Abstract
Background:
Cam-type femoroacetabular impingement (FAI) is a femoral head-neck deformity that causes abnormal contact between the femoral head and acetabular rim, leading to pain. However, some individuals with the deformity do not experience pain and are referred to as having a femoroacetabular deformity (FAD). To date, only a few studies have examined muscle activity in patients with FAI, which were limited to gait, isometric and isokinetic hip flexion, and extension tasks.
Purpose:
To compare (1) hip muscle strength during isometric contraction and (2) lower limb kinematics and muscle activity of patients with FAI and FAD participants with body mass index–matched healthy controls during a deep squat task.
Study Design:
Controlled laboratory study.
Methods:
Three groups of participants were recruited: 16 patients with FAI (14 male, 2 female; mean age, 38.5 ± 8.0 years), 18 participants with FAD (15 male, 3 female; mean age, 32.5 ± 7.1 years), and 18 control participants (16 male, 2 female; mean age, 32.8 ± 7.0 years). Participants were outfitted with electromyography electrodes on 6 muscles and reflective markers for motion capture. The participants completed maximal strength tests and performed 5 deep squat trials. Muscle activity and biomechanical variables were extrapolated and compared between the 3 groups using 1-way analysis of variance.
Results:
The FAD group was significantly stronger than the FAI and control groups during hip extension, and the FAD group had greater sagittal pelvic range of motion and could squat to a greater depth than the FAI group. The FAI group activated their hip extensors to a greater extent and for a longer period of time compared with the FAD group to achieve the squat task.
Conclusion:
The stronger hip extensors of the FAD group are associated with greater pelvic range of motion, allowing for greater posterior pelvic tilt, possibly reducing the risk of impingement while performing the squat, and resulting in a greater squat depth compared with those with symptomatic FAI.
Clinical Relevance:
The increased strength of the hip extensors in the FAD group allowed these participants to achieve greater pelvic mobility and a greater squat depth by preventing the painful impingement position. Improving hip extensor strength and pelvic mobility may affect symptoms for patients with FAI.
Keywords: femoroacetabular impingement, cam deformity, electromyography, biomechanics, motion analysis, squat
Cam-type hip morphology, which in some individuals is associated with femoroacetabular impingement (FAI), affects the articular surfaces of the anterosuperior portion at the femoral head-neck junction4,14 and has been implicated as a cause of labral-chondral damage as well as an early cause of hip osteoarthritis.14,24,33,49 Several studies have suggested that cam-type FAI, defined by an aspherical femoral head and/or insufficient femoral head-neck offset25,50 with larger alpha angles,41 could result in anterior hip or groin pain, labral tears, and damage to the acetabular articular cartilage.7,15,25,51 Symptomatic patients demonstrate a positive flexion, adduction, and internal rotation (FADIR) test finding,7,35,42 greater superoposterior femoral coverage and a higher pelvic incidence,16,40 a decreased neck-shaft angle,38,39 and decreased range of motion (ROM),27,29,30 which may result in greater mechanical stress at the anterosuperior portion of the acetabulum.38 However, some individuals with a cam deformity may not experience symptoms or clinical signs,1,17,18,26,28,37,46 and to our knowledge, no study has compared muscular activity in symptomatic patients with FAI to asymptomatic individuals with a femoroacetabular deformity (FAD) during a deep squat task.
When compared with healthy population, patients with FAI were shown to have muscle weakness in all hip muscle groups except for the hip extensors and internal rotators.9 During maximal isometric hip flexion, electromyography (EMG) activity was lower in patients with FAI compared with healthy participants9 for the tensor fasciae latae (TFL) but not the rectus femoris (RF) muscle. Another study that examined hip flexion strength under isometric and isokinetic conditions showed hip flexor weakness in patients with FAI under both conditions compared with healthy control participants, but no differences existed in muscle activity.8 To date, only a few studies have reported on muscle activity in patients with FAI during daily activities.8,9,11 However, these studies have only compared presurgical symptomatic patients with FAI with healthy control participants; they did not track or include asymptomatic individuals with cam morphology (FAD) in motion analysis. It remains unclear if this muscle weakness is part of the pathological process of FAI or something that could be modified by conservative treatment. Also, muscle weakness and muscle imbalance can be determinants for joint stability.53
Usually reported as pain-free and not involving the range of hip impingement, subtle gait alterations in FAI patients have been reported.6,23,27,48 Patients with FAI have also reported pain triggered by sitting in a low chair.32 A functional task that requires large sagittal hip and pelvic ROM and that may lead to impingement, such as squatting, may be a more challenging task that better reproduces the motion of sitting; squatting may also be demanding enough to evaluate lower limb function.
The objectives of this study were (1) to compare hip muscle strength during maximum voluntary isometric contraction (MVIC) and (2) to compare lower limb kinematics and muscle activity of symptomatic patients with FAI and asymptomatic participants with FAD during a deep squat task and compare the results with those of healthy body mass index–matched controls (CTRL group). It was hypothesized that the FAI group may show less hip flexion and hip abduction during squatting when compared with the FAD and CTRL groups. It was also hypothesized that patients with FAI would have weaker hip flexor muscles and consequently higher normalized muscle activation when performing the squat trials. This was expected as a way for patients with FAI to compensate for their weakness while performing the same task.
Methods
Participants
After approval from the hospital’s and university’s ethics committees, 16 patients with FAI were initially recruited by clinical research staff from the senior orthopaedic surgeon’s (P.E.B.) clinical practice during a 2-year recruitment period at the local hospital. Thirty-six participants (31 male, 5 female) were recruited from the community to serve as controls. Initial radiographs of all the CTRL participants were taken to screen for the presence of a cam-type deformity. Several CTRL participants showed the presence of a cam deformity but did not experience any clinical symptoms. After this finding, the decision was made to have all participants (with and without the cam-type deformity) undergo full radiographic screening using low-dose computed tomography (CT). CT from the pelvis to knee was performed using a clinical CT scanner (Aquilion CT Scanner [Toshiba] or Discovery CT750 HD [GE Healthcare]). The CT scans of all participants were read by a musculoskeletal radiologist to confirm the presence of a cam deformity. Alpha angles greater than 50.5° (anteriorly at the 3:00 clock-face position about the femoral neck) or 60° (anterosuperiorly at 1:30) were considered positive for cam morphology.3,17,28,45,52 Participants with neurological or musculoskeletal disorders, degenerative diseases, or any previous major lower limb injuries or surgeries were excluded from the study.
