Abstract
For neurological disorders, pharmacological tests have shown promising results in the reduction of side effects when using plants with known therapeutic effects in the treatment of some types of dementia. Therefore, the goals of this study are to gather data about the major medicinal plants used in the nervous system as described in ethnopharmacological surveys from South America and Brazil and to compare this data with the results from pharmacological tests on the active principles of those same plants found in the scientific literature. After collecting the data about each plant, their respective popular indication was compared with the results found through pharmacological tests. The discrepancy rate between the effects observed by ethnopharmacological and pharmacological methods in this study is greater than 50%. In conclusion, despite the importance of ethnopharmacological data, it is important to make comparisons with pharmacological tests for the same plants, since the pharmacological studies, although few, have shown a high rate of discrepancy in the results.
1. Introduction
The knowledge of medicinal plants for therapeutic purposes originated from indigenous tribal cultures [1–4] or ancient civilizations such as those once found in Iran, India, or China [1–3, 5–7] and was passed from generation to generation mostly by means of oral tradition. Presently, knowledge is commonly limited to a village and rural areas or by families isolated from urban centers [8]. Most likely, original information of plants used for therapeutic purpose underwent modifications through time. This was due to their discovery by trial and error over many generations and the oral transmission of information rather than through writing.
A previous study associated culturally propagated therapeutic effects of different medicinal plants obtained by ethnopharmacological/ethnobotanical means with those found in laboratory tests, showing approximately 66% discrepancy in the results [9]. Trading and distribution mistakes [10], similarity of plant names for different species [11], presence of impurities during preparation from other plants, insects, and mushrooms [12], and unexpected reactions and interactions with the active compounds [13] are all examples of commonly encountered problems in the therapeutic use of medicinal plants.
It is not suggested that the medicinal use of plants should be banned, decreased, or hampered. However, there is a need for each procedure to be evaluated by government agencies, institutions, and specialists who understand the therapeutic use of biodiversity in societies with an increasing interest in alternative treatments [6, 14, 15] or in populations with limited or no access to other types of therapeutic resources. Medicinal plant-based therapy may offer benefits, like decreased side effects [16–18], higher autonomy for individuals in caring for their own health [3], reduced or nonexistent costs, and easy access for social groups located in inaccessible areas or away from urban centers and for people in poor urban areas with limited or no access to a healthcare system [6, 14, 15, 19, 20]. Indeed, those groups rely on alternative therapeutic methods for their health care, especially those derived from local medicinal plants, which is a major issue in countries with higher income gaps.
Many ethnopharmacological surveys were performed in countries and regions representing the greatest biodiversity to identify plants used, with the aim of preserving the cultural heritage of the plant therapy [1–3, 5–7, 21, 22] and acquiring new active compounds for the pharmaceutical industry [8]. Brazil presents the largest biodiversity on the planet [23] and has a large amount of unexplored resources available for ethnopharmacological and herbal studies given that only 16% of Brazil's medicinal plants or just 8% of Brazilian national flora [24] has been evaluated for therapeutic potential [25]. This country represents around 47% of all territories of the South American continent.
Countries in South America present important data about medicinal plants, because of their specific locations in the Andean region, close/into the Amazon Forest [8] or the pampas. Indeed, the use of some medicinal plants was first found in the population in the Andes Ridge, in the pampas, Patagonia [10], or Brazilian's savanna (cerrado) [9]. Probably because of the large population or size, most of the studies in South America are found in Brazil, while ethnopharmacological studies are incipient in other countries in this continent [8, 10].
However, quality or reliability of medicinal plant effects cannot be ensured if ethnobotanical studies do not provide laboratory verification of the effects when prescribing compounds derived from those medicinal plants. Healthcare professionals and patients should note that studies about the correspondence or discrepancy between ethnopharmacological knowledge and laboratory tests for the same plant are lacking [9] and must be done for each class of drug.
There is a growing evidence from in vitro, animal, and clinical studies reporting that medicinal plants might be beneficial for treating various mental and neurological disorders including Alzheimer disease, depression, anxiety, and insomnia [363–366]. For neurological disorders, in particular, pharmacological tests have shown promising results in the reduction of side effects when using plants with known therapeutic effects in the treatment of some types of dementia [18, 22, 367–372]. Medicinal plants have been sought as an alternative therapy [18, 373–375] owing to the inefficacy of some industrial medications on certain diseases, such as degenerative ones. Examples are the use of Melissa officinalis, Salvia officinalis, Ginkgo biloba, and Huperzia serrata for treating the symptoms of Alzheimer disease [18, 373–375].
The problem is that, especially in developing and/or populated countries, people rely on medicinal plants as primary healthcare [376]. The situation is true for mental and neurological disorders. Patient complaints associated directly or indirectly with neurological or neuropsychiatric disorders, such as headache, insomnia, amnesia, anxiety, or depression, are very common [146, 298, 377, 378], and the use of medicinal plants for these purposes is very frequent in populated countries such as Brazil, India, and China [1–3, 5–7, 22] but without support of adequate pharmacological tests.
Considering the errors in the use and sale of alternative medicines as a whole, we hypothesize that the same errors could happen with plants that act directly on the nervous system. Therefore, the goal of this study is to gather data about the major medicinal plants used in the neural system, as described in ethnopharmacological surveys from South America like in Brazil and compare this data with the results from pharmacological tests on the active principles of those same plants found in the scientific literature. Specifically, this study intends to present reliable data for the use of medicinal plants in primary healthcare and assisting conventional treatments of neurological disorders.
2. Materials and Methods
This study was done through literature review of ethnopharmacological surveys on the medicinal plants used by groups in South America (with emphasis on Brazil) found in academic databases (MEDLINE, LILACS, Scopus, SciELO, Google Academic, and Elsevier). The terms searched were ethnobotanical studies, medicinal plants, ethnopharmacology, neural system, South America, and Brazil. The search was restricted to the most recent and classical articles/books written in Portuguese, English, or Spanish. After collecting the data about each plant, their respective popular indication was compared with the results found through pharmacological tests.
For the first phase, 55 ethnobotanical survey articles were selected and then the most commonly used plants by the population for treating neural system disorders were identified. A table was prepared with data regarding family, scientific name, part of the plant utilized, preparation method, indications, and comparison with pharmacological tests.
In the second phase, 181 articles in which pharmacological tests had been performed with the chosen plants were selected. Unfortunately, scientific tests for the proposed indication or toxicity for all the plants could not be found.
Statistical analysis was done using central tendency measures such as modal frequency.
3. Results
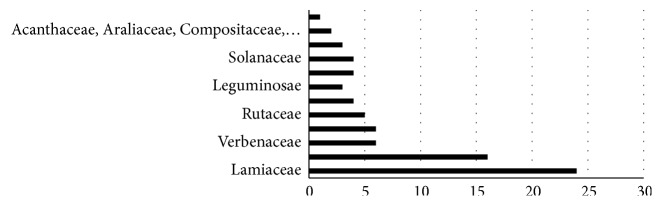
Data on South American medicinal plants that act on the nervous system was summarized by family, scientific name, part of the plant utilized, preparation method, indications, and comparison with pharmacological tests (Table 1). The most cited families were Lamiaceae (24/138), Asteraceae (16/138), and Verbenaceae (6/138), representing 33.7% of the medicinal plants analyzed (Figure 1).
Table 1.
Family names, forms of preparation, used part of the plants, medicinal effects cited by population, the pharmacological effects tested for cited plants with the references, and the divergence between the cited effects by population and pharmacological tests.
| Family Scientific name/common name |
Forms of preparation/used part | Medicinal effects cited by population | Pharmacological tests | Divergences |
|---|---|---|---|---|
| Acanthaceae | ||||
|
| ||||
| Hygrophila tyttha Leonard/Tame-male | Infusion/Part air plant | Calmative [26] | Anxiolytic effect, anticonvulsant and sedative [26] | No |
|
| ||||
| Justicia pectoralis Jacq./Anador | Decoction/Leaf | Headache [27] | Anxiolytic and depressor Neural Central System [28], analgesic and anti-inflammatory [29], estrogenic, progestagenic and anti-inflammatory effects [30], antioxidant [31] | No |
|
| ||||
| Alismataceae | ||||
|
| ||||
| Echinodorus grandiflorus (Cham. & Schltdl.) Mich./Hat leatherback | Decoction/Leaf | Analgesic [21] | Anti-inflammatory and analgesic [32, 33], diuretic [33], antihypertensive [34, 35] | No |
|
| ||||
| Amaranthaceae | ||||
|
| ||||
| Alternanthera paronychioides St-Hil./Anador | Not found/Leaf, stalk | Analgesic [36] | Antioxidant [37] | Yes |
|
| ||||
| Apiaceae | ||||
|
| ||||
| Apium graveolens L./Celery | Not found/Complete plant | Calmative [36] | Vasorelaxant and antihypertensive [38] | Yes |
|
| ||||
| Coriandrum sativum L./Coriander | Infusion/Seed | Headache [39] | Antioxidant [40], anti-inflammatory [41], antibacterial [42], anxiolytic, sedative and muscle relaxant [43], antifungal [44], hypoglycemic, hypolipidemic and hepatoprotective [45], analgesic [46] | No |
|
| ||||
| Pimpinella anisum L./Fennel | Infusion/Seed | Calmative [7, 27, 39, 47–49] | Antibacterial [50], neuroprotective and anticonvulsant [51], antiviral and immunostimulating [52], antioxidant [53], anticancer [54] | No |
|
| ||||
| Foeniculum vulgareMill./Fennel | Decoction/Stalk | Headache and calmative [13, 36, 55–60] | Antimicrobial [61], diuretic [62], antihelminthic [63], antioxidant [64], anxiolytic [65] | No |
|
| ||||
| Aquifoliaceae | ||||
|
| ||||
| Ilex paraguariensis/Erva Mate | Infusion/leaves, branches | Stimulant [66] | Stimulant [66] | No |
|
| ||||
| Araliaceae | ||||
|
| ||||
|
Didymopanax macrocarpum (C. & S.) Seem./ Five leaves |
Compress, bathe/Leaf | Analgesic [67] | Not found | Not found |
|
| ||||
| Hedera helix/Hiedra | Cataplasm/Leaf | Analgesic, neuritis, neuralgia [68] | Expectorant and antitussive [69], mucolytic and bronchodilator [70], anti-inflammatory [71] | No |
|
| ||||
| Aristolochiaceae | ||||
|
| ||||
| Aristolochia esperanzae O. Kuntze./Papo de peru, cipo-millhomem | Decoction/Complete plant | Analgesic [67] | Antiophidic activity [72], antimicrobial [73] | Yes |
|
| ||||
| Aristolochia gilbertii Hook/Milhomem | Infusion/Root | Headache [7] | Not found | Not found |
|
| ||||
|
Aristolochia melastoma Manso ex. Duchtra/Capitãozinho |
Decoction/Root, leaf | Sedative [67] | Not found | Not found |
|
| ||||
| Asteraceae | ||||
|
| ||||
| Achillea millefolium L./Ponta-alívio | Decoction/Complete plant | Calmative, analgesic [21, 36, 47, 57, 74, 75] | Immunostimulating [76] | Yes |
|
| ||||
| Achyrocline satureioides D.C./Macela | Infusion/Flower | Sedative, calmative, headache [56, 67, 75, 77, 78] | Anticancer [79], calmative effect, anti-inflammatory and antispasmodic [80], antiviral [81] | No |
|
| ||||
| Artemisia absinthium L./Losna | Decoction/Leaf | Analgesic [21, 82] | Anticancer [83], antifungal [84], antibacterial [85], antileishmanial [86] | Yes |
|
| ||||
| Artemisia camphorata Vill./Camphor | Infusion/Leaves | Calmative [58] antiepileptic [87] | Not found | Not found |
|
| ||||
| Artemisia vulgaris L./Artemisia | Not found | Headache [88] | Antifungal [89] | Yes |
|
| ||||
| Chamomilla recutita (L.) Rauschter/Camomile | Infusion/Flower | Calmative, sedative [36, 39, 48, 57, 90–92] | Antibacterial and anti-inflammatory [92, 93], gastroprotection [94], antihyperglycemic and antioxidant [95] | Yes |
|
| ||||
| Chrysanthemum parthenium Bernhadi/Artemisia | Decoction, infusion/Leaves | Calmative [78] | Not found | Not found |
|
| ||||
| Cynara scolymus L./Artichoke | Not found | Calmative [74] | Diuretic [96], prolonged satiety sensation and hypoglycemic [97], antioxidant [98] | Yes |
|
| ||||
| Lactuca sativa L./Lettuce | In nature, infusion/Leaves, root | Calmative, sedative [74, 99] | Antioxidant [100] | Yes |
|
| ||||
| Matricaria chamomilla L./Camomile | Infusion/Leaves | Calmative [56, 75, 78, 101, 102] | Antibacterial and antioxidant [103] | Yes |
|
| ||||
| Mikania hirsutissima DC./Cipó-cabeludo | Not found | Calmative [67, 104] | Antiophidic activity and antidiarrheal [105] | Yes |
|
| ||||
| Solidago chilensis Meyen/Arnica | Compress/Complete plant | Analgesic [106] | Anti-inflammatory [107] | Yes |
|
| ||||
| Spilanthes oleracea/Anestesiol | Not found | Anesthetic [108] | Peptic antiulcer and contraception [109] | Yes |
|
| ||||
| Tanacetum sp./Macelinha | Decoction/Complete plant | Analgesic [23] | Not found | Not found |
|
| ||||
| Tanacetum vulgare L./Catinga-de-mulata | Decoction, maceration/Leaves | Analgesic [23] | Antibacterial and antifungal [110], antiviral [111], cytotoxic [112], treatment of infections caused by Trypanosoma cruzi and Leishmania amazonensis [113], immunomodulatory [114], antihelminthic [115] | Yes |
|
| ||||
| Vernonia cf. condensata Baker./Boldo do chile | Infusion/Bark | Calmative [57] | Antitumor and anti-inflammatory [116], antioxidant [117] | Yes |
|
| ||||
| Bignoniaceae | ||||
|
| ||||
| Anemopaegma arvense/Catuaba | Infusion, decoction/Root, bark, leaves | Nervous exhaustion [118] | Increased weight and testicular parenchyma [119], antifungal [120] | Yes |
|
| ||||
| Bombacaceae | ||||
|
| ||||
| Eriotheca candolleana (K. Schum.)/Catuaba | Infusion/Root | Nervous exhaustion [121] | Not found | Not found |
|
| ||||
| Boraginaceae | ||||
|
| ||||
| Cordia verbenacea DC./Maria preta | Bathe/Leaves | Analgesic [49] | Antimicrobial [122], anti-inflammatory [123] | No |
|
| ||||
| Brassicaceae | ||||
|
| ||||
|
Coronopus didymus (L.) Smith/Mastruz |
Maceration/Leaves | Analgesic [49] | Healing [124], anti-inflammatory [125] | No |
|
| ||||
| Bromeliaceae | ||||
|
| ||||
| Tillandsia usneoides (L.) L/Barba de velho | Not found | Antiepileptic [49] | Abortion [126], antiviral [127] | Yes |
|
| ||||
| Buddlejaceae | ||||
|
| ||||
| Buddleja brasiliensis Jacq./Verbasco | Infusion, cataplasm/Part air plant | Calmative [67] | Low potential hemolytic [128] | Yes |
|
| ||||
| Burseraceae | ||||
|
| ||||
| Commiphora myrrha (T. Nees) Engl/Myrrh | Infusion/Leaves | Calmative [49] | Antioxidant [117], analgesic [129] | Yes |
|
| ||||
| Caesalpiniaceae | ||||
|
| ||||
| Bauhinia forficata Link./Pata de vaca | Decoction/Leaves | Analgesic [23] | Antioxidant and increased liver glycogen [130], antimutagenic [131] | Yes |
|
| ||||
| Bauhinia rutilans Spruce ex. Benth/Escada-de-macaco | Infusion/Part air plant | Analgesic [99] | Not found | Not found |
|
| ||||
| Canellaceae | ||||
|
| ||||
| Capsicodendron dinissi Occhioni/Pepper | Not found | Migraine [104] | Not found | Not found |
|
| ||||
| Capparaceae | ||||
|
| ||||
| Cleome spinosa Jacq./Mussambê | Infusion/Complete plant | Headache [132] | Cytotoxic [49], antioxidant [133], anti-inflammatory and antinociceptive [134] | No |
|
| ||||
| Caprifoliaceae | ||||
|
| ||||
| Sambucus nigra L./Elderberry | Decoction/Leaves | Analgesic [23, 49] | Anti-inflammatory and antioxidant [134], parasiticidal [135] | No |
|
| ||||
| Chenopodiaceae | ||||
|
| ||||
| Chenopodium ambrosioides L./Yerba Santa Maria | Maceration, infusion/Leaves, bark, seed | Analgesic, calmative [23, 48, 57] | Antitumor [79], hypotensive [136], antipyretic and anxiolytic [137] | Yes |
|
| ||||
| Compositaceae | ||||
|
| ||||
| Baccharis trimera (Less) D.C./Gorse | Infusion/Leaves | Headache [138] | Antiulcer and antioxidant [139], anti-inflammatory [140], anti-inflammatory and analgesic [141] | No |
|
| ||||
| Vernonia condensata B./Boldo | Infusion, decoction/Leaves | Calmative [138] | Antioxidant [117], analgesic [142] | Yes |
|
| ||||
| Cucurbitaceae | ||||
|
| ||||
| Cayaponia tayuya (Vell.) Cogn./Taiuia | Infusion, decoction/Root | Neuralgia [67] | Hepatotoxic [142], anti-inflammatory [143] | Yes |
|
| ||||
| Dilleniaceae | ||||
|
| ||||
| Davilla rugosa Poir./Vine cabloco | Bathe/Root | Sedative [67] | Antioxidant [144], antiulcer [145] | Yes |
|
| ||||
| Euphorbiaceae | ||||
|
| ||||
| Jatropha curcas L./Pião-bravo | Infusion/Seed | Headache [102, 132] | Acetylcholinesterase inhibitor [146], antibacterial, antioxidant and antitumor [147, 148], cytotoxic [149] | Yes |
