Abstract
Introduction
Reusable endoscopes have some limitations regarding their continued use. To sort out these problems, several disposable devices have appeared on the market. Our objective is to show our clinical results with a new digital flexible single-use ureteroscope.
Materials and methods
This study presents a prospective series of patients who underwent endoscopic surgery as treatment for renal stones using the digital disposable endoscope Uscope 3022™. Demographic, procedure and stone information were registered including surgery time, stone-free rate, need of ureteral catheterization and complications, among others. The behavior of the ureteroscope in terms of image quality and problems associated with flexibility and the working channel were also registered.
Results
A total of 71 procedures were included in the analysis. The mean age was 49.9 years old, with 70.4% of male patients. Mean stone size was 11.4 mm (4 to 40 mm). The most frequent stone location was in the lower calyces (28.2%). The stone burden was high (>2 cm) in 8.4% of patients. The mean surgical time was 56.6 minutes (15–180 min). In 94.4% of the cases, a laser was used with dusting parameters. The global stone-free rate (SFR) was 95.2%, but in the subgroups analysis SFR were significantly superior in stones less than 10 mm (97.9%) versus stones between 10 and 20 mm (94.5%) and greater than 20 mm (78.3%) (p <0.01). The postoperative placement of double-J stents was required in 66.2% of patients. Two minor complications were recorded and they were related to the ureteral access sheath used. There were no problems regarding the performance of the ureteroscope.
Conclusions
The clinical data observed in this series does not differ from the results traditionally obtained with other reusable devices. To our knowledge, this series is the first worldwide report evaluating the clinical behavior and results in humans of the Uscope 3022.
Keywords: urolithiasis, ureteroscopy, retrograde intrarenal surgery
INTRODUCTION
The incidence of renal calculi is rising around the world [1, 2, 3]. The main purpose of urinary stone treatment is to provide the best possible stone-free rate (SFR) with the fewest associated morbidities, using a minimally invasive approach. As such, retrograde intrarenal surgery (RIRS) using a flexible ureteroscope (fURS) has become widely embraced and employed as a valid option for the first line treatment of upper urinary tract stones <2 mm [4, 5]. However, common problems associated with the use of flexible endoscopes include scope performance deterioration, costly repairs, and the need for dedicated sterilization equipment. To improve the performance of fURS, disposable devices have recently been developed. Polyscope™ is a removable, modular, and flexible ureteroscope that uses single optical fiber technology. Different studies have shown that a stable, clear image can be obtained with this endoscope, positioning it as a meaningful alternative for fURS [6, 7, 8]. The LithoVue™ (Boston Scientific, Marlborough, MA), introduced in 2015, is the first single-use digital disposable fURS [9]. Recent publications have confirmed its usefulness and competitiveness in comparison to other reusable devices [10, 11]. One of the main advantages of LithoVue™ over other endoscopes is the inclusion of a metal oxide semiconductor sensor (CMOS) located at the tip of the endoscope which provides a 0° direct view with a 85° field of vision. The Uscope UE3022 is a novel single-use digital disposable fURS developed by Pusen™ (Zhuhai Pusen Medical Technology Co, Ltd., Zhuhai, China). The goal of this study was to assess the clinical results obtained with the Uscope UE3022.
MATERIAL AND METHODS
This prospective cohort study was conducted at Clinica Santa María (tertiary reference center). Patients 18 years or older were included. All procedures were performed by the same urologist and all patients were admitted for endoscopic treatment of proximal ureteral or renal stone. The exclusion criteria were: known ureteral stricture, pregnancy, the presence of renal insufficiency, and active kidney infection. Upon recruitment, each patient provided written informed consent. As part of our regular database registry, we collected the following information for each patient: demographic parameters, stone characteristics, duration of surgery (total time from insertion of the endoscope to end of the procedure), duration of fluoroscopy (total time of irradiation, including double-J catheter placement, if necessary), SFRs, ureteral catheter use, and complications (according to the Clavien-Dindo classification). Scope failure (including loss of image quality), active deflection malfunction, and working channel problems were also registered.
