Abstract
Objectives. To examine whether subsidized housing, specifically public housing and rental assistance, is associated with asthma in the Boston, Massachusetts, adult population.
Methods. We analyzed a pooled cross-sectional sample of 9554 adults taking part in 3 Boston Behavioral Risk Factor Surveillance System surveys from 2010 to 2015. We estimated odds ratios for current asthma in association with housing status (public housing development [PHD] resident, rental assistance [RA] renter, non-RA renter, nonrenter nonowner, homeowner as reference) in logistic regression analyses adjusting for year, age, sex, race/ethnicity, education, and income.
Results. The odds of current asthma were 2.02 (95% confidence interval [CI] = 1.35, 3.03) and 2.34 (95% CI = 1.60, 3.44) times higher among PHD residents and RA renters, respectively, than among homeowners. We observed smoking-related effect modification (interaction P = .04); elevated associations for PHD residents and RA renters remained statistically significant (P < .05) only among ever smokers. Associations for PHD residents and RA renters remained consistent in magnitude in comparison with non-RA renters who were eligible for subsidized housing according to income.
Conclusions. Public housing and rental assistance were strongly associated with asthma in this large cross-sectional sample of adult Boston residents.
The population burden of asthma in the United States is significant, with the total economic cost of asthma, including costs incurred through absenteeism and mortality, estimated at $81.9 billion in 2013.1 The asthma prevalence among US adults is approximately 9%2 and is higher among individuals with lower educational attainment and household incomes; in comparison with non-Latino Whites, the prevalence is higher among Blacks and lower among Latinos.3 The adult asthma prevalence in the city of Boston, Massachusetts (12%) is higher than the nationwide estimate, and, similar to the situation in the United States overall, it is correlated with lower educational attainment and household income.4 However, the adult asthma prevalence in Boston is higher among both non-Latino Black and Latino residents than among non-Latino White residents.4
Housing is also an important social determinant of asthma,5 and its association with asthma is thought to be mediated by environmental and social stressors affecting housing quality5 and housing stability.6 Substandard indoor environmental quality in home and school settings (including excessive dampness, mold and fungus, pet dander, pest and rodent infestation, secondhand tobacco smoke [SHS], and poor ventilation) is associated with asthma-related outcomes.7–14 Less is known about the association between asthma and housing stability factors, including housing cost, housing tenure, perceived lack of housing control, and residential instability.6
Public housing is frequently linked to poorer indoor housing quality,10,11,15–17 and there is moderate evidence supporting the association between poor indoor housing quality in public housing and asthma-related outcomes.9–11,18–20 However, few population-based studies have assessed whether subsidized housing itself, of which major types include public housing and rental assistance (both tenant based and project based), is associated with overall health or with asthma specifically.10,21,22 Variations between subsidized housing programs in how housing is maintained or how assistance is administered may result in differences in housing quality and stability.
Public housing developments (PHDs) are owned and managed by public housing authorities and provide rental assistance for low-income families. Tenant-based rental assistance allows low-income families to use vouchers to help pay for housing in the private market, and, unlike project-based rental assistance tied to a specific privately owned property, the voucher stays with the tenant. In a previous cross-sectional analysis of 2919 adults participating in the 2001 and 2003 Boston Behavioral Risk Factor Surveillance System (Boston BRFSS) surveys, reports of living in public housing or receiving rental assistance (relative to not living in such housing or receiving assistance) were associated with current asthma (odds ratio [OR] = 1.57; 95% confidence interval [CI] = 0.92, 2.65)21; however, the authors did not examine public housing and rental assistance associations separately.
In our study, we used data from 3 Boston BRFSS surveys conducted between 2010 and 2015 to examine associations between housing status and lifetime and current asthma among PHD residents, renters receiving rental assistance (RA renters), renters not receiving rental assistance (non-RA renters), and adults who neither rent nor own (the nonrenter nonowner group); our comparison group was homeowners. In addition, we restricted our analyses to adults meeting household income eligibility criteria for subsidized housing.
METHODS
In this cross-sectional study, we gathered data from a modified version of the BRFSS survey administered in Boston. The BRFSS survey is an annual random-digit-dial household telephone survey that collects information on health-related behaviors and conditions among noninstitutionalized adults (aged 18 years or older) residing in the United States. It is undertaken by state health departments in collaboration with the US Centers for Disease Control and Prevention (details on the methodology used in each survey year are available from the Centers for Disease Control and Prevention).23
The Boston Public Health Commission conducted the Boston BRFSS survey (which is administered in English and Spanish) biennially in odd years from 1999 through 2005, in even years from 2006 through 2010, and then in odd years beginning in 2013. The sample size ranges approximately from 1400 to 4000 respondents per survey year. As with the nationwide BRFSS survey, the Boston survey methodology involves stratified random sampling with a probability of selection related to the number of adults and telephone lines in a given household. One adult from each eligible household contacted is randomly selected for an interview. In the 2010, 2013, and 2015 study years, respectively, 9%, 39%, and 36% of the sample consisted of households with only cell phones. We poststratified our data to age, sex, race/ethnicity, education, and marital status population parameters for Boston, and we subsequently scaled the data to produce weighting proportionate to population size across years.