|
| ||||
| Ricinus communis L./Castor beans | Infusion/Leaves | Headache [77, 87] | Antimicrobial and anticancer [150], antimicrobial [151] | Yes |
|
| ||||
| Fabaceae | ||||
|
| ||||
| Caesalpinia ferrea Mart. ex. Tul./Pau ferro | Not found | Analgesic [57] | Nutritional supplementation of iron, zinc and manganese [152] anti-inflammatory and healing [153], antihyperglycemic [154], antimicrobial [155] | No |
|
| ||||
| Cajanus flavus De Candolle/Andu beans | Infusion/Leaves | Headache [99] | Not found | Not found |
|
| ||||
| Erythrina falcata Benth/Surina, mulungu | Not found | Sedative and antiepileptic [67, 104] | Depressant CNS [156] | No |
|
| ||||
| Indigofera anil/Anil | Not found | Sedative [107] | Not found | Not found |
|
| ||||
| Indigofera suffruticosa Mill./Anileira | Decoction, infusion/Complete plant | Sedative [67] | Anti-inflammatory [157], lectin activity [158], antiepileptic [159], antiparasitic [160] | Yes |
|
| ||||
| Pterodon emarginatus/Sucupira | Infusion/leaves, fruit | Headache [120] | Antimicrobial [161–163], analgesic and anti-inflammatory [164]; antileishmanial, anticancer, hypoglycemic [165] | No |
|
| ||||
| Ginkgoaceae | ||||
|
| ||||
| Ginkgobiloba/Ginco | Decoction, infusion/Leaves | Vasodilator, brain dysfunction, dizziness and concentration and memory [160] | Treatment of Alzheimer disease [166], prevention of dementia [167], antioxidant, vasodilator, stimulant of SNC [168] | No |
|
| ||||
| Geraniaceae | ||||
|
| ||||
|
Pelargonium graveolens L'Her/ Mauve smelling |
Not found | Sedative [87] | Anxiolytic and antidepressant [159], antibacterial [169], hypoglycemic and antioxidant [170] | No |
|
| ||||
| Mimosa pudica L./Dormideira | Infusion/Complete plant | Sedative [99] | Reduction of fertility [171], hepatotoxic [172], lipid-lowering [173], anxiolytic and antipyretic [137], antiophidic [174] | No |
|
| ||||
| Iridaceae | ||||
|
| ||||
| Calydorea sp./Jabotitana | Decoction/Rhizome | Analgesic [23] | Not found | Not found |
|
| ||||
| Labiatae | ||||
|
| ||||
| Agastache mexicana Kunth/Toronjil | Not found | Sedative [102] | Antihypertensive [175], vasorelaxant [176], anti-inflammatory and antinociceptive [177], antinociceptive [178], anxiolytic [179] | No |
|
| ||||
| Lavandula latifolia/Lavanda | Oil | Stimulant [68] | Anxiolytic [180], antifungal [181], antioxidant [182] | Yes |
|
| ||||
| Origanum vulgare/oregano | Infusion/Leaf | Sedative [68] | Antimicrobial [183] proapoptotic effect and cytotoxic [184], antiurolithic [185] | Yes |
|
| ||||
| Lamiaceae | ||||
|
| ||||
| Coleus barbatus Benth./Falso-boldo | Tisane mate/Leaf | Headache, calmative [56] | Hepatoprotective [186] | Yes |
|
| ||||
| Cunila microcephala Benth./Hortelã-miúdo, hortelã-pimenta, poejo | Decoction/Complete plant | Analgesic [23, 58] | Anti-inflammatory and antioxidant [187] | No |
|
| ||||
| Hyptis suaveolens Poit./Samba-coité | Tea/Leaf | Headache [188] | Hypoglycemic and antioxidant [189], hepatoprotective and antioxidant [190], gastroprotective activity [191], neuroprotective and antioxidant [192], antifungal [193] | Yes |
|
| ||||
| Lavandula officinalis Chaix & Kitt/Alfazema | Tea/Leaf, stalk | Calmative [49] | Antimicrobial [194], antioxidant [195], sedative and hypnotic [196] | No |
|
| ||||
| Leonotis nepetifolia (L.) R. Br./Cordão de São Francisco | Infusion, decoction/Leaf, branches | Sedative, headache [132, 138] | Antimicrobial [197], anti-inflammatory [198] | Yes |
|
| ||||
| Melissa officinalisL./Erva-cidreira, melissa | Decoction/Leaf | Calmative, migraine, sedative [23, 36, 55, 58, 59, 87, 89, 90, 101, 102, 138, 199] | Anti-inflammatory [200], calmative [201], antioxidant [202], antigenotoxic and antimutagenic [203], neuroprotective [199, 204] | No |
|
| ||||
| Mentha arvensis L./Hortelã-mentol | Tea/Leaf | Headache [188] | Antibacterial [205], antifungal [206], anti-inflammatory and sedative [207], peptic antiulcer [208] | Yes |
|
| ||||
| Mentha cf. suaveolens Ehrh./Hortelã, hortelã-grande | Decoction, maceration/Leaf | Calmative, Analgesic [23, 199] | Antifungal [209, 210], antioxidant [211], antibacterial [212] | Yes |
|
| ||||
| Mentha piperita L./Hortelã, hortelã-roxo | Decoction/Complete plant | Analgesic [23, 102] | Antifungal [213, 214], antioxidant [211], anthelmintic [215], hypoglycemic and hypolipidemic [216], anticancer [217] analgesic [218] | No |
|
| ||||
| Mentha pulegium L./Poejo | Decoction/Stalk | Calmative, sedative [47, 56, 58, 78] | Antioxidant [211], antimicrobial [219] | Yes |
|
| ||||
| Mentha sp./Hortelã | Decoction/Stalk | Headache, Calmative [36, 47, 49, 55–57] | Anthelmintic [215] | Yes |
|
| ||||
| Mentha spicata L./∗ | ∗∗∗ | Headache [87] | Hypoglycemic and hypolipidemic [216], antioxidant [220], antiemetic [221] | Yes |
|
| ||||
| Mentha × villosa Huds./Hortelã | Tea/Leaf | Headache [188] | Antifungal and antibacterial [222], antimicrobial and antioxidant [223], analgesic and antispasmodic [153] | No |
|
| ||||
| Ocimum basilicum L./Alfavaca | Decoction, maceration/Leaf | Calmative, analgesic [23, 39] | Antidepressant and anticonvulsant [224] | Yes |
|
| ||||
|
Ocimum gratissimum L./l Louro |
Tea/Leaf | Headache, calmative [49, 87, 188] | Anticonvulsant [225, 226], antifungal [227] | Yes |
|
| ||||
| Ocimum minimum L./Manjericão | Maceration/Leaf | Headache [94] | Antiulcerogenic and antioxidant [35] | Yes |
|
| ||||
| Ocimum selloi Benth./Alfavaca | Infusion, tea/Leaf | Calmative [138] | Antibacterial [219], analgesic and antidiarrheal [220] | Yes |
|
| ||||
| Origanum majoranaL./Manjerona | Decoction/Stalk | Calmative [56] | Antibacterial [228], antioxidant [49], antimetastatic and antitumor [229], antihyperglycemic and antihyperlipidemic [230] | Yes |
|
| ||||
| Plectranthus barbatus Andr./Boldo | Decoction, maceration/Leaf | Analgesic [23, 57, 60] | Cytotoxic [231], acetylcholinesterase inhibitor [232], antimicrobial [233] | Yes |
|
| ||||
| Plectranthus neochilus Schlechter/Boldo do Chile | Infusion/Leaf | Headache [89] | Analgesic [234] | No |
|
| ||||
| Rosmarinus officinalis L./Alecrim | Decoction/Leaf | Analgesic, calmative [23, 39, 48, 58, 59, 102, 138, 235] | Antibacterial [236], antioxidant [237], antifungal [238], anticancer [239], antidepressant [240], analgesic [241], antioxidant, anti-inflammatory, metal chelation [242], prevention and treatment of dementia [243], neuroprotective [244] | No |
|
| ||||
| Salvia lachnostachys Benth./Melissa | Decoction/Leaf | Somniferous [23, 78] | Anti-inflammatory and analgesic [244] | Yes |
|
| ||||
| Salvia lavandulifolia Vahl./Mariselva | Oil/∗∗ | Nervous disorders [245] | Hypoglycemic [245], neuroprotective [246] | No |
|
| ||||
| Salvia officinalis L./Salvia, barcelona | Decoction/Leaf | Calmative, Analgesic [23] | Antibacterial [228], anti-inflammatory [247], antidiarrheal and antispasmodic [185], analgesic and anti-inflammatory [248] | No |
|
| ||||
| Lauraceae | ||||
|
| ||||
| Cinnamomum zeylanicum Breyn./Canela | Infusion, maceration/Stalk | Calmative [39] | Antifungal [249] antimicrobial [250], antioxidant [251], antidiabetic [252] | Yes |
|
| ||||
| Nectandra megapotamica (Spreng.) Mez/Canela-preta | Infusion/leaf | Calmative [253] | Anesthetic [254] | Yes |
|
| ||||
| Leguminosae | ||||
|
| ||||
| Acosmium subelegans (Mohlenbr) Yakovl/Perobinha do campo | ∗∗∗ | Sedative, epilepsy and nervous exhaustion [255] | Depressant effect SNC and anticonvulsant [255] | No |
|
| ||||
| Hymenaea courbaril L./Jatobá | Infusion, maceration/Bark, fruit | Sedative [132] | Not found. | Not found |
|
| ||||
| Tamarindus indica/Tamarindo | Compress, bathe, infusion/Stalk, leaves, fruit | Treatment of fever, stomach upset, diarrhea, jaundice and as skin cleansers [256], inflammation, urinary tract infection and laxative [257], headache and stress [258] | Antibacterial [256], antihelminthic [257], antioxidant [259], antinociceptive [260], analgesic and anti-inflammatory [261], antihistaminic and antianaphylactic [262], antiulcer [263] | No |
|
| ||||
| Liliaceae | ||||
|
| ||||
| Allium sativum L./Alho | ∗∗∗ | Headache [59] | Hypotensive [264], synergism with antibiotics [265], antioxidant [266] | Yes |
|
| ||||
| Malpighiaceae | ||||
|
| ||||
|
Banisteriopsis caapi/Mariri, ayahuasca |
Decoction, infusion/vine | Hallucinogen, emotional and cognitive sensory changes, psychoactive [267–269] aid in treatment of abuse of other Psychoactives [270] | Hallucinogen [271] inhibiting the reuptake of serotonin, in addition to inhibiting MAO [272] | No |
|
| ||||
| Galphimia glauca/Amarilla | Maceration/Part air plants | Calmative [273] | Anxiolytic [273] | No |
|
| ||||
| Meliaceae | ||||
|
| ||||
| Cedrela fissilis/Cedro-rosa | Infusion/Bark | Headache [121] | Not found | Not found |
|
| ||||
| Moraceae | ||||
|
| ||||
| Cannabis sativa/maconha, marijuana, cânhamo | Oil, inhalation/Leaves, stalk, flowers | Treatment of pain, nausea and vomiting, multiple sclerosis and other neurological disorders, loss of appetite and eating disorders, Insomnia, anxiety and depression, neuroprotective action [274], antiemetic, appetite stimulant [275], clinical and experimental studies in the treatment of dementias [276], schizophrenia, antipsychotic, anxiety [277], antipsychotic [278] | Treatment of pain, nausea and vomiting, multiple sclerosis and other neurological disorders, loss of appetite and eating disorders, Insomnia, anxiety and depression, neuroprotective action [273], antiemetic, appetite stimulant [274], clinical and experimental studies in the treatment of dementias [275], schizophrenia, antipsychotic, anxiety [276], antipsychotic [277], psychoactive [278] | No |
|
| ||||
| Dorstenia brasiliensis Lam./Carapiá | Cataplasm/Rhizome | Anesthetic [67] | Anti-inflammatory [278] | Yes |
|
| ||||
| Myrtaceae | ||||
|
| ||||
| Eucalyptus globulus Labill./Eucalipto | Infusion, Bathe/Leaf | Headache [48] | Toxic effect [279], antibacterial [280, 281] | Yes |
|
| ||||
| Eugenia uniflora L./Pitangueira | Decoction/Leaf | Calmative [23, 282] | Antimicrobial and antioxidant [283], anti-Trypanosoma cruzi [206] | Yes |
|
| ||||
| Orchidaceae | ||||
|
| ||||
| Vanilla planifolia Jack. ex Andrews/Baunilha | ∗∗∗ | Calmative [67] | Not found | Not found |
|
| ||||
| Oxalidaceae | ||||
|
| ||||
| Averrhoa Carambola L./Carambola | Infusion/Leaf | Analgesic [99] | Analgesic [284] | No |
|
| ||||
| Papaveraceae | ||||
|
| ||||
| Papaver somniferum/Planta do ópio | ∗∗∗ | Analgesic and sedative [68] | Not found | Not found |
|
| ||||
| Passifloraceae | ||||
|
| ||||
| Passiflora alata Curtis/Maracujá | Fruit | Calmative [55, 59, 77, 90] | Sedative [285] | No |
|
| ||||
| Passiflora caerulea L./Maracujá | Infusion/Part air plant | Sedative and calmative [91, 286] | Anxiolytic [287] | No |
|
| ||||
| Passiflora edulis Sims./Maracujá | Tea/Leaf | Calmative and insomnia [39, 48, 74, 77, 78, 90, 99, 257] | Anxiolytic [288] | No |
|
| ||||
| Passiflora miersii Mart./Maracujazinho | Infusion/Leaf | Calmative and antidepressant [67] | Not found | Not found |
|
| ||||
| Pedaliaceae | ||||
|
| ||||
| Sesamum orientale L./Gergelim | Seed/Juice | Anticonvulsant [99] | Hypoglycemic [289] | Yes |
|
| ||||
| Phytolaccaceae | ||||
|
| ||||
| Petiveria alliacea L./Guiné, tira capeta | Decoction/Complete plant | Analgesic [23, 74, 99, 290] | Antimicrobial [291], antinociceptive, sedative, anticonvulsant and depressant [292] | Yes |
|
| ||||
| Piperaceae | ||||
|
| ||||
| Pothomorphe umbellata Miq./Pariparoba | Infusion/Leaf | Headache [121] | Antioxidant [293], antitumor [294], antihelminthic [295] | Yes |
|
| ||||
| Poaceae | ||||
|
| ||||
| Cymbopogon citratusStapf./Capim santo, capim limão | Decoction/Leaf | Calmative, analgesic and sedative [7, 23, 27, 36, 39, 47–49, 55–58, 74, 77, 78, 88–90, 99, 101, 102, 138, 296] | Anxiolytic, sedative and anticonvulsant [297] | No |
|
| ||||
| Polygalaceae | ||||
|
| ||||
| Polygala paniculata L./Arnica | Decoction/Complete plant | Analgesic [23] | Analgesic and antidermatogenic [298], antinociceptive and gastric cytoprotective activity [299] | No |
|
| ||||
| Polygonaceae | ||||
|
| ||||
| Homalocladium platycladum Bailey/Carquejinha | Decoction/Stalk | Analgesic [23] | Antibacterial [300], analgesic, anti-inflammatory [301] | No |
|
| ||||
| Rosaceae | ||||
|
| ||||
| Rosa centifolia L./Rosa branca | Decoction/Leaf, flower | Analgesic [23] | Anti-inflammatory and antiarthritic [302], antioxidant [303], antiulcer and cytoprotective [304] | No |
|
| ||||
| Sanguisorba minor Scop./Pimpinela | Tea/Leaf, flower | Calmative [102] | Inhibitory action of acetylcholinesterase [305] | Yes |
|
| ||||
| Rubiaceae | ||||
|
| ||||
| Coffea arabica L./Café | Cataplasm/Leaf | Headache [101] | Antioxidant [306], antioxidant and stimulant [307] | Yes |
|
| ||||
| Cinchona officinalis L./∗ | Decoction/Bark | Analgesic [23] | Not found | Not found |
|
| ||||
| Psychotria viridis/chacrona, ayahuasca | Infusion/Leaves | Hallucinogen, emotional and cognitive sensory changes, psychoactive [267–269] aid in treatment of abuse of other Psychoactives [268] | Hallucinogen [308] | |
|
| ||||
| Alibertia sp./Marmelo | Decoction, infusion/Root, fruit | Calmative [118] | Not found | Not found |
|
| ||||
| Rutaceae (5) | ||||
|
| ||||
| Casimiroa edulis Llave & Lex./Zapote blanco | ∗∗∗ | Sedative [102] | Vasodilator [309, 310], anticoagulants and antimicrobial [310], anxiolytic [311], anxiolytic and antidepressant [312] | No |
|
| ||||
| Citrus aurantium L./Laranja | Decoction/Bark | Headache and calmative [36, 48, 56, 59, 78, 90, 194] | Low toxicity [313], anxiolytic [314, 315] | Yes |
|
| ||||
| Citrus limon (L.) Burm. f./Limão-galego, | ∗∗∗ | Calmative and sedative [90, 194] | Neuroprotective activity and anticonvulsant [316] | Yes |
|
| ||||
| Citrus sinensis (L.) Osbeck | Infusion/Leaf | Calmative, analgesic and sedative [23, 27, 49, 74, 99, 138] | Antioxidant, antithyroid and antihyperglycemic [317] | Yes |
|
| ||||
| Ruta graveolens L./Arruda | Decoction, maceration/Leaf | Calmative and headache [23, 39, 48, 57, 60, 102] | Antimicrobial [318], antioxidant [319], antitumor [320], antinociceptive, anti-inflammatory and antipyretic [321] | Yes |
|
| ||||
| Solanaceae | ||||
|
| ||||
| Atropa belladonna L./Beladona | Decoction/Leaf | Calmative [23] | Healing [322] | Yes |
|
| ||||
| Cestrum sendtnerianum Mart./Guiné-do-campo | Infusion, Decoction/Leaf | Sedative [67] | Not found | Not found |
|
| ||||
| Solanum americanum Mill./Maria-pretinha | Decoction/Leaf, Stalk | Sedative, Analgesic [45, 67] | Antifungal [323], antioxidant and anticancer [324] | Yes |
|
| ||||
| Solanum cernuum Vell/Pata de mono | ∗∗∗ | Calmative [87] | Antiulcerogenic [325] | Yes |
|
| ||||
| Umbelliferae | ||||
|
| ||||
| Anethum graveolens/Eneldo | ∗∗∗ | Sedative [68] | Antifungal [326], anticonvulsant [327], anti Helicabator pylori [328], decreased fertility rate [329], participates in the regulation of Diabetes Mellitus [330] | Yes |
|
| ||||
| Coriandrum sativum/Cilantro | Infusion/Leaf, fruit | Stimulant [68] | Antioxidant [40], sedative and muscle relaxant [43], antibacterial [331], antiarthritic [332], anti-inflamatory [41], antifungal [333], hypoglycemic and hypolipidemic [334] | Yes |
|
| ||||
| Petroselinum hortense/Salsa da horta | ∗∗∗ | Sedative [107] | Diuretic and hypotensive [335] | Yes |
|
| ||||
| Urticaceae | ||||
|
| ||||
| Urera baccifera (L.)/Urtiga | Leaf | Analgesic [36] | Antioxidant [336], anti-inflamatory [337] | No |
|
| ||||
| Verbenaceae (6) | ||||
|
| ||||
| Aloysia citrodora Palau/Erva luíza | ∗∗∗ | Calmative [74, 286] | Not found. | Not found |
|
| ||||
| Aloysia triphylla Royle/Cidrão | ∗∗/Leaf | Sedative [55, 235] | Treatment of intestinal disorders [338], anti Trypanosoma Cruzi [339], anti-Helicobacter pylori [328], antibacterial [340], spasmolytic and anti-inflammatory [341], antinociceptive [244] | Yes |
|
| ||||
| Lantana camara L./Camará | Infusion, Decoction/Leaf | Headache [132] | Antibacterial [342], antioxidant [343], anxiolytic [344] | Yes |
|
| ||||
| Lippia alba (Mill.) N.E. Br./Erva-cidreira | Leaf/Infusion | Headache and calmative [39, 49, 55, 58–61, 75, 77, 94, 97] | Antimicrobial [345], antispasmodic [346], anxiolytic [347], anesthetic [348] | No |
|
| ||||
| Lippia gracillis Schauer/Alecrim da serra | Infusion/Leaf | Headache [132] | Antimicrobial [349], antitumor [350], anti-inflammatory and healing [351] | Yes |
|
| ||||
| Verbena cf. minutifolia Phil./∗ | Decoction/Complete plant | Analgesic [23] | Not found | Not found |
|
| ||||
| Violaceae | ||||
|
| ||||
| Viola odorata L./ | ∗∗∗ | Sedative [87] | Antitumoral [352], antioxidant and antibacterial [353], antimicrobial [354], vasodilator and antidyslipidemic [355] | Yes |
|
| ||||
| Zingiberaceae | ||||
|
| ||||
| Alpinia zerumbet (Pers.) Burtt & Smith/Colônia | Decoction/Leaf | Calmative [39, 48, 49, 101] | Hypotensive [356], vasodilator [357], antioxidant [358] | Yes |
|
| ||||
| Zingiber officinale Rosc./Gengibre | Decoction/root | Analgesic and headache [23, 57, 78] | Antioxidant [359], antihyperglycemic [360], antibacterial [361], androgenic [362] | Yes |
|
| ||||
| Costus brasiliensis Schum./Cana-de-macaco | Not found | Calmative [67] | Not found | Not found |
∗It is the popular name that was quoted. ∗∗It was not mentioned how to prepare. ∗∗∗It is the portion used or how to prepare that was quoted.
Figure 1.
The cited families of medicinal plants according to popular knowledge.
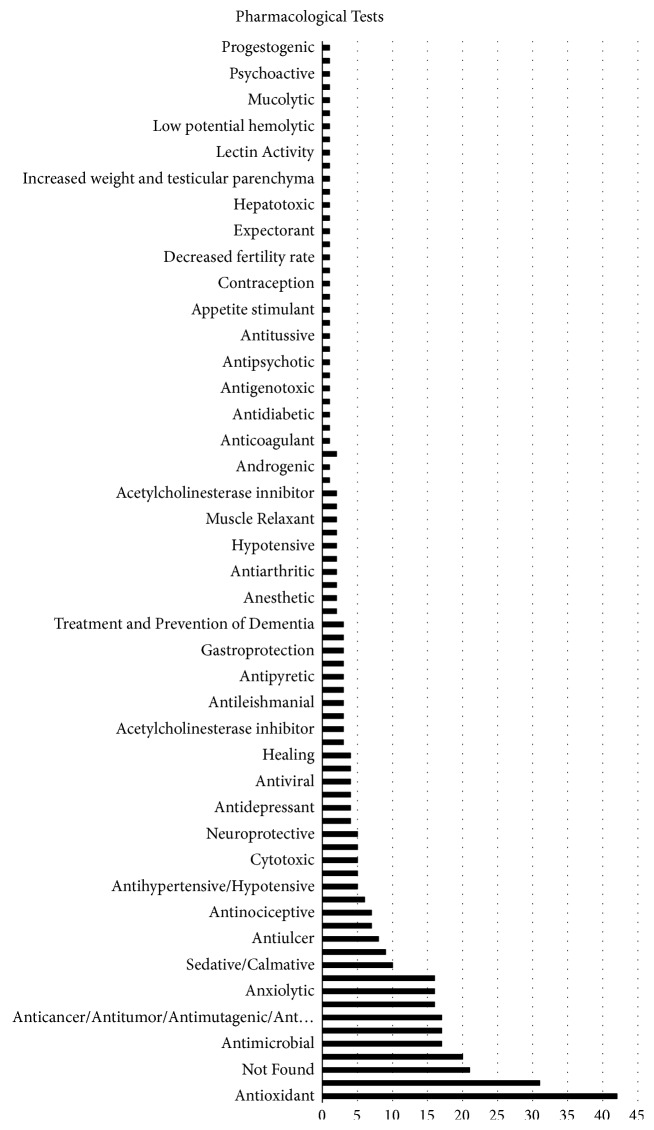
The most common indications, according to ethnopharmacological surveys, were calmative/sedative (72/167), analgesic (39/167), and headache (35/167), representing 86,2% of all indications (Figure 2).
Figure 2.