All patients were preoperatively evaluated with a non-contrast computed tomography (CT) scan, urinalysis, and renal function. The surgery was performed under general anesthesia in the lithotomy position. As part of our routine practice, a nitinol safety guidewire (0.038 in) was used in all cases. The semirigid ureteroscope was then inserted using a second guidewire in order to achieve optic dilation of the distal ureter. If adequate dilatation was not achieved with this maneuver, a double-J catheter was installed and the definitive procedure was postponed for at least 10 days. The ureteral access sheath, 12 Fr (Bi-Flex™, Rocamed), was then placed and the fURS was advanced under fluoroscopic control. The entire kidney collecting system was visualized and evaluated before initiating the stone dusting with a 273 fiber. Depending on the case, the lower pole stones were moved to the upper poles for treatment using an N-Gage grasper™ (COOK Medical). At the end of the procedure a double-J stent (Inlay®, 26/6, BARD MEDICAL) was placed if clinically significant residual stone fragments were left. Patients were evaluated as outpatients at 15 days, 30 days, and 3 months post-procedure. Stone-free status was defined as the absence of fragment >2 mm at 3 months, observed with a non-contrast CT.
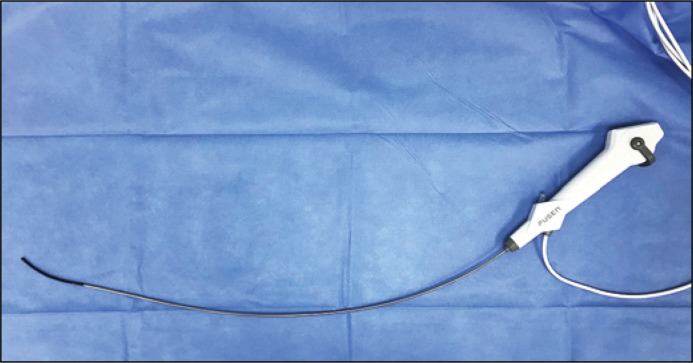
PUSEN Uscope 3022
The Uscope 3022 is a single-use, flexible digital ureteroscope with a design similar to that of other reusable devices (Figure 1). It has a plastic ergonomic handle and an integrated fixed camera that is connected using a cable to its own touchscreen monitor with CMOS digital imaging, or alternatively, to an operating room screen through DVI connection (Figure 2). Surgery photos and videos can be stored on the computer that comes incorporated into the endoscope monitor, and can be later transferred to an external disk through a USB port. The shaft of the Uscope 3022 is 9.5 Fr with a 3.6 Fr working channel, and the deflection mechanism can achieve 270° in both directions (Figure 3). The total length of the equipment is 63 cm, and it weighs 147 g.
Figure 1.
The USCOPE 3022 from PUSEN™.
Figure 2.
Touchscreen monitor with CMOS digital imaging.
Figure 3.
270º deflection mechanism.
Statistical analysis
Data was analyzed using Stata 12.0v software. After descriptive statistics analysis for the variables referred, categorical variables were compared using Fisher's exact test. T-tests were used to analyze continuous variables. Statistical significance was accepted as p <0.05.
