Abstract
Objectives. To assess the relationship between health care system and economic factors and early childhood caries (ECC) data availability and prevalence.
Methods. We estimated ECC data for 193 United Nations countries from studies published between 2007 and 2017. We obtained other variables from the World Health Organization and the World Bank databases. We assessed association with ECC data availability by using logistic regression and with ECC prevalence by using linear regression.
Results. We included 190 publications from 88 (45.6%) countries. The mean ECC prevalence was 23.8% and 57.3% in children younger than 36 months and children aged 36 to 71 months, respectively. The odds of ECC data availability were significantly higher for countries with more physicians and more dentists. In children younger than 36 months, ECC prevalence was associated with universal health coverage (B = −6.56). In children aged 36 to 71 months, it was associated with growth of gross national income (B = 0.27).
Conclusions. Countries with more physicians and more dentists were more likely to have ECC data. Among those with data, countries with higher economic growth had higher ECC prevalence.
Early childhood caries (ECC) is a global epidemic, affecting the quality of life of young children and their families1 with effects on growth and development2 in addition to an economic burden caused by the need for oral rehabilitation under general anesthesia.3 It requires attention to interrelated multiple etiological factors at the micro (family), meso (organizations such as schools), exo (community norms), and macro (national and cultural systems) levels.4,5
Most studies on ECC identify risk factors at the micro and meso levels. These include oral health behaviors of children shaped by their personality and close family members, friends, or other social contacts.6 The social–ecological model explaining ECC posits that exo- and macro-level factors also affect caries risk in children.5
Few studies have investigated the impact of macro (country)–level factors on caries prevalence in adults.7,8 In children, a study assessed the association of wealth, dentist availability, sugar availability, and toothpaste sales with the oral health of 12-year-old children in 29 European countries.9 Another study assessed the impact of income and inequality on the association of sugar consumption and caries experience measured by the number of decayed, missing, and filled teeth in 12-year-old children in 73 countries.10 Only 1 study was found to address the association between ECC and income inequalities in 22 rich countries.11
National health care systems—a macro-level factor—can affect ECC prevalence4,12 by having an impact on access to preventive and curative care.13 The distribution of health professionals14 and the availability of health-related data give insight about the performance of national health care systems.8,12 When data are available, health problems can be more readily addressed. For example, the World Health Organization (WHO) provided access to information on dentists’ numbers, and this improved countries’ investment in workforce planning to meet oral health needs.15 Data on ECC are sparse16 limiting analysis and prescription for policy formulation, program design, and implementation to address ECC problems at country and global levels.
We aimed to identify the macro-level factors associated with ECC data availability and prevalence. Specifically, we assessed how determinants including the number of dentists per 1000 population, number of physicians per 1000 population, universal health coverage (UHC), growth in per-capita gross national income (GNI), and per-capita health expenditure are associated with (1) availability of country data on ECC and (2) prevalence of ECC.
METHODS
We collected macro-level data covering the period January 2007 to October 2017 for 193 member states of the United Nations.17
Data Sources
Early childhood caries prevalence.
For each country, we extracted data on ECC prevalence from the WHO Country Oral Health Profile database.16 We also searched other databases—MEDLINE, Web of Science, Scopus, and Google Scholar (first 100 search results)—by using a country’s name combined with “caries” or “dental decay.” We complemented this by searching master’s and doctoral degree theses about ECC, articles published in local journals, and government reports.18 We applied no language filter.
We included studies if they (1) were conducted on humans in an epidemiological, nonlaboratory setting; (2) assessed ECC (defined as the presence of 1 or more decayed, missing, or filled tooth surface in any primary tooth in a child aged 71 months or younger)19 or data were available to allow its estimation; and (3) included healthy children. Excluded studies were (1) duplicates such as theses and resulting publications, (2) publications from which needed information could not be extracted (article with no full text or information not mentioned), and (3) studies published before 2007.