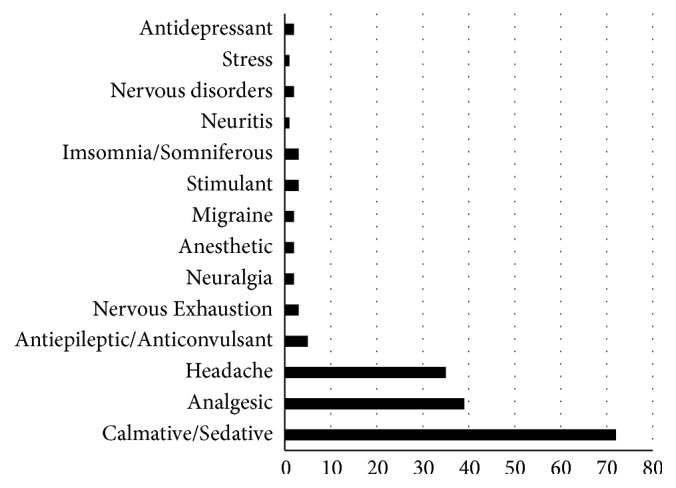
The indications for use of the medicinal plants according to popular knowledge.
Ethnobotanical surveys revealed that the leaves (70/160) and the whole plant (13/160) amounted to 51.7% of all plant parts most commonly used, but, in 18% of the studied plants, there were no citations about the used part for making medicines (Figure 3).
Figure 3.
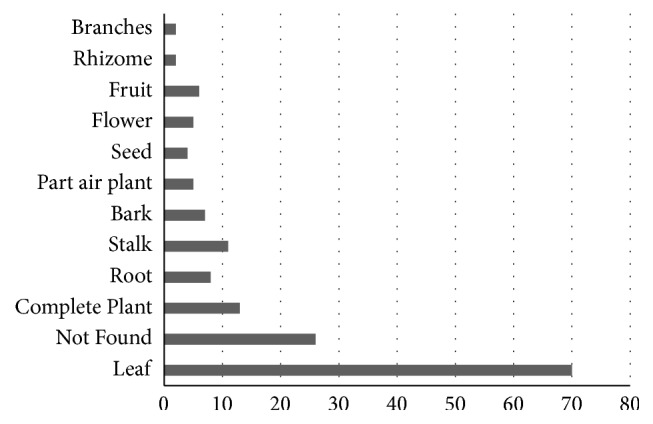
Part of plants used for indications according to the popular knowledge.
The most common preparation methods provided in the surveys were infusion (59/167) and decoction (49/167), representing 63.7% of all the methods (Figure 4).
Figure 4.
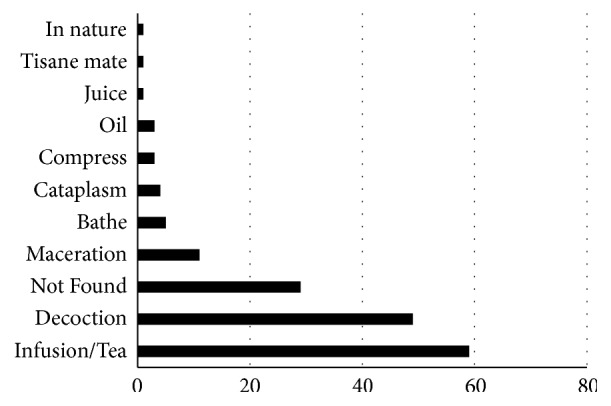
Preparation methods cited by population for medicinal plants.
Common effects attributed to the plants in the ethnopharmacological surveys were antioxidant (42/401), anti-inflammatory (31/401), antibacterial (20/401), and antimicrobial (17/401), totaling 31.9% (Figure 5).
Figure 5.
Attributed effects of the medicinal plants according to popular knowledge.
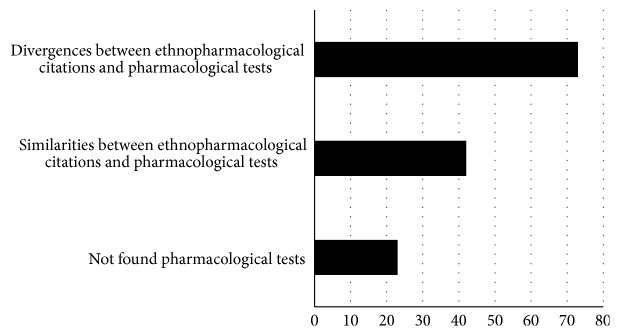
Comparison between ethnopharmacological data and pharmaceutical tests for the same plants and compounds found differences in 52.9% (73/138) of the cases and similarities in 30.4% (42/138) (Figure 6). No pharmacological tests were found for 16.9% (23/138) of the plants mentioned in the ethnopharmacological surveys (Table 1).
Figure 6.
Comparison between ethnopharmacological data and pharmaceutical tests for the same plants and compounds.
Table 1 shows a list of the medicinal plants analyzed in this study. The pharmacological effects including “anticonvulsant” and “anxiolytic” were considered to correspond to “calmative” in medicinal effects cited by population since both effects are attributed to the same action in the neural system, that is, inhibitory action. Furthermore, the pharmacological effect “anti-inflammatory” was also considered to correspond to “analgesic” in medicinal effects cited by population since anti-inflammatory agents are effective in treating pain diseases.
4. Discussion
The most frequent indications of medicinal plant use for neural system disorders in our survey (i.e., calmative, analgesic, headache, and insomnia) are associated with the most common occurrences seen in medical practice [7, 36, 47, 55, 68, 77, 104, 132, 235, 258] (Figure 2).
The plant families analyzed (Lamiaceae and Asteraceae) are in accordance with general ethnobotanical studies [4, 7, 379–382] (Figure 1), as well as the most utilized plant parts (leaves) [1, 7, 379, 383, 384], and preparation methods (infusion and decoction) [7, 253, 379, 383, 384] (Figure 4).
Despite that, the frequency of effects observed by most pharmacological tests does not coincide with those reported for the same plants when analyzed by ethnopharmacological means, (i.e., antioxidant, anti-inflammatory, antibacterial, and antimicrobial), demonstrating a high discrepancy between proven and popularly mentioned effects (Figure 6).
It is important to remember that results of pharmacological tests were not found for all the plants mentioned in the ethnopharmacological studies, although those represent a small minority (16.9%) (Figure 5).
The discrepancy rate between the effects observed by ethnopharmacological and pharmacological methods in this study is in agreement with a previous study [9] and, in both cases, a disagreement of over 50% was found. This data indicates the need for better control in the use of medicinal plants as a whole, especially in countries with a large proportion of economically backward population where such therapy is most common, such as China, India, and Brazil. However, there are possibilities that scientific studies are not enough or they are missing to corroborate the ethnopharmacological activities.
Tables like the one produced in this study can be used as a basis for the indication of medications for health professionals working in the neural area who choose to substitute alternative therapies with conventional methods. The tables can be used to maintain the patient's health and help make these treatments more accessible to people of all economic levels [385], bring medical practice closer to the care of cultural groups [386], and expand the idea of wholeness in healthcare.
Performing pharmacological tests in the medicinal plants mentioned in ethnopharmacological studies will help avoid prescription errors based only on popular knowledge, which, despite the importance, exhibits extensive methodological shortcomings from its propagation through generations (see Introduction). Although the pharmacological tests cannot solve problems related to contamination during preparation and/or mistakes when identifying plants by unskilled people, performing those tests would decrease the problems caused by adverse effects and wrong prescriptions.
Neurological disorders present complex etiologies often with aggravating social influences, requiring special care when making prescriptions; many critically ill patients are secluded from society and require medical monitoring and medications derived from modern pharmaceutical technology since indications for complex etiologies like dementias were not addressed in the ethnopharmacological articles analyzed in this study.
In conclusion, despite the importance of ethnopharmacological data, it is important to make comparisons with pharmacological tests for the same plants, since the pharmacological studies, although few, have shown a high rate of discrepancy in the results, nevertheless, to be important to cite that the scientific studies could not be enough, or are missing, to corroborate the ethnopharmacological activities. Tables containing the plants names and their effects according to pharmacological tests should be consulted by health professionals before prescribing those medications. No medicinal plants were mentioned in ethnopharmacological data for treating complex etiology neural disorders such as dementia, indicating the need for new studies of broader geographical amplitude and pharmaceutical classes all around the world. Emphasis of these studies should occur in developing countries in order to decrease prescription errors associated with medicinal plants and increase the coverage of plant-based therapy for the global population while prioritizing people in need.
Acknowledgments
Tales Alexandre Aversi-Ferreira acknowledges CNPq, Brazil, for scholarship in productivity research.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Garlet T. M. B., Irgang B. E. Medicinal plants used in folk medicine by rural women workers in Cruz. Revista Brasileira de Plantas Medicinais. 2001;4(1):9–18. [Google Scholar]
- 2.Grynberg N. F., Echevarria A., Maciel M. A. M., Pinto A. C., Veiga Junior P. V. F. Plantas medicinais: a necessidade de estudos multidisciplinares. Química Nova. 2002;25(3):429–438. [Google Scholar]
- 3.Rezende H. A., Cocco M. I. The phytoterapy utilization in the rural population routine. Revista da Escola de Enfermagem da USP. 2002;36(3):282–288. doi: 10.1590/S0080-62342002000300011. [DOI] [PubMed] [Google Scholar]
- 4.Rodrigues E., Carlini E. A. Possible effects on the Central Nervous System of plants used by two Brazilian cultures (Maroons and Indians) Arquivos Brasileiros de Fitomedicina Científica. 2003;11(3):147–154. [Google Scholar]
- 5.Vale N. B. A farmacobotânica, ainda tem lugar na moderna anestesiologia? Revista Brasileira de Anestesiologia. 2002;52(3):368–380. doi: 10.1590/S0034-70942002000300013. [DOI] [PubMed] [Google Scholar]
- 6.França I. S., Souza J. A., Baptista R. S., Britto V. R. Medicina popular: benefícios e malefícios das plantas medicinais. Revista Brasileira de Enfermagem. 2008;61(2):201–208. doi: 10.1590/S0034-71672008000200009. [DOI] [PubMed] [Google Scholar]
- 7.Soares N. P., Camilo Neves A., de Abreu T., de Abreu Pfrimer G., Nishijo H., Aversi-Ferreira T. A. Medicinal plants used by the population of Goianápolis, Goiás State, Brazil. Acta Scientiarum - Biological Sciences. 2013;35(2):263–271. doi: 10.4025/actascibiolsci.v35i2.13077. [DOI] [Google Scholar]
- 8.Gómez-Estrada H., Díaz-Castillo F., Franco-Ospina L., et al. Folk medicine in the northern coast of Colombia: an overview. Journal of Ethnobiology and Ethnomedicine. 2011;7(1):27–37. doi: 10.1186/1746-4269-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aversi-Ferreira T. A., Ribeiro P. P., Silva N. C., et al. Confrontation between ethnopharmacology and scientific results of the herbal medicaments from Brazil to be applied in primary health care. Journal of Medicinal Plants Research. 2013;7(4):845–856. [Google Scholar]
- 10.Cuassolo F., Ladio A., Ezcurra C. Aspectos de lacomercialización y control de calidad de las plantas medicinales más vendidas en una comunidad urbana del no de la Patagonia Argentina. Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas. 2009;9(3):166–176. [Google Scholar]
- 11.Coulaud-Cunha S., Oliveira R. S., Waissmann W. Sale free Sorocea bomplandii Bailon as Espinheira Santa in the city of Rio de Janeiro-RJ. Revista Brasileira de Farmacognosia. 2004;14(4):51–53. doi: 10.1590/S0102-695X2004000300019. [DOI] [Google Scholar]
- 12.Andriolo D. S. M., Cunha L. H., Santana A. S., et al. Investigação da presença de anorexígenos, benzodiazepínicos e antidepressivos em formulações fitoterápicas emagrecedoras. Revista do Instituto Adolfo Lutz. 2012;71(1):148–152. [Google Scholar]
- 13.Miranda G. S., Souza S. R., Amaro M. O. F., Rosa M. B., Carvalho C. A. Avaliação do conhecimento etnofarmacológico da população de Teixeiras-MG. Revista de Ciências Farmacêuticas Básica e Aplicada. 2013;34(4):559–563. [Google Scholar]
- 14.Oliveira F. Q., Gonçalves L. A. Knowledge on medicinal plants and phythomedicines and potential of toxicity by users from Belo Horizonte, Minas Gerais. Revista Eletrônica de Farmácia. 2006;3(2):36–41. [Google Scholar]
- 15.Tomazzoni M. I., Negrelle R. R. B., Centa M. L. Popular phytotherapy: the instrumental search as therapy. Texto e Contexto de Enfermagem. 2006;15(1):115–121. [Google Scholar]
- 16.Rates K. S. M. Promoting the rational use of herbal medicines: an approach to teaching pharmacognosy. Revista Brasileira de Farmacognosia. 2001;11(2):57–69. [Google Scholar]
- 17.Maioli-Azevedo V., Fonseca-Kruel V. F. Medicinal and ritual plants sold in street markets of Rio de Janeiro, RJ, Brazil. Acta Botanica Brasilica. 2007;27(2):263–275. [Google Scholar]
- 18.Chaves M. D., Aversi Ferreira T. A. Terapia medicamentosa da doença de Alzheimer. Revista Eletrônica de Farmácia. 2008;5(1):1–7. doi: 10.5216/ref.v5i1.4608. [DOI] [Google Scholar]
- 19.Silva M. I., Gondim A. P., Nunes I. F., Sousa F. C. Utilização de fitoterápicos nas unidades básicas de atenção à saúde da família do município de Maracanaú (CE) Revista Brasileira de Farmacognosia. 2006;6(1):455–462. [Google Scholar]
- 20.Albertasse P. D., Thomaz L. D., Andrade M. A. Plantas medicinais e seus usos na comunidade da Barra do Jucu, Vila Velha, ES. Revista Brasileira de Plantas Medicinais. 2010;12(3):250–260. doi: 10.1590/S1516-05722010000300002. [DOI] [Google Scholar]
- 21.Negrelle R. R. B., Fornazzari K. R. C. Estudo etnobotânico em duas comunidades rurais (Limeira e Ribeirão Grande) de Guaratatuba (Paraná, Brasil) Revista Brasileira de Plantas Medicinais. 2007;9(2):36–54. [Google Scholar]
- 22.Alabashi R. H., Melzig M. F. Plectrantus barbatus: a review of phytochemistry, ethnobotanical and pharmacology - part 1. Planta Medica. 2010;76(7):653–661. doi: 10.1055/s-0029-1240898. [DOI] [PubMed] [Google Scholar]
- 23.Miranda T. M., Hanazaki N. Conhecimento e uso de recursos vegetais de restinga por comunidades das ilhas Cardoso (SP) e de Santa Catarina (SC), Brasil. Acta Botanica Brasilica. 2008;22(1):203–215. doi: 10.1590/S0102-33062008000100020. [DOI] [Google Scholar]
- 24.Garcia E. S., Gilbert A. C. P., Corrêa C. B. V., Cavalheiro M. V. S., Santos R. R., Tomasini T. Fitoterápicos. Campinas: André Tosello. 1996;17 [Google Scholar]
- 25.Soejarto D. D. Biodiversity prospecting and benefit-sharing: Perspectives from the field. Journal of Ethnopharmacology. 1996;51(1-3):1–15. doi: 10.1016/0378-8741(95)01345-8. [DOI] [PubMed] [Google Scholar]
- 26.Ariza S. Y., Rueda D. C., Rincón J., Linares E. L., Guerrero M. F. fectos farmacológicos sobre el sistema nervioso central inducidos por cumarina, aislada de Hygrophilatyttha Leonard. Vitae. 2007;14(2):51–58. [Google Scholar]
- 27.Franco E. A. P., Barros R. F. M. Uso e diversidade de plantas medicinais no Quilombo Olho D’água dos Pires, Esperantina, Piauí. Revista Brasileira de Plantas Medicinais. 2006;8(3):78–88. [Google Scholar]
- 28.Venâncio T. E. Dissertação. Fortaleza, Brazil: Universidade Federal do Ceará, Faculdade de Medicina; 2009. Estudo dos efeitos comportamentais e neuroquímicos do extrato padronizado de Justicia pectoralis (chambá) em camundongos. [Google Scholar]
- 29.Lino C. S., Taveira M. L., Viana G. S. B., Matos F. J. A. Analgesic and antiinflammatory activities of Justicia pectoralis Jacq and its main constituents: Coumarin and umbelliferone. Phytotherapy Research. 1997;11(3):211–215. doi: 10.1002/(SICI)1099-1573(199705)11:3<211::AID-PTR72>3.0.CO;2-W. doi: 10.1002/(SICI)1099-1573(199705)11:3<211::AID-PTR72>3.0.CO;2-W. [DOI] [Google Scholar]
- 30.Locklear T. D., Huang Y., Frasor J., et al. Estrogenic and progestagenic effects of extracts of Justicia pectoralis Jacq. an herbal medicine from Costa Rica used for the treatment of Menopause and PMS. Maturitas. 2010;66(3):315–322. doi: 10.1016/j.maturitas.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trueba G. P., Martínez R. R., Ruiz Z. P., Chanfrau J. R. Evaluación de la actividad antioxidant de Justicia Pectoralis. Revissta cubana de Investigaçoes Biomedicas. 2001;20(1):30–33. [Google Scholar]
- 32.Dutra R. C., Tavares C. Z., Ferraz S. O., Sousa O. V., Pimenta D. S. Investigação das atividades analgésica e antiinflamatória do extrato metanólico dos rizomas de Echinodorus grandiflorus. Brazilian Journal of Pharmacognosy. 2006;16(4):469–474. doi: 10.1590/S0102-695X2006000400005. [DOI] [Google Scholar]
- 33.Cardoso G. L. C., Pereira N. A., Lainetti R. Avaliação das atividades antinociceptiva, antiinflamatória e diurética do chapéu-de-couro (Echinodorus grandiflorus, [Cham e Schl] Mitch, Alismataceae. Revista Brasileira de Farmácia. 2003;84(1):5–7. [Google Scholar]
- 34.Conceição G. F. Dissertação. Rio de Janeiro, Brazil: Instituto Oswaldo Cruz; 2011. Efeitos anti-hipertensivos e microcirculatórios do extrato hidro-alcóolico de Echinodorus grandiflorus (chapéus-de-couro) em ratos espontaneamente hipertensos. [Google Scholar]
- 35.Lessa M. A., Araújo C. V., Kaplan M. A., Pimenta D., Figueiredo M. R., Tibiriçá E. Antihypertensive effects of crude extracts from leaves of Echinodorus grandifolius. Fundamental & Clinical Pharmacology. 2008;22(2):161–168. doi: 10.1111/j.1472-8206.2008.00565.x. [DOI] [PubMed] [Google Scholar]
- 36.Silva M. D., Dreveck S., Zeni A. L. B. Estudo etnobotânico de plantas medicinais utilizadas pela população rural no entorno do Parque Nacional da Serra do Itajaí - Indaial. Revista Saúde e Ambiente. 2009;10(2):54–64. [Google Scholar]
- 37.Wu C.-H., Hsieh H.-T., Lin J.-A., Yen G.-C. Alternanthera paronychioides protects pancreatic β-cells from glucotoxicity by its antioxidant, antiapoptotic and insulin secretagogue actions. Food Chemistry. 2013;139(1-4):362–370. doi: 10.1016/j.foodchem.2013.01.026. [DOI] [PubMed] [Google Scholar]
- 38.Jorge V.-G., Ángel J.-R. L., Adrián T.-S., et al. Vasorelaxant activity of extracts obtained from Apium graveolens: Possible source for vasorelaxant molecules isolation with potential antihypertensive effect. Asian Pacific Journal of Tropical Biomedicine. 2013;3(10):776–779. doi: 10.1016/S2221-1691(13)60154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mosca V. P., Loiola M. I. B. Uso popular de plantas medicinais no rio grande do norte, nordeste do Brasil. Revista Caatinga. 2009;22(4):225–234. [Google Scholar]
- 40.Melo E. d., Mancini Filho J., Guerra N. B., Maciel G. R. Atividade antioxidante de extratos de coentro (Coriandrum sativum L.) Ciência e Tecnologia de Alimentos. 2003;23(1):195–199. doi: 10.1590/S0101-20612003000400036. [DOI] [Google Scholar]
- 41.Zanusso-Junior G., Melo J., Romero A., et al. Avaliação da atividade antiinflamatória do coentro (Coriandrum sativum L.) em roedores. Revista Brasileira de Plantas Medicinais. 2011;13(1):17–23. doi: 10.1590/S1516-05722011000100003. [DOI] [Google Scholar]
- 42.Pedrosa V. Z. Tese. Centro de Ciências de Saúde, Universidade Federal da Paraíba; 2014. Atividade do Coriandrum sativum L. sobre cepas de Echerichia coli produtoras de B- lactamases de expectro estendido. [Google Scholar]
- 43.Emamghoreishi M., Khasaki M., Aazam M. F. Coriandrum sativum: Evaluation of its anxiolytic effect in the elevated plus-maze. Journal of Ethnopharmacology. 2005;96(3):365–370. doi: 10.1016/j.jep.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 44.Freires I. A., Murata R. M., Furletti V. F., et al. Coriandrum sativum L. (Coriander) essential oil: antifungal activity and mode of action on Candida spp., and molecular targets affected in human whole-genome expression. PLoS ONE. 2014;9(3):1–13. doi: 10.1371/journal.pone.0099086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sreelatha S., Inbavalli R. Antioxidant, antihyperglycemic and antihyperlipidemic effects of Coriandrum sativum Leaf and stem in alloxan-induced biabetic rats. Journal of Food Science. 2012;77(7):119–123. doi: 10.1111/j.1750-3841.2012.02755.x. [DOI] [PubMed] [Google Scholar]
- 46.Taherian A. A., Vafaei A. A., Ameri J. Opiate system mediate the atinociceptive effects of Coriandrum sativum in mice. Iranian Journal of Pharmaceutical Research. 2012;11(2):679–688. [PMC free article] [PubMed] [Google Scholar]
- 47.Barrella W., Breier T. B., Leme G. A. Levantamento etnobotânico do uso popular de plantas medicinais por comunidade rurais atendidas pela UBSF/Jundiaquara/ Araçoiaba da Serra/ SP. Revista Eletrônica de Biologia. 2010;3(4):89–105. [Google Scholar]