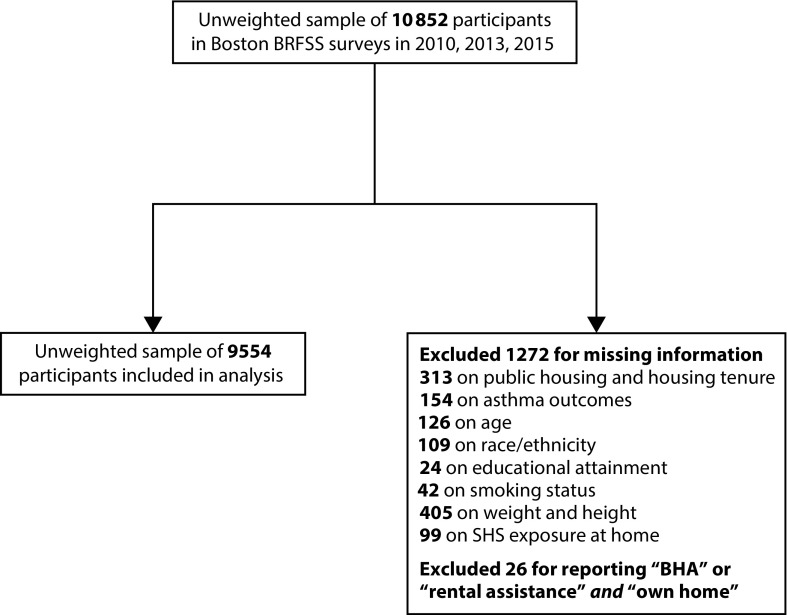
Beginning in 2001, a single question was included in the Boston survey indicating public housing status, and a single question involving housing tenure was introduced in 2010. In our analyses, we included a pooled cross-sectional unweighted sample of 9554 individuals who participated in the Boston BRFSS 2010 to 2015 surveys (88% of the 10 852 participants in these surveys) and had complete information on public housing status, housing tenure, asthma, and covariates of interest (Figure 1).
FIGURE 1—
Study Participation and Inclusion Flowchart: Boston, MA; Boston Behavioral Risk Factor Surveillance System (BRFSS); 2010–2015
Note. BHA = Boston Housing Authority; SHS = secondhand tobacco smoke.
Assessment of Asthma, Housing Status, and Covariates
Lifetime asthma was defined as a positive response to the following question: “Have you ever been told by a doctor, nurse, or health professional that you had asthma?” Among those classified as having a history of asthma, current asthma was defined as a positive response to the question “Do you still have asthma?”
Participants provided demographic information on age, sex, race/ethnicity, highest educational attainment, and household income. Information was also collected on weight and height, cigarette smoking, and SHS exposure at home (additional descriptions of these variables are provided in the Appendix, available as a supplement to the online version of this article at http://www.ajph.org).
Public housing status was ascertained from the following question: “Are you (1) a public housing resident living in a building owned by the Boston Housing Authority, (2) part of a household that receives rental assistance such as Section 8 or any other rental assistance program, or (3) neither of the above?” Housing tenure was ascertained from the question “Do you (1) own or (2) rent your home, or (3) have some other arrangement?” We combined the responses to the 2 questions and constructed a modified housing status variable with the following categories: PHD resident, RA renter, non-RA renter, nonrenter nonowner, and home owner.
Participants who responded “have some other arrangement” for housing tenure were classified in the nonrenter nonowner category independent of their response with respect to public housing status. Thus, participants classified as PHD residents and RA renters reported “public housing resident” and “receiving rental assistance” for public housing status, respectively, and reported “rent your home” for housing tenure. Non-RA renters reported “neither of the above” and “rent your home” for public housing status and housing tenure status, respectively. Participants classified as homeowners reported “own” and “neither of the above” for housing tenure and public housing status, respectively. Owing to small sample sizes, participants who reported their public housing status as “public housing resident” (unweighted n = 9) or “receiving rental assistance” (unweighted n = 11) and their housing tenure status as “own” were excluded from our analyses.
Statistical Analysis
We used SAS version 9.2 (SAS Institute Inc., Cary, NC) in conducting all of our analyses. All statistical procedures involved a design-based approach accounting for the disproportionate probability of selection among survey respondents and subsequent poststratification to Boston’s noninstitutionalized adult population. Logistic regression (PROC SURVEYLOGISTIC) was used to estimate odds ratios (and 95% confidence intervals) for lifetime and current asthma in association with housing status (PHD resident, RA renter, non-RA renter, nonrenter nonowner, homeowner as reference).
Logistic regression models included adjustment for the following covariates: survey year, age (35–54 years, 55 years or older, 18–34 years as reference), sex (male as reference), race/ethnicity (non-Latino Black, Latino, other, non-Latino White as reference), highest educational attainment (high school, some college, college or above, less than high school as reference), and household income (less than $20 000, $20 000–$34 999, missing, $35 000 or above as reference). In separate models, we also adjusted for smoking status (current, former, never as reference), obesity status (body mass index of 30 kg/m2 or above, body mass index less than 30 kg/m2 as reference), and extent of SHS exposure at home (1 or more hours per week, less than 1 hour or 0 hours as reference).
The percentages of missing values for the primary variables in our analysis ranged from 0.2% (educational attainment) to 3.7% (weight and height combined). In all of our logistic regression models, we used Taylor series variance estimation to accommodate the stratified design and conservatively treated missing responses as not missing completely at random by invoking the SAS NOMCAR option.