After these exclusions, 190 publications on ECC from 88 countries (45.6% of the UN member states) were available (Appendix, Table A, available as a supplement to the online version of this article at http://www.ajph.org). We extracted data from studies reporting prevalence figures from nationally representative samples if they were available (n = 25; Appendix). Otherwise, we used the retrieved data to calculate ECC prevalence for a country by dividing the total number of children affected by ECC in the study or studies by the total number of children examined and multiplying by 100.
Population characteristics.
We obtained the numbers of children younger than 36 months and children aged 36 to 71 months in each country from the World Bank Databank by using the 2015 estimates.20 We obtained the number of dentists per 1000 population and the number of physicians per 1000 population from the WHO Global Health Observatory data repository updated in February 2017.21
Country characteristics.
We assessed the UHC status of each country according to the definition by Feigl and Ding22 including (1) the presence of laws ordaining that all citizens in the country have access to a core set of health care services, (2) 85% or more of the population have formal health coverage, (3) 90% or more have access to skilled health care workers’ attendance at birth, and (4) 25% or less of the total health expenditure is out-of-pocket payment, thereby ensuring financial risk protection.
Gross national income is the sum of value added by all resident producers plus any product taxes (less subsidies) not included in the valuation of output plus net receipts of primary income (compensation of employees and property income) from abroad. This was converted to international dollars based on purchasing power parity to allow across-country comparisons. An international dollar has the same purchasing power as a US dollar in the United States. We obtained data on per-capita GNI between 2006 and 2016 (latest available) from the World Bank Databank.23
Per-capita health expenditure is the sum of public and private health expenditures as a ratio of total population. It covers the provision of health services (preventive and curative), family planning activities, nutrition activities, and emergency aid designated for health. We obtained data for 2006 and 2014 (the latest available) from the World Bank Databank.24
Analysis
The outcome variables were (1) global ECC data availability and (2) ECC prevalence for children younger than 36 months and children aged 36 to 71 months. This cut-off point for age was in line with children’s categorization by the American Academy of Pediatrics.25 We assessed the health care system and economic factors associated with these 2 outcome variables.
We categorized the UN member states on the basis of ECC data availability into countries with (1) no data, (2) outdated data (data available before 2007), and (3) countries with data available from 2007 to 2017. For each category, we calculated the number and percentages of countries and child population.
We categorized the UN member states into countries with ECC prevalence of (1) 0% to 25%, (2) 26% to 50%, (3) 51% to 75%, and (4) 76% to 100%. We used ArcGIS (Esri, Redlands, CA), a geographic information system for working with maps and geographic information, to map the global ECC distribution. We calculated the number and percentages of countries and children affected by ECC in each category (estimated child population in a country in this age group multiplied by the prevalence).
The health care system factors were (1) number of physicians per 1000 population, (2) number of dentists per 1000 population, and (3) having UHC.
The economic factors were growth rate of per-capita GNI between 2006 and 2016 calculated as
 |
and growth rate of per-capita total health expenditure between 2006 and 2014 calculated as
 |
We categorized countries by the 2016 World Bank regions26 into
North America,
Latin America/Caribbean,
Europe/Central Asia,
Middle East/North Africa,
sub-Saharan Africa,
South Asia, and
East Asia/Pacific.
We reported ECC data availability and prevalence by regions.
We assessed the odds of a country having available ECC data (a binary, yes-or-no variable) for children younger than 36 months and children aged 36 to 71 months by using binary logistic regression univariate and multiple models. We determined the association between ECC prevalence (as a quantitative variable) for each age group and the independent variables by using univariate and multiple linear regression models. We calculated odds ratios (ORs), parameter estimates, 95% confidence intervals (CIs), and P values. We adjusted for whether the ECC prevalence estimates were obtained from representative samples by using national surveys. We calculated partial η squared as measure of effect size. We used SPSS version 22.0 (IBM, Somers, NY) for analysis. We considered P ≤ .05 statistically significant.
