5:261–75. [Google Scholar]
- 15.Burdett RG, Brown KE, Fall MP. Reliability and validity of four instruments for measuring lumbar spine and pelvic positions. Phys Ther. 1986;66:677–84. doi: 10.1093/ptj/66.5.677. [DOI] [PubMed] [Google Scholar]
- 16.de Oliveira TS, Candotti CT, La Torre M, Pelinson PP, Furlanetto TS, Kutchak FM, et al. Validity and reproducibility of the measurements obtained using the flexicurve instrument to evaluate the angles of thoracic and lumbar curvatures of the spine in the sagittal plane. Rehabil Res Pract 2012. 2012 doi: 10.1155/2012/186156. 186156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Babai E, Khodamoradi A, Mosavi Z, Bahari S. An innovative software method for measuring lumbar lordosis. Ann Biol Res. 2012;3:204–13. [Google Scholar]
- 18.López-Miñarro PA, Muyor JM, Belmonte F, Alacid F. Acute effects of hamstring stretching on sagittal spinal curvatures and pelvic tilt. J Hum Kinet. 2012;31:69–78. doi: 10.2478/v10078-012-0007-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willner S. Spinal pantograph – A non-invasive technique for describing kyphosis and lordosis in the thoraco-lumbar spine. Acta Orthop Scand. 1981;52:525–9. doi: 10.3109/17453678108992142. [DOI] [PubMed] [Google Scholar]
- 20.Macintyre NJ, Bennett L, Bonnyman AM, Stratford PW. Optimizing reliability of digital inclinometer and flexicurve ruler measures of spine curvatures in postmenopausal women with osteoporosis of the spine: An illustration of the use of generalizability theory. ISRN Rheumatol 2011. 2011 doi: 10.5402/2011/571698. 571698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hegazy AA, Hegazy RA. Midsagittal anatomy of lumbar lordosis in adult Egyptians: MRI study. Anat Res Int 2014. 2014 doi: 10.1155/2014/370852. 370852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lonstein JE. Patient evaluation. In: Lonstein JE, Bradford DS, Winter RB, Ogilve JW, editors. Moe's Textbook of Scoliosis and Other Disorders. 3rd ed. Philadelphia: W.B. Saunders; 1995. pp. 45–86. [Google Scholar]
- 23.Mosner EA, Bryan JM, Stull MA, Shippee R. A comparison of actual and apparent lumbar lordosis in black and white adult females. Spine (Phila Pa 1976) 1989;14:310–4. doi: 10.1097/00007632-198903000-00011. [DOI] [PubMed] [Google Scholar]
- 24.Propst-Proctor SL, Bleck EE. Radiographic determination of lordosis and kyphosis in normal and scoliotic children. J Pediatr Orthop. 1983;3:344–6. doi: 10.1097/01241398-198307000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Saraste H, Broström LA, Aparisi T, Axdorph G. Radiographic measurement of the lumbar spine. A clinical and experimental study in man. Spine (Phila Pa 1976) 1985;10:236–41. doi: 10.1097/00007632-198504000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Hicks GE, George SZ, Nevitt MA, Cauley JA, Vogt MT. Measurement of lumbar lordosis: Inter-rater reliability, minimum detectable change and longitudinal variation. J Spinal Disord Tech. 2006;19:501–6. doi: 10.1097/01.bsd.0000210116.94273.ad. [DOI] [PubMed] [Google Scholar]
- 27.Polly DW, Jr, Kilkelly FX, McHale KA, Asplund LM, Mulligan M, Chang AS, et al. Measurement of lumbar lordosis. Evaluation of intraobserver, interobserver, and technique variability. Spine (Phila Pa 1976) 1996;21:1530–5. doi: 10.1097/00007632-199607010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Vacari DA, Neves EB, Ulbricht L. Comparison between methods of assessing lumbosacral curve obtained by radiographic image. Acta Ortop Bras. 2015;23:67–71. doi: 10.1590/1413-78522015230200840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okpala FO. Normal pediatric lumbar lordosis: Measurement of magnitude and age of maximum development using three radiographic techniques. West Afr J Radiol. 2016;23:82–8. [Google Scholar]
- 30.Oliver J, Middleditch A. Functional Anatomy of the Spine. Oxford: Butterworth-Heinemann; 1998. Lumbar spine; pp. 36–58. [Google Scholar]
- 31.Hansson T, Bigos S, Beecher P, Wortley M. The lumbar lordosis in acute and chronic low-back pain. Spine (Phila Pa 1976) 1985;10:154–5. doi: 10.1097/00007632-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Murrie VL, Dixon AK, Hollingworth W, Wilson H, Doyle TA. Lumbar lordosis: Study of patients with and without low back pain. Clin Anat. 2003;16:144–7. doi: 10.1002/ca.10114. [DOI] [PubMed] [Google Scholar]
- 33.Bogduk N, Macintosh JE, Pearcy MJ. A universal model of the lumbar back muscles in the upright position. Spine (Phila Pa 1976) 1992;17:897–913. doi: 10.1097/00007632-199208000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Okpala F. Measurement of lumbosacral angle in normal radiographs: A retrospective study in Southeast Nigeria. Ann Med Health Sci Res. 2014;4:757–62. doi: 10.4103/2141-9248.141548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hellems HK, Jr, Keats TE. Measurement of the normal lumbosacral angle. Am J Roentgenol Radium Ther Nucl Med. 1971;113:642–5. doi: 10.2214/ajr.113.4.642. [DOI] [PubMed] [Google Scholar]
- 36.Damasceno LH, Catarin SR, Campos AD, Defino HL. Lumbar lordosis: A study of angle values and of vertebral bodies and intervertebral discs role. Acta Ortop Bras. 2006;14:193–8. [Google Scholar]
- 37.Mitchell T, O’Sullivan PB, Burnett AF, Straker L, Smith A. Regional differences in lumbar spinal posture and the influence of low back pain. BMC Musculoskelet Disord. 2008;9:152. doi: 10.1186/1471-2474-9-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stagnara P, De Mauroy JC, Dran G, Gonon GP, Costanzo G, Dimnet J, et al. Reciprocal angulation of vertebral bodies in a sagittal plane: Approach to references for the evaluation of kyphosis and lordosis. Spine (Phila Pa 1976) 1982;7:335–42. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Vedantam R, Lenke LG, Keeney JA, Bridwell KH. Comparison of standing sagittal spinal alignment in asymptomatic adolescents and adults. Spine (Phila Pa 1976) 1998;23:211–5. doi: 10.1097/00007632-199801150-00012. [DOI] [PubMed] [Google Scholar]
- 40.Physiopedia. Lumbosacral Biomechanics. [Last accessed on 2017 Oct 30]. Available from: http://www.physio-pedia.com/Lumbosacral_Biomechanics .
- 41.Andersson GB, Murphy RW, Ortengren R, Nachemson AL. The influence of backrest inclination and lumbar support on lumbar lordosis. Spine (Phila Pa 1976) 1979;4:52–8. doi: 10.1097/00007632-197901000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Frymoyer JW, Newberg A, Pope MH, Wilder DG, Clements J, MacPherson B, et al. Spine radiographs in patients with low-back pain. An epidemiological study in men. J Bone Joint Surg Am. 1984;66:1048–55. [PubMed] [Google Scholar]