We assessed the overall presence of effect modification in the association between housing status and current asthma according to age (18–34 years, 35 years or older), smoking status (ever, never), and obesity status (obese, not obese) by including an interaction term between housing status and the modifying variable in the model; we set the significance level for interaction terms at P < .05. In addition, we conducted a domain analysis in which we calculated odds ratios and 95% confidence intervals for the associations between housing status and current asthma in subpopulations defined by age, smoking status, and obesity status. Among those in the nonrenter nonowner category, small samples in some of the variable groupings (i.e., sex, educational attainment, race/ethnicity, household income) prohibited domain analyses for these variables.
Secondary Analyses
We also adjusted our logistic regression models for proxies of health care access, specifically inability to see a doctor in the preceding 12 months because of cost (no such inability as reference), number of personal health care providers (0, 1 or more as reference), and routine check-up with a doctor in the preceding year (no check-up as reference). In an effort to compare PHD residents and RA renters with a group more sociodemographically similar than homeowners, we repeated our logistic regression models with non-RA renters as the reference group; we further restricted these logistic regression models to subpopulations in lower household income and educational attainment categories. Those in the lower household income categories met the family income criteria for most (less than $35 000) if not all (less than $20 000) public housing and RA programs offered by the Boston Housing Authority.
The distributions of the demographic characteristics of PHD residents, RA renters, and non-RA renters included in the restricted analyses are summarized in Tables A through C (available as supplements to the online version of this article at http://www.ajph.org). Adults in all housing categories were included in the model restricted to those reporting household incomes below $35 000; however, because of insufficient sample sizes, homeowners and those in the nonrenter nonowner group were excluded from the model restricted to those reporting household incomes below $20 000. Additional details about the methodology used in the secondary analyses are provided in the appendix.
RESULTS
The weighted prevalence of lifetime asthma among Boston adults was 17.9%, and the weighted prevalence of current asthma was 11.4% (Table 1). The prevalence of current asthma was approximately 2-fold higher among PHD residents (17.8%) and RA renters (21.7%) than among homeowners (9.1%). In comparison with homeowners, PHD residents and RA renters were more likely to be 18 to 34 years old, non-Latino Black or Latino, current smokers, and obese; also, their highest educational attainment was more likely to be high school or lower, their household income was more likely to be less than $20 000, and they were more likely to have experienced SHS exposure at home.
TABLE 1—
Weighted Prevalence of Selected Population Characteristics Among Boston Adult Residents, by Housing Status: Boston, MA; Boston Behavioral Risk Factor Surveillance System; 2010–2015
| Characteristic | PHD Resident (n = 668), % (95% CI) | RA Renter (n = 829), % (95% CI) | Non-RA Renter (n = 2690), % (95% CI) | Nonrenter Nonowner (n = 412), % (95% CI) | Homeowner (n = 4955), % (95% CI) |
| Asthma | |||||
| Lifetime | 23.3 (18.9, 27.7) | 28.3 (23.4, 33.2) | 16.3 (14.2, 18.4) | 23.4 (17.5, 29.3) | 15.0 (13.3, 16.6) |
| Current | 17.8 (13.9, 21.6) | 21.7 (17.4, 26.1) | 9.9 (8.3, 11.5) | 13.5 (8.8, 18.1) | 9.1 (7.7, 10.5) |
| Age, y | |||||
| 18–34 | 32.8 (27.0, 38.7) | 34.4 (28.9, 39.9) | 61.8 (59.4, 64.3) | 74.0 (69.1, 78.9) | 24.5 (22.1, 27.0) |
| 35–54 | 36.8 (31.6, 42.0) | 35.7 (30.9, 40.4) | 24.6 (22.6, 26.7) | 13.7 (10.1, 17.4) | 37.5 (35.5, 39.5) |
| ≥ 55 | 30.4 (25.8, 35.0) | 29.9 (25.9, 33.9) | 13.6 (12.2, 14.9) | 12.3 (9.0, 15.5) | 38.0 (36.1, 39.8) |
| Sex | |||||