- 48.Soares M. A. A., Braga J. R. P., Mourão A. E. B., Parente K. M. S., Parente E. G. Levantamento etnobotânico das plantas medicinais utilizadas pela população do município de Gurinhém- Paraíba. Revista Homem, Espaço e Tempo. 2009;3(2):36–47. [Google Scholar]
- 49.Silva W. A., Fagundes N. C. A., Coutinho C. A., Soares A. C. M., Campos P. V., Figueiredo L. S. Levantamento etnobotânico de plantas medicinais na cidade de São João da Ponte-MG. Revista de Biologia e Farmácia. 2012;7(1):122–131. [Google Scholar]
- 50.Trajano V. N., Lima E. d., Souza E. L., Travassos A. E. Propriedade antibacteriana de óleos essenciais de especiarias sobre bactérias contaminantes de alimentos. Ciência e Tecnologia de Alimentos. 2009;29(3):542–545. doi: 10.1590/S0101-20612009000300014. [DOI] [Google Scholar]
- 51.Karimzadeh F., Hosseini M., Mangeng D., et al. Anticonvulsant and neuroprotective effects of Pimpinella anisum in rat brain. BMC Complementary and Alternative Medicine. 2012;12(76):1–10. doi: 10.1186/1472-6882-12-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee J.-B., Yamagishi C., Hayashi K., Hayashi T. Antiviral and immunostimulating effects of lignin- carbohydrate- protein complexes from Pimpinella anisium. Bioscience, Biotechnology, and Biochemistry. 2011;75(3):459–465. doi: 10.1271/bbb.100645. [DOI] [PubMed] [Google Scholar]
- 53.Gülçin I., Oktay M., Kireçci E., Küfrevıoğlu Ö. I. Screening of antioxidant and antimicrobial activities of anise (Pimpinella anisum L.) seed extracts. Food Chemistry. 2003;83(3):371–382. doi: 10.1016/S0308-8146(03)00098-0. [DOI] [Google Scholar]
- 54.Kadan S., Rayan M., Rayan A. Anticancer activity of anise (Pimpinella anisum L.) seed extract. The Open Nutraceuticals Journal. 2013;6(1):1–5. doi: 10.2174/1876396001306010001. [DOI] [Google Scholar]
- 55.Merétika A. H. C., Peroni N., Hanazaki N. Local knowledge of medicinal plants in three artisanal fishing communities (Itapoá, Southern Brazil), according to gender, age, and urbanization. Acta Botanica Brasilica. 2010;24(2):386–394. doi: 10.1590/S0102-33062010000200009. [DOI] [Google Scholar]
- 56.Cruz-Silva C. T. A., Pelinson A. P., Campelo A. M. Abordagem etnobotânica acerca do uso de plantas medicinais na região urbana no município de Quedas do Iguaçu - Paraná. Cultivando o Saber. 2009;2(1):14–25. [Google Scholar]
- 57.Pilla M. A., Amorozo M. C., Furlan A. Obtenção e uso das plantas medicinais no distrito de Martim Franscisco, Município de Mogi-Mirim, SP, Brasil. Acta Botanica Brasilica. 2006;20(4):789–802. doi: 10.1590/S0102-33062006000400005. [DOI] [Google Scholar]
- 58.Fuck S. B., Athanázio J. C., Lima C. B., Ming L. C. Plantas medicinais utilizadas na medicina popular por moradores da área urbana de Bandeirantes, PR, Brasil. Semina: Ciências Agrárias. 2005;26(3):291–296. doi: 10.5433/1679-0359.2005v26n3p291. [DOI] [Google Scholar]
- 59.Almeida N. F. L., Silva S. R. S., Souza J. M., Queiroz A. P. N., Miranda G. S., Oliveira H. B. Levantamento etnobotânico de plantas medicinais na cidade de Viçosa-MG. Revista Brasileira de Ciências Farmacêuticas. 2009;90(4):316–320. [Google Scholar]
- 60.Martins A. G., Rosário D. L., Barros M. N., Jardim M. A. G. Levantamento etnobotânico de plantas medicinais, alimentares e tóxicas da Ilha do Combu, Município de Belém, Estado do Pará, Brasil. Revista Brasileira de Farmácia. 2005;26(1):21–30. [Google Scholar]
- 61.Tinoco M. T., Martins M. R., Cruzmorais J. Atividade antimicrobiana do óleo essencial do Foeniculum vulgare Miller. Revista de Ciências Agrárias. 2013;30(1):448–454. [Google Scholar]
- 62.Beaux D., Fleurentin J., Mortier F. Diuretic action of hydroalcohol extracts of Foeniculum vulgare var dulce (D.C.) roots in rats. Phytotherapy Research. 1997;11(4):320–322. doi: 10.1002/(SICI)1099-1573(199706)11:4<320::AID-PTR92>3.0.CO;2-N. [DOI] [Google Scholar]
- 63.Wakabayashi K. A. L., De Melo N. I., Aguiar D. P., et al. Anthelmintic effects of the essential oil of fennel (Foeniculum vulgare., Apiaceae) against Schistosoma mansoni. Chemistry & Biodiversity. 2015;12(7):1105–1114. doi: 10.1002/cbdv.201400293. [DOI] [PubMed] [Google Scholar]
- 64.Mansouri E., Kooti W., Bazvand M., et al. The effect of hydro-alcoholic extract of Foeniculum vulgare mill on leukocytes and hematological tests in male rats. Jundishapur Journal of Natural Pharmaceutical Products. 2015;10(1):1–5. doi: 10.17795/jjnpp-18396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mesfin M., Asres K., Shibeshi W. Evaluation of anxiolytic activity of the essential oil of the aerial part of Foeniculum vulgare Miller in mice. BMC Complementary and Alternative Medicine. 2014;14(310):1–7. doi: 10.1186/1472-6882-14-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gnoatto S. C., Bassani V. L., Coelho G. C., Schenkel E. P. Influência do método de estração nos teores de metilxantinas em erva-mate (Ilex paraguariensisa. St. - Hil., aquifoliaceae) Quimica Nova. 2007;30(2):304–307. doi: 10.1590/S0100-40422007000200012. [DOI] [Google Scholar]
- 67.Rodrigues V. E. G., Carvalho D. A. Levantamento etnobotânico de plantas medicinais no domínio do cerrado na região do Alto Rio Grande- Minas Gerais. Ciência e Agrotecnologia. 2001;25(1):102–123. [Google Scholar]
- 68.Ortiz A. C., Lombardo M. C. M. Cultivo de plantas medicinales en la provincia de Jaén. Boletín Instituto de Estudios Giennenses. 2009;2(200):195–230. [Google Scholar]
- 69.Mello F. B., Mello J. R. B. Avaliação dos Efeitos Antitussígenos e Expectorantes de Duas Formulações Fitoterápicas Existentes no Mercado Brasileiro. Acta Farmeceutica Bonorence. 2006;25(1):64–70. [Google Scholar]
- 70.Kiertsman B., Zuquim S. L. O extrato seco de Hedera helix no tratamento das infecções de vias aéreas na infância. Pediatria Moderna. 2008;44(4):143–149. [Google Scholar]
- 71.Rai A. The antiinflammatory and antiarthritic properties of ethanol extract of hedera helix. Indian Journal of Pharmaceutical Sciences. 2013;75(1):99–102. doi: 10.4103/0250-474X.113537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rodriguez G. I. I. Dissertação. Ciências Farmacêuticas de Ribeirão Preto, USP; 2010. Avaliação da Atividade antiofídica de Aristolochia sprucei: Isolamento e caracterização estrutural de composto bioativo. [Google Scholar]
- 73.Pacheco G. A. Dissertação. Departamento de Química do Instituto de Ciências Exatas da Universidade Federal de Minas; 2009. Estudo fitoquímico de Aristolochia esperanazae Kuntze (Aristolochia) [Google Scholar]
- 74.Ritter M. R., Sobierajski G. R., Schenkel E. P., Mentz L. A. Plantas usadas como medicinais no município de Ipê, RS, Brasil. Revista Brasileira de Farmacognosia. 2002;12(2):51–62. doi: 10.1590/s0102-695x2002000200001. [DOI] [Google Scholar]
- 75.Sousa M. J. M., Moral F. F., Nascimento G. N. L., Soares N. P., Aversi-Ferreira T. A. Medicinal plants used by Itamaraty community nearby Anápolis, Goiás State, Brazil. Acta Scientiarum - Health Sciences. 2010;2(32):177–184. doi: 10.4025/actascihealthsci.v32i2.8155. [DOI] [Google Scholar]
- 76.Lopes F., Placeres M., Moreira R., Santos L. d., Carlos I. Avaliação da atividade imunológica Achillea millefolium L. ('mil-folhas') Revista Brasileira de Farmacognosia. 2003;13(2):11–13. doi: 10.1590/S0102-695X2003000400005. [DOI] [Google Scholar]
- 77.Brito M. R., Senna-Valle L. d. Plantas medicinais utilizadas na comunidade caiçara da Praia do Sono, Paraty, Rio de Janeiro, Brasil. Acta Botanica Brasilica. 2011;25(2):363–372. doi: 10.1590/S0102-33062011000200012. [DOI] [Google Scholar]
- 78.Borba A. M., Macedo M. Plantas medicinais usadas para a saúde bucal pela comunidade do bairro Santa Cruz, Chapada dos Guimarães, MT, Brasil. Acta Botanica Brasilica. 2006;20(4):771–782. doi: 10.1590/S0102-33062006000400003. [DOI] [Google Scholar]
- 79.Ruffa M. J., Ferraro G., Wagner M. L., Calcagno M. L., Campos R. H., Cavallaro L. Cytotoxic effect of Argentine medicinal plant extracts on human hepatocellular carcinoma cell line. Journal of Ethnopharmacology. 2002;79(3):335–339. doi: 10.1016/S0378-8741(01)00400-7. [DOI] [PubMed] [Google Scholar]
- 80.Oliveira A. L., Padilha C. D., Ortega G. G., Pretrovick P. R. Achyrocline satureioides (Lam.) DC., Asteraceae: comparative evaluation of the vegetal drug and preliminary optimization studies on extraction . Caderno de Farmßcia. Vol. 17. Asteraceae: comparative evaluation of the vegetal drug and preliminary optimization studies on extraction . Caderno de Farmácia; 2001. [Google Scholar]
- 81.Bettega R. P. J. M. Dissertação. Florianópolis, Brazil: Universidade Federal de Santa Catarina; 2000. Avaliação da atividade antiviral de extratos nebulizados de Achyrocline saturioides (Lam) D C. Asteraceae - Marcela. [Google Scholar]
- 82.Ochoa J. J., Ladio A. H., Lozada M. Uso de recursos herbolarios entre mapuches y criollos de la comunidad campesina Arroyo Las Minas (Río Negro, Argentina) Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromáticas. 2010;9(4):269–276. [Google Scholar]
- 83.Shafi G., Hasan T. N., Syed N. A., et al. Artemisia absinthium (AA): A novel potential complementary and alternative medicine for breast cancer. Molecular Biology Reports. 2012;39(7):7373–7379. doi: 10.1007/s11033-012-1569-0. [DOI] [PubMed] [Google Scholar]
- 84.Obistioiu D., Cristina R. T., Schmerold I., et al. Chemical characterization by GC-MS and in vitro activity against Candida albicans of volatile fractions prepared from Artemisia dracunculus, Artemisia abrontanum, Artemisia absinthium and Artemisia vulgaris. Chemistry Central Journal. 2014;8(6):1–11. doi: 10.1186/1752-153X-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Moslemi H. R., Hoseinzadeh H., Badouei M. A., Kafshdouzan K., Fard R. M. N. Antimicrobial anctivity of Artemisia absinthium against surgical wounds infected by Staphylococcus aureus in a rat model. Indian Journal of Microbiology. 2012;52(4):601–604. doi: 10.1007/s12088-012-0283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tariku Y., Hymete A., Hailu A., Rohloff J. In vitro evaluation of antileishmanial activity and toxicity of essential oils of Artemisia absinthium and Echinops kebericho. Chemistry & Biodiversity. 2011;8(4):614–623. doi: 10.1002/cbdv.201000331. [DOI] [PubMed] [Google Scholar]
- 87.Gallotte D. C., Ribeiro L. F. Levantamento etnobotânico das plantas medicinais do horto da Escola Superior São Franscisco de Assis - ESFA, Santa Teresa, ES. Natureza Online. 2005;3(1):19–24. [Google Scholar]
- 88.Brito V. F. S., Dantas I. C., Dantas G. D. S. Plantas medicinais utilizadas pela comissão de mulheres na zona rural no município de Lagoa Seca- PB. Revista de Biologia e Farmácia. 2009;3(1):112–123. [Google Scholar]
- 89.Oliveira A. K. M., Oliveira N. A., Resende U. M., Martins P. F. R. B. Ethnobotany and traditional medicine of the in habitants of the Pantanal Negro sub-region and the raizeiros of Miranda and Aquidauna, Mato Grosso do Sul, Brazil. Brazilian Journal of Biology. 2011;71(1):283–289. doi: 10.1590/S1519-69842011000200007. [DOI] [PubMed] [Google Scholar]
- 90.Giraldi M., Hanazaki N. Uso e conhecimento tradicional de plantas medicinais no Sertão do Ribeirão, Florianópolis, SC, Brasil. Acta Botanica Brasilica. 2010;24(2):395–406. doi: 10.1590/s0102-33062010000200010. [DOI] [Google Scholar]
- 91.Hernández M. P., Civitella S. M., Rosato V. G. Uso medicinal popular de plantas y líquenes de la Isla Paulino, Provincia de Buenos Aires, Argentina. Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromaticas. 2010;9(4):258–268. [Google Scholar]
- 92.Wehba C., Fernandes F., Oppi E. Aplicação de pomada a base de extrato de camomila como coadjuvante na redução da sintomatologia dolorosa das lesões ulceradas da mucosa oral. Revista Brasileira de Medicina. 2008;65(5):129–132. [Google Scholar]
- 93.Cogo L. L., Monteiro C. L. B., Miguel M. D., et al. Anti- Helicobacter pylori activity of plant extracts traditionally used for the treatment of gastrointestinal disorders. Brazilian Journal of Microbiology. 2010;41(2):304–309. doi: 10.1590/S1517-83822010000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Al-Hashem F. H. Gastroprotective effects of aqueous extract of chamomilla recutita against ethanol-induced gastric ulcers. Saudi Medical Journal. 2010;31(11):1211–1216. [PubMed] [Google Scholar]
- 95.Cemek M., Kağa S., Şimşek N., Büyükokuroğlu M. E., Konuk M. Antihyperglycemic and antioxidative potential of Matricaria chamomilla L. in streptozotocin-induced diabetic rats. Journal of Natural Medicines. 2006;62(3):284–293. doi: 10.1007/s11418-008-0228-1. [DOI] [PubMed] [Google Scholar]
- 96.Noldin V. F., Cechinel Filho V., Monache F. D., et al. Composição química e atividades biológicas das folhas de Cynara scolymus L. (alcachofra) cultivada no Brasil. Química Nova. 2003;26(3):331–334. doi: 10.1590/S0100-40422003000300008. [DOI] [Google Scholar]
- 97.Zaru A., MacCioni P., Riva A., et al. Reducing effect of a combination of phaseolus vulgaris and cynara scolymus extracts on operant self-administration of a chocolate-flavoured beverage in rats. Phytotherapy Research. 2013;27(6):944–947. doi: 10.1002/ptr.4814. [DOI] [PubMed] [Google Scholar]
- 98.Gebhardt R. Antioxidative and protective properties of extracts from leaves of the artichoke (Cynara scolymus C.) againt hydroperoxide-induced oxidative stress in cultured rat hepatocytes. Toxicology and Applied Pharmacology. 1997;144(2):279–286. doi: 10.1006/taap.1997.8130. [DOI] [PubMed] [Google Scholar]
- 99.Luz F. J. Plantas medicinais de uso popular em Boa Vista, Roraima, Brasil. Horticultura Brasileira. 2001;19(1):88–96. doi: 10.1590/S0102-05362001000100019. [DOI] [Google Scholar]
- 100.Harsha S. N., Anilakumar K. R., Mithila M. V. Antioxidant properties of Lactuca sativa leaf extract involved in the protection of biomolecules. Biomedicine & Preventive Nutrition. 2013;3(4):367–373. doi: 10.1016/j.bionut.2013.06.003. [DOI] [Google Scholar]
- 101.Medeiros M. F., Fonseca V. S., Andreata R. H. Plantas medicinais e seus usos pelos sitiantes da Reserva do Rio das Pedras, Mangaratiba, RJ, Brasil. Acta Botanica Brasilica. 2004;18(2):391–399. [Google Scholar]
- 102.Madaleno I. M. Etnofarmacología en Iberoamérica, una alternativa a la globalización de las prácticas de cura. Cuadernos Geográficos. 2008;41(2):61–95. [Google Scholar]
- 103.Owlia P., Rasooli I., Saderi H. Antistreptcoccal and antioxidant activity of essential oil from Matricaria chamomilla L. Research Journal of Biological Sciences. 2007;2(2):155–160. [Google Scholar]
- 104.Rodrigues C. V. E. e. A., Carvalho D. Florística de plantas medicinais nativas de remanescentes de floresta estacional semidecidual na região de Alto do Rio Grande- Minas Gerais. Revista Cerne. 2005;15(3):93–112. [Google Scholar]
- 105.Salgado H. R. N., Roncari A. F. F., Moreira R. R. D. Antidiarrhoeal effects of Mikania glomerata Spreng. (Asteraceae) leaf extract in mice. Revista Brasileira de Farmacognosia. 2005;15(3):205–208. doi: 10.1590/S0102-695X2005000300007. [DOI] [Google Scholar]
- 106.Assini F., Fabrício E., Lang K. Efeitos farmacológicos do extrato aquoso de Solidago chilensis Meyen em camundongos. Revista Brasileira de Plantas Medicinais. 2013;15(1):130–134. doi: 10.1590/S1516-05722013000100018. [DOI] [Google Scholar]
- 107.Costa F. G. C., Nunes F. G. C. C., Peres V. Mapeamento etnofarmacológico e etnobotânico de espécies de cerrado, na microregião de Patos de Minas. Revista do Núcleo Interdisciplinar de Pesquisa e Extensão. 2010;2(7):93–111. [Google Scholar]
- 108.Nascimento M. A. Dissertação. Departamento de Bioquímica e Biologia Molecular, Setor de Ciências Biológicas., Universidade Federal do Paraná; 2012. Polissacarídeos e metabólitos secundários de Spilanthes olaracea L. (Jambu) [Google Scholar]
- 109.Pessini G., Holetz F., Sanches N., Cortez D., Dias Filho B., Nakamura C. Avaliação da atividade antibacteriana e antifúngica de extratos de plantas utilizados na medicina popular. Revista Brasileira de Farmacognosia. 2003;13(1):21–24. doi: 10.1590/S0102-695X2003000300009. [DOI] [Google Scholar]
- 110.Álvarez Á. L., Habtemariam S., Juan-Badaturuge M., Jackson C., Parra F. In vitro anti HSV-1 and HSV-2 activity of Tanacetum vulgare extracts and isolated compounds: an approach to their mechanism of action. Phytotherapy Research. 2011;25(2):296–301. doi: 10.1002/ptr.3382. [DOI] [PubMed] [Google Scholar]
- 111.Rosselli S., Bruno M., Raimondo F. M., et al. Cytotoxic effect of eudesmanolides isolated from flowers of Tanacetum vulgare ssp. Siculum. Molecules. 2012;17(7):8186–8195. doi: 10.3390/molecules17078186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Luize P. S., Tiuman T. S., Morello L. G., et al. Effects of medicinal plant extracts on growth of Leishmania (L.) amazonensis and Trypanossoma cruzi. Brazilian Journal of Pharmaceutical Sciences. 2005;41(1):85–94. doi: 10.1590/S1516-93322005000100010. [DOI] [Google Scholar]
- 113.Xie G., Schepetkin I. A., Quinn M. T. Immunomodulatory activity of acidic polysaccharides isolated from Tanacetum vulgare L. International Immunopharmacology. 2007;7(13):1639–1650. doi: 10.1016/j.intimp.2007.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Godinho L. S., de Carvalho L. S. A., de Castro C. C. B., et al. Anthelmintic activity of crude extract and essential oil of Tanacetum vulgare (Asteraceae) against adult worms of schistosoma mansoni. The Scientific World Journal. 2014;2014:10. doi: 10.1155/2014/460342.460342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Pagno T., Blind L. Z., Biavatti M. W., Kreuger M. R. O. Cytotoxic activity of the dichloromethane fraction the Vernonia scorpioides (Lam.) Pers. (Asteraceae) against Ehrlich's tumor cells in mice. Brazilian Journal of Medical and Biological Research. 2006;39(11):1483–1491. doi: 10.1590/S0100-879X2006001100012. [DOI] [PubMed] [Google Scholar]
- 116.Silva C. E., Valota R., Gebara K. S., Silva R. C., Simionatto E. Avaliação da atividade antioxidante e o teor de compostos fenólicos em extrato metanólico obtido de folhas da Commiphora Myrrha. Semina: Ciências Exatas e Tecnológicas. 2013;34(1):117–124. doi: 10.5433/1679-0375.2013v34n1p117. [DOI] [Google Scholar]
- 117.Vila Verde G., Paula J., Caneiro D. Levantamento etnobotânico das plantas medicinais do cerrado utilizadas pela população de Mossâmedes (GO) Revista Brasileira de Farmacognosia. 2003;13(1):64–66. doi: 10.1590/S0102-695X2003000300024. [DOI] [Google Scholar]