RESULTS
In the included studies, there were 68 031 children younger than 36 months and 154 452 children aged 36 to 71 months. Data were less available for children younger than 36 months: 141 countries (73.1% of UN member states) had no ECC data about their 133.7 million children of that age while 89 countries (46.1%) had no data about 55.9 million children aged 36 to 71 months (Appendix, Table B, available as a supplement to the online version of this article at http://www.ajph.org). The ECC data were least available in sub-Saharan Africa: only 4 (8.3%) of the 48 countries in this region had data for children younger than 36 months and 10 (20.8%) countries had data for children aged 36 to 71 months (Appendix, Figure A, available as a supplement to the online version of this article at http://www.ajph.org). National surveys of ECC were conducted in 25 (13.0%) countries.
The mean global physicians per 1000 population ratio was 1.6 (SD = 1.5) and the mean global dentists per 1000 population ratio was 0.3 (SD = 0.3) with 32 countries (12.8%) having UHC. The mean growth rate of per-capita GNI was 44.0 (SD = 28.7) and the mean growth rate of per-capita health expenditure was 53.6 (SD = 53.2). The growth in per capita GNI was moderately, negatively, and significantly correlated with per-capita GNI in 2006 (Pearson correlation coefficient = −0.39; P < .001).
Table 1 shows that the ORs of having ECC data for both age groups were significantly higher among countries with greater number of physicians (P = .01 and .002) and dentists (P = .005 and < .001). For children aged 36 to 71 months, countries with UHC had significantly higher ORs of data availability than countries without UHC (P = .004). In the multiple regression models, all variables lost significance. In addition, the ORs of some variables were reduced (UHC in the model of children younger than 36 months and UHC and dentists per 1000 population in the model of children aged 36 to 71 months).
TABLE 1—
Factors Associated With Global Early Childhood Caries Data Availability in Children Younger Than 36 Months and Aged 36 to 71 Months: 2007–2017
| Variables | Children Younger Than 36 Months (n = 39 Countries) | Children Aged 36–71 Months (n = 86 Countries) | ||
| UOR (95% CI) | AOR (95% CI) | UOR (95% CI) | AOR (95% CI) | |
| Health care system factors | ||||
| Physicians/1000 population | 1.33 (1.06, 1.66) | 1.24 (0.82, 1.86) | 1.39 (1.14, 1.71) | 1.33 (0.89, 1.99) |
| Dentists/1000 population | 3.96 (1.52, 10.35) | 4.07 (0.77, 21.50) | 5.55 (2.19, 14.06) | 3.95 (0.71, 22.00) |
| Has universal health coverage | 2.07 (0.89, 4.83) | 0.68 (0.24, 1.94) | 3.33 (1.48, 7.51) | 1.11 (0.39, 3.15) |
| Economic factors | ||||
| Growth in per capita GNI (2006–2015) | 1.00 (0.99, 1.02) | 1.00 (0.99, 1.02) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.02) |
| Growth in per capita health expenditure (2006–2014) | 1.00 (0.99, 1.01) | 1.00 (0.99, 1.01) | 1.00 (1.00, 1.01) | 1.01 (1.00, 1.01) |
Note. AOR = adjusted odds ratio; CI = confidence interval; GNI = gross national income; UOR = unadjusted odds ratio.
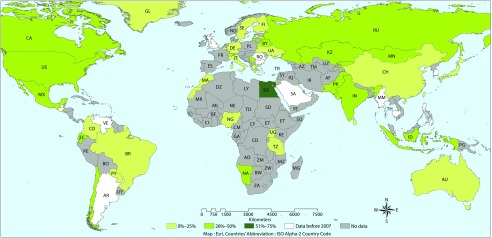
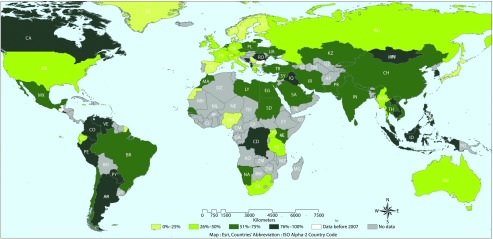
Figures 1 and 2 show the global prevalence of ECC in children younger than 36 months and children aged 36 to 71 months, respectively. The prevalence ranged from 0.3% to 69.6% and from 6.3% to 98.1%, respectively.