| Male | 45.0 (39.4, 50.8) | 34.0 (28.9, 39.2) | 50.9 (48.1, 53.8) | 51.2 (44.5, 57.8) | 48.7 (46.6, 50.9) |
| Female | 55.0 (49.2, 60.5) | 66.0 (60.8, 71.1) | 49.1 (46.2, 51.9) | 48.8 (42.2, 55.5) | 51.3 (49.1, 53.4) |
| Race/ethnicity | |||||
| Non-Latino White | 18.8 (14.2, 23.4) | 19.1 (14.8, 23.3) | 52.0 (49.3, 54.8) | 41.1 (34.3, 48.0) | 68.2 (66.1, 70.2) |
| Non-Latino Black | 32.6 (27.7, 37.6) | 41.3 (36.4, 46.2) | 17.9 (16.2, 19.7) | 32.3 (26.5, 38.2) | 16.7 (15.3, 18.2) |
| Latino | 37.3 (32.2, 42.5) | 30.5 (25.7, 35.4) | 18.2 (16.2, 20.2) | 13.1 (9.3, 16.8) | 5.2 (4.3, 6.1) |
| Other | 11.3 (6.6, 16.0) | 9.1 (5.9, 12.3) | 11.8 (9.9, 13.8) | 13.5 (8.7, 18.3) | 9.9 (8.3, 11.5) |
| Educational attainment | |||||
| < high school | 35.1 (29.8, 40.4) | 29.6 (24.4, 34.8) | 12.2 (10.3, 14.1) | 16.1 (11.3, 20.8) | 5.2 (4.1, 6.3) |
| High school | 32.7 (27.6, 37.9) | 31.5 (26.7, 36.3) | 18.3 (16.2, 20.5) | 27.6 (21.6, 33.6) | 14.1 (12.6, 15.5) |
| Some college | 24.2 (19.3, 29.1) | 27.9 (23.6, 32.1) | 22.3 (20.0, 24.5) | 31.1 (24.7, 37.4) | 21.0 (19.2, 22.9) |
| ≥ college | 7.9 (5.1, 10.8) | 11.0 (8.3, 13.7) | 47.2 (44.4, 50.0) | 25.2 (19.5, 30.9) | 59.7 (57.6, 61.9) |
| Household income, $ | |||||
| < 20 000 | 54.1 (48.5, 59.6) | 51.5 (46.4, 56.6) | 19.3 (17.0, 21.5) | 25.1 (19.5, 30.8) | 4.6 (3.7, 5.4) |
| 20 000–34 999 | 21.1 (16.8, 25.4) | 26.9 (22.3, 31.4) | 21.1 (18.8, 23.4) | 19.1 (13.2, 25.0) | 9.3 (8.1, 10.5) |
| ≥ 35 000 | 9.6 (6.0, 13.2) | 10.8 (7.0, 14.6) | 49.1 (46.3, 51.9) | 32.5 (26.4, 38.7) | 77.4 (75.7, 79.2) |
| Missing | 15.2 (11.2, 19.2) | 10.8 (7.4, 14.3) | 10.5 (8.7, 12.3) | 23.2 (17.8, 28.6) | 8.7 (7.4, 9.9) |
| Smoking status | |||||
| Current smoker | 30.5 (25.1, 35.8) | 32.3 (26.9, 37.6) | 20.0 (17.6, 22.4) | 20.0 (14.8, 25.1) | 9.7 (8.3, 11.0) |
| Former smoker | 13.3 (10.2, 16.4) | 15.9 (12.9, 18.9) | 15.9 (14.1, 17.8) | 12.3 (7.5, 17.1) | 28.5 (26.7, 30.3) |
| Never smoker | 56.2 (50.7, 61.7) | 51.8 (46.6, 57.0) | 64.1 (61.4, 66.8) | 67.7 (61.4, 74.0) | 61.9 (59.8, 63.9) |
| Obesity status | |||||
| Obese | 30.7 (25.9, 35.5) | 35.2 (30.4, 40.0) | 18.2 (16.2, 20.2) | 23.5 (18.1, 28.9) | 20.0 (18.3, 21.6) |
| Not obese | 69.3 (64.5, 74.1) | 64.8 (60.0, 69.6) | 81.8 (79.8, 83.8) | 76.5 (71.1, 81.9) | 80.0 (78.4, 81.7) |
| SHS exposure at home | |||||
| Yes | 26.6 (21.4, 31.9) | 27.9 (22.7, 33.0) | 15.4 (13.4, 17.5) | 19.4 (13.9, 24.8) | 8.0 (6.6, 9.4) |
| No | 73.4 (68.1, 78.6) | 72.1 (67.0, 77.3) | 84.6 (82.5, 86.6) | 80.6 (75.2, 86.1) | 92.0 (90.6, 93.4) |
Note. CI = confidence interval; PHD = public housing development; RA = rental assistance; SHS = secondhand tobacco smoke. The sample size was n = 9954.
RA renters accounted for the highest proportion of women. Higher proportions of adults 18 to 34 years of age were observed among non-RA renters and those in the nonrenter nonowner group. In comparison with PHD residents and RA renters, non-RA renters and those in the nonrenter nonowner group were more likely to be younger, non-Latino White, college educated, and never smokers and to have household incomes above $35 000.
In the fully adjusted models, the odds of current asthma were 2.02 (95% CI = 1.35, 3.03) and 2.34 (95% CI = 1.60, 3.44) times higher among PHD residents and RA renters, respectively, than among homeowners (Table 2). No statistically significant (P < .05) associations with current asthma were observed among non-RA renters and those in the nonrenter nonowner group. The findings were similar for lifetime asthma. In comparison with the estimates from the fully adjusted model, the current asthma odds ratios for PHD residents and RA renters attenuated only slightly after additional adjustment for smoking status, obesity status, and SHS exposure at home. As shown in Table D (available as a supplement to the online version of this article at http://www.ajph.org), current smoking and former smoking were positively associated with current asthma, but the associations were not statistically significant. Current asthma was strongly associated with obesity (OR = 1.91; 95% CI = 1.55, 2.35), whereas no association was found for SHS exposure at home.