Based on the CT scans, we divided our cohort of participants into 3 groups: those with symptomatic cam-type FAI, those with a cam deformity but no symptoms (FAD), and the CTRL group (Table 1). Patients with FAI had experienced hip pain for longer than 6 months near the groin/lateral aspect of the hip and had produced a positive impingement test (FADIR) result.7,31 The CT scans of participants with FAD indicated the presence of a cam deformity, but these participants did not experience any hip pain or produce a positive impingement test finding. CTRL participants did not have the presence of a cam deformity as indicated by CT, nor did they experience any hip pain or produce a positive FADIR test finding. As a matter of comparison, the affected hip in patients with FAI with a bilateral cam deformity was the one with greater clinical signs; in the FAD group, the side of interest was the one with the larger alpha angle, and the selected hip for the CTRL participants was based on their dominant leg.
TABLE 1.
Demographics and Patient-Reported Outcomesa
| FAI (n = 16) | FAD (n = 18) | CTRL (n = 18) | |
|---|---|---|---|
| Presence of cam deformity | Yes | Yes | No |
| Positive impingement test result | Yes | No | No |
| Sex, male/female, n | 14/2 | 15/3 | 16/2 |
| Height, m | 1.74 ± 0.07 | 1.77 ± 0.09 | 1.74 ± 0.09 |
| Age,b y | 38.5 ± 8.0 | 32.5 ± 7.1 | 32.8 ± 7.0 |
| Body mass index, kg/m2 | 26.8 ± 5.0 | 25.7 ± 1.9 | 25.5 ± 3.3 |
| Axial alpha angle, deg | 57 ± 6 | 58 ± 7 | 43 ± 4 |
| Radial alpha angle, deg | 67 ± 5 | 70 ± 7 | 52 ± 5 |
| Femoral neck-shaft angle,b deg | 123 ± 3 | 127 ± 3 | 127 ± 2 |
| HOOS | |||
| Symptomsb | 65.6 ± 14.4 | 95.3 ± 7.2 | 97.8 ± 5.7 |
| Painb | 66.3 ± 16.3 | 98.2 ± 4.6 | 98.8 ± 4.2 |
| Activities of daily livingb | 75.7 ± 17.9 | 99.6 ± 1.2 | 100.0 ± 0.0 |
| Sport/recreationb | 56.3 ± 22.0 | 97.9 ± 6.4 | 99.7 ± 1.5 |
| Quality of lifeb | 39.5 ± 19.3 | 95.8 ± 8.3 | 98.6 ± 4.6 |
aData are reported as mean ± SD unless otherwise indicated. CTRL, control; FAD, femoroacetabular deformity; FAI, femoroacetabular impingement; HOOS, Hip disability and Osteoarthritis Outcome Score.
bThe FAI group differed significantly from the FAD and CTRL groups (P < .001).
The initial cohort was composed of 68 participants; however, 16 were excluded for various reasons (CT malperformance: 1 FAI; recent surgical treatment: 1 FAI; data collection complications: 1 FAI and 1 FAD; EMG malfunction or poor signals: 2 FAI, 4 FAD, and 1 CTRL; did not perform a minimum of 90° of knee flexion during squat: 1 FAI, 2 FAD, and 2 CTRL). A total of 52 participants were included in the analysis (Table 1).
Protocol
Following the CT scans, participants were transferred to the motion analysis laboratory. After warming up for 5 minutes on a cycle ergometer and performing uninstructed stretching, participants completed 2 trials of a sit-and-reach flexibility test while barefoot.54
After the flexibility test, participants were instrumented with wireless EMG probes (FREEEMG 300; BTS Bioengineering) placed on the RF, biceps femoris (BF), semitendinosus (ST), TFL, gluteus medius (GMed), and gluteus maximus (GMax) muscles according to the SENIAM guidelines.19,20 Muscle strength activity was recorded using a handheld dynamometer (Manual Muscle Testing System Model 01163; Lafayette Instrument) and the EMG system during MVIC in the following movements: hip flexion, hip extension, hip abduction, hip flexion with hip abduction, and knee flexion (Table 2). Participants were verbally encouraged to complete 2 MVIC trials of 5 seconds for each selected motion as forcefully as possible without causing pain. A rest period of 30 seconds was provided between the 2 MVIC trials. Participants were then outfitted with 45 reflective markers according to the University of Ottawa Motion Analysis Model marker set.34 To improve accuracy, the markers at the anterior superior iliac spine (ASIS), posterior superior iliac spine (PSIS), and lateral and medial epicondyles were placed according to identification through the CT scans. All participants remained barefoot for motion capture testing to standardize the movement because shoes with different heel-stack heights could have affected the squat.
TABLE 2.