RESULTS
Between March and August 2017, 71 procedures were performed. The study included 21 women (29.6%) and 50 men (70.4%), with a mean age of 49.9 years (range: 20–90 years) at the time of surgery. The mean stone size and density were 11.4 mm (CI: 4–40 mm) and 911.3 HU (CI: 350–1627 HU), respectively. This cohort of patients included 6 cases of stones >2 cm. Thirty-five patients (49.3%) had a ureteral stent placed before the surgery. Twelve stones were located in the proximal ureter, and all other stones were inside the kidney, including 20 cases of lower pole stones (Table 1). The laser was set to a 0.5 J, 15–20 Hz, and 800 s pulse for the dusting technique. In 21 cases, retrieval of the stone was done using a basket. The median durations of surgery and fluoroscopy were 56.6 min (CI: 15–180 min) and 69.9 s (CI: 10–300 s), respectively. The comparison of the lower pole subgroup versus the rest of the locations showed no significant difference in operating time (61.3 vs. 58.5 min, p = 0.6), radioscopy time (69.3 vs. 76.6 s, p = 0.5), or SFR (93.7 vs. 95.5%, p = 0.3). A double-J stent was left in place in 66.2% of cases (Table 2). The use of a prior double-J catheter significantly reduced the number of patients in whom a new pigtail was placed after the endoscopic surgery. All patients (100%) who did not have a previous catheter had one installed; only 32% of patients with a previous catheter ended up with a new catheter at the end of the surgery (p <0.001).
Table 1.
Patient demographic parameters and stone characteristics
| Parameter | Mean ±SD/ n | Range / % |
|---|---|---|
| Age at surgery (years) | 49.9 ±13.9 | 20–90 |
| Gender Female Male |
21 50 |
29.6% 70.4% |
| Total stone burden (mm in CT Scan) | 11.4 ±7.5 | 4–40 |
| Stone density (HU) | 911.3 ±253 | 350–1627 |
| Stone location Proximal ureter Renal pelvis Upper calyx Middle calyx Lower calyx Multiple location in the kidney |
12 11 6 16 20 6 |
16.9% 15.5% 8.5% 22.5% 28.2% 8.5% |
Table 2.
Intraoperative outcomes
| Parameter | Mean ±SD/ n | Range / % |
|---|---|---|
| Surgical time (minutes) | 56.6 ±38.0 | 15–180 |
| Fluoroscopy time (seconds) | 69.9 ±54.5 | 10–300 |
| Lithotriptor device Laser Basket only Access sheath use Postoperative double-J stent placement |
67 4 67 47 |
94.4% 5.6% 94.4% 66.2% |
A subset analysis comparing results between stones <10 mm, 10–20 mm, and >20 mm showed the poorest results in the last group. Whereas the SFR for the group of stones <10 mm was 97.8%, the SFR for the group of stones >20 mm was 78.3% (p >0.001). The same results were observed in the analysis of fluoroscopy time and surgical time, always in favor of the first group (Table 3). In terms of complications, two Clavien-Dindo class I lesions were observed, and one of them was attributed to the use of an access sheath and not directly related to the endoscope. The other complication was prolonged hematuria secondary to renal mucosal erosion, which required a prolonged hospital stay. In the group analyzed, there was no case of ureteroscope malfunction (image or deflection system).
Table 3.