TABLE 2—
Associations Between Lifetime and Current Asthma and Housing Status: Boston, MA; Boston Behavioral Risk Factor Surveillance System; 2010–2015
| Asthma and Housing Status | Minimally Adjusted Model, OR (95% CI) | Fully Adjusted Model, OR (95% CI) | Fully Adjusted Model + Smoking, OR (95% CI) | Fully Adjusted Model + Obesity, OR (95% CI) | Fully Adjusted Model + SHS Exposure at Home, OR (95%CI) |
| Lifetime asthma | |||||
| PHD resident | 1.76 (1.30, 2.39) | 1.66 (1.18, 2.33) | 1.58 (1.12, 2.24) | 1.64 (1.17, 2.31) | 1.63 (1.15, 2.30) |
| RA renter | 2.15 (1.61, 2.88) | 2.01 (1.46, 2.78) | 1.88 (1.36, 2.59) | 1.95 (1.41, 2.69) | 1.97 (1.43, 2.72) |
| Non-RA renter | 0.98 (0.78, 1.22) | 0.94 (0.75, 1.19) | 0.92 (0.73, 1.16) | 0.95 (0.75, 1.19) | 0.94 (0.74, 1.18) |
| Nonrenter nonowner | 1.44 (0.98, 2.11) | 1.41 (0.96, 2.09) | 1.40 (0.95, 2.08) | 1.39 (0.94, 2.06) | 1.41 (0.95, 2.09) |
| Home owner (ref) | 1 | 1 | 1 | 1 | 1 |
| Current asthma | |||||
| Housing status | |||||
| PHD resident | 2.16 (1.53, 3.06) | 2.02 (1.35, 3.03) | 1.95 (1.30, 2.92) | 1.99 (1.33, 2.98) | 2.01 (1.30, 3.01) |
| RA renter | 2.50 (1.80, 3.48) | 2.34 (1.60, 3.44) | 2.23 (1.52, 3.26) | 2.25 (1.53, 3.32) | 2.33 (1.58, 3.41) |
| Non-RA renter | 1.06 (0.80, 1.41) | 1.03 (0.76, 1.40) | 1.01 (0.74, 1.38) | 1.03 (0.76, 1.40) | 1.03 (0.76, 1.39) |
| Nonrenter nonowner | 1.48 (0.93, 2.37) | 1.43 (0.87, 2.35) | 1.42 (0.87, 2.33) | 1.39 (0.86, 2.27) | 1.43 (0.87, 2.35) |
| Home owner (ref) | 1 | 1 | 1 | 1 | 1 |
Note. CI = confidence interval; OR = odds ratio; PHD = public housing development; RA = rental assistance SHS = secondhand tobacco smoke. ORs for lifetime and current asthma were estimated in logistic regression models with homeowner as the reference category. Minimally adjusted models controlled for survey year, age, sex, and race/ethnicity, and fully adjusted models controlled for these variables along with highest educational attainment and household income. Separate models included adjustment for smoking status, obesity status, and SHS exposure at home.
The association between housing status and current asthma was modified by smoking status (Table 3); among ever smokers, the odds of current asthma were more than twice as high for PHD residents as for homeowners (OR = 2.58; 95% CI = 1.47, 4.54) and 3 times higher for RA renters than for homeowners (OR = 3.28; 95% CI = 1.97, 5.46). Among never smokers, positive associations were observed for PHD residents and RA renters, but these associations were weaker in magnitude and not statistically significant. There was no effect modification by obesity or age. The strong associations for residence in a PHD and current asthma shown in Table 2 were observed mainly among adults older than 34 years; there was no association among PHD residents aged 34 years or younger.
TABLE 3—
Associations Between Current Asthma and Housing Status in Study Subpopulations According to Age, Smoking Status, and Obesity Status: Boston, MA; Boston Behavioral Risk Factor Surveillance System; 2010–2015
| Housing Status (Ref = Homeowner) |
|||||
| Subpopulation Variable | PHD Resident, OR (95% CI) | RA Renter, OR (95% CI) | Non-RA Renter, OR (95% CI) | Nonrenter Nonowner, OR (95% CI) | Interaction P |
| Age, y | .19 | ||||
| 18–34 | 1.08 (0.46, 2.53) | 2.08 (0.94, 4.58) | 0.79 (0.46, 1.38) | 1.14 (0.55, 2.39) | |
| ≥ 35 | 2.74 (1.86, 4.05) | 2.46 (1.70, 3.54) | 1.27 (0.98, 1.66) | 1.54 (0.84, 2.82) | |
| Smoking status | .04 | ||||
| Ever smoker | 2.58 (1.47, 4.54) | 3.28 (1.97, 5.46) | 0.99 (0.62, 1.58) | 1.72 (0.80, 3.69) | |
| Never smoker | 1.60 (0.92, 2.81) | 1.61 (0.92, 2.81) | 1.06 (0.71, 1.58) | 1.27 (0.67, 2.41) | |
| Obesity status | .19 | ||||
| Obese | 1.97 (1.05, 3.69) | 2.23 (1.22, 4.05) | 0.81 (0.48, 1.34) | 1.94 (0.90, 4.16) | |
| Not obese | 1.93 (1.15, 3.25) | 2.10 (1.25, 3.52) | 1.12 (0.78, 1.62) | 1.10 (0.58, 2.11) | |
Note. CI = confidence interval; OR = odds ratio; PHD = public housing development; RA = rental assistance. ORs for lifetime and current asthma were estimated in logistic regression models with homeowner as the reference category and with the domain statement variable as the subpopulation variable. All models adjusted for survey year, age, sex, race/ethnicity, highest educational attainment, and household income but did not adjust for any of the covariates included in the domain statement. We assessed the overall presence of effect modification according to subpopulation variable by including an interaction term between public housing status and the subpopulation variable; P values for the interaction terms are presented.