Hip Muscle Strength Produced During MVIC Normalized by Body Weighta
| Movement | Illustration | Normalized Torque, N·m/kg | ||
|---|---|---|---|---|
| FAI | FAD | CTRL | ||
| Hip flexionb,c |
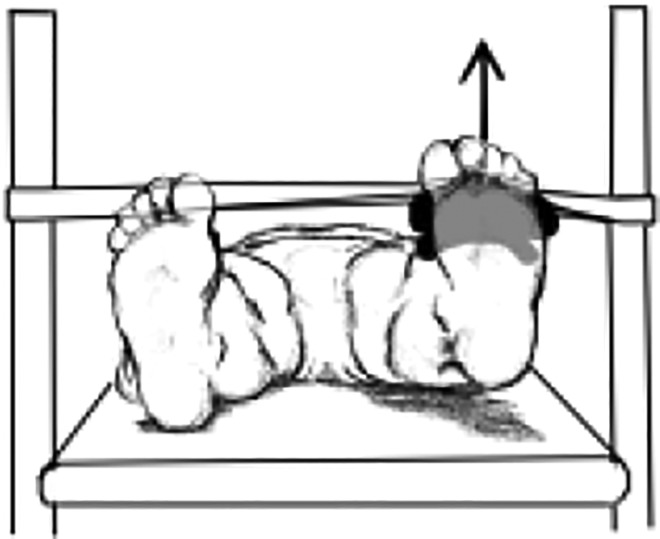
|
1.56 ± 0.62 | 2.12 ± 0.74 | 2.11 ± 0.63 |
| Hip extensionb,d |
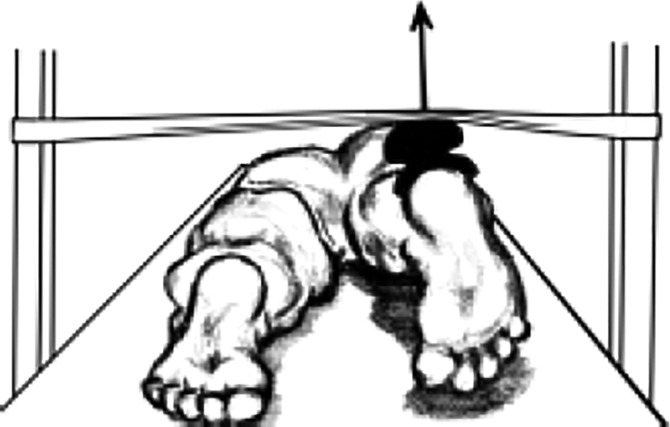
|
1.62 ± 0.82 | 2.13 ± 0.80 | 1.69 ± 0.67 |
| Hip abduction |
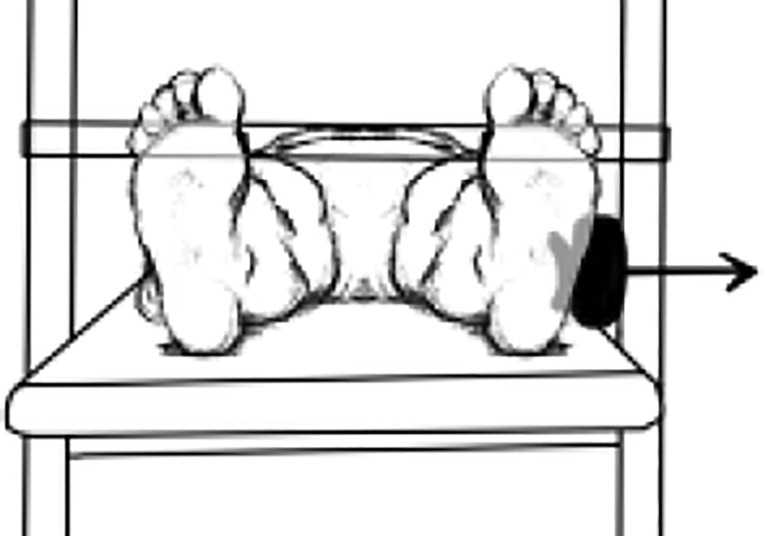
|
1.39 ± 0.45 | 1.53 ± 0.50 | 1.60 ± 0.51 |
| Hip flexion with hip abduction |
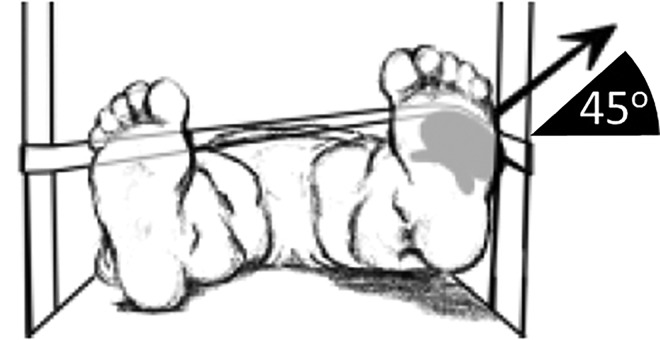
|
1.36 ± 0.41 | 1.50 ± 0.51 | 1.60 ± 0.50 |
| Knee flexion |
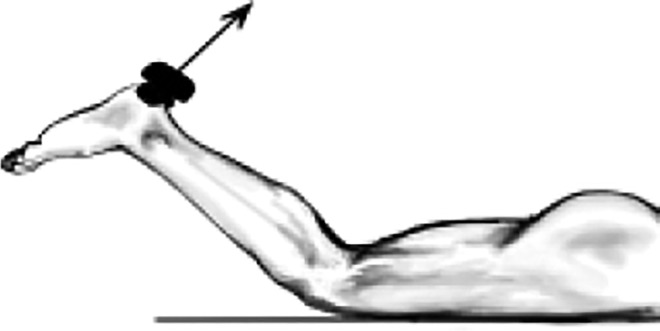
|
0.88 ± 0.38 | 0.99 ± 0.35 | 0.92 ± 0.35 |
aData are reported as mean ± SD. CTRL, control; FAD, femoroacetabular deformity; FAI, femoroacetabular impingement; MVIC, maximum voluntary isometric contraction.
bThe FAI group differed significantly from the FAD group (P < .05).
cThe FAI group differed significantly from the CTRL group (P < .05).
dThe FAD group differed significantly from the CTRL group (P < .05).
Motion capture was performed using 10 infrared cameras (MX13; Vicon Motion Systems) sampled at 200 Hz and 2 force plates (Force Plate FP4060-08; Bertec) measuring ground-reaction forces at 1000 Hz. Data were recorded, synchronized, and labeled using Nexus software (version 1.8.5; Vicon Motion Systems).
The participants performed 5 squat trials in a controlled position with their feet pointing forward and hip-width apart with each foot on a force plate. They were instructed to keep their arms elevated in front of the torso at shoulder width during the task. Participants were instructed to squat as deeply as possible without lifting their heels off the floor. The task was performed at the participants’ self-selected pace, with a brief pause at the bottom of the squat. An adjustable bench was set to one-third the height of the participants’ tibia for safety to prevent them from falling.
Statistical Analysis
Three-dimensional kinematic data were processed and filtered. The ground-reaction force data were filtered and used to calculate joint kinetics. Joint kinematics and kinetics were taken as the average of the 5 squat trials.
Maximal squat depth (percentage of leg length) was defined as the lowest point attained by the origin of the pelvis (calculated as the midpoint between the left and right ASIS and PSIS markers) during the squat, divided by the participant’s leg length, which corresponded to the averaged linear distance between the participant’s medial malleoli and ASIS. A lower value indicated a deeper squat.