Outcome subgroup analysis for stones <10 mm, 10–20 mm and >20 mm
| Parameter Mean ±SD/ n / % | <10 mm (n = 43) | 10–20 mm (n = 22) | >20 mm (n = 6) | p value |
|---|---|---|---|---|
| Stone free rate | 97.9 ±7.1 | 94.5 ±8.6 | 78.3 ±22.5 | <0.001 |
| Surgical time | 37.2 ±15.7 | 76.4 ±40.7 | 123.3 ±29.4 | <0.001 |
| Fluoroscopy time | 48.4 ±26.7 | 98.6 ±71.9 | 119.2 ±57.5 | <0.001 |
| Preoperative double-J stent placement | 23 (53.5%) | 10 (45.5%) | 2 (33.3%) | 0.584 |
| Postoperative double-J stent placement | 23 (53.5%) | 18 (81.8%) | 6 (100.0%) | 0.013 |
| Complications | 0 (0.0%) | 2 (9.1%) | 0 (0.0%) | 0.152 |
DISCUSSION
This is the first study to evaluate clinical results obtained using the Uscope 3022 from PUSEN™. We are facing a new era in the development of disposable flexible equipment with better image quality and adequate efficiency for intrarenal navigation. The reasons for this are the cost of reusable equipment and its maintenance, making them too expensive for some centers. In 2015, Del Santo et al. published an article showing that, in a French university hospital, the cost of using a fURS alone – excluding the cost associated with sterilization or high-level disinfection – was estimated to be €625 per patient [12]. Another recently published study analyzed the cost of reusable ureteroscopes over the course of 655 procedures and demonstrated that repairs are required after 21 procedures. The authors further demonstrated that the fURS was out of service for an average of 11 days per repair (range: 3–20 days), and that the average repair cost was $355 per flexible ureteroscopy performed [13]. Martin and coworkers reported in their cost-benefit analysis that in centers wherein fewer than 99 flexible ureteroscopies are performed per year, the use of disposable ureteroscopes would be justified [in this study the LithoVue and Flex-XCTM (Karl Storz, Tuttlingen, Germany)] digital fURS were compared] [14]. Since costs may vary by region, it is not possible to generalize the conclusion drawn in the previous report. For example, in the Chilean market, the Uscope 3022 is roughly 42% cheaper than the LithoVue ureteroscope, and certainly cheaper than reusable equipment, which can cost 32 times more than a disposable endoscope.
The results of RIRS depend on several factors related to the characteristics of the stones (size, composition/hardness, number, and location), renal anatomy, and surgeon experience. The 95% SFR achieved in this study is similar to that in previous reports. The Clinical Research Office of the Endourological Society (CROES) study showed prospectively collected data from more than 10,000 patients. The authors of this study found SFRs of 90% and 80% for stones <10 mm and <15 mm in size, respectively, after a single session of RIRS [15]. In another recent study, Goldberg et al. evaluated the appropriate limit for performing RIRS and found a 94.1% SFR for stones up to 10 mm. In the case of lower pole stones, the SFR did not decrease (93.7 vs. 95%), and was even slightly higher than rates reported in recent studies [16, 17]. A potential explanation for the high SFR obtained in lower pole stones could be that when using disposable equipment, the surgeon may be less concerned about damaging the device and therefore could maximally increase the deflection of the endoscope without fear of damaging the device.
All patients without a previous ureteral catheter had a double-J stent installed after the procedure. In comparison, only 32% of patients who had a prior catheter needed to have a new one installed. This finding is consistent with other studies; for patients with a prior catheter, is not necessary to place a new stent after surgery, given that they are a safer group on which to perform fURS [18, 19, 20].
Another interesting outcome that we measured was the X-ray exposure time required for intrarenal navigation. As this is a new device, it was unknown whether the fluoroscopic intraoperative time would be influenced. However, the average of 74.6 s of fluoroscopy per case in this group of patients does not differ from previously published ureteroscopy reports, and is certainly lower than percutaneous nephrolithotomy [21, 22].
The subset analysis showed a slightly higher SFR in stones >20 mm, compared to previous literature [23, 24, 25]. It is difficult to determine whether this result could be influenced by digital technology, which could deliver a better visualization in situations like this.
A limitation of this endoscope is the need to use a larger diameter access sheath, which is not always achieved in the first attempt. So, in some cases, passive dilatation – via installation of a double-J catheter – is required for at least 10 days. A second limitation may be the actual aptness of this new disposable endoscope to reach stones in unfavorable anatomical locations of the upper urinary tract − for example, in the treatment of calculi located in the lower pole with a steep infundibular pelvic angle, horseshoe kidneys, or calyceal diverticulum. A final weakness of this study is the lack of comparison with reusable equipment under similar conditions. However, the data shown here fill the gaps regarding the potential use of the Uscope 3022 and therefore can serve as a point of departure for future research with this device. Regarding the ureteroscope behavior, the first European experience with LithoVueTM showed a 5% (2 cases) rate of malfunction [26]. However, in our first 71 cases, no damage to the instrument (including loss of deflection or image quality, and working channel malfunction) was evident.