The associations between housing status and current asthma remained consistent in direction and magnitude after additional adjustment for variables related to health care access (Table E, available as a supplement to the online version of this article at http://www.ajph.org). The odds of current asthma were approximately 2-fold higher among PHD residents and RA renters than among non-RA renters, and these strong associations persisted after the analysis was restricted to those with household incomes under $35 000, household incomes under $20 000, and both household incomes under $20 000 and educational attainment not exceeding high school (Table F, available as a supplement to the online version of this article at http://www.ajph.org).
DISCUSSION
To our knowledge, this is the first population-based adult study to examine the association between housing status and asthma and compare forms of subsidized housing with home ownership and non-RA renting. In comparison with home ownership, living in PHDs and RA units was strongly associated with lifetime and current asthma, and the observed associations with current asthma among PHD residents and RA renters were robust to adjustments for smoking, obesity, SHS exposure at home, and health care access proxies. Smoking was also found to modify the association between housing status and current asthma, and the associations for PHD residents and RA renters were highest in magnitude among ever smokers. In addition, the associations among PHD residents and RA renters remained consistent even when non-RA renters with similar incomes and educational attainment served as the reference group. In comparison with home owners and non-RA renters, associations were consistently of highest magnitude among RA renters.
Given that we examined more specific types of subsidized housing, our findings are not entirely comparable with those of the earlier-described analysis that leveraged data from the 2001 to 2003 surveys. However, as shown in the previous analysis, the specific associations with current asthma among PHD residents and RA renters are larger in magnitude than for the combined group (PHD residents or RA renters), further underscoring the need for a collective effort to address asthma among individuals living in public housing or RA-based low-income housing. Such interventions should consider the role of social determinants of health and will require collaborations among multiple sectors including health, housing, city planning and development, education, and public safety.24
A coalition of different local- and national-level partners from the public health, housing, academic, nonprofit, hospital, and foundation sectors has led several interventions aimed at improving indoor housing quality in Boston’s PHDs in recent years.9,15,25–28 Notable examples include a series of interventions between 2006 and 2010 designed to reduce pest infestation,25 redevelopment of PHD sites to conform with green standards in 2010,9 adoption of a smoke-free policy in PHDs by the Boston Housing Authority in 2012 (with a similar rule enacted by the US Department of Housing and Urban Development in 2016),15,26,27 and free on-site tobacco cessation counseling offered to PHD residents and staff beginning in 2010 as part of the smoke-free housing policy development process.15,28 Subsequent Boston BRFSS surveys will allow examinations of whether the elevated odds of current asthma among PHD residents and RA renters, relative to homeowners and non-RA renters, have persisted after the aforementioned interventions.
Our intent in conducting a restricted analysis according to household income (and educational attainment) was to construct a comparison group of non-RA renters that more closely resembled adults who were eligible for subsidized housing and to minimize unmeasured confounding from social and economic stressors correlated with household income and educational attainment. Restricting our analysis to adults with household incomes below $20 000 led to more similar race/ethnicity and educational attainment distributions between non-RA renters and PHD residents and RA renters, although marked contrasts in age and sex distributions between these groups persisted.
In Boston, eligibility criteria differ between PHD and RA (i.e., Section 8 housing) programs; whereas PHD programs require that applicants earn less than 80% of area median income, RA programs require that applicants earn less than 50% of area median income and are further restricted in that 75% of new voucher holders can earn no greater than 30% of area median income. It is of interest that the associations with current asthma for PHD residents and RA renters in comparison with non-RA renters persisted after the analyses were restricted to subpopulations with household incomes that met the family income criteria for most (less than $35 000) if not all (less than $20 000) public housing and RA programs offered by the Boston Housing Authority. Associations for asthma were consistently of a higher magnitude among RA renters, suggesting that these individuals may have additional vulnerabilities contributing to poor health. The Department of Housing and Urban Development assists more than 1.2 million low-income families with affordable housing through RA programs and expects landlords to provide healthy housing conditions; however, little is known about the perceived opportunities and challenges related to reducing barriers and capitalizing on the benefits of implementing healthy practices in RA-based housing.29 There is limited evidence suggesting that exposure to environmental asthma triggers (e.g., cockroaches and rodents, parental smoking, and pets with fur) may not decrease significantly when families relocate from public housing to RA-based housing.30
We also identified a novel interaction between housing and smoking status. However, we did not collect information on factors related to housing quality and stability, which may have offered further insight as to why smokers are possibly more vulnerable to asthma associated with subsidized housing. This finding warrants replication in longitudinal studies of subsidized housing populations that involve detailed assessments of housing quality and stability-related factors.