EMG data were processed using custom software designed in MATLAB (MathWorks). All EMG signals were high-pass filtered, bias removed, and rectified, and a low-pass filter defined their linear envelope. The peak level of activation of the MVIC linear envelope was then taken as the amplitude normalization value. Signals were time-normalized for the squat descent and squat ascent phases separately. The selected variables were linear envelope peak (PeakLE), time to reach the PeakLE, and total muscle activity (iEMG), which was the integral of the linear envelope. All variables were averaged across the respective groups for each muscle and phase of the squat.
Data were assessed for normality using the Shapiro-Wilk test. One-way analysis of variance was used to examine differences between the 3 groups, with a Bonferroni post hoc test conducted to determine between-group differences (P < .05).
Results
No significant differences existed between the 3 groups for the sit-and-reach flexibility test findings. Differences in strength values during MVIC trials occurred for the hip flexion and hip extension movements (Table 2). The FAI group had lower hip flexion strength compared with both the FAD (P = .003) and CTRL (P = .003) groups. The FAD group had greater hip extension strength compared with the FAI (P = .026) and the CTRL (P = .047) groups. No significant differences in strength existed between the groups for knee flexion, neutral hip abduction, or hip abduction with hip flexion.
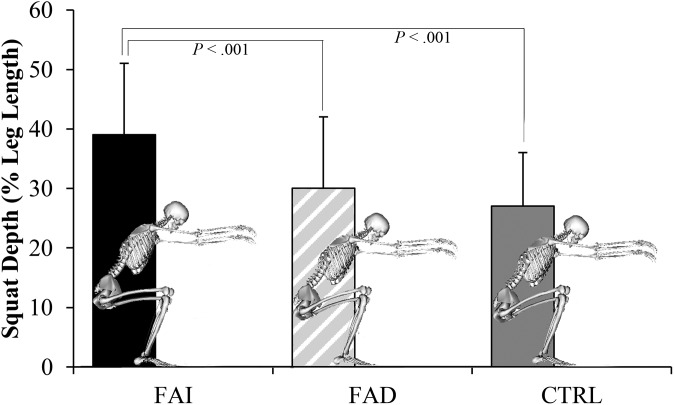
The maximal squat depths achieved during the squat cycle were the following: FAI, 39.4% ± 12.3%; FAD, 30.0% ± 12.2%; and CTRL, 27.1% ± 8.8% (Figure 1). The FAI group was unable to achieve as deep a squat as the FAD (P < .001) and CTRL (P < .001) groups, while no differences were found between the FAD and CTRL groups (P = .252).
Figure 1.
Maximum squat depth achieved for the femoroacetabular impingement (FAI), femoroacetabular deformity (FAD), and control (CTRL) groups.
Pelvic sagittal ROM is illustrated in Figure 2. During the first half of the descent phase of the squat, pelvic ROM was significantly lower (P = .015) for the FAI group (12.0° ± 5.0°) compared with the FAD group (18.4° ± 6.0°) but not compared with the CTRL group (16.9° ± 3.8°) (Figure 2B). During the second half of the descent phase of the squat, pelvic ROM was significantly lower for the FAI group (7.2° ± 4.1°) compared with the FAD (14.2° ± 7.2°) and CTRL (12.7° ± 6.6°) groups (P = .006 and .037, respectively) (Figure 2C). During the first half of the ascent phase of the squat, pelvic ROM was significantly lower (P = .039) in the FAI group (7.2° ± 3.7°) than in the CTRL group (12.5° ± 7.5°) (Figure 2E).
Figure 2.
Sagittal pelvic tilt and range of motion (ROM) during a squat task in the femoroacetabular impingement (FAI), femoroacetabular deformity (FAD), and control (CTRL) groups. (A) Sagittal pelvic tilt during the descent phase, (B) trough-to-peak ROM during the descent phase, (C) peak-to-trough ROM during the descent phase, (D) sagittal pelvic tilt during the ascent phase, (E) trough-to-peak ROM during the ascent phase, and (F) peak-to-trough ROM during the ascent phase. *Significant difference in ROM between groups (P < .05).
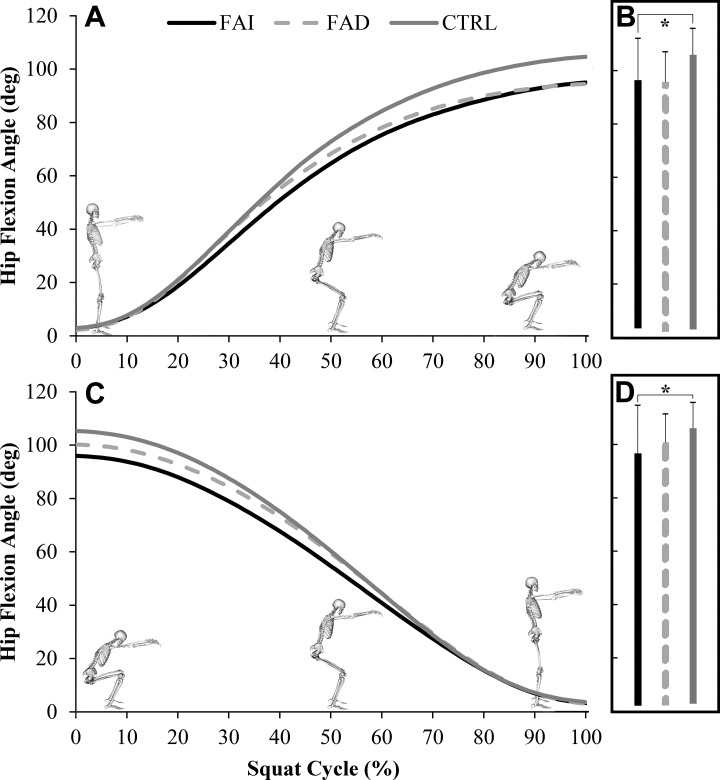
Peak hip flexion was lower for the FAI group compared with the CTRL group for both the descent phase (P = .038) and the ascent phase (P = .028) of the squat (Figure 3). During the descent phase of the squat, sagittal hip ROM was significantly (P = .025) lower in the FAI group (88.6° ± 23.5°) compared with the CTRL group (103.8° ± 10.6°) but not compared with the FAD group (97.5° ± 11.8°) (Figure 3B). During the ascent phase of the squat, sagittal hip ROM was significantly (P = .037) lower in the FAI group (90.7° ± 20.5°) compared with the CTRL group (103.5° ± 11.0°) but not compared with the FAD group (97.2° ± 11.2°) (Figure 3D). No significant differences in hip abduction or hip joint kinetics (frontal and sagittal) existed between any of the groups.