FIGURE 1—
Global Prevalence of Early Childhood Caries Among Children Younger Than 36 Months: 2007–2017
Note. ISO = International Organization for Standardization.
FIGURE 2—
Global Prevalence of Early Childhood Caries Among Children Aged 36 to 71 Months: 2007–2017
Note. ISO = International Organization for Standardization.
Among children younger than 36 months, the mean prevalence was highest in North America (31.7%) and South Asia (30%) and lowest in sub-Saharan Africa (14.3%; P = .86). For children aged 36 to 71 months, the mean prevalence was highest in East Asia/Pacific (68.7%) and Middle East/North Africa (66.2%) and lowest in Europe/Central Asia (43.9%; P = .004; Appendix, Figure B, available as a supplement to the online version of this article at http://www.ajph.org).
Between 2007 and 2017, an estimated 64.6 million children younger than 36 months were affected by ECC. In 1 country (Egypt), ECC prevalence ranged between 51% and 75%. The number of affected children aged 36 to 71 months was estimated to be 173.5 million. In this age group, 55 countries had caries prevalence greater than 50% with estimated 152.8 million children affected (88% of all affected children in this age group globally). The mean prevalence for children younger than 36 months was 23.8% (SD = 14.8%) and 57.3% (SD = 22.4%) for children aged 36 to 71 months (Appendix, Table C, available as a supplement to the online version of this article at http://www.ajph.org).
Table 2 shows that, among children younger than 36 months, none of the health care system factors was significantly associated with ECC prevalence, while among children aged 36 to 71 months an increase of 1 physician per 1000 population (P = .001) and the presence of UHC (P = .001) were significantly associated with lower ECC prevalence. One-percent growth in per-capita GNI and in per-capita health expenditure was associated with significantly higher prevalence in children aged 36 to 71 months (P = .002 and .02, respectively). In the multiple linear regression model for children younger than 36 months, none of the variables showed a significant association with ECC prevalence and the greatest effect size was calculated for UHC and growth in GNI (partial η squared = 0.04 and 0.03, respectively). The model, however, explained a minor portion of the variation in ECC prevalence (adjusted R2 = 0.03). For children aged 36 to 71 months, the only variable with significant association was growth in GNI (P = .01). This variable had the greatest effect size (partial η squared = 0.09), followed by the number of physicians per 1000 population and UHC (partial η squared = 0.05 and 0.04, respectively). The model explained 22% of the variation among countries in ECC prevalence (adjusted R2 = 0.22).