CONCLUSIONS
The clinical results obtained with the Uscope 3022 are similar to those published using reusable equipment. This new endoscope performs safely and efficiently in this group of patients treated for stones of the upper urinary tract. The routine worldwide incorporation of this technology is still a matter of debate, however, and its real potential and economic advantages remain unclear.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Scales Dr, Jr, Smith AC, Hanley JM, et al. Prevalence of Kidney stones in the United States. Eur Urol. 2012;62:160–165. doi: 10.1016/j.eururo.2012.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heers H, Turney BW. Trends in urological stone disease: a 5-year update of hospital episode statistics. BJU Int. 2016;118:785–789. doi: 10.1111/bju.13520. [DOI] [PubMed] [Google Scholar]
- 3.Shoag J, Tasian GE, Goldfarb DS, Eisner BH. The new epidemiology of nephrolithiasis. Adv Chronic Kidney Dis. 2015;22:273–278. doi: 10.1053/j.ackd.2015.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Zheng C, Xiong B, Wang H, et al. Retrograde intrarenal surgery versus percutaneous nephrolithotomy for treatment of renal stones >2 cm: a meta-analysis. Urol Int. 2014;93:417–724. doi: 10.1159/000363509. [DOI] [PubMed] [Google Scholar]
- 5.Giusti G, Proietti S, Luciani L, et al. Is retrograde intrarenal surgery for the treatment of renal stones with diameters exceeding 2 cm still a hazard? Can J Urol. 2014;21:7207–7212. [PubMed] [Google Scholar]
- 6.Gu SP, Huang YT, You ZY, et al. Clinical effectiveness of the PolyScope TM endoscope system combined with holmium laser lithotripsy in the treatment of upper urinary calculi with a diameter of less than 2 cm. Exp Ther Med. 2013;6:591–595. doi: 10.3892/etm.2013.1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bansal H, Swain S, Sharma GK, et al. Polyscope: a new era in flexible ureterorenoscopy. J Endourol. 2011;25:317–321. doi: 10.1089/end.2009.0584. [DOI] [PubMed] [Google Scholar]
- 8.Bander MJ, Gratzke C, Walther S, et al. The Polyscope: a modular design, semi disposable flexible ureterorenoscope system. J Endourol. 2010;24:1061–1066. doi: 10.1089/end.2010.0077. [DOI] [PubMed] [Google Scholar]
- 9.Buttice S, Sener TE, Netsch C, et al. LithoVue: A new single-use digital flexible ureteroscope. Cent European J Urol. 2016;69:302–305. doi: 10.5173/ceju.2016.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Usawachintachit M, Isaacson D, Taguchi K, et al. A Prospective Case Control Study Comparing LithoVueTM, a Single-Use Flexible Disposable Ureteroscope, to Flexible Reusable Fiber-Optic Ureteroscopes. J Endourol. 2017;31:468–475. doi: 10.1089/end.2017.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emiliani E, Traxer O. Single use and disposable flexible ureteroscopes. Curr Opin Urol. 2017;27:176–181. doi: 10.1097/MOU.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 12.Del Santo K, Audouin M, Ouzaid I, et al. Evaluation of the operating results and costs associated with the implementation of a flexibleureteroscopy activity within a university hospital center. Prog Urol. 2017;27:375–380. doi: 10.1016/j.purol.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Kramolowsky E, McDowell Z, Moore B, et al. Cost Analysis of Flexible Ureteroscope Repairs: Evaluation of 655 Procedures in a Community-Based Practice. J Endourol. 2016;30:254–256. doi: 10.1089/end.2015.0642. [DOI] [PubMed] [Google Scholar]