Figure 3.
Sagittal hip movement during a squat task in the femoroacetabular impingement (FAI), femoroacetabular deformity (FAD), and control (CTRL) groups. (A) Hip flexion during the descent phase, (B) range of motion (ROM) during the descent phase, (C) hip flexion during the ascent phase, and (D) ROM during the ascent phase. *Significant difference in ROM between groups (P < .05).
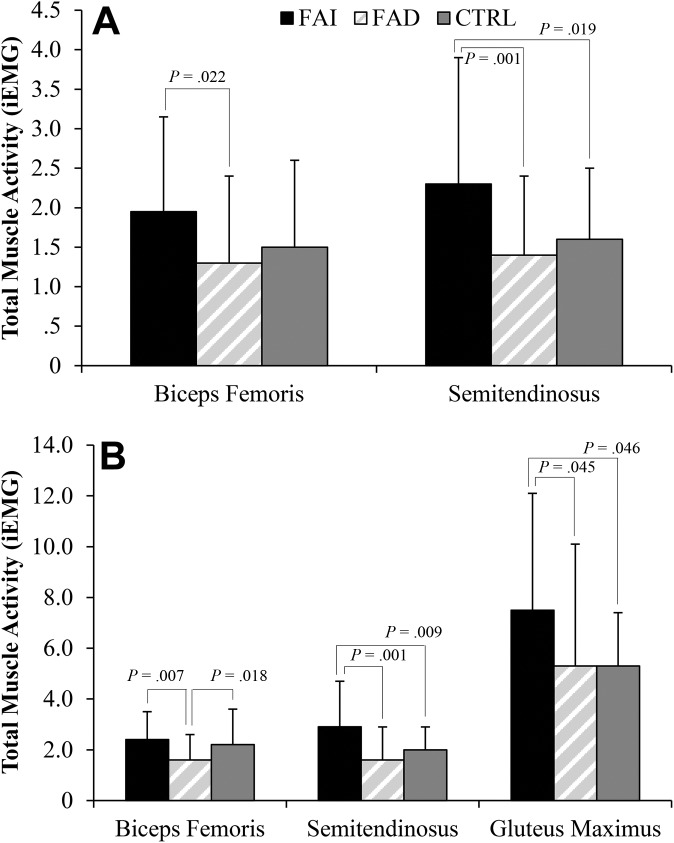
For the EMG analyses, because the signals were normalized by their maximum, the muscle activity results were inversely proportional to the muscle’s ability to produce force, as a weaker muscle will need higher muscle activity to perform the same task as its normal-strength counterpart. The FAI group had a significantly greater PeakLE for the BF and ST muscles compared with the FAD group for both squat descent and squat ascent (Figure 4). During squat descent, the PeakLE of the RF muscle was significantly lower for the FAD group compared with both the FAI and CTRL groups (Figure 4A). During squat ascent, the PeakLE of the GMax muscle was significantly lower (P = .005) for the FAD group than for the FAI group (Figure 4B). No significant differences in the PeakLE were observed for the TFL and GMed muscles or in the time to reach the PeakLE in any of the groups for any of the muscles.
Figure 4.
Linear envelope peak for the femoroacetabular impingement (FAI), femoroacetabular deformity (FAD), and control (CTRL) groups during the (A) squat descent and (B) squat ascent tasks. MVIC, maximum voluntary isometric contraction.
The FAI group had significantly greater iEMG for the BF and ST muscles compared with the FAD group for both squat descent and squat ascent (Figure 5). During squat ascent, the FAI group had significantly greater iEMG for the GMax muscle compared with the FAD group (P = .045) and the CTRL group (P = .046) (Figure 5B) . No significant differences in iEMG were observed for the RF, TFL, and GMed muscles.
Figure 5.
Total muscle activity for the femoroacetabular impingement (FAI), femoroacetabular deformity (FAD), and control (CTRL) groups during the (A) squat descent and (B) squat ascent tasks. iEMG, total muscle activity.
Discussion
Our study hypothesis was that the FAI group would show decreased hip flexion and hip abduction during the squat task when compared with the FAD and CTRL groups. The hypothesis also stated that patients with FAI would have weaker hip flexor muscles and that higher normalized activation for hip flexors would compensate for their weakness while performing the dynamic task. Although we focused the hypothesis on the hip joint, and differences in hip sagittal ROM were found when comparing the FAI and CTRL groups, the most relevant finding was regarding pelvic tilt, as the FAI group had significantly less ROM when compared with the other 2 groups, specifically in the descending phase of the squat. The muscle strength analyses showed that patients with FAI not only had weaker hip flexors than the other groups but also that participants with FAD demonstrated stronger hip extensors when compared with the symptomatic patients. This strength difference was indicated in the EMG analyses, as the FAI group showed higher muscular activation during the squat task compared with the other groups.
Squat tasks have previously been proposed as a diagnostic tool for assessing FAI, as squatting requires large sagittal hip and pelvic ROM, attainable by many healthy participants but few patients with FAI.30 It has already been shown that patients with FAI are unable to squat as deeply as their healthy peers because of mobility restrictions at the hip and pelvis.30 However, no research has included participants with FAD in their comparison; these individuals have the same cam morphology but do not experience any of the pain symptoms. If the restriction in mobility was caused by the presence of femoral cam morphology, then participants with FAD should have achieved a squat depth similar to that of the FAI group; however, their movement was similar to that of the CTRL group (Figure 1). It is still elusive that a soft tissue abnormality (ie, labrum, capsule) could be a cause of the mobility restriction in patients with FAI, but more research is needed to investigate the effect of soft tissue abnormalities on hip motion restriction.