Strengths and Limitations
Our study has numerous strengths, including a large sample size, control for confounding, and inclusion of a comparison group that met income criteria for housing assistance. However, there are several limitations inherent to any cross-sectional population-based survey. We were not able to evaluate the temporality of associations between housing status and asthma in our cross-sectional analysis. In addition, we were not able to assess the impact on asthma prevalence of public housing policy changes or interventions that occurred in Boston during the study period. Self-reported survey measurements of asthma may also be less accurate than physical measurements, and the associations we observed may have been biased by inaccurate recall. However, a 1993 review of asthma questionnaires revealed a mean sensitivity level of 68% and a mean specificity level of 94% for self-reported asthma validated in relation to clinically diagnosed asthma.31
Although our results are relatively robust to potential confounding from a wide array of factors at the individual level, we were not able to adjust for all known confounders. Our findings can potentially be explained by unmeasured confounding, particularly from environmental and social stressors that may correlate with housing status such as outdoor air pollution, violence-related crime, and housing costs. As public housing has been shown to be associated with a number of adult chronic conditions other than asthma,21 adjustment for other possible risk factors shared between adult asthma and other chronic diseases, particularly sleep quality, is warranted.32,33 Also, it is plausible to consider the poorer quality and stability of subsidized housing as consequences of structural and systemic racism, and future population-based studies focusing on public housing and asthma should consider adjustment for area-level measures of racial segregation.34 We may have encountered selection bias, as our poststratification method for weighting accounted for neither housing status nor household income. Potential underweighting or overweighting in our sample of adults living in subsidized housing or having lower household incomes may have led to underestimation or overestimation of true associations. Although our study population was limited to Boston adult residents, our findings may be generalizable to adult populations of urban US cities with similar demographic profiles, including similar eligibility criteria for housing assistance.
Public Health Implications
Living in PHDs and RA units was strongly associated with current asthma in our large cross-sectional sample of adult Boston residents. More research is warranted to assess asthma risk factors among adults living in RA-based low-income housing, and our results highlight the need for intensifying multiple-sector interventions designed to reduce asthma among individuals living in public housing and low-income RA-based housing.
ACKNOWLEDGMENTS
This study was supported by the Boston Public Health Commission and by the Centers for Disease Control and Prevention (CDC), National Center for Chronic Disease Prevention and Health Promotion (grants NU58DP005629-03-05 and 1U58DP005629-01).
Note. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the CDC. The CDC did not participate in the study design; in the collection, analysis, or interpretation of data; or in the writing of the article.
HUMAN PARTICIPANT PROTECTION
No protocol approval was needed because this study involved a secondary analysis of existing de-identified data obtained as part of routine surveillance activities.
Footnotes
REFERENCES
- 1.Nurmagambetov T, Kuwahara R, Garbe P. The economic burden of asthma in the United States, 2008–2013. Ann Am Thorac Soc. 2018;15(3):348–356. doi: 10.1513/AnnalsATS.201703-259OC. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. BRFSS prevalence and trends data. Available at: https://www.cdc.gov/brfss/brfssprevalence. Accessed May 17, 2018.
- 3.Centers for Disease Control and Prevention. National Center for Environmental Health, Air Pollution and Respiratory Health Branch. 2015 asthma data: BRFSS prevalence tables and maps. Available at: https://www.cdc.gov/asthma/brfss/2015/default.html. Accessed May 17, 2018.
- 4.Boston Public Health Commission. Health of Boston 2016–2017. Available at: http://www.bphc.org/boardofhealth/board-meeting-materials/Documents/Health%20of%20Boston%2005-17-17.pdf. Accessed May 17, 2018.
- 5.Krieger J, Higgins DL. Housing and health: time again for public health action. Am J Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sandel M, Wright RJ. When home is where the stress is: expanding the dimensions of housing that influence asthma morbidity. Arch Dis Child. 2006;91(11):942–948. doi: 10.1136/adc.2006.098376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banda E, Persky V, Chisum G, Damitz M, Williams R, Turyk M. Exposure to home and school environmental triggers and asthma morbidity in Chicago inner-city children. Pediatr Allergy Immunol. 2013;24(8):734–741. doi: 10.1111/pai.12162. [DOI] [PubMed] [Google Scholar]
- 8.Jones R, Recer GM, Hwang SA, Lin S. Association between indoor mold and asthma among children in Buffalo, New York. Indoor Air. 2011;21(2):156–164. doi: 10.1111/j.1600-0668.2010.00692.x. [DOI] [PubMed] [Google Scholar]
- 9.Colton MD, Laurent JG, MacNaughton P et al. Health benefits of green public housing: associations with asthma morbidity and building-related symptoms. Am J Public Health. 2015;105(12):2482–2489. doi: 10.2105/AJPH.2015.302793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Northridge J, Ramirez OF, Stingone JA, Claudio L. The role of housing type and housing quality in urban children with asthma. J Urban Health. 2010;87(2):211–224. doi: 10.1007/s11524-009-9404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hynes HP, Brugge D, Osgood ND, Snell J, Vallarino J, Spengler J. “Where does the damp come from?” Investigations into the indoor environment and respiratory health in Boston public housing. J Public Health Policy. 2003;24(3–4):401–426. [PubMed] [Google Scholar]