- 118.Chieregatto C. L. Dissertação. Universidade Federal de Viçosa; 2005. Efeito do tratamento crônico com extratos de Heteropterys afrodisíaca O. Mach. E Anamopaegma arvense. (Vell). Stellf. no testículo de ratos wistar adultos. [Google Scholar]
- 119.Costanzo C. D. G., Fernandes V. C., Zingaretti S., et al. Isolation of flavonoids from Anemopaegma arvense (Vell) Stellf. ex de Souza and their antifungal activity against Trichophyton rubrum. Brazilian Journal of Pharmaceutical Sciences. 2013;49(3):559–565. doi: 10.1590/S1984-82502013000300016. [DOI] [Google Scholar]
- 120.Bueno N. R., Castilho R. O., da Costa R. B., et al. Medicinal plants used by the kaiowá and guarani indigenous populations in the caarapó reserve, Mato Grosso do Sul, Brazil. Acta Botanica Brasilica. 2005;19(1):39–44. doi: 10.1590/S0102-33062005000100005. [DOI] [Google Scholar]
- 121.Pinho L. d., Souza P. N., Macedo Sobrinho E., Almeida A. C., Martins E. R. Atividade antimicrobiana de extratos hidroalcoólicos das folhas de alecrim-pimenta, aroeira, barbatimão, erva baleeira e do farelo da casca de pequi. Ciência Rural. 2011;42(2):326–331. doi: 10.1590/S0103-84782012005000003. [DOI] [Google Scholar]
- 122.Pimentel S. P., Barrella G. E., Casarin R. C. V., et al. Protective effect of topical Cordia verbenacea in a rat periodontitis model: immune-inflammatory, antibacterial and morphometric assays. BMC Complementary and Alternative Medicine. 2012;12(224):1–8. doi: 10.1186/1472-6882-12-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nitz A. C., Ely J. B., D’Acampora A. J., Tames D. R., Corrêa B. P. Estudo morfométrico no processo de cicatrização de feridas cutâneas em ratos, usando: Coronopu didymus e Calendula officinali. Arquivos Catarinenses de Medicina. 2006;35(4):74–79. [Google Scholar]
- 124.Busnardo T. C. P. M., Padoani C., Mora T. C., et al. Anti-inflammatory evaluation of Coronopus didymus in the pleurisy and paw edema models in mice. Journal of Ethnopharmacology. 2010;128(2):519–525. doi: 10.1016/j.jep.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 125.Fracaro S. N., Nakashima T., Deconto I. Potencial abortivo de Tillandsia usneoides L. (barba-de- pau) em coelhas gestantes- Nota prévia. Arquivos de ciências veterinárias e zoologia da UNIPAR. 2014;7(2):181–185. [Google Scholar]
- 126.Andrighetti-Fröhner C. R., Sincero T. C. M., Da Silva A. C., et al. Antiviral evaluation of plants from Brazilian Atlantic Tropical Forest. Fitoterapia. 2005;76(3-4):374–378. doi: 10.1016/j.fitote.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 127.Oliveira D. M. S., Ocampos F. M. M., Moreira T. F., et al. Physico-Chemical assays, hemolytic, and antimicrobial activity of extracts and fractions of Buddleja stachyoides Cham and Schltdl. (Schrophulariaceae) Visão Acadêmica. 2013;14(3):14–25. [Google Scholar]
- 128.Su S., Wang T., Duan J., et al. Anti-inflammatory and analgesic activity of different extracts of Chommiphora myrrha. Journal of Ethnopharmacology. 2011;134(2):251–258. doi: 10.1016/j.jep.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 129.Damasceno D. C., Volpato G. T., de Mattos Paranhos Calderon I., Aguilar R., Rudge M. V. C. Effect of Bauhinia forficata extract in diabetic pregnant rats: Maternal repercussions. Phytomedicine. 2004;11(2-3):196–201. doi: 10.1078/0944-7113-00348. [DOI] [PubMed] [Google Scholar]
- 130.Düsman E., Almeida I. V. D., Coelho A. C., Balbi T. J., Düsman Tonin L. T., Vicentini V. E. P. Antimutagenic effect of medicinal plants achillea millefolium and bauhinia forficata in vivo. Evidence-Based Complementary and Alternative Medicine. 2013;2013:6. doi: 10.1155/2013/893050.893050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Marinho M. G. V., Silva C. C., Andrade L. H. C. Levantamento etnobotânico de plantas medicinais em áreas de caatinga no município de São José de Espinharas, Paraíba, Brasil. Revista Brasileira de Plantas Medicinais. 2011;13(2):170–180. doi: 10.1590/S1516-05722011000200008. [DOI] [Google Scholar]
- 132.Leal S. R. Tese. Universidade Federal do Rio Grande do Norte, Centro de Ciências exatas e da terra; 2008. Estudo etnofarmacológico e fitoquímico espécies medicinais Cleome spinosa Jacq, Pavonia varians Moric e Croton cajucara Benth. [Google Scholar]
- 133.Albarello N., Simões-Gurgel C., Castro T. C., et al. Anti-inflammatory and antinociceptive activity of fieldgrowth plants and tissue culture of Cleome Spinosa (Jacq.) in mice. Journal of Medicinal Plants Research [Google Scholar]
- 134.Scopel M. Dissertação. Faculdade de Farmácia, Programa de Pós Graduação em Ciências Farmacêuticas; 2005. Análise botânica, química e biológica comparativa entre flores das espécies Sambuncus nigra L. e Sambuncus australis Chan e Schltdl. avaliação preliminar de sua estabilidade. [Google Scholar]
- 135.Daryani A., Ebrahimzadeh M. A., Sharif M., et al. Anti-toxoplasma activities of methanolic extract of sambucus nigra (caprifoliaceae) fruits and leaves. Revista de Biología Tropical. 2015;63(1):7–12. doi: 10.15517/rbt.v63i1.14545. [DOI] [PubMed] [Google Scholar]
- 136.Bum E. N., Soudi S., Ayissi E. R., et al. Anxiolityc activity evaluation of four medicinal plants from Cameroon. African Journal of Traditional, Complementary and Alternative Medicines. 2011;8(5):130–139. doi: 10.4314/ajtcam.v8i5S.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Dias L. F., Melo E. S., Hernandes L. S., Bacchi E. M. Atividades antiúlcera e antioxidante Baccharis trimera (Less) DC (Asteraceae) Revista Brasileira de Farmacognosia. 2009;19(1):309–314. doi: 10.1590/S0102-695X2009000200022. [DOI] [Google Scholar]
- 138.Lima R. A., Magalhães S. A., Santos M. R. A. Levantamento etnobotânico de plantas medicinais utilizadas na cidade de Vilhena, Rondônia. Revista Pesquisa e Criação. 2011;10(2):112–123. [Google Scholar]
- 139.Paul E. L., Lunardelli A., Caberlon E., et al. Anti-inflammatory and immunomodulatory effects of Bacharis trimera aqueous extract on induced pleurisy in rats and lymphoproliferation In Vitro. Inflammation. 2009;32(6):419–425. doi: 10.1007/s10753-009-9151-1. [DOI] [PubMed] [Google Scholar]
- 140.Gené R. M., Cartañá C., Adzet T., Marín E., Parella T., Cañigueral S. Anti-inflammatory and analgesic activity of Bacharis trimera: identification of its active constituents. Planta Medica. 1996;62(3):232–235. doi: 10.1055/s-2006-957866. [DOI] [PubMed] [Google Scholar]
- 141.Valverde A. L., Cardoso G. L. C., Pereira N. A., Silva A. J. R., Kuster R. M. Analgesic and antiinflammatory activities of vernonioside B2 from Vernonia condensata. Phytotherapy Research. 2001;15(3):263–264. doi: 10.1002/ptr.733. [DOI] [PubMed] [Google Scholar]
- 142.Batista A. G. U., Lopes R. A., Souza M. A., et al. Hepatotoxidade de plantas medicinais. XLIX. Ação da infusão de Cayaponia tayuya (Vell.) Cong. no camundongo. Investigação – Revista Científica da Universidade de Franca. 2006;6(1):7–12. [Google Scholar]
- 143.Aquila S., Giner R. M., Recio M. C., Spegazzini E. D., Ríos J. L. Anti-inflammatory activity of flavonoids from Cayaponia tayuya roots. Journal of Ethnopharmacology. 2009;121(2):333–337. doi: 10.1016/j.jep.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 144.Macedo J. M., Souza L. G. P., Valenzuela V. C. T., Oliveira A. B., Castilho R. O., Jácome R. L. R. P. Variação sazonal nos teores de flavonoides, taninos e atividade antioxidante de Davilla rugosa Poir. Revista de Ciências Farmacêuticas Básica e Aplicada. 2013;4(4):585–590. [Google Scholar]
- 145.Guaraldo L., Sertiè J. A. A., Bacchi E. M. Antiulcer action of the hydroalcoholic extract and fractions of Davilla rugosa Poiret in thhe rat. Journal of Ethnopharmacology. 2001;76(2):191–195. doi: 10.1016/S0378-8741(01)00198-2. [DOI] [PubMed] [Google Scholar]
- 146.Feitosa C. M., Freitas R. M., Luz N. N. N., Bezerra M. Z. B., Trevisan M. T. S. Acetylcholinesterase inhibition by somes promising Brazilian medical plants. Brazilian Journal of Biology. 2011;71(3):783–789. doi: 10.1590/S1519-69842011000400025. [DOI] [PubMed] [Google Scholar]
- 147.Oskoueian E., Abdullah N., Ahmad S., Saad W. Z., Omar A. R., Ho Y. W. Bioactive compounds and biological activities of Jatropha curcas L. kernel meal extract. International Journal of Molecular Sciences. 2011;12(9):5955–5970. doi: 10.3390/ijms12095955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Igbinosa O. O., Igbinosa I. H., Chigor V. N., et al. Polyphenolic contents and antioxidant potential of stem bark extracts from jatropha curcas (Linn) International Journal of Molecular Sciences. 2011;12(5):2958–2971. doi: 10.3390/ijms12052958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Aiyelaagbe O. O., Hamid A. A., Fattorusso E., Taglialatela-Scafati O., Schröder H. C., Müller W. E. Cytotoxic activity of crude from Jatropha species, plants used extensively in African traditional medicine. Evidence-Based Complementary and Alternative Medicine. 2011;2011:7. doi: 10.1155/2011/134954.134954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Leite V. M. F., Pinheiro J. B., Pisani M. X., et al. In vitro antimicrobial activity of an experimental dentifrice based on Ricinus Communis. Brazilian Dental Journal. 2014;25(3):191–196. doi: 10.1590/0103-6440201302382. [DOI] [PubMed] [Google Scholar]
- 151.Silva C. S., Nunes P. O., Mescouto C. S., Müller R. C. S. T., Palheta D. C., Fernandes K. G. Avaliação do uso da casca do fruto e das folhas de Caesalpinia ferrea Martius como suplemento nutricuinal de Fe, Mn e Zn. Ciência e Tecnologia de Alimentos. 2010;3(30):751–754. doi: 10.1590/S0101-20612010000300028. [DOI] [Google Scholar]
- 152.Oliveira A., Batista J., Paiva E., et al. Avaliação da atividade cicatrizante do jucá (Caesalpinia ferrea Mart. ex Tul. var. ferrea) em lesões cutâneas de caprinos. Revista Brasileira de Plantas Medicinais. 2010;12(3):302–310. doi: 10.1590/S1516-05722010000300007. [DOI] [Google Scholar]
- 153.Sousa V. H., Barbosa A. P. O., Cardoso G. C., et al. Avaliação do potencial antidiabético decinco plantas medicinais em ratos. Latin American Journal of Pharmacy [Google Scholar]
- 154.Magalhães L. S., Pussente C. G., Azevedo L. R., Crespo J. M. R. S. Avaliação da atividade antibacteriana do extrato de Caesalpinia ferrea Martius e desenvolvimento de uma formulação fitocosmética. Revista Científica da Faminas. 2015;11(1):27–43. [Google Scholar]
- 155.Dias S. A., Neves A. E. O., de Ferraz A. B. F., Picada J. N., Pereira P. Neuropharmacological and genotoxic evaluation of ethanol extract from Erythrina falcata leaves, a plant used in Brazilian folk medicine. Revista Brasileira de Farmacognosia. 2013;23(2):335–341. doi: 10.1590/S0102-695X2013005000015. [DOI] [Google Scholar]
- 156.Chen T., Sun H., Yao H., et al. Suppressive effects of Indigofera suffruticosa Mill extracts on lipopolysaccharide- induced inflammatory responses in murine RAW 264.7 macrophages. Food and Chemical Toxicology. 2013;55(55):257–264. doi: 10.1016/j.fct.2012.12.056. [DOI] [PubMed] [Google Scholar]
- 157.Alejo J. L. P., Miranda R., Rodríguez G. Actividad anticonvulsivante (antiepleptica) del extracto fluido de Indigofera suffruticosa (anil cimarron) Revista Cubana de Plantas Medicinais. 1996;1(2):7–10. [Google Scholar]
- 158.Calixto T. G., Gonzalez M. E. R., Wiltshire M. C. P., et al. Tratamiento eficaz con tintura de añil 5 % de una paciente infestada por Pediculus capitis. Revista Cubana de Medicina Tropical y Parasitología. 2011;63(3):275–277. [PubMed] [Google Scholar]
- 159.Coelho G. M. Dissertação. Departamento de Biologia da Escola de Ciências, Universidade do Minho.; 2009. Óleos essenciais para aromaterapia. [Google Scholar]
- 160.Melo J. G., Nascimento V. T., Amorim E. L., Andrade Lima C. S., Albuquerque U. P. Avaliação da qualidade de amostras comerciais de boldo (Peumus boldus Molina), pata-de-vaca (Bauhinia spp.) e ginco (Ginkgo biloba L.) Revista Brasileira de Farmacognosia. 2004;14(2):111–120. doi: 10.1590/S0102-695X2004000200004. [DOI] [Google Scholar]
- 161.Silva I. D., Takatsuka F. S., Rocha M. R., Cunha M. G. Efeito do extrato de sucupira (Pterodon emarginatus Vog.) sobre o desenvolvimento de fungos e bactérias fitopatogênico. Pesquisa Agropecuária Tropical. 2005;35(2):109–115. [Google Scholar]
- 162.Santos A. P., Zatta D. T., Moraes W. F., et al. Composição química, atividade antimicrobiana do óleo essencial e ocorrência de esteróides nas folhas de Pterodon emarginatus Vogel, Fabaceae. Revista Brasileira de Farmacognosia. 2010;20(6):891–896. doi: 10.1590/s0102-695x2010005000052. [DOI] [Google Scholar]
- 163.Bustamante K. G. L., Lima A. D. F., Soares M. L., et al. Avaliação da atividade antimicrobiana do extrato etanólico bruto da casca da sucupira branca (Pterodon emarginatus Vogel)—fabaceae. Revista Brasileira de Plantas Medicinais. 2010;12(3):341–345. doi: 10.1590/s1516-05722010000300012. [DOI] [Google Scholar]
- 164.De Moraes W. F., De Matos L. G., Mariano Nascimento M. V., et al. Anti-inflammatory and anti-nociceptive effects of Pterodon emarginatus stem bark alcohol extract. Pharmaceutical Biology. 2009;47(2):146–150. doi: 10.1080/13880200802436117. [DOI] [Google Scholar]
- 165.Hoscheid J., Cardoso M. L. Sucupira as a potential plant for arthritis treatment and other diseases. Arthritis & Rheumatology. 2015;2015:1–12. doi: 10.1155/2015/379459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Oken B. S., Storzbach D. M., Kaye J. A. The efficacy of Ginkgo biloba on cognitive function in Alzheimer disease. Archives of Neurology. 1998;55(11):1409–1415. doi: 10.1001/archneur.55.11.1409. [DOI] [PubMed] [Google Scholar]
- 167.DeKosky S. T., Williamson J. D., Fitzpatrick A. L., et al. Ginkgo biloba for prevention of dementia: a randomized controlled trial. The Journal of the American Medical Association. 2008;300(19):2253–2262. doi: 10.1001/jama.2008.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Passos C. S., Arbo M. D., Rates S. M. K., von Poser G. L. Terpenóides com atividade sobre o Sistema Nervoso Central (SNC) Revista Brasileira de Farmacognosia. 2009;19(1):140–149. doi: 10.1590/s0102-695x2009000100024. [DOI] [Google Scholar]
- 169.Bigos M., Wasiela M., Kalemba D., Sienkiewicz M. Antimicrobial activity of geranium oil against clinical strains of Staphylococcus aureus. Molecules. 2012;17(9):10276–10291. doi: 10.3390/molecules170910276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Boukhris M., Bouaziz M., Feki I., Jemai H., El Feki A., Sayadi S. Hypoglycemic and antioxidant effects of leaf essential oil of Pelargonium graveolens L’Hér. in alloxan induced diabetic rats. Lipids in Health and Disease. 2012;11(81):1–10. doi: 10.1186/1476-511X-11-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Arroyo J., Almora Y., Condorhuamán M., et al. Efecto del extracto alcohólico de Mimosa pudica (mimosa) sobre la fertilidad en ratas. Anales de la Facultad de Medicina. 2011;71(4):265–270. doi: 10.15381/anales.v71i4.106. [DOI] [Google Scholar]
- 172.Trujillo N. E. G., Toro I. C. D., Anido Y. C., Gra T. R., Ojeda L. S., Graña T. R. Hepatotoxicidad aguda de la decocci≤n de la planta Mimosa pudica em ratas Sprague Dawley. Correo Cientifico Medico. 2014;18(1):25–32. [Google Scholar]
- 173.Rajendran R., Krishnakumar E. Hypolipidemic activity of chloroform extract of Mimosa pudica leaves. Avicenna Journal of Medical Biotechnology. 2010;2(4):215–221. [PMC free article] [PubMed] [Google Scholar]
- 174.Sia F. Y., Vejayan J., Jamuna A., Ambu S. Efficacy of tannins from Mimosa pudica and tannic acid in neutralizing cobra (Naja kaouthia) venom. Journal of Venomous Animals and Toxins including Tropical Diseases. 2011;17(1):42–48. doi: 10.1590/S1678-91992011000100006. [DOI] [Google Scholar]
- 175.Hernández-Abreu O., Castillo-España P., León-Rivera I., et al. Antihypertensive and vasorelaxant effects of tilianin isolated from Agastache mexicana are mediated by NO/cGMP pathway and potassium channel opening. Biochemical Pharmacology. 2009;78(1):54–61. doi: 10.1016/j.bcp.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 176.Hernández-Abreu O., Durán-Gómez L., Best-Brown R., Villalobos-Molina R., Rivera-Leyva J., Estrada-Soto S. Validated liquid chromatographic method and analysis of content of tilianin on several extracts obtained from Agastache mexicana and its correlation with vasorelaxant effect. Journal of Ethnopharmacology. 2011;138(2):487–491. doi: 10.1016/j.jep.2011.09.041. [DOI] [PubMed] [Google Scholar]
- 177.González-Ramírez A., Gonzalez-Trujano M. E., Pellicer F., Lopez-Munoz F. J. Anti-nociceptive and anti-inflammatory activities of the Agastache mexicana extracts by using several experimental models in rodents. Journal os Ethnopharmacology. 2012;142(3):700–705. doi: 10.1016/j.jep.2012.05.044. [DOI] [PubMed] [Google Scholar]
- 178.Verano J., González-Trujano M. E., Déciga-Campos M., Ventura-Martínez R., Pellicer F. Ursolic acid from Agastache mexicana aerial parts produces antinociceptive activity involving TRPV1 receptors, cGMP and a serotonergic synergism. Pharmacology Biochemistry & Behavior. 2013;110:255–264. doi: 10.1016/j.pbb.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 179.González-Trujano M. E., Ponce-Muñoz H., Hidalgo-Figueroa S., Navarrete-Vázquez G., Estrada-Soto S. Depressant effects of Agastache mexicana methanol extract and one of major metabolites tilianin. Asian Pacific Journal of Tropical Medicine. 2015;8(3):185–190. doi: 10.1016/S1995-7645(14)60312-6. [DOI] [PubMed] [Google Scholar]
- 180.Chioca L. R. Tese. Setor de Ciências Biológicas, Universidade Federal do Paraná; 2013. Avaliação do mecanismo de ação do efeito tipo ansiolítico da inalação do óleo essencial de lavanda em camundongos. [Google Scholar]
- 181.Silva L. Dissertação. Instituto de Higiene e Medicina Tropical, Universidade Nova de Lisboa; 2013. Ocorrência, diagnóstico molecular e resistência a antifúngicos de Candida sp. de infecções vaginais em Portugal e Cabo-Verde. [Google Scholar]
- 182.Sariri R., Seifzadeh S., Sajedi R. H. Anti-tyrosinase and antioxidant activity of Lavandula sp. extracts. Pharmacologyonline. 2009;3:319–326. [Google Scholar]