As observed in previous research, a lower neck-shaft angle also differentiates symptoms for patients with cam-type FAI.37,38 A greater pelvic incidence is also another morphological parameter that can contribute as a predictor of symptomatic cam-type FAI.16 The differences in motion and symptoms between the FAI and FAD groups cannot be explained by static bony geometry but rather implicate dynamic motion of the femur and pelvis, which are affected by the soft tissues around the hip. In this study, we examined the role of various muscles in dynamic hip movement and found that, as observed in other studies,9 patients with FAI did not perform as well in hip flexion tasks compared with participants with FAD and healthy controls. In this study, there were no differences in abduction and abduction with hip flexion strength. Interestingly, the FAD group had significantly stronger hip extensor strength (see Table 2). As a mechanism to compensate for muscular weakness during a dynamic task, higher normalized EMG activity was expected from the weak muscle when compared with its stronger counterpart. Although the FAI group was shown to have weaker hip flexors, higher EMG activity was not found for the hip flexor measured in this study when compared with the CTRL group. Perhaps one of the deeper hip flexors not measured in this study (eg, iliacus or psoas major) may be primarily responsible for the lack of strength in the FAI group. Future studies should therefore include muscle activity for more hip flexors, either through indwelling EMG or optimization, to determine which hip flexors are weaker.
EMG activity for all hip extensor muscles was recorded in this study, with the exception of the semimembranosus muscle. As muscle activity results were collected through surface EMG and the semimembranosus lies deep to the ST, the signal output might have been compromised by muscle crosstalk. Moreover, the SENIAM guideline,19,20 which was used in this study, does not have any placement recommendation regarding the semimembranosus. An examination of the PeakLE during the descent phase of the squat (eccentric) highlighted hip extensor strength in the FAD group, as both the BF and ST muscles had lower peaks compared with the other 2 groups. As for the ascent phase (concentric), higher peaks in the FAI group showed that these patients had to activate these muscles to a greater extent while standing up compared with the FAD and CTRL groups (Figure 4).
Sparse research exists that quantifies the muscle activity of patients with FAI. A previous study that compared hip muscle strength between patients with FAI and healthy controls found that the FAI group had weaker hip muscles, with the exception of the internal rotators and extensors .9 When comparing the FAI and CTRL groups, we also found hip flexor weakness, comparable hip extensor strength, and no differences in TFL strength. The major difference in this study was that we were able to compare these data for the FAD group, which had significantly stronger hip extensors than the FAI and CTRL groups (see Table 2). Hip extensor strength may play a significant role in preventing symptomatic cam impingement.
Hip motion is complex from a biomechanical perspective, and its kinematics are influenced by many factors, including osseous, ligamentous, and muscular structures.5 Hip flexion and extension are often thought of as movement of the femoral head within the acetabulum. Our research highlights the importance of pelvic motion (ie, anterior and posterior pelvic tilt) in hip kinematics and the role of the hip flexors and extensors in changing the orientation of the acetabulum in various activities, such as squatting. Weakness in hip flexors and extensors may result in restricted ability to control the pelvis for good posture and stabilization. While weakness in the hip extensors would result in anterior pelvic tilt, strong hip extensors can contribute to improved posterior pelvic tilt. Patients with FAI experience painful impingement when their femoral cam deformity abuts against the acetabulum. Increased anterior pelvic tilt can lead to early impingement, which could explain why patients with FAI could not squat as deeply as their counterparts with FAD (see Figure 1), who were able to posteriorly tilt their pelvis and avoid painful impingement. The result of this muscle imbalance was restricted pelvis ROM in the FAI group during the squat task (see Figure 2).
During both squat phases, the FAI group had to activate the ST and BF muscles to a greater degree than the FAD group (Figure 4A and 4B). The same occurred for the GMax muscle during squat ascent (Figure 4B). It was speculated that decreased activation of the GMax and hamstring muscles could contribute to the lack of posterior tilt during a deep squat2; however, our findings show the exact opposite. This is because of the origin of these muscles, as any anterior pelvic tilt increases the moment arm of these muscles, requiring the FAI group to activate to a greater extent to achieve the same movement as the FAD group, which was in a posterior pelvic tilt position.
Because the ST and BF muscles originate on the ischial tuberosity and the GMax originates on the gluteal surface of the ilium, anterior pelvic tilt would increase the length of these muscles, as shown by the FAI group. To overcome this lengthened position, these muscles had greater peak activation (Figure 4) and iEMG (Figure 5), resulting in a less efficient squat performance. Stronger hip extensors would allow the pelvis to be brought to a posterior position during the midphase of the squat, perhaps avoiding impingement.
Possible overdiagnosis and overtreatment of patients with suspected FAI have always been a concern.18,43 Surgical procedures for correcting FAI have increased by as much as 18-fold in the United States from 1999 to 2009.10 Such surgical interventions are associated with many possible complications, including prolonged pain, nerve damage, fractures, and the development of hip osteoarthritis.13,36 Despite these surgical interventions to address FAI, some patients may still need total hip arthroplasty.21,44 Current evidence for the conservative treatment of FAI is limited to case series12,22 (level 4 evidence) and is affected by patient demand for surgical treatment as well as a paucity of effective exercises.47 In these studies, however, a staged physical therapy approach with activity modification and exercise led to improved patient-reported outcomes.12,22 The use of conservative treatment in patients with FAI could be a strategy for avoiding surgery to ease hip pain.
Previous research suggests that hip extensors are not weaker in patients with FAI compared with healthy control participants9; therefore, hip extensor therapy was not a vital component in physical therapy protocols. However, healthy participants do not have the same cam deformity as patients with FAI, so they are still able to achieve a low, pain-free squat without controlling the pelvis in the same manner as participants with FAD. Compared with the FAI group, the FAD group in our cohort had significantly stronger hip extensors (see Table 2) and significantly better posterior pelvic tilt at the bottom of the squat (see Figure 2). We believe that these stronger hip extensors play an important role in sagittal pelvic ROM, allowing the FAD group to avoid impingement between the acetabular rim and femoral head-neck junction and allowing them to achieve a much lower squat depth than the FAI group (see Figure 1). Thus, improving hip extensor strength and pelvic mobility may affect symptoms for patients with FAI. Future studies should perform an intervention that tests this hypothesis as a way to possibly prevent some corrective surgical procedures. As the participants with FAD were younger than the patients with FAI and had similar cam-type morphology, it can be speculated that they were in the early progression of FAI. It may not be until labral tears or capsular lesions occur as a result of cam impingement that these individuals progress to symptoms and into the FAI group. Therefore, a longitudinal study of FAD is necessary to accept or reject the hypothesis that some participants with FAD will progress to the symptomatic group.