TABLE 2—
Economic and Health Care System Determinants of Global Early Childhood Caries Prevalence in Children Younger Than 36 Months and Aged 36 to 71 Months: 2007–2017
| Variables | Children Younger Than 36 Months | Children Aged 36–71 Months | ||||
| Univariate Model (n = 39), B (95% CI) | Multiple Model (n = 38), B (95% CI) | Partial η Squared | Univariate Model (n = 86), B (95% CI) | Multiple Model (n = 77), B (95% CI) | Partial η Squared | |
| Health care system factors | ||||||
| Physicians/1000 population | −1.09 (−4.53, 2.36) | 1.43 (−3.15, 6.01) | 0.01 | −5.93 (−9.26, −2.60) | −4.60 (−9.36, 0.17) | 0.05 |
| Dentists/1000 population | −7.99 (−19.57, 3.60) | −1.56 (−17.91, 14.79) | 0.001 | −13.16 (−26.79, 0.46) | 12.21 (−6.14, 30.56) | 0.03 |
| Has universal health coverage | −6.73 (−17.66, 4.20) | −6.56 (−19.11, 5.99) | 0.04 | −18.32 (−28.64, −8.00) | −9.94 (−22.15, 2.27) | 0.04 |
| Economic factors | ||||||
| Growth in per-capita GNI | 0.11 (−0.06, 0.28) | 0.16 (−0.18, 0.51) | 0.03 | 0.28 (0.11, 0.45) | 0.27 (0.06, 0.47) | 0.09 |
| Growth in per-capita health expenditure | 0.06 (−0.05, 0.18) | 0.05 (−0.13, 0.23) | 0.009 | 0.09 (0.01, 0.16) | 0.05 (−0.03, 0.13) | 0.02 |
| Model adjusted R2 | . . . | 0.03 | . . . | 0.22 | ||
Note. CI = confidence interval; GNI = gross national income. Multiple models are adjusted by whether there are national surveys providing representative samples or not: For children younger than 36 months, B = 1.58 (95% CI = −11.41, 14.57). For children aged 36–71 months, B = −5.92 (95% CI = −16.13, 4.28).
DISCUSSION
This study suggested that, during the past decade, most UN member states either did not have or had outdated ECC data, with no information about 40% of children younger than 36 months and 20% of children aged 36 to 71 months. Countries with higher densities of physicians and dentists were more likely to have ECC data. We found an indication that, among countries with recent ECC data, those with UHC were more likely to have lower ECC prevalence whereas those with higher growth rate of GNI were more likely to have higher prevalence. Our findings may help fill a knowledge gap by reporting on ECC data availability and prevalence in the UN member states for children younger than 36 months and children aged 36 to 71 months in 39 and 86 countries. This adds to the findings of the only previous report of global ECC11 among children aged 5 to 6 years from 48 countries. The present study is also the first to highlight the possible impact of macro-level factors on ECC for countries with various health care and economic profiles. This presents a call to action to control this disease and address its impact on the health and well-being of young children.
The results showed different patterns of ECC data availability by age with more data available for children aged 36 to 71 months. This is possibly because they can be more easily sampled and accessed. There were also age differences in ECC prevalence and associated determinants. We recommend that future studies address ECC questions separately for children younger than 36 months and those aged 36 months and older because combining both may obscure differences that are important for policy and program development.
We observed higher odds of having ECC data in countries with greater number of physicians and dentists. We also observed that dentists’ availability was associated with ECC prevalence and the effect size (partial η squared) was lower than that associated with physicians’ availability. The lower effect size for dentists’ availability is probably attributable to the lower global presence of dentists and the role physicians play in providing primary oral health care to preschool children when dentists are not adequately available.27 Also, the number of physicians may be an indicator of the quality and availability of health care reflecting better children’s health and reduced ECC prevalence.28 These results differ from previous studies reporting on older children. For example, Downer et al.9 reported a weak, negative nonsignificant correlation (ρ = −0.082) between population per active dentist and decayed, missing, and filled teeth among 12-year-old children in European countries. Pinilla and Gonzalez,14 on the other hand, reported no correlation between decayed, missing, and filled teeth of 12-year-old children and dentists’ number in European countries.
This study provided initial evidence on the influence UHC may have on ECC prevalence, especially in children aged 36 to 71 months. It may be because countries with UHC also implement oral health policies allowing preschool children to access preventive oral care. This agrees with a previous observation that health care systems and the services they provide may be related to differences in oral diseases profile among countries.29 However, it was reported that dental services availability in the public health sector was not associated with reduction in caries prevalence in children.14 In addition, previous studies concluded that UHC offering generous care may lead individuals to engage in risky health behaviors thereby increasing the odds of disease or its severity.30 Not all countries providing UHC include oral health care in their package14 so that the presence of UHC may be more indicative of strategies for care delivery by allocating resources rather than greater focus on dental care. This may explain the negative association between ECC data availability and UHC in younger children in the multiple regression model. Therefore, further studies are needed to explain this association.