- 14.Martin CJ, McAdams SB, Abdul-Muhsin H, et al. The Economic Implications of a Reusable Flexible Digital Ureteroscope: A Cost-Benefit Analysis. J Urol. 2017;197:730–735. doi: 10.1016/j.juro.2016.09.085. [DOI] [PubMed] [Google Scholar]
- 15.Skolarikos A, Gross AJ, Krebs A, et al. Outcomes of flexible ureterorenoscopy for solitary renal stones in the CROES URS global study. J Urol. 2015;194:137–143. doi: 10.1016/j.juro.2015.01.112. [DOI] [PubMed] [Google Scholar]
- 16.Donaldson JF, Lardas M, Scrimgeour D, et al. Systematic review and meta-analysis of the clinical effectiveness of shock wave lithotripsy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower-pole renal stones. Eur Urol. 2015;67:612–616. doi: 10.1016/j.eururo.2014.09.054. [DOI] [PubMed] [Google Scholar]
- 17.Bozzini G, Verze P, Arcaniolo D, et al. A prospective randomized comparison among SWL, PCNL and RIRS for lower calyceal stones less than 2 cm: a multicenter experience: A better understanding on the treatment options for lower pole stones. World J Urol. 2017;35:1967–1975. doi: 10.1007/s00345-017-2084-7. [DOI] [PubMed] [Google Scholar]
- 18.Torricelli F, De S, Hinck S, et al. Flexible ureteroscopy with a ureteral access sheath: when to stent? Urology. 2014;83:278–281. doi: 10.1016/j.urology.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Chu L, Sternberg KM, Averch TD. Preoperative Stenting Decreases Operative Time and Reoperative Rates of Ureteroscopy. J Endourol. 2011;25:751–754. doi: 10.1089/end.2010.0400. [DOI] [PubMed] [Google Scholar]
- 20.Astroza G, Catalán M, Consigliere L, et al. Is a ureteral stent required after use of ureteral access sheath in presented patients who undergo flexible ureteroscopy? Cent European J Urol. 2017;70:88–92. doi: 10.5173/ceju.2016.919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ritter M, Krombach P, Martinschek A, et al. Radiation exposure during endoscopic procedures using over the table fluoroscopy sources. J Endourol. 2012;26:47–51. doi: 10.1089/end.2011.0333. [DOI] [PubMed] [Google Scholar]
- 22.Weld L, Nwoye UO, Knight R, et al. Fluoroscopy time during uncomplicated unilateral ureteroscopy for urolithiasis decreases with urology resident experience. World J Urol. 2015;33:119–124. doi: 10.1007/s00345-014-1264-y. [DOI] [PubMed] [Google Scholar]
- 23.Akman T, Binbay M, Ozgor F, et al. Comparison of percutaneous nephrolithotomy and retrograde flexible nephrolithotripsy for the management of 2-4 cms stones: a matched-pair analysis. BJU Int. 2012;109:1384–1389. doi: 10.1111/j.1464-410X.2011.10691.x. [DOI] [PubMed] [Google Scholar]
- 24.El-Anany FG, Hammouda HM, Maghraby HA, et al. Retrograde ureteropyeloscopic holmium laser lithotripsy for large renal calculi. BJU Int. 2001;88:850–853. doi: 10.1046/j.1464-4096.2001.01248.x. [DOI] [PubMed] [Google Scholar]
- 25.Breda A, Ogunyemi O, Leppert JT, Lam JS, Schulam PG. Flexible ureteroscopy and laser lithotripsy for single intrarenal stones 2 cm or greater - is this the new frontier. J Urol. 2008;179:981–984. doi: 10.1016/j.juro.2007.10.083. [DOI] [PubMed] [Google Scholar]
- 26.Doizi S, Kamphuis G, Giusti G, et al. First clinical evaluation of a new single use flexible ureterocope (Lithovue™): a European prospective multicentric feasibility study. World J Urol. 2017;35:809–818. doi: 10.1007/s00345-016-1936-x. [DOI] [PubMed] [Google Scholar]