Some limitations of this study must be acknowledged. One limitation was the small cohort, which included 16 patients with symptomatic cam-type FAI. The recruitment of 18 participants with an asymptomatic cam deformity can be considered a challenge, as they do not present pain and are difficult to track in the clinical practice. The strength measurements were performed in an isometric condition, and the analyses were extrapolated to the dynamic squat task. A better condition to assess the participants’ strength could be achieved on an isokinetic device; however, this would have drastically increased the overall data collection time. Although EMG data collection was rigorously completed and followed all requirements19 regarding skin preparation and probe placement and was also normalized by MVIC, muscle activation signal variability among participants must be noted, as individual skin adipose tissue and motor point location may vary.
This study provides a greater understanding of the role of the muscles and soft tissues around the hip that contribute to the possible development of symptomatic FAI. The patients with symptomatic cam-type FAI were unable to achieve as deep of a squat as those in the FAD and the CTRL groups, and the asymptomatic participants with FAD had significantly stronger hip extensors and greater pelvic mobility compared with patients with FAI. Future research should investigate rehabilitation and conservative treatments that focus on both strengthening hip extensor muscles and increasing pelvic mobility for their potential to reduce symptoms or even delay or avoid corrective surgery in patients with FAI.
Acknowledgment
The authors thank Kevin Dwyer, MSc, Giulia Mantovani, PhD, and K.C. Geoffrey Ng, PhD, from the Human Movement Biomechanics Laboratory, University of Ottawa, for their help with data collection, and Matthew Kennedy, MD, for providing the illustrations of the MVIC trials. The authors also thank the research staff of the Division of Orthopaedic Surgery, University of Ottawa, for help in patient recruitment and data collection.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was funded by a scholarship from Science Without Borders, Brazil (1098/13-06 to D.S.C.) and the Canadian Institutes of Health Research (97778A to M.L.). P.E.B. is a consultant for Zimmer Biomet. M.L. has received research support from Medacta and MicroPort.
Ethical approval for this study was obtained from the University of Ottawa’s Office of Research Ethics and Integrity.
References
- 1. Allen D, Beaule PE, Ramadan O, Doucette S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg Br. 2009;91(5):589–594. [DOI] [PubMed] [Google Scholar]
- 2. Bagwell JJ, Snibbe J, Gerhardt M, Powers CM. Hip kinematics and kinetics in persons with and without cam femoroacetabular impingement during a deep squat task. Clin Biomech (Bristol, Avon). 2016;31:87–92. [DOI] [PubMed] [Google Scholar]
- 3. Barton C, Salineros MJ, Rakhra KS, Beaulé PE. Validity of the alpha angle measurement on plain radiographs in the evaluation of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2011;469(2):464–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beck M, Kalhor M, Leuning M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 5. Bowman KF, Fox J, Sekiya JK. A clinically relevant review of hip biomechanics. Arthroscopy. 2010;26(8):1118–1129. [DOI] [PubMed] [Google Scholar]
- 6. Brisson N, Lamontagne M, Kennedy MJ, Beaulé PE. The effects of cam femoroacetabular impingement corrective surgery on lower-extremity gait biomechanics. Gait Posture. 2013;37(2):258–263. [DOI] [PubMed] [Google Scholar]
- 7. Byrd JWT. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med. 2014;42(3):737–751. [DOI] [PubMed] [Google Scholar]
- 8. Casartelli NC, Leunig M, Item-Glatthorn JF, Lepers R, Maffiuletti NA. Hip flexor muscle fatigue in patients with symptomatic femoroacetabular impingement. Int Orthop. 2012;36(5):967–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Casartelli NC, Maffiuletti NA, Item-Glatthorn JF, et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19(7):816–821. [DOI] [PubMed] [Google Scholar]
- 10. Colvin AC, Harrast J, Harner C, et al. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94(4):e23. [DOI] [PubMed] [Google Scholar]
- 11. Diamond LE, Van den Hoorn W, Bennell KL, et al. Coordination of deep hip muscle activity is altered in symptomatic femoroacetabular impingement. J Orthop Res. 2017;35(7):1494–1504. [DOI] [PubMed] [Google Scholar]
- 12. Emara K, Samir W, Motasem EH, El Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong). 2011;19(1):41–45. [DOI] [PubMed] [Google Scholar]
- 13. Ganz R, Gill T, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. [DOI] [PubMed] [Google Scholar]
- 14. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. [DOI] [PubMed] [Google Scholar]
- 15. Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49(4):436–441. [DOI] [PubMed] [Google Scholar]
- 16. Grammatopoulos G, Speirs AD, Ng KCG, et al. The acetabular and spino-pelvic morphologies are different in subjects with symptomatic cam femoro-acetabular impingement [published online January 11, 2018]. J Orthop Res. doi:10.1002/jor.23856 [DOI] [PubMed] [Google Scholar]
- 17. Hack K, Di Primio G, Rakhra K, Beaulé PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92(14):2436–2444. [DOI] [PubMed] [Google Scholar]
- 18. Hartofilakidis G, Bardakos N, Babis G, Georgiades G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg Br. 2011;93(5):580–586. [DOI] [PubMed] [Google Scholar]
- 19. Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361–374. [DOI] [PubMed] [Google Scholar]
- 20. Hermens HJ, Freriks B, Merletti R, et al. SENIAM 8: European Recommendations for Surface Electromyography. Enschede, the Netherlands: Roessingh Research and Development; 1999. [Google Scholar]
- 21. Horisberger M, Brunner A, Herzog RF. Arthroscopic treatment of femoroacetabular impingement of the hip: a new technique to access the joint. Clin Orthop Relat Res. 2010;468(1):182–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hunt D, Prather H, Hayes MH, Clohisy JC. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders. PM R. 2012;4(7):479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hunt MA, Gunether JR, Gilbart MK. Kinematic and kinetic differences during walking in patients with and without symptomatic femoroacetabular impingement. Clin Biomech (Bristol, Avon). 2013;28(5):519–523. [DOI] [PubMed] [Google Scholar]