Our results suggest that countries with greater economic growth had higher ECC prevalence. This observation may be the result of a “harvesting” phenomenon in which improved economy makes it possible to generate more ECC data. The association may alternatively be explained by the negative correlation between GNI growth rate and GNI in 2006 so that more growth occurred in less-affluent countries. This observed direct association between GNI growth and ECC prevalence may reflect greater exposure of growing economies to risk factors that may not have been matched with concomitant institution of preventive measures and practices.31 Our results are indirectly supported by previous studies that measured economic condition at 1 time point rather than measuring change in economic status over time like we did. For example, Bernabé and Hobdell11 demonstrated lower oral diseases in countries with better economies. Pinilla and Gonzalez14 also reported lower decayed, missing, and filled teeth among 12-year-old children in countries with higher gross national product (coefficient = −0.05) and Bernabé et al.7 reported negative correlation between the number of decayed teeth and GNI (coefficient = −0.26) among 12-year-old children.
Limitations
This study had some limitations. First, by following the American Academy of Pediatric Dentistry’s definition of ECC, we minimized variation attributable to different diagnostic criteria. However, we had no control over data quality and in-country geographic coverage. In some cases, data from localized areas were used to represent a country. In other cases, country estimates could have been based on populations with higher caries risk increasing the possibility for overestimation of ECC prevalence. However, we adjusted for the presence of nationally representative data in multiple regression, and its impact on the conclusions is thus accounted for. These limitations were reported by other investigators.9 In addition, a similar approach is used in the WHO database where oral diseases’ estimates may be derived from samples that are not nationally representative.16 Data limitations also reduced sample size. This may have affected the power of the regression models to detect significant associations, especially if they were of small effect size. We tried to address this by calculating partial η squared as a measure of effect size to show the relative strength of various factors in each model. Partial η squared, however, has limited use for comparison with other studies that might have used other combinations of explanatory variables measured differently.
Second, data were collected at different levels. For example, dentist-to-population ratio, physician-to-population ratio, GNI, and health expenditure were calculated for the whole country whereas ECC data were based on samples of children aged 71 months or younger.9,11 This ecological fallacy may affect interpretation. It is a trade-off for the macro-level insights this kind of study offers.
Third, we used the latest available data and tried to match the time of data whenever possible. However, we appreciate that temporal differences were unavoidable and might have had an impact on the observed association depending on the magnitude of change expected to occur by time in these factors.
Fourth, we considered the number of physicians to the population and the number of dentists to the population. These are rough estimates of professionals’ availability that do not take into account differences in specialties, productivity, and administrative versus geographic scope. We also did not include other professionals who, in some countries, may provide care to children such as dental hygienists and therapists. Nevertheless, these factors were used in similar studies.9,14,15 Finally, the impact of other confounding factors on ECC was not assessed because of data availability constraints. Factors such as oral hygiene, dietary practices, and infant feeding practices need to be considered in future studies.
Public Health Implications
This study highlights the need for global action to support growing economies to reduce ECC risk. This includes help for periodic systematic data collection on ECC using standardized methods in regions that lack data altogether, such as sub-Saharan Africa. It is important to use an upstream approach by addressing factors that are closely associated with ECC causation and at the same time address existing treatment needs of affected children so that their development is not jeopardized. Optimal resources allocation is needed to address the limited availability of financial, human, and infrastructural capacity in countries worst affected by ECC such as those in East Asia and the Pacific and those in Latin America and the Caribbean. Global discussion among professional associations, academicians, policymakers, and community leaders supported by evidence and sharing of experience will help set a global agenda to address these challenges. This helps achieve the targets of the third sustainable development goal of the United Nations, to ensure healthy lives through UHC, increasing the recruitment and retention of health workforce, and strengthening the capacity to manage health risks, especially in developing countries.32
HUMAN PARTICIPANT PROTECTION
No institutional review board approval was needed because publicly available, de-identified data were involved.