- 183.Pereira A. d., Cardoso M. d., Abreu L. R., Morais A. R., Guimarães L. G., Salgado A. P. Caracterização química e efeito inibitório de óleos essenciais sobre o crescimento de Staphylococcus aureus e Escherichia coli. Ciência e Agrotecnologia. 2008;32(3):887–893. doi: 10.1590/S1413-70542008000300028. [DOI] [Google Scholar]
- 184.Savini I., Arnone R., Catani M. V., Avigliano L. Origanum vulgare Iinduces apoptosis in human colon cancer caco2 cells. Nutrition and Cancer. 2009;61(3):381–389. doi: 10.1080/01635580802582769. [DOI] [PubMed] [Google Scholar]
- 185.Khan A., Bashir S., Khan S. R., Gilani A. H. Antiurolithic activity of Origanum vulgare is mediated through multiple pathways. BMC Complementary and Alternative Medicine. 2011;11, article no. 96:1–16. doi: 10.1186/1472-6882-11-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Battochio A. P. R., Coelho K. L. R., Sartori M. S., Coelho C. A. R. Hepatoprotective effect of water soluble extract of Coleus barbatus on cholestasis on young rats. Acta Cirurgica Brasileira. 2008;23(3):220–229. doi: 10.1590/S0102-86502008000300002. [DOI] [PubMed] [Google Scholar]
- 187.Felisbino S. Monografia. Criciúma , Brazil: Universidade do Extremo Sul Catarinense; 2010. Análise Farmacognóstica de Cunila microcephala Benth. [Google Scholar]
- 188.Paulino R. D. C., Henriques G. P. D. S. A., Moura O. N. S., Coelho M. D. F. B., Azevedo R. A. B. Medicinal plants at the Sítio do Gois, Apodi, Rio Grande do Norte State, Brazil. Revista Brasileira de Farmacognosia. 2011;22(1):29–39. doi: 10.1590/S0102-695X2011005000203. [DOI] [Google Scholar]
- 189.Mishra S. B., Verma A., Mukerjee A., Vijayakumar M. Anti-hyperglycemic activity of leaves extract of Hyptis suaveolens L. Poit in streptozotocin induced diabetic rats. Asian Pacific Journal of Tropical Medicine. 2011;4(9):689–693. doi: 10.1016/S1995-7645(11)60175-2. [DOI] [PubMed] [Google Scholar]
- 190.Ghaffari H., Ghassam B. J., Prakash H. S. Hepatoprotective and cytoprotective properties of Hyptis suaveolens against oxidative stress-induced damage by CCl4 and H2O2. Asian Pacific Journal of Tropical Medicine. 2012;5(11):868–874. doi: 10.1016/S1995-7645(12)60162-X. [DOI] [PubMed] [Google Scholar]
- 191.Vera-Arzave C., Antonio L. C., Arrieta J., et al. Gastroprotection of suaveolol, isolated from hyptis suaveolens, against ethanol-induced gastric lesions in wistar rats: Role of prostaglandins, nitric oxide and sulfhydryls. Molecules. 2012;17(8):8917–8927. doi: 10.3390/molecules17088917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ghaffari H., Ghassam B. J., Chandra Nayaka S., Ramachandra Kini K., Prakash H. S. Antioxidant and neuroprotective activities of Hyptis suaveolens (L.) Poit. against oxidative stress-induced neurotoxicity. Cellular and Molecular Neurobiology. 2014;34(3):323–331. doi: 10.1007/s10571-013-0016-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Moreira Í. J. A., Moreno M. P. N., Fernandes M. F. G., et al. Vasorelaxant effect of Hyptis fruticosa Salzm. ex Benth., Lamiaceae, dichloromethane extract on rat mesenteric artery. Revista Brasileira de Farmacognosia. 2010;20(5):762–766. doi: 10.1590/S0102-695X2010005000003. [DOI] [Google Scholar]
- 194.Novacosk R., Torres R. S. A. Atividade antimicrobiana sinérgica entre óleos essenciais de lavanda (Lavandula officinalis), melaleuca (Melaleuca alternifolia), cedro (Juniperus irginiana), tomilho (Thymus vulgaris) e cravo (Eugenia caryophylatta) Revista Analytica. 2006;21(21):36–39. [Google Scholar]
- 195.Rabiei Z., Rafieian-Kopaei M. Neuroprotective effect of pretreatment with Lavandula officinalis ethanolic extract on blood-brain barrier permeability in a rat stroke model. Asian Pacific Journal of Tropical Medicine. 2014;7(1):S421–S426. doi: 10.1016/S1995-7645(14)60269-8. [DOI] [PubMed] [Google Scholar]
- 196.Alnamer R., Alaoui K., Bouidida E. H., Benjouad A., Cherrah Y. Sedative and hypnotic activities of the methanolic and aqueous extracts of Lavandula officinalis from Morocco. Advances in Pharmacological Sciences. 2012;2012:1–5. doi: 10.1155/2012/270824.270824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Gopal H., Vasanth S., Vasudevan S. V. Antimicrobial activity of essential oil of Leonotis nepetaefolia. Ancient Science of Life. 1994;14:68–70. [PMC free article] [PubMed] [Google Scholar]
- 198.Parra-Delgado H., Ruiz G. G., Camacho A. N., Martínez-Vázquez M. Anti-inflammatory activity of some extracts and isolates from Leonotis nepetaefolia on TPA-induced edema model. Revista de la Sociedad Química de México. 2004;48:293–295. [Google Scholar]
- 199.Cadena-González A. L., Sørensen M., Theilade I. Use and valuation of native and introduced medicinal plant species in Campo Hermoso and Zetaquira, Boyacá, Colombia. Journal of Ethnobiology and Ethnomedicine. 2013;9(1, article no. 23):1–34. doi: 10.1186/1746-4269-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Müzell D. P., Lunardelli A., Leite C. E., et al. Nephroprotective and anti-inflammatory effects of aqueous extract of Melissa officinalis L. on acetaminophen-induced and pleurisy-induced lesions in rats. Brazilian Archives of Biology and Technology. 2013;56(3):383–392. doi: 10.1590/S1516-89132013000300006. [DOI] [Google Scholar]
- 201.Feliú-Hemmelmann K., Monsalve F., Rivera C. Melissa Officinalis and Passiflora caerulea infusion as physiological stress decreaser. International Journal of Clinical and Experimental Medicine. 2013;6(6):444–451. [PMC free article] [PubMed] [Google Scholar]
- 202.Barros L., Dueñas M., Dias M. I., Sousa M. J., Santos-Buelga C., Ferreira I. C. F. R. Phenolic profiles of cultivated, in vitro cultured and commercial samples of Melissa officinalis L. infusions. Food Chemistry. 2013;136(1):1–8. doi: 10.1016/j.foodchem.2012.07.107. [DOI] [PubMed] [Google Scholar]
- 203.de Carvalho N. C., Corrêa-Angeloni M. J. F., Leffa D. D., et al. Evaluation of the genotoxic and antigenotoxic potential of Melissa officinalis in mice. Genetics and Molecular Biology. 2011;34(2):290–297. doi: 10.1590/S1415-47572011000200021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bayat M., Azami Tameh A. A., Ghahremani M. H., et al. Neuroprotective properties of Melissa officinalis after hypoxic-ischemic injury both in vitro and in vivo. DARU Journal of Pharmaceutical Sciences. 2012;20, article 42:1–10. doi: 10.1186/2008-2231-20-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Johnson M., Wesely E. G., Kavitha M. S., Uma V. Antibacterial activity of leaves and inter-nodal callus extracts of Mentha arvensis L. Asian Pacific Journal of Tropical Medicine. 2011;4(3):196–200. doi: 10.1016/S1995-7645(11)60068-0. [DOI] [PubMed] [Google Scholar]
- 206.Santos K. K. A., Matias E. F. F., Souza C. E. S., et al. Anti-Candida activity of Mentha arvensis and Turnera ulmifolia. Journal of Medicinal Food. 2012;15(3):322–324. doi: 10.1089/jmf.2011.0128. [DOI] [PubMed] [Google Scholar]
- 207.Verma S. M., Arora H., Dubey R. Antiinflamatory and sedative hypnotic activity of the methanolic extract of the leaves of Mentha arvensis. Ancient Science of Life. 2003;;23, article 2:95–99. [PMC free article] [PubMed] [Google Scholar]
- 208.Londonkar R. L., Poddar P. V. Studies on activity of various extracts of Mentha arvensis Linn against drug induced gastric ulcer in mammals. World Journal of Gastrointestinal Oncology. 2009;1(1):82–88. doi: 10.4251/wjgo.v1.i1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Stringaro A., Vavala E., Colone M. Effects of Mentha suaveolens essential oil alone or in combination with other drugs in Candida albicans. Evidence-Based Complementary and Alternative Medicine. 2014;2014:9. doi: 10.1155/2014/125904.125904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Pietrella D., Angiolella L., Vavala E., Rachini A., Mondello F., Ragno R. Beneficial effect of Mentha suaveolens essential oil in the treatment of vaginal candidiasis assessed by real-time monitoring of infection. BMC Complementary and Alternative Medicine. 2011;11, article 8 doi: 10.1186/1472-6882-11-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.López V., Martín S., Gómez-Serranillos M. P., Carretero M. E., Jäger A. K., Calvo M. I. Neuroprotective and neurochemical properties of mint extracts. Phytotherapy Research. 2010;24(6):869–874. doi: 10.1002/ptr.3037. [DOI] [PubMed] [Google Scholar]
- 212.Oumzil H., Ghoulami S., Rhajaoui M. Antibacterial and antifungal activity of essential oils of Mentha suaveolens. Phytotherapy Research. 2002;16(8):727–731. doi: 10.1002/ptr.1045. [DOI] [PubMed] [Google Scholar]
- 213.Pereira M. C., Vilela G. R., Costa L. M., et al. Inibição do desenvolvimento fúngico através da utilização de óleos essenciais de condimentos. Ciência e Agrotecnologia. 2006;30(4):731–738. doi: 10.1590/S1413-70542006000400020. [DOI] [Google Scholar]
- 214.Carretto C. d., Junqueira J. C., Almeida R. B., Furlan M. R., Jorge A. O. Antimicrobial activity of Mentha piperita L. against Candida sp. Brazilian Dental Science. 2010;13(1):4–9. doi: 10.14295/bds.2010.v13i1/2.160. [DOI] [Google Scholar]
- 215.Maggiore M. A., Albanese A. A., Gende L. B., Eguaras M. J., Denegri G. M., Elissondo M. C. Anthelmintic effect of Mentha spp. essential oils on Echinococcus granulosus protoscoleces and metacestodes. Parasitology Research. 2012;110(3):1103–1112. doi: 10.1007/s00436-011-2595-x. [DOI] [PubMed] [Google Scholar]
- 216.Barbalho S. M., Machado F. M. V. F., Guiger E. L., et al. Espécies de Mentha podem auxiliar na redução de fatores de risco vascular em pacientes diabéticos. Revista Saúde e Pesquisa. 2011;4(3):387–392. [Google Scholar]
- 217.Jain D., Pathak N., Khan S., et al. Evaluation of cytotoxicity and anticarcinogenic potential of Mentha leaf extracts. International Journal of Toxicology. 2011;30(2):225–236. doi: 10.1177/1091581810390527. [DOI] [PubMed] [Google Scholar]
- 218.Taher Y. A. Antinociceptive activity of Mentha piperita leaf aqueous extract in mice. Libyan Journal of Medicine. 2012;7(1):1–5. doi: 10.3402/ljm.v7i0.16205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Mahboubi M., Haghi G. Antimicrobial activity and chemical composition of Mentha pulegium L. essential oil. Journal of Ethnopharmacology. 2008;119(2):325–327. doi: 10.1016/j.jep.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 220.Arumugam P., Priya N. G., Subathra M., Ramesh A. Anti-inflammatory activity of four solvent fractions of ethanol extract of Mentha spicata L. investigated on acute and chronic inflammation induced rats. Environmental Toxicology and Pharmacology. 2008;26(1):92–95. doi: 10.1016/j.etap.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 221.Tayarani-Najaran Z., Talasaz-Firoozi E., Nasiri R., Jalali N., Hassanzadeh M. K. Antiemetic activity of volatile oil from Mentha spicata and Mentha × piperita in chemotherapy-induced nausea and vomiting. ecancermedicalscience. 2013;7(1, article no. 290):1–6. doi: 10.3332/ecancer.2013.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Arruda T. A., Antunes R. M., Catão R. M., et al. Preliminary study of the antimicrobial activity of Mentha x villosa Hudson essential oil, rotundifolone and its analogues. Revista Brasileira de Farmacognosia. 2006;16(3):307–311. doi: 10.1590/S0102-695X2006000300005. [DOI] [Google Scholar]
- 223.Freitas A. V. L., Azevedo R. A. B., Pereira Y. B., Freitas Neto E. C., Coelho M. F. B. Uses of medicinal plants in Rio Grande do Norte. Journal of Global Biosciences. 2014;3(4):749–762. [Google Scholar]
- 224.Oliveira J. S., Porto L. A., Estevam C. S., et al. Phytochemical screening and anticonvulsant property of Ocimum basilicum leaf essential oil. Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromaticas. 2009;8(3):195–202. [Google Scholar]
- 225.Nakamura C. V., Ueda-Nakamura T., Bando E., Negrão Melo A. F., Garcia Cortez D. A., Dias Filho Filho B. P. Antibacterial activity of Ocimum gratissimum L. essential oil. Memórias do Instituto Oswaldo Cruz. 1999;94(5):675–678. doi: 10.1590/s0074-02761999000500022. [DOI] [PubMed] [Google Scholar]
- 226.Amagase H., Petesch B. L., Matsuura H., Kasuga S., Itakura Y. Intake of garlic and its bioactive components. Journal of Nutrition. 2001;131(3):955–962. doi: 10.1093/jn/131.3.955S. [DOI] [PubMed] [Google Scholar]
- 227.De Aquino Lemos J., Passos X. S., Lisboa Fernandes O. D. F., et al. Antifungal activity from Ocimum gratissimum L. towards Cryptococcus neoformans. Memórias do Instituto Oswaldo Cruz. 2005;100(1):55–58. doi: 10.1590/s0074-02762005000100011. [DOI] [PubMed] [Google Scholar]
- 228.Haida K. S., Parzianello L., Werner S., Garcia D. R., Inácio C. V. Avaliação in vitro da atividade antimicrobiana de oito espécies de plantas medicinais. Arquivos de Ciências da Saúde da UNIPAR. 2007;11(3):185–192. [Google Scholar]
- 229.Al Dhaheri Y., Attoub S., Arafat K., et al. Anti-metastatic and anti-tumor growth effects of Origanum majorana on highly metastatic human breast cancer cells: inhibition of NFκB signaling and reduction of nitric oxide production. PLoS ONE. 2013;8(7):1–17. doi: 10.1371/journal.pone.0068808.e68808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Pimple B. P., Kadam P. V., Patil M. J. Comparative antihyperglycaemic and antihyperlipidemic effect of Origanum majorana extracts in NIDDM rats. Oriental Pharmacy and Experimental Medicine. 2012;12(1):41–50. doi: 10.1007/s13596-011-0047-x. [DOI] [Google Scholar]
- 231.Costa M. C., Nascimento S. C. Atividade citotóxica de Plectranthus barbatus Andr. (Lamiaceae) Revista Acta Farmacêutica Bonaerense [Google Scholar]
- 232.Falé P. L., Madeira P. J., Florêncio M. H., Ascensão L., Serralheiro M. L. Function of Plectranthus barbatus herbal tea as neuronal acetylcholinesterase inhibitor. Food and Function. 2010;2(2):130–136. doi: 10.1039/c0fo00070a. [DOI] [PubMed] [Google Scholar]
- 233.Santos Veríssimo R., Lins T., Assis Bastos M., et al. Antimicrobial activity of Plectranthus barbatus (Lamiacea) BMC Proceedings. 2014;8(Suppl 4) doi: 10.1186/1753-6561-8-S4-P264. [DOI] [Google Scholar]
- 234.Silva N. S., N P. I., Marinho M. L., Santana C. C., Assis M. B., Nóbrega Neto P. I. Utilização do extrato hidroalcoólico de Plectranthus neochilus no controle da dor pós-operatória em gatas. Revista Verde. 2012;7(5):34–40. [Google Scholar]
- 235.Cavalcante A. C. P., Silva A. G. Levantamento etnobotânica e utilização de plantas medicinais na comunidade Moura, Bananeiras-PB. Revista Monografias Ambientais. 2014;14(2):3225–3230. [Google Scholar]
- 236.Silva M. A. S., Silva M. A., Higino J. S., Pereira M. S., Carvalho A. A. T. Atividade antimicrobiana e antiaderente in vitro do extrato de Rosmarinus officinalis Linn. sobre bactérias orais planctônicas. Revista Brasileira de Farmacognosia. 2008;18(2):236–240. doi: 10.1590/S0102-695X2008000200017. [DOI] [Google Scholar]
- 237.Gauch L. M., Pedrosa S. S., Esteves R. A., et al. Antifungal activity of Rosmarinus officinalis Linn. Essential oil against Candida albicans, Candida dubliniensis, Candida parapsilosis and Candida krusei. Revista Pan-Amazônica de Saúde. 2014;5(1):61–66. doi: 10.5123/S2176-62232014000100007. [DOI] [Google Scholar]
- 238.Wang W., Li N., Luo M., Zu Y., Efferth T. Antibacterial activity and anticancer activity of Rosmarinus officinalis L. essential oil compared to that of its main components. Molecules. 2012;17(3):2704–2713. doi: 10.3390/molecules17032704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.MacHado D. G., Cunha M. P., Neis V. B., et al. Antidepressant-like effects of fractions, essential oil, carnosol and betulinic acid isolated from Rosmarinus officinalis L. Food Chemistry. 2013;136(2):999–1005. doi: 10.1016/j.foodchem.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 240.Lucarini R., Bernardes W. A., Ferreira D. S., et al. In vivo analgesic and anti-inflammatory activities of Rosmarinus officinalis aqueous extracts, rosmarinic acid and its acetyl ester derivative. Pharmaceutical Biology. 2013;51(9):1087–1090. doi: 10.3109/13880209.2013.776613. [DOI] [PubMed] [Google Scholar]
- 241.Habtemariam S. The therapeutic potential of rosemary (Rosmarinus officinalis) Diterpenes for Alzheimer's Disease. Evidence-Based Complementary and Alternative Medicine. 2016;2016:1–15. doi: 10.1155/2016/2680409.2680409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Ozarowski M., Mikolajczak P. L., Bogacz A., et al. Rosmarinus officinalis L. leaf extract improves memory impairment and affects acetylcholinesterase and butyrylcholinesterase activities in rat brain. Fitoterapia. 2013;91:261–271. doi: 10.1016/j.fitote.2013.09.012. [DOI] [PubMed] [Google Scholar]
- 243.Satoh T., Kosaka K., Itoh K., et al. Carnosic acid, a catechol-type electrophilic compound, protects neurons both in vitro and in vivo through activation of the Keap1/Nrf2 pathway via S-alkylation of targeted cysteines on Keap. Journal of Neurochemistry. 2008;104(4):1116–1131. doi: 10.1111/j.1471-4159.2007.05039.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Piccinelli A. C., Figueiredo de Santana Aquino D., Morato P. N., et al. Anti-inflammatory and antihyperalgesic activities of ethanolic extract and fruticulin a from salvia lachnostachys leaves in mice. Evidence-Based Complementary and Alternative Medicine. 2014;2014:1–8. doi: 10.1155/2014/835914.835914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Jimenez J., Risco S., Ruiz T., Zarzuelo A. Hypoglycemic activity of Salvia lavandulifolia. Planta Medica. 1986;4:260–262. [PubMed] [Google Scholar]
- 246.Porres Martínez M., Gómez-Serranillos M. P., Carretero Accame M. E. Neuroprotective activity of Salvia lavandulifolia Vahl. Essential oil. Ars Pharmaceutica. 2010;51(3):657–675. [Google Scholar]
- 247.Tosun A., Khan S., Kim Y. S., Calín-Sánchez A., Hysenaj X. Essential oil composition and anti-inflammatory activity of Salvia officinalis L. (Lamiaceae) in murin macrophages. Tropical Journal of Pharmaceutical Research. 2014;13(6):111–116. doi: 10.4314/tjpr.v13i6.16. [DOI] [Google Scholar]
- 248.Qnais E. Y., Abu-Dieyeh M., Abdulla F. A., Abdalla S. S. The antinociceptive and anti-inflammatory effects of Salvia officinalis leaf aqueous and butanol extracts. Pharmaceutical Biology. 2010;48(10):1149–1156. doi: 10.3109/13880200903530763. [DOI] [PubMed] [Google Scholar]
- 249.Lima I. O., Oliveira R. A. G., Lima E. O., Farias N. M. P., Souza E. L. Atividade antifúngica de óleos essenciais sobre espécies de Candida. Brazilian Journal of Pharmacognosy. 2006;16(2):197–201. [Google Scholar]
