Abstract
Introduction
The purpose of the present study was to clinically evaluate two new single-use Pusen ureteroscopes, one semirigid with a flexible tip (srURS) and one flexible (fURS).
Materials and methods
During ten consecutive procedures (five srURS and five fURS), we subjectively evaluated on a scale from 0 (poor) to 10 (excellent), the scope's deflection, image quality, and maneuverability prior to, during and after the surgery. Patient demographics, complications with the devices, and troubleshooting were recorded.
Results
There were a total of ten patients, five of which were female while the other five were male. Mean age was 58.9 years. Seven patients had a single kidney stone with mean size of 9.6 mm (1.6–20 mm). Half of the patients were pre-stented. For the fURS, the preoperative image quality rating was 8.4 (8–10), compared with 6.8 (4–9) during surgery. The preoperative deflection rating was 9.6+ 0.9 (8–10), while during surgery this decreased to 8.0 (6–10) and to 6.0 (4–8) when using a laser fiber. The srURS had a preoperative image quality rating of 9.2 (8–10), which decreased to 7.6 (6–9) while using the scope. The deflection rating decreased from 9.4 (7–10) preoperatively to 7.0 (1–10) postoperatively, and a similar reduction was observed in the maneuverability rating, from 9.6 (8–10) to 7.4 (1–10). Ureteroscopy was considered as a standard in four of the fURS and three of the srURS procedures. The mean overall satisfaction rating was 6.
Conclusions
The two new single-use ureteroscopes, one flexible and one semirigid, were considered to have allowed standard ureteroscopy in four and three out of the five procedures for each scope, respectively. The image quality, deflection, and maneuverability ratings decreased during the procedure for both scopes.
Keywords: ureteroscopy, urolithiasis, single-use ureteroscope, flexible ureteroscope, semirigid ureteroscope, Pusen
INTRODUCTION
Flexible ureterorenoscopy is a well-established procedure for stone management [1]. Technological advances in flexible ureteroscopes (fURS), such as reductions in the size of the scopes or introduction of digital vision, have made it possible to maintain good performance while improving surgical outcomes and lowering surgical times [2].
In recent years, single-use fURS have been developed to overcome some disadvantages of the reusable scopes. These include the purchase and repair costs of reusable devices and issues relating to sterility, including the risk that complete sterilization procedures will reduce the scope's lifespan [3].
Recently, the medical company Pusen (Zhuhai Pusheng Medical Technology Co., Ltd. China) has launched onto the market two single-use ureteroscopes: a fURS (the ‘Uscope’) and a semirigid scope with a flexible tip (srURS). The purpose of this study was to clinically evaluate the performance of these new devices (Figure 1). The operation room was set as shown on Figure 2.
Figure 1.
On top Pusen's flexible ureteroscope, below Pusen's semirigid ureterecoscope.
Figure 2.
Operation room settings for the use of both devices. Notice that the x-ray is placed on surgeon's left. While the screens and plug-ins are placed on the right.
MATERIAL AND METHODS
Ten single-use scopes were evaluated (five fURS and five srURS) in the prospective observational study. Patients were randomly selected from the department waiting list. The srURS was tested in adult patients with proximal ureteric stones and both the fURS and the srURS were tested in adults with kidney stones of <2 cm. Two surgeons subjectively evaluated the clinical performance of the scopes by using a checklist developed specifically for this test that allowed the evaluation of various parameters on a scale from 0 (poor) to 10 (excellent). The first surgeon performed 2 surgeries, the second surgeon performed 8 surgeries.
Prior to the surgery we evaluated the unboxing, image quality, deflection, and maneuverability (defining maneuverability as a synonym of torque, where the movement in the handle was transmitted and precisely reproduced at the tip of the scope). During surgery, image quality, deflection, and maneuverability with and without a basket and a laser fiber were assessed. Ease of passage of disposable instruments through the working channel was also tested. Laser settings for each procedure were recorded and stone samples were sent for analysis after each surgery. Complications were recorded with the ureteral lesion scale according to Traxer et al. [4], classifying ureteral wall damage in 4 grades being: 0 – no damage, 1 – mucosal flap without smooth muscular injury, 2 – mucosal and smooth muscular involved, 3 – ureteral perforation and 4 – total ureteral avulsion; and by the Clavien-Dindo classification system [5]. Troubleshooting with the devices was recorded. Abnormalities not included in our checklist, but encountered during surgery were documented. After surgery, image quality, deflection, and maneuverability were evaluated. Personal opinions from the surgeon and an overall evaluation of the device used were documented.
RESULTS
Ten procedures (five srURS and five fURS) were performed in ten consecutive patients (four right-sided and six left-sided). All patients underwent general anesthesia. The mean age was 58.9 +14.1 years (42–89). Half of the patients were male and half female. Half of the patients were pre-stented. Seven patients had a unique stone and three multiple stones. The mean size of the stones was 9.6 mm (1.6–20 mm) for the largest diameter and 7.2 mm (1.6–20 mm) for the smallest diameter