Footnotes
See also Tschampl, p. 980.
REFERENCES
- 1.Martins MT, Sardenberg F, Bendo CB et al. Dental caries remains as the main oral condition with the greatest impact on children’s quality of life. PLoS One. 2017;12(10):e0185365. doi: 10.1371/journal.pone.0185365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moimaz SA, Borges HC, Saliba O et al. Early childhood caries: epidemiology, severity and sociobehavioural determinants. Oral Health Prev Dent. 2016;14:77–83. doi: 10.3290/j.ohpd.a34997. [DOI] [PubMed] [Google Scholar]
- 3.Phantumvanit P, Makino Y, Ogawa H et al. WHO global consultation on public health intervention against early childhood caries. Community Dent Oral Epidemiol. 2018;46(3):280–287. doi: 10.1111/cdoe.12362. [DOI] [PubMed] [Google Scholar]
- 4.Newton JT, Bower EJ. The social determinants of oral health: new approaches to conceptualizing and researching complex causal networks. Community Dent Oral Epidemiol. 2005;33(1):25–34. doi: 10.1111/j.1600-0528.2004.00190.x. [DOI] [PubMed] [Google Scholar]
- 5.Folayan MO, Chukwumah NM, Onyejaka N et al. Appraisal of the national response to the caries epidemic in children in Nigeria. BMC Oral Health. 2014;14(1):76. doi: 10.1186/1472-6831-14-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris R, Nicoll AD, Adair PM et al. Risk factors for dental caries in young children: a systematic review of the literature. Community Dent Health. 2004;21(1 suppl):71–85. [PubMed] [Google Scholar]
- 7.Bernabé E, Sheiham A, Sabbah W. Income, income inequality, dental caries and dental care levels: an ecological study in rich countries. Caries Res. 2009;43(4):294–301. doi: 10.1159/000217862. [DOI] [PubMed] [Google Scholar]
- 8.Guarnizo-Herreño CC, Watt RG, Stafford M et al. Do welfare regimes matter for oral health? A multilevel analysis of European countries. Health Place. 2017;46:65–72. doi: 10.1016/j.healthplace.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Downer MC, Drugan CS, Blinkhorn AS. Correlates of dental caries in 12-year-old children in Europe: a cross-sectional analysis. Community Dent Health. 2008;25(2):70–78. [PubMed] [Google Scholar]
- 10.Masood M, Masood Y, Newton T. Impact of national income and inequality on sugar and caries relationship. Caries Res. 2012;46(6):581–588. doi: 10.1159/000342170. [DOI] [PubMed] [Google Scholar]
- 11.Bernabé E, Hobdell MH. Is income inequality related to childhood dental caries in rich countries? J Am Dent Assoc. 2010;141(2):143–149. doi: 10.14219/jada.archive.2010.0131. [DOI] [PubMed] [Google Scholar]
- 12.Palència L, Espelt A, Cornejo-Ovalle M et al. Socioeconomic inequalities in the use of dental care services in Europe: what is the role of public coverage? Community Dent Oral Epidemiol. 2014;42(2):97–105. doi: 10.1111/cdoe.12056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Casamassimo PS, Thikkurissy S, Edelstein BL et al. Beyond the dmft: the human and economic cost of early childhood caries. J Am Dent Assoc. 2009;140(6):650–657. doi: 10.14219/jada.archive.2009.0250. [DOI] [PubMed] [Google Scholar]
- 14.Pinilla J, Gonzalez B. Exploring changes in dental workforce, dental care utilisation and dental caries levels in Europe, 1990–2004. Int Dent J. 2009;59(2):87–95. [PubMed] [Google Scholar]
- 15.Jakovljevic M, Kanjevac TV, Lazarevic M et al. Long term dental work force build-up and DMFT-12 improvement in the European region. Front Physiol. 2016;7:48. doi: 10.3389/fphys.2016.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malmo University. Oral health database. Country oral health profiles: alphabetical order. 2017. Available at: http://www.mah.se/CAPP/Country-Oral-Health-Profiles/According-to-Alphabetical/?id=41424. Accessed October 29, 2017.