- 250.Freire J. M., Cardoso M. G., Batista L. R., Andrade M. A. Essential oil of Origanum majorana L., Illicium verum Hook. f. and Cinnamomum zeylanicum Blume: Chemical and antimicrobial characterization. Revista Brasileira de Plantas Medicinais. 2011;13(2):209–214. doi: 10.1590/S1516-05722011000200013. [DOI] [Google Scholar]
- 251.Ranjbar A., Ghasmeinezhad S., Zamani H., et al. Antioxidative stress potential of Cinnamomum zeylanicum in humans: A comparative cross-sectional clinical study. Thérapie. 2006;3(1):113–117. doi: 10.1586/14750708.3.1.113. doi: 10.1586/14750708.3.1.113. [DOI] [Google Scholar]
- 252.Tailang M., Gupta B. K., Sharma A. Antidiabetic activity of alcoholic extract of Cinnamomum zeylanicum leaves in alloxon induced diabetic rats. Peoples Journal of Scientific Research. 2008;(1):9–11. [Google Scholar]
- 253.Alves E. O., Mota J. H., Soares T. S., Vieira M. C., Silva C. B. Levantamento etnobotânico e caracterização de plantas medicinais em fragmentos florestais de Dourados-MS. Ciência e Agrotecnologia. 2008;32(2):651–658. doi: 10.1590/S1413-70542008000200048. [DOI] [Google Scholar]
- 254.Tondolo J. S. M., De Amaral L. P., Simões L. N., et al. Anesthesia and transport of fat snook snook Centropomus parallelus with the essential oil of Nectandra megapotamica (Spreng.) Mez. Neotropical Ichthyology. 2013;11(3):667–674. doi: 10.1590/S1679-62252013000300020. [DOI] [Google Scholar]
- 255.Vieira R. A., Lapa A. J., Lima T. C. Evaluation of the central activity of the ethanolic extract of Acosmium subelegans (Mohlenbr) in mice. Revista Brasileira de Farmacognosia. 2002;12(supplement 1):50–51. doi: 10.1590/S0102-695X2002000300024. [DOI] [Google Scholar]
- 256.Doughari J. H. Antimicrobial activity of Tamarindus indica Linn. Tropical Journal of Pharmaceutical Research. 2006;5(2):597–603. [Google Scholar]
- 257.Teixeira A. H., Bezerra M. M., Chaves H. V., Val D. R., Filho S. M. P., Silva A. A. R. Conhecimento popular sobre o uso de plantas medicinais no município de Sobral-Ceará, Brasil. Sanare [Google Scholar]
- 258.Souza M. D., Fernandes R. R., Pasa M. C. Estudo etnobotânico de plantas medicinais na comunidade São Gonçalo beira rio, Cuiabá, MT. Revista Biodiversidade. 2010;9(1):91–100. [Google Scholar]
- 259.Canuto G. A. B., Xavier A. A. O., Leandro C. N., de Benassi M. T. Physical and chemical characterization of fruit pulps from Amazonia and their correlation to free radical scavenger activity. Revista Brasileira de Fruticultura. 2010;32(4):1196–1205. doi: 10.1590/S0100-29452010005000122. [DOI] [Google Scholar]
- 260.Khalid S., Shaik Mossadeq W. M., Israf D. A., et al. In vivo analgesic effect of aqueous extract of tamarindus indica L. fruits. Medical Principles and Practice. 2010;19(4):255–259. doi: 10.1159/000312710. [DOI] [PubMed] [Google Scholar]
- 261.Suralkaz A. A., Rodge K. N., Kamble R. D., Maske K. S. Evaluation of anti-inflammatory and analgesic activities of Tamarindus indica seeds. International Journal of Pharmaceutical Sciences and Drug Research. 2012;4(3):213–217. [Google Scholar]
- 262.Tayade P. M., Jadhav B., Angadi S. S., et al. Anti-histaminic activity of methanolic extract of leaves of Tamarindus indica Linn. Journal of Chemical and Pharmaceutical Sciences. 2009;2(4):273–277. [Google Scholar]
- 263.Kalra P., Sharma S., Suman S. K. Antiulcer effect of the methanolic extract of Tamarindus indicaseeds in different experimental models. Journal of Pharmacy and Bioallied Sciences. 2011;2(3):236–241. doi: 10.4103/0975-7406.80778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Singi G., Damasceno D., D'Andréa E., Silva G. Efeitos agudos dos extratos hidroalcólicos do alho (Allium sativum L.) e do capim-limão (Cymbopogon citratus (DC.) Stapf) sobre a pressão arterial média de ratos anestesiados. Revista Brasileira de Farmacognosia. 2005;15(2):94–97. doi: 10.1590/S0102-695X2005000200004. [DOI] [Google Scholar]
- 265.Almeida G. D., Godoi E. P., Santos E. C., Lima L. R. P., Oliveira M. E. Extrato aquoso de Allium sativum potencializa a ação dos antibióticos vancomicina, gentamicina e tetraciclina frente Staphylococcus aureus. Revista de Ciências Farmacêuticas Básica e Aplicada. 2013;34(4):487–492. [Google Scholar]
- 266.Tope S. A., Sunday O. F., Gabriel A. T. Mechanisms of antiulcerogenic effect of garlic (Allium sativum) in albino rats. European Journal of Medicinal Plants. 2013;4(5):571–578. [Google Scholar]
- 267.Riba J., Romero S., Grasa E., Mena E., Carrió I., Barbanoj M. J. Increased frontal and paralimbic activation following ayahuasca, the pan-amazonian inebriant. Psychopharmacology. 2006;186(1):93–98. doi: 10.1007/s00213-006-0358-7. [DOI] [PubMed] [Google Scholar]
- 268.Santos R. G., Moraes C. C., Holanda A. Ayahuasca e redução do uso abusivo de psicoativos: eficácia terapêutica? Psicologia: Teoria e Pesquisa. 2006;22(3):363–370. doi: 10.1590/S0102-37722006000300014. [DOI] [Google Scholar]
- 269.Pires A. P. S., Oliveira C. D. R., Yonamine M. Ayahuasca: a review of pharmacological and toxicologia aspects. Revista de Ciências Farmacêutica Básica e Ampliada. 2010;31(1):15–23. [Google Scholar]
- 270.Motta L. S. G. D. Dissertação - Mestrado em Ciências da Saúde. Universidade de Brasilia; 2013. Toxicidade aguda, neurotoxicidade reprodutiva e embriotoxicidade do chá ayahuasca (Banisteriopsis caapi e Psychotria viridis) em ratas wistar. [Google Scholar]
- 271.Tortoriello J., Herrera-Arellano A., Herrera-Ruiz M. L., Rojas-Bribiesca G., Zamilpa A., Gonzáles V. PL04 Aplicación clinica de um ansiolítico obtenido de Galphimia glauca. Revista de Fitoterapia. 2006;6(supplement 1):37–40. [Google Scholar]
- 272.Ribeiro J. A. C. Dissertation. Porto, Portugal: Faculdade de Ciênias da Saúde, Universidade Fernando Pessoa; 2014. A Cannabis e suas aplicações terapêuticas. [Google Scholar]
- 273.Honório K. M., Arroio A., Silva A. B. Aspectos terapêuticos de compostos da planta Cannabis sativa. Química Nova. 2006;29(2):318–325. doi: 10.1590/S0100-40422006000200024. [DOI] [Google Scholar]
- 274.Hill A. J., Williams C. M., Whalley B. J., Stephens G. J. Phytocannabinoids as novel therapeutic agents in CNS disorders. Pharmacology & Therapeutics. 2012;133(1):79–97. doi: 10.1016/j.pharmthera.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 275.Zuardi A. W., Crippa J. A. S., Hallak J. E. C., Moreira F. A., Guimarães F. S. Cannabidiol, a Cannabis sativa constituent, as an antipsychotic drug. Brazilian Journal of Medical and Biological Research. 2006;39(4):421–429. doi: 10.1590/s0100-879x2006000400001. [DOI] [PubMed] [Google Scholar]
- 276.Pedrazzi J. F., Pereira A. C., Gomes F. V., Bel E. D. Perfil antipsicótico do canabidiol. Medicina. 2014;47(2):112–119. doi: 10.11606/issn.2176-7262.v47i2p112-119. [DOI] [Google Scholar]
- 277.Ribeiro J. A. C. A cannabis e suas aplicações terapêuticas. Porto, Portugal: Universidade Fernando Pessoa. Faculdade de Ciencias da Saude.; 2014. (Dissertatiom). [Google Scholar]
- 278.Ruppelt B. M., Pereira E. F., Gonçalves L. C., Pereira N. A. Pharmacological screening of plants recommended by folk medicine as anti-snake venom - I. analgesical and anti-inflamatory activities. Memórias do Instituto Oswaldo Cruz. 1991;86(supplement 2):203–205. doi: 10.1590/s0074-02761991000600046. [DOI] [PubMed] [Google Scholar]
- 279.Arise R. O., Malomo S. O., Adebayo J. O., Igunnu A. Effects of aqueous extract of Eucalyptus globulus on lipid peroxidation and selected enzymes of rat liver. Journal of Medicinal Plants Research. 2009;3(2):77–81. [Google Scholar]
- 280.Bachir R. G., Benali M. Antibacterial activity of the essential oils from the leaves of Eucalyptus globulus against Escherichia coli and Staphylococcus aureus. Asian Pacific Journal of Tropical Biomedicine. 2012;2(9):739–742. doi: 10.1016/S2221-1691(12)60220-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Damjanović-Vratnica B., Đakov T., Šuković D., Damjanović J. Antimicrobial effect of essential oil isolated from Eucalyptus globulus Labill. from Montenegro. Czech Journal of Food Sciences. 2011;29(3):277–284. doi: 10.17221/114/2009-CJFS. [DOI] [Google Scholar]
- 282.Alves E. O., Mota J. H., Soares T. S., Vieira M. C., Silva C. B. Levantamento etnobotânico e caracterização de plantas medicinais em fragmentos florestais de Dourados-MS. Ciência e Tecnologia. 2008;32(2):651–658. doi: 10.1590/S1413-70542008000200048. [DOI] [Google Scholar]
- 283.Auricchio M. T., Bugno A., Barros S. B. M., Bacchi E. M. Atividades antimicrobiana e antioxidante e toxicidade de Eugenia uniflora. Latin American Journal of Pharmacy. 2006;1(26):78–81. [Google Scholar]
- 284.Das B. N., Ahmed M. Analgesic activity of fruit extract of Averrhoa carambola. International Journal of Life Sciences Biotechnology and Pharma Research. 2013;1(3):22–26. [Google Scholar]
- 285.Romanini C. V., Machado M. W., Biavatti M. W., Oliveira R. M. W. Avaliação da atividade ansiolítica e antidepressiva do extrato fluido e fração aquosa de folhas de Passiflora alata Curtis em camundongos. Acta Scientarum Health Sciences. 2006;28(2):159–164. doi: 10.4025/actascihealthsci.v28i2.1100. [DOI] [Google Scholar]
- 286.Pirondo A., Coulleri J. P., Keller H. A., Ferruci M. S. Influencia de factores externos sobre La comercialización de plantas medicinales em um medio urbano: el caso de vendedores criollos e indígenas en Corrientes, Argentina. Boletín Latinoamericano y del Caribe de Plantas Medicinales y Aromaticas. 2011;10(6):553–569. [Google Scholar]
- 287.Wolfman C., Viola H., Paladini A., Dajas F., Medina J. H. Possible anxiolytic effects of chrysin, a central benzodiazepine receptor ligand isolated from Passiflora coerulea. Pharmacology Biochemistry & Behavior. 1994;47(1):1–4. doi: 10.1016/0091-3057(94)90103-1. [DOI] [PubMed] [Google Scholar]
- 288.Coleta M., Batista M. T., Campos M. G., et al. Neuropharmacological evaluation of the putative anxiolytic effects of Passiflora edulis Sims, its sub-fractions and flavonoid constituents. Phytotherapy Research. 2006;20(12):1067–1073. doi: 10.1002/ptr.1997. [DOI] [PubMed] [Google Scholar]
- 289.Figueiredo A. S., Modesto-Filho J. Efeito do uso da farinha desemgordura do Sesamum indicum L nos níveis glícemicos em diabetics tipo 2. Revista Brasileira de Farmacognosia. 2008;18(1):77–83. doi: 10.1590/S0102-695X2008000100015. [DOI] [Google Scholar]
- 290.Pantojas S. C. C. S., Sul N. A. S., Miguel N. N. N. Levantamento etnobotânico de Petiveria alliacea L. (phytolaccaceae) comercializadas no mercadão de Madureira – RJ. Revista Eletrônica Novo Enfoque. 2013;17(17):184–190. [Google Scholar]
- 291.Guedes R. C. M., Nogueira N. G. P., Almeida A. M. F., Souza C. R., Oliveira W. P. Atividade antimicrobiana de extratos brutos de Petiveria alliacea L. Latin American Journal of Pharmacy. 2009;28(4):520–524. [Google Scholar]
- 292.Gomes B. P. Dissertação. Universidade Federal do Ceará, Faculdade de Medicina; 2006. Avaliação dos efeitos centrais e atinociceptivos das frações isoladas da raiz de Petiveria alliacea (TIPI) em camundongos. [Google Scholar]
- 293.Fernandes K. S., Silva A. H. M., Mendanha S. A., Rezende K. R., Alonso A. Antioxidant effect of 4- nerolidylcatechol and α-tocopherol in erythrocyte ghost membranes and phospholipid bilayers. Brazilian Journal of Medical and Biological Research. 2013;46(9):780–788. doi: 10.1590/1414-431X20132940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Sacoman J. L., Monteiro K. M., Possenti A., Figueira G. M., Foglio M. A., Carvalho J. E. Cytotoxicity and antitumoral activity of dichloromethane extract and its fractions from Pothomorphe umbellate. Brazilian Journal of Medical and Biological Research. 2008;41(5):411–415. doi: 10.1590/S0100-879X2008000500010. [DOI] [PubMed] [Google Scholar]
- 295.Ferreira L., Castro P., Suzelei F., Rene B. In vitro anthelmintic activity of Pothomorphe umbellata (L.) Miq. (Piperaceae) against gastrointestinal parasites from sheep. BMC Proceedings. 2014;8, article 155(supplement 4) doi: 10.1186/1753-6561-8-S4-P155. [DOI] [Google Scholar]
- 296.Miranda G. S., Souza S. R., Amaro M. O. F., Rosa M. B., Carvalho C. A. Avaliação do conhecimento etnofarmacológico da população de Teixeiras- MG, Brasil. Brasil. Revista de Ciências Farmacêuticas Básica e Aplicada. 2013;34(4):559–563. [Google Scholar]
- 297.Blanco M. M., Costa C. A. R. A., Freire A. O., Santos J. G., Jr., Costa M. Neurobehavioral effect of essential oil of Cymbopogon citratus in mice. Phytomedicine. 2009;16(2-3):265–270. doi: 10.1016/j.phymed.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 298.Nogueira F., Fernandes S., Reis G., et al. Atividade analgésica e antiedematogênica de Polygala paniculata L. (Poygalaceae) selvagem e obtida por micropigmentação. Brazilian Journal of Pharmacognosy. 2005;15(4):310–315. [Google Scholar]
- 299.Lapa R. F. Dissertação. Departamento de Farmacologia, Setor e Ciências Biológicas, Universidade Federal do Paraná; 2006. Avaliação da atividade antinociceptiva, antiinflamatória e protetora gástrica do extrato hidroalcoólico bruto da Polygala paniculata L. [Google Scholar]
- 300.Nuria M. C. Antibacterial activities from Jangkang (Homalocladium platycladum (F. Muell) Bailey) Leaves. Mediagro. 2010;6(2):9–15. [Google Scholar]
- 301.Perazzo F. F., Souza G. H. B., Lopes W., et al. Anti-inflammatory and analgesic properties of water–ethanolic extract from Pothomorphe umbellata (Piperaceae) aerial parts. Journal of Ethnopharmacology. 2005;99(2):215–220. doi: 10.1016/j.jep.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 302.Kumar R., Nair V., Gupta Y. K., Singh S. Anti-inflammatory and anti-arthritic activity of aqueous extract of Rosa centifolia in experimental models in rats. International Journal of Rheumatic Diseases. 2015 doi: 10.1111/1756-185X.12625. [DOI] [PubMed] [Google Scholar]
- 303.Selvan C. T., Velavan S., Milton M. C. J. Antioxidant activity of Rosa centifolia flowers. International Journal of Research in Plant Science. 2014;4(3):68–71. [Google Scholar]
- 304.Chandragopal S., Kumar S., Archana B. Evaluations of anti-ulcer activity of Rosa centifolia (Linn) flowers in experimental rats. Journal of Natural Remedies. 2012;12(1):22–29. [Google Scholar]
- 305.Ferreira A., Proença C., Serralheiro M. L. M., Araújo M. E. M. The in vitro screening for acetylcholinesterase inhibition and antioxidant activity of medicinal plants from Portugal. Journal of Ethnopharmacology. 2006;108(1):31–37. doi: 10.1016/j.jep.2006.04.010. [DOI] [PubMed] [Google Scholar]
- 306.Andrade S. K. Dissertação. Universidade Federal de Santa Catarina, Programa de Pó-Graduação em Engenharia de Alimentos; 2011. Avaliação das técnicas de extração e do potencial antioxidante dos estratos obtidos a partir de casca e de borra de café (Coffea arábica) [Google Scholar]
- 307.Motta. Dissertação. Universidade de Brasília; 2013. Luciana Soares Gueiros da. Toxicidade aguda, neurotoxicidade reprodutiva e embriotoxicidade do chá ayahuasca (Banisteriopsis caapi e Psychotria viridis) em ratas wistar. [Google Scholar]
- 308.Santos V. L., Costa V. B. M., Agra M. F., Silva B. A., Batista L. M. Pharmacological studies of ethanolic extracts of Maytenus rigida Mart (Celastraceae) in animal models. Revista Brasileira de Farmacognosia. 2007;17(3):336–342. [Google Scholar]
- 309.Bertin R., Garcia-Argaéz A., Martnez-Vzquez M., Froldi G. Age-dependent vasorelaxation of Casimiroa edulis and Casimiroa pubescens extracts in rat caudal artery in vitro. Journal of Ethnopharmacology. 2011;137(1):934–936. doi: 10.1016/j.jep.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 310.Froldi G., Bertin R., Secchi E., Zagotto G., Martínez-Vázquez M., García-Argaéz A. Vasorelaxation by extracts of Casimiroa spp. in rat resistance vessels and pharmacological study of cellular mechanisms. Journal of Ethnopharmacology. 2011;134(3):637–643. doi: 10.1016/j.jep.2011.01.008. [DOI] [PubMed] [Google Scholar]
- 311.Molina-Hernández M., Tellez-Alcántara N. P., Pérez García J., Lopez J. I. O., Jaramillo M. T. Anxiolytic-like actions of leaves of Casimiroa edulis (Rutaceae) in male Wistar rats. Journal of Ethnopharmacology. 2004;93(1):93–98. doi: 10.1016/j.jep.2004.03.039. [DOI] [PubMed] [Google Scholar]
- 312.Mora S., Diaz-Veliz G., Lungenstrass H., et al. Central nervous system activity of the hydroalcoholic extract of Casimiroa edulis in rats and mice. Journal of Ethnopharmacology. 2005;97(2):191–197. doi: 10.1016/j.jep.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 313.Arbo D. M. Dissertação. Faculdade de Farmácia, Programa de Pós-Graduação em Ciências Farmacêuticcas, UFRGS; 2008. Avaliação toxicológica de p-sinefrina e extrato de Citrus aurantium L. (Rutaceae) [Google Scholar]
- 314.Costa C. A. R. A., Cury T. C., Cassettari B. O., Takahira R. K., Flório J. C., Costa M. Citrus aurantium L. essential oil exhibits anxiolytic-like activity mediated by 5-HT1A-receptors and reduces cholesterol after repeated oral treatment. BMC Complementary and Alternative Medicine. 2013;13(42):1–10. doi: 10.1186/1472-6882-13-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Akhlaghi M., Shanamian G., Rafieian-Kopaei M., Parvin N., Saadat M., Akhlaghi M. Flor de Citrus aurantium e ansiedade pré-operatória. Revista Brasileira de Anestesiologia. 2011;61:702–712. doi: 10.1016/S0034-7094(11)70079-4. [DOI] [PubMed] [Google Scholar]
- 316.Campêlo L. M. L., de Almeida A. A. C., de Freitas R. L. M., et al. Antioxidant and antinociceptive effects of Citrus limon essential oil in mice. Journal of Biomedicine and Biotechnology. 2011;2011:8. doi: 10.1155/2011/678673.678673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Parmar H. S., Kar A. Antiperoxidative, antithyroidal, antihyperglycemic and cardioprotective role of Citrus sinensis peel extract in male mice. Phytotherapy Research. 2008;22(6):791–795. doi: 10.1002/ptr.2367. [DOI] [PubMed] [Google Scholar]
- 318.Nogueira J. C., Diniz M. d., Lima E. O. Atividade antimicrobiana in vitro de produtos vegetais em otite externa aguda. Brazilian Journal of Otorhinolaryngology. 2008;74(1):118–124. doi: 10.1590/S0034-72992008000100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Asolini F. C., Tedesco A. M., Carpes S. T., Ferraz C., Alencar S. D. Atividade antioxidante e antibacteriana dos compostos fenólicos dos extratos de plantas usadas como chás. Brazilian Journal of Food Technology [Google Scholar]