- 24. Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;(429):262–271. [DOI] [PubMed] [Google Scholar]
- 25. Ito K, Minka M, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83(2):171–176. [DOI] [PubMed] [Google Scholar]
- 26. Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93(10):1303–1307. [DOI] [PubMed] [Google Scholar]
- 27. Kennedy MJ, Lamontagne M, Beaulé PE. Femoroacetabular impingement alters hip and pelvic biomechanics during gait: walking biomechanics of FAI. Gait Posture. 2009;30(1):41–44. [DOI] [PubMed] [Google Scholar]
- 28. Khanna V, Caragianis A, Diprimio G, Rakhra K, Beaulé PE. Incidence of hip pain in a prospective cohort of asymptomatic volunteers: is the cam deformity a risk factor for hip pain? Am J Sports Med. 2014;42(4):793–797. [DOI] [PubMed] [Google Scholar]
- 29. Lamontagne M, Brisson N, Kennedy MJ, Beaulé PE. Preoperative and postoperative lower-extremity joint and pelvic kinematics during maximal squatting of patients with cam femoroacetabular impingement. J Bone Joint Surg Am. 2011;93(suppl 2):40–45. [DOI] [PubMed] [Google Scholar]
- 30. Lamontagne M, Kennedy MJ, Beaulé PE. The effect of cam FAI on hip and pelvic motion during maximum squat. Clin Orthop Relat Res. 2009;467(3):645–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lamontagne M, Ng KG, Mantovani G, Catelli DS. Biomechanics of femoroacetabular impingement In: Doral M, Karlsson J, eds. Sports Injuries. Berlin: Springer; 2015:783–795. [Google Scholar]
- 32. Laude F, Boyer T, Nogier A. Anterior femoroacetabular impingement. Joint Bone Spine. 2007;74(2):127–132. [DOI] [PubMed] [Google Scholar]
- 33. Leunig M, Beaulé PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467(3):616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mantovani G, Lamontagne M. How different marker sets affect joint angles in inverse kinematics framework. J Biomech Eng. 2016;139(4). doi:10.1115/1.4034708. [DOI] [PubMed] [Google Scholar]
- 35. Martin HD, Kelly BT, Leunig M, et al. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26(2):161–172. [DOI] [PubMed] [Google Scholar]
- 36. Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27(2):252–269. [DOI] [PubMed] [Google Scholar]
- 37. Ng KC, Lamontagne M, Adamczyk AP, Rahkra KS, Beaulé PE. Patient-specific anatomical and functional parameters provide new insights into the pathomechanism of cam FAI. Clin Orthop Relat Res. 2015;473(4):1289–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ng KC, Mantovani G, Lamontagne M, Labrosse MR, Beaulé PE. Increased hip stresses resulting from a cam deformity and decreased femoral neck-shaft angle during level walking. Clin Orthop Relat Res. 2017;475(4):998–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ng KCG, Lamontagne M, Beaulé PE. Differences in anatomical parameters between the affected and unaffected hip in patients with bilateral cam-type deformities. Clin Biomech (Bristol, Avon). 2016;33:13–19. [DOI] [PubMed] [Google Scholar]
- 40. Ng KCG, Lamontagne M, Jeffers JRT, Grammatopoulos G, Beaulé PE. Anatomic predictors of sagittal hip and pelvic motions in patients with a cam deformity. Am J Sports Med. 2018;46(6):1331–1342. [DOI] [PubMed] [Google Scholar]
- 41. Nötzli H, Wyss T, Stoecklin C, Schmid M, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement: commentary. J Bone Joint Surg Br. 2002;84(4):556–560. [DOI] [PubMed] [Google Scholar]
- 42. Nussbaumer S, Leunig M, Glatthorn JF, Stauffacher S, Gerber H, Maffiuletti NA. Validity and test-retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord. 2010;11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Palmer WE. Femoroacetabular impingement: caution is warranted in making imaging-based assumptions and diagnoses. Radiology. 2010;257(1):4–7. [DOI] [PubMed] [Google Scholar]
- 44. Philippon MJ, Briggs KK, Yen YM, Kuppersmith DA. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91(1):16–23. [DOI] [PubMed] [Google Scholar]
- 45. Rakhra KS, Sheikh AM, Allen D, Beaulé PE. Comparison of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res. 2009;467(3):660–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ranawat AS, Schulz B, Baumbach SF, Meftah M, Ganz R, Leunig M. Radiographic predictors of hip pain in femoroacetabular impingement. HSS J. 2011;7(2):115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Reiman MP, Thorborg K. Femoroacetabular impingement surgery: are we moving too fast and too far beyond the evidence? Br J Sports Med. 2015;49(12):782–784. [DOI] [PubMed] [Google Scholar]
- 48. Rylander J, Shu B, Favre J, Safran M, Andriacchi T. Functional testing provides unique insights into the pathomechanics of femoroacetabular impingement and an objective basis for evaluating treatment outcome. J Orthop Res. 2013;31(9):1461–1468. [DOI] [PubMed] [Google Scholar]
- 49. Santori N, Villar RN. Arthroscopic findings in the initial stages of hip osteoarthritis. Orthopedics. 1999;22(4):405–409. [DOI] [PubMed] [Google Scholar]
- 50. Siebenrock K, Wahab K, Werlen S, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;(418):54–60. [DOI] [PubMed] [Google Scholar]
- 51. Speirs A, Beaulé P, Rakhra K, Schweitzer M, Frei H. Increased acetabular subchondral bone density is associated with cam-type femoroacetabular impingement. Osteoarthritis Cartilage. 2013;21(4):551–558. [DOI] [PubMed] [Google Scholar]
- 52. Sutter R, Dietrich TJ, Zingg PO, Pfirrmann CWA. How useful is the alpha angle for discriminating between symptomatic patients with cam-type femoroacetabular impingement and asymptomatic volunteers? Radiology. 2012;264(2):514–521. [DOI] [PubMed] [Google Scholar]
- 53. Tateuchi H, Taniguchi M, Mori N, Ichihashi N. Balance of hip and trunk muscle activity is associated with increased anterior pelvic tilt during prone hip extension. J Electromyogr Kinesiol. 2012;22(3):391–397. [DOI] [PubMed] [Google Scholar]
- 54. Wells KF, Dillon EK. The sit and reach: a test of back and leg flexibility. Res Q Exerc Sport. 1952;23(1):115–118. [Google Scholar]