- 17.United Nations. Member states. 2017. Available at: http://www.un.org/en/member-states. Accessed November 1, 2017.
- 18.Folayan MO. A Compendium on Oral Health of Children Around the World: Early Childhood Caries. Hauppauge, NY: NOVA Science Publishers; 2018. [Google Scholar]
- 19.American Academy of Pediatric Dentistry. Definition of early childhood caries. 2008. Available at: http://www.aapd.org/assets/1/7/d_ecc.pdf. Accessed October 22, 2017.
- 20.The World Bank. Data. Population estimates and projections. 2017. Available at: http://databank.worldbank.org/data/reports.aspx?source=Health%20Nutrition%20and%20Population%20Statistics:%20Population%20estimates%20and%20projections#. Accessed October 28, 2017.
- 21.World Health Organization. Global Health Observatory data repository: Density per 1000; data by country. 2017. Available at: http://apps.who.int/gho/data/view.main.92100. Accessed October 28, 2017.
- 22.Feigl AB, Ding EL. Evidenced Formal Coverage Index and universal healthcare enactment: a prospective longitudinal study of economic, social, and political predictors of 194 countries. Health Policy. 2013;113(1-2):50–60. doi: 10.1016/j.healthpol.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 23.The World Bank. Data. GNI per capita, PPP (current international $). 2017. Available at: https://data.worldbank.org/indicator/NY.GNP.PCAP.PP.CD. Accessed October 28, 2017.
- 24.The World Bank. Data. Health expenditure per capita, PPP. 2017. Available at: https://datamarket.com/data/set/15n0/health-expenditure-per-capita-ppp-constant-2011-international#!ds=15n0!hnn=5u&display=line. Accessed November 1, 2017.
- 25.American Academy of Pediatrics. Ages & stages. 2017. Available at: https://www.healthychildren.org/English/ages-stages/Pages/default.aspx. Accessed October 22, 2017.
- 26.The World Bank. Data. World Bank list of economies June 2017. Available at: http://databank.worldbank.org/data/download/site-content/CLASS.xls. Accessed October 29, 2017.
- 27.Herndon JB, Tomar SL, Catalanotto FA. Effect of training pediatricians and family physicians in early childhood caries prevention. J Pediatr. 2015;166(4):1055–1061.e1. doi: 10.1016/j.jpeds.2014.12.040. [DOI] [PubMed] [Google Scholar]
- 28.Twetman S. Dental caries and general health in children and adults. In: Lynge Pedersen A, editor. Oral Infections and General Health. Cham, Switzerland: Springer; 2015. [Google Scholar]
- 29.Petersen PE. World Health Organization global policy for improvement of oral health—World Health Assembly 2007. Int Dent J. 2008;58(3):115–121. doi: 10.1111/j.1875-595x.2008.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 30.Kino S, Bernabé E, Sabbah W. The role of healthcare and education systems in co-occurrence of health risk behaviours in 27 European countries. Eur J Public Health. 2018;28(1):186–192. doi: 10.1093/eurpub/ckx071. [DOI] [PubMed] [Google Scholar]
- 31.Burt B, Eklund S. Dentistry, Dental Practice and the Community. 6th ed. St Louis, MO: Elsevier Saunders; 2005. [Google Scholar]
- 32.United Nations. Sustainable Development Goals—Goal 3: Good health and well-being. 2017. Available at: http://www.un.org/sustainabledevelopment/health. Accessed March 2, 2018.