- 320.Preethi K. C., Kuttan G., Kuttan R. Anti-Tumour activity of Ruta Graveolens extract. Asian Pacific Journal of Cancer Prevention. 2006;7(3):439–443. [PubMed] [Google Scholar]
- 321.Loonat F., Amabeoku G. J. I. Antinociceptive, anti-inflammatory and antipyretic activities of the leaf methanol extract of Ruta graveolens L. (Rutaceae) in mice and rats. African Journal of Traditional, Complementtary and Alternative Medicine. 2014;11(3):173–181. doi: 10.4314/ajtcam.v11i3.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Gál P., Toporcer T., Grendel T., et al. Effect of Atropa belladonna L. on skin wound healing: Biomechanical and histological study in rats and in vitro study in keratinocytes, 3T3 fibroblasts, and human umbilical vein endothelial cells. Wound Repair and Regeneration. 2009;17(3):378–386. doi: 10.1111/j.1524-475X.2009.00475.x. [DOI] [PubMed] [Google Scholar]
- 323.Guerra M. J. M., Barreiro M. L., Rodríguez Z. M., Rodríguez E. B., Hernádez A. I. Actividad antimicrobiana e irritabiliadad vaginal e dérmica de estractos acuosos de hojas secas de Solanum americanum Mill. Revista Cubana de Plantas Medicinales. 2009;14:1–8. [Google Scholar]
- 324.Aboul-Eneim A. M., El-Ela F. A., Shalaby E. A., El-Shemy H. A. Potent anticancer and antioxidant activities of active ingredients separated from Solanum nigrum and Cassia italica extracts. Journal of Arid Land Studies. 2014;24(1):145–152. [Google Scholar]
- 325.Araújo C. E. P., Rodrigues R. F. O., Oliveira F., Schreiner L. Análise preliminar da atividade antiulcerogênica do extrato hidroalcoólico de Solanum cernuum Vell. Acta Farmacéutica Bonaerense. 2002;21(4):283–286. [Google Scholar]
- 326.Zeng H., Tian J., Zheng Y., et al. In vitro and in vivo activities of essential oil from the seed of Anethum graveolens L. against Candida spp. Evidence-Based Complementary and Alternative Medicine. 2011;2011:8. doi: 10.1155/2011/659704.659704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Arash A., Mohammad M.-Z., Jamal M. S., Mohammad T. A., Azam A. Effects of the aqueous extract of anethum graveolens leaves on seizure induced by pentylenetetrazole in mice. Malaysian Journal of Medical Sciences. 2013;20(5):23–30. [PMC free article] [PubMed] [Google Scholar]
- 328.Masadeh M. M., Alkofahi A. S., Alzoubi K. H., Tumah H. N., Bani-Hani K. Anti-Helicobactor pylori activity of some Jordanian medicinal plants. Pharmaceutical Biology. 2014;52(5):566–569. doi: 10.3109/13880209.2013.853811. [DOI] [PubMed] [Google Scholar]
- 329.Monsefi M., Zahmati M., Masoudi M., Javidnia K. Effects of Anethum graveolens L. on fertility in male rats. The European Journal of Contraception and Reproductive Health Care. 2011;16(6):488–497. doi: 10.3109/13625187.2011.622815. [DOI] [PubMed] [Google Scholar]
- 330.Panda B. B., Gaur K., Kori M. L., et al. Anti-inflammatory and analgesic activity of Jatropha gossypifoliain experimental animal models. Global Journal of Pharmacology. 2009;3(1):1–5. [Google Scholar]
- 331.Lo Cantore P., Iacobellis N. S., De Marco A., Capasso F., Senatore F. Antibacterial activity of Coriandrum sativum L. and Foeniculum vulgare Miller var. vulgare (miller) essential oils. Journal of Agricultural and Food Chemistry. 2004;52(26):7862–7866. doi: 10.1021/jf0493122. [DOI] [PubMed] [Google Scholar]
- 332.Rajeshwari C. U., Siri S., Andallu B. Antioxidant and antiarthritic potential of coriander (Coriandrum sativum L.) leaves. Clinical Nutrition Espen. 2012;7(6):223–228. doi: 10.1016/j.clnme.2012.09.005. [DOI] [Google Scholar]
- 333.Silva F., Ferreira S., Duarte A., Mendona D. I., Domingues F. C. Antifungal activity of Coriandrum sativum essential oil, its mode of action against Candida species and potential synergism with amphotericin B. Phytomedicine. 2011;19(1):42–47. doi: 10.1016/j.phymed.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 334.Aissaoui A., Zizi S., Israili Z. H., Lyoussi B. Hypoglycemic and hypolipidemic effects of Coriandrum sativum L. in Meriones shawi rats. Journal of Ethnopharmacology. 2011;137(1):652–661. doi: 10.1016/j.jep.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 335.Campos K. E., Balbi A. P. C., Alves M. J. Q. D. F. Diuretic and hipotensive activity of aqueous extract of parsley seeds (Petroselinum sativum Hoffm.) in rats. Revista Brasileira de Farmacognosia. 2009;19(1):41–45. doi: 10.1590/S0102-695X2009000100010. [DOI] [Google Scholar]
- 336.Gindri A. L., Silva M., Marchi M. B., Brum L. S., Athayde M. L., Hoelze S. C. S. M. Análise fitoquímica das cascas e do miolo da raiz de Urera baccifera (L.) Gaudich (Urticaceae) Saúde. 2010;36(2):63–70. [Google Scholar]
- 337.Badilla B., Mora G., Lapa A. J., Emim J. A. S. Anti-inflammatory activity of Urera baccifera (Urticaceae) in Sprague-Dawley rats. Revista de Biología Tropical. 1999;47(3):365–371. [PubMed] [Google Scholar]
- 338.Calzada F., Arista R., Pérez H. Effect of plants used in Mexico to treat gastrointestinal disorders on charcoal-gum acacia-induced hyperperistalsis in rats. Journal of Ethnopharmacology. 2010;128(1):49–51. doi: 10.1016/j.jep.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 339.Rojas J., Solís H., Palacios O. Evaluación in vitro de la actividad anti Trypanosoma cruzi de aceites esenciales de diez plantas medicinales. Anales de la Facultad de Medicina. 2010;71(3):161–165. doi: 10.15381/anales.v71i3.89. [DOI] [Google Scholar]
- 340.Parodi T. V., de Castagna Vargas A. P., Krewer C., et al. Chemical Composition and Antibacterial Activity of Aloysia triphylla (L'Hérit) Britton Extracts Obtained by Pressurized CO2 Extraction. Brazilian Archives of Biology and Technology. 2013;56(2):283–292. doi: 10.1590/S1516-89132013000200014. [DOI] [Google Scholar]
- 341.Ponce-Monter H., Fernández-Martínez E., Ortiz M. I., et al. Spasmolytic and anti-inflammatory effects of Aloysia triphylla and citral, in vitro and in vivo studies. Journal of Smooth Muscle Research. 2010;46(6):309–319. doi: 10.1540/jsmr.46.309. [DOI] [PubMed] [Google Scholar]
- 342.Costa J. G. M., Sousa E. O., Rodrigues F. F. G., de Lima S. G., Braz-Filho R. Composição química e avaliação das atividades antibacteriana e de toxicidade dos óleos essenciais de Lantana camara L. e Lantana sp. Revista Brasileira de Farmacognosia. 2008;19(3):710–714. [Google Scholar]
- 343.Mahdi-Pour B., Jothy S. L., Latha L. Y., Chen Y., Sasidharan S. Antioxidant activity of methanol extracts of different parts of Lantana camara. Asian Pacific Journal of Tropical Biomedicine. 2012;2(12):960–965. doi: 10.1016/S2221-1691(13)60007-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Kazmi I., Afzal M., Ali B., Damanhouri Z. A., Ahmaol A., Anwar F. Anxiolytic potential of ursolic acid derivative-a stearoyl glucoside isolated from Lantana camara L. (verbanaceae) Asian Pacific Journal of Tropical Medicine. 2013;6(6):433–437. doi: 10.1016/S1995-7645(13)60069-3. [DOI] [PubMed] [Google Scholar]
- 345.Barbosa-Filho J. M., Medeiros K. C. P., Diniz M. F. F. M., et al. Natural products inhibitors of the enzyme acetylcholinesterase. Revista Brasileira de Farmacognosia. 2006;16(2):258–285. doi: 10.1590/S0102-695X2006000200021. [DOI] [Google Scholar]
- 346.Blanco M. A., Colareda G. A., Van Baren C., Bandoni A. L., Ringuelet J., Consolini A. E. Antispasmodic effects and composition of the essential oils from two South American chemotypes of Lippia alba. Journal of Ethnopharmacology. 2013;149(3):803–809. doi: 10.1016/j.jep.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 347.Hatano V. Y., Torricelli A. S., Giassi A. C. C., Coslope L. A., Viana M. B. Anxiolytic effects of repeated treatment with an essential oil from Lippia alba and (R)-(-)-carvone in the elevated T-maze. Brazilian Journal of Medical and Biological Research. 2012;45(3):238–243. doi: 10.1590/S0100-879X2012007500021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Sousa D. G., Sousa S. D. G., Silva R. E. R., et al. Essential oil of Lippia alba and its main constituent citral block the excitability of rat sciatic nerves. Brazilian Journal of Medical and Biological Research. 2015;48(8):697–702. doi: 10.1590/1414-431X20154710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Bitu V. C. N., Fecundo H. D. T. F., Costa J. G. M., et al. Chemical composition of the essential oil of Lippia gracilis Schauer leaves and its potential as modulator of bacterial resistance. Natural Product Research (Formerly Natural Product Letters) 2014;28(6):399–402. doi: 10.1080/14786419.2013.867343. [DOI] [PubMed] [Google Scholar]
- 350.Ferraz R. P. C., Bomfim D. S., Carvalho N. C., et al. Cytotoxic effect of leaf essential oil of Lippia gracilis Schauer (Verbenaceae) Phytomedicine. 2013;20(7):615–621. doi: 10.1016/j.phymed.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 351.Riella K. R., Marinho R. R., Santos J. S., et al. Anti-inflammatory and cicatrizing activities of thymol, a monoterpene of the essential oil from Lippia gracilis, in rodents. Journal of Ethnopharmacology. 2012;143(2):656–663. doi: 10.1016/j.jep.2012.07.028. [DOI] [PubMed] [Google Scholar]
- 352.Gerlach S. L., Rathinakumar R., Chakravarty G., et al. Anticancer and chemosensitizing abilities of cycloviolacin O2 from Viola odorata and psyle cyclotides from Psychotria leptothyrsa. Peptide Science. 2010;94(5):617–625. doi: 10.1002/bip.21435. [DOI] [PubMed] [Google Scholar]
- 353.Akhbari M., Batooli H., Kashi F. J. Composition of essential oil and biological activity of extracts of Viola odorata L. from central Iran. Natural Product Research (Formerly Natural Product Letters) 2012;26(9):802–809. doi: 10.1080/14786419.2011.558013. [DOI] [PubMed] [Google Scholar]
- 354.Zarrabi M., Dalirfardouei R., Sepehrizade Z., Kermanshahi R. K. Comparison of the antimicrobial effects of semipurified cyclotides from Iranian Viola odorata against some of plant and human pathogenic bacteria. Journal of Applied Microbiology. 2013;115(2):367–375. doi: 10.1111/jam.12251. [DOI] [PubMed] [Google Scholar]
- 355.Siddiqi H. S., Mehmood M. H., Rehman N. U., Gilani A. H. Studies on the antihypertensive and antidyslipidemic activities of Viola odorata leaves extract. Lipids in Health and Disease. 2012;11(6):1–12. doi: 10.1186/1476-511X-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Barcelos F. F., Oliveira M. L., Giovaninni N. P. B., et al. Estudo químico e da atividade biológica cardiovascular do óleo essencial de folhas de Alpinia zerumbet (Pers.) B. L. Burtt & R. M. Sm. em ratos. Revista Brasileira de Plantas Medicinais. 2010;12(1):48–56. [Google Scholar]
- 357.Emiliano F. A. Dissertação. Departamento de Fisiopatologia Clinica e Experimental, Universidade Estadual do Rio de Janeiro; 2002. Efeito vasodilatador do extrato hidroalcóolico da Alpinia zerumbet (Pers.) Burtt e Smith no leito vascular mesentérico. [Google Scholar]
- 358.Chompoo J., Upadhyay A., Fukuta M., Tawata S. Effect of Alpinia zerumbet components on antioxidant and skin diseases-related enzymes. BMC Complementary and Alternative Medicine. 2012;12(106):1–9. doi: 10.1186/1472-6882-12-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Beal H. B. Dissertação. Centro de Ciências Agrárias; 2006. Atividade antioxidante e identificação dos ácidos fenólicos do gengibre (Zingiber officinale Roscoe) [Google Scholar]
- 360.Bhandari U., Kanojia R., Pillai K. K. Effect of ethanolic extract of Zingiber officinale on dyslipidaemia in diabetic rats. Journal of Ethnopharmacology. 2005;97(2):227–230. doi: 10.1016/j.jep.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 361.Akoachere J.-F. T. K., Ndip R. N., Chenwi E. B., Ndip L. M., Njock T. E., Anong D. N. Antibacterial effect of Zingiber officinale and Garcinia kola on respiratory tract pathogens. East African Medical Journal. 2002;79(11):588–592. doi: 10.4314/eamj.v79i11.8804. [DOI] [PubMed] [Google Scholar]
- 362.Kamtchouing P., Fandio G. Y. M., Dimo T., Jatsa H. B. Evaluation of androgenic activity of Zingiber officinale and Pentadiplandra brazzeana in male rats. Asian Journal of Andrology. 2002;4(4):299–301. [PubMed] [Google Scholar]
- 363.Sarris J. Herbal medicines in the treatment of psychiatric disorders: a systematic review. Phytotherapy Research. 2007;21(8):703–716. doi: 10.1002/ptr.2187. [DOI] [PubMed] [Google Scholar]
- 364.Sarris J., Panossian A., Schweitzer I., Stough C., Scholey A. Herbal medicine for depression, anxiety and insomnia: a review of psychopharmacology and clinical evidence. European Neuropsychopharmacology. 2011;21(12):841–860. doi: 10.1016/j.euroneuro.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 365.Anekonda T. S., Reddy P. H. Can herbs provide a new generation of drugs for treating Alzheimer's disease? Brain Research Reviews. 2005;50(2):361–376. doi: 10.1016/j.brainresrev.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 366.Dey A., Bhattacharya R., Mukherjee A., Pandey D. K. Natural products against Alzheimer's disease: Pharmaco-therapeutics and biothecnological interventions. Biothecnology Advances. 2017;35:178–216. doi: 10.1016/j.biotechadv.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 367.Mota W., Barros M., Cunha P., et al. Avaliação da inibição da acetilcolinesterase por extratos de plantas medicinais. Revista Brasileira de Plantas Medicinais. 2012;14(4):624–628. doi: 10.1590/S1516-05722012000400008. [DOI] [Google Scholar]
- 368.Carvalho R. B., Almeida A. A., Freitas R. M., et al. Composição química e atividade anticolinesterásica de uma fração ativa do extrato de folhas de Citrus limon (L.) Burm. Química Nova. 2013;36(9):1375–1379. doi: 10.1590/S0100-40422013000900017. [DOI] [Google Scholar]
- 369.Trevisan M. T. S., Macedo F. V. V., Meent M. V., Rhee I. K., Verpoorte R. Seleção de plantas com atividade anticolinasterase para tratamento da doença de Alzheimer. Química Nova. 2003;26(3):301–304. doi: 10.1590/s0100-40422003000300002. [DOI] [Google Scholar]
- 370.Rodrigues E., Gianfratti B., Tabach R., Negri G., Mendes F. R. Preliminary investigation of the central nervous system effects of 'Tira-capeta' (Removing the Devil), a cigarette used by some Quilombolas living in pantanal wetlands of Brazil. Phytotherapy Research. 2008;22(9):1248–1255. doi: 10.1002/ptr.2474. [DOI] [PubMed] [Google Scholar]
- 371.Giorgetti M., Negri G., Rodrigues E. Brazilian plants with possible action on the central nervous system-A study of historical sources from the 16th to 19th century. Journal of Ethnopharmacology. 2007;109(2):338–347. doi: 10.1016/j.jep.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 372.Otsuka R. D., Lago J. H. G., Rossi L., Galduróz J. C. F., Rodrigues E. Psychoactive plants described in a brazilian literary work and their chemical compounds. Central Nervous System Agents in Medicinal Chemistry. 2010;10(3):218–237. doi: 10.2174/1871524911006030218. [DOI] [PubMed] [Google Scholar]
- 373.Akhondzadeh S., Abbasi S. H. Herbal medicine In the treatment of Alzheimer’s disease. American Journal of Alzheimer’s Disease & Other Dementias. 2006;21(2):113–118. doi: 10.1177/153331750602100211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Barnes J. Cognitive Deficiency and dementia. The Pharmaceutical Journal. 2002;269:160–162. [Google Scholar]
- 375.Houghton P. J., Howes M.-J. Natural Products and Derivates affecting Neurotransmission relevant to Alzheimer's e Parkinson's disease. Neurosignals. 2005;14(1):6–22. doi: 10.1159/000085382. [DOI] [PubMed] [Google Scholar]
- 376.Ekor M. The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety. Frontiers in Pharmacology. 2014;4:1–10. doi: 10.3389/fphar.2013.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Veloso D. P., Guidini P., Comério R. M., Silva A. G. Plantas utilizadas em fitomedicamentos pra os distúrbios do sono. Natureza on Line. 2008;6(1):29–35. [Google Scholar]
- 378.Romanini C. V., Machado M. W., Biavatti M. W., Rúbia M. W. Avaliação da atividade ansiolítica e antidepressiva do extrato fluido e fraçao aquosa de folhas de Passiflora alata Curtis em camundongos. Acta Scientiarum Health Sciences. 2006;26(2):159–164. [Google Scholar]
- 379.Pasa M. C., Soares J. J., Guarim Neto G. Estudo etnobotânico na comunidade de Conceição-Açu (alto da bacia do rio Aricá Açu, MT, Brasil) Acta Botanica Brasilica. 2005;19(2):195–207. doi: 10.1590/S0102-33062005000200001. [DOI] [Google Scholar]
- 380.Vendrúscolo S. E. G. A., Mentz L. Levantamento etnobotânicodas plantas utilizadas como medicinais por moradores do bairro Ponta Grossa, Porto Alegre, Rio Grande do Sul, Brasil. Iheringia Série Botânica. 2006;61(1-2):83–103. [Google Scholar]
- 381.Silva C. S. P., Proença C. E. B. Uso e disponibilidade de recursos medicinais no município de Ouro Verde de Goiás, GO, Brasil. Acta Botanica Brasilica. 2008;22(2):481–492. [Google Scholar]
- 382.Leitão F., Da Fonseca-Kruel V. S., Silva I. M., Reinert F. Urban ethnobotany in Petrópolis and Nova Friburgo (Rio de Janeiro, Brazil) Revista Brasileira de Farmacognosia. 2009;19(1 B):333–342. doi: 10.1590/S0102-695X2009000200026. [DOI] [Google Scholar]
- 383.Amorozo M. C. Uso e diversidade de plantas medicinais em Santo Antonio do Leverger, MT, Brasil. Acta Botanica Brasilica. 2002;16(2):189–203. doi: 10.1590/S0102-33062002000200006. [DOI] [Google Scholar]
- 384.Pereira Z. V., Mussury R. M., de Almeida A. B., Sangalli A. Medicinal plants used by Ponta Porã community, Mato Grosso do Sul State. Acta Scientiarum - Biological Sciences. 2009;31(3):293–299. doi: 10.4025/actascibiolsci.v31i3.3206. [DOI] [Google Scholar]
- 385.Alves A. R., Silva M. J. The use of phytotherapy in the care of children up to 5 years of age in urban and suburban areas of São Paulo city-brazil. Revista da Escola de Enfermagem da USP. 2003;37(4):85–91. doi: 10.1590/S0080-62342003000400010. [DOI] [PubMed] [Google Scholar]
- 386.Ceolin T., Heck R. M., Barbieri R. L., Schwartz E., Muniz R. M., Pillon C. N. Plantas medicinais: transmissão do conhecimento nas famílias de agricultores de base ecológica no Sul do RS. Revista da Escola de Enfermagem da USP. 2011;45(1):47–54. doi: 10.1590/S0080-62342011000100007. [DOI] [PubMed] [Google Scholar]