- 12.Findley S, Lawler K, Bindra M, Maggio L, Penachio MM, Maylahn C. Elevated asthma and indoor environmental exposures among Puerto Rican children of East Harlem. J Asthma. 2003;40(5):557–569. doi: 10.1081/jas-120019028. [DOI] [PubMed] [Google Scholar]
- 13.Williamson IJ, Martin CJ, McGill G, Monie RD, Fennerty AG. Damp housing and asthma: a case-control study. Thorax. 1997;52(3):229–234. doi: 10.1136/thx.52.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu FB, Persky V, Flay BR, Richardson J. An epidemiological study of asthma prevalence and related factors among young adults. J Asthma. 1997;34(1):67–76. doi: 10.3109/02770909709071205. [DOI] [PubMed] [Google Scholar]
- 15.Russo ET, Hulse TE, Adamkiewicz G et al. Comparison of indoor air quality in smoke-permitted and smoke-free multiunit housing: findings from the Boston Housing Authority. Nicotine Tob Res. 2015;17(3):316–322. doi: 10.1093/ntr/ntu146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adamkiewicz G, Spengler JD, Harley AE et al. Environmental conditions in low-income urban housing: clustering and associations with self-reported health. Am J Public Health. 2014;104(9):1650–1656. doi: 10.2105/AJPH.2013.301253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenfeld L, Chew GL, Rudd R et al. Are building-level characteristics associated with indoor allergens in the household? J Urban Health. 2011;88(1):14–29. doi: 10.1007/s11524-010-9527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lambertino A, Turyk ME, Curtis L, Persky VW. Asthma morbidity in adult Chicago public housing residents. J Asthma. 2009;46(2):202–206. doi: 10.1080/02770900802627286. [DOI] [PubMed] [Google Scholar]
- 19.Levy JI, Brugge D, Peters JL, Clougherty JE, Saddler SS. A community-based participatory research study of multifaceted in-home environmental interventions for pediatric asthmatics in public housing. Soc Sci Med. 2006;63(8):2191–2203. doi: 10.1016/j.socscimed.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Clougherty JE, Levy JI, Hynes HP, Spengler JD. A longitudinal analysis of the efficacy of environmental interventions on asthma-related quality of life and symptoms among children in urban public housing. J Asthma. 2006;43(5):335–343. doi: 10.1080/02770900600701408. [DOI] [PubMed] [Google Scholar]
- 21.Digenis-Bury EC, Brooks DR, Chen L, Ostrem M, Horsburgh CR. Use of a population-based survey to describe the health of Boston public housing residents. Am J Public Health. 2008;98(1):85–91. doi: 10.2105/AJPH.2006.094912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fenelon A, Mayne P, Simon AE et al. Housing assistance programs and adult health in the United States. Am J Public Health. 2017;107(4):571–578. doi: 10.2105/AJPH.2016.303649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: annual survey data. Available at: https://www.cdc.gov/brfss/annual_data/annual_data.htm. Accessed May 17, 2018.
- 24.Raphael JL, Colvin JD. More than wheezing: incorporating social determinants into public policy to improve asthma outcomes in children. Pediatr Res. 2017;81(1):2–3. doi: 10.1038/pr.2016.223. [DOI] [PubMed] [Google Scholar]
- 25.Scammell MK, Duro L, Litonjua E, Berry L, Reid M. Meeting people where they are: engaging public housing residents for integrated pest management. Prog Community Health Partnersh. 2011;5(2):177–182. doi: 10.1353/cpr.2011.0017. [DOI] [PubMed] [Google Scholar]
- 26.MacNaughton P, Adamkiewicz G, Arku RE, Vallarino J, Levy DE. The impact of a smoke-free policy on environmental tobacco smoke exposure in public housing developments. Sci Total Environ. 2016;557–558:676–680. doi: 10.1016/j.scitotenv.2016.03.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Department of Housing and Urban Development. Instituting smoke-free public housing. Available at: https://www.hud.gov/sites/documents/SMOKEFREEPHFINALRULE.PDF. Accessed May 17, 2018.
- 28.Brooks DR, Burtner JL, Borrelli B et al. Twelve-month outcomes of a group-randomized community health advocate-led smoking cessation intervention in public housing. Nicotine Tob Res. 2017 [Epub ahead of print] doi: 10.1093/ntr/ntx193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Polletta VL, Reid M, Barros E et al. Role of landlords in creating healthy homes: section 8 landlord perspectives on healthy housing practices. Am J Health Promot. 2017;31(6):511–514. doi: 10.1177/0890117116671081. [DOI] [PubMed] [Google Scholar]
- 30.Fortson JG, Sanbonmatsu L. Child health and neighborhood conditions: results from a randomized housing voucher experiment. J Hum Resour. 2010;45(4):840–864. [Google Scholar]
- 31.Torén K, Brisman J, Jarvholm B. Asthma and asthma-like symptoms in adults assessed by questionnaires. A literature review. Chest. 1993;104(2):600–608. doi: 10.1378/chest.104.2.600. [DOI] [PubMed] [Google Scholar]
- 32.Curtis DS, Fuller-Rowell TE, El-Sheikh M, Carnethon MR, Ryff CD. Habitual sleep as a contributor to racial differences in cardiometabolic risk. Proc Natl Acad Sci U S A. 2017;114(33):8889–8894. doi: 10.1073/pnas.1618167114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kong DL, Qin Z, Shen H, Jin HY, Wang W, Wang ZF. Association of obstructive sleep apnea with asthma: a meta-analysis. Sci Rep. 2017;7(1):4088. doi: 10.1038/s41598-017-04446-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31(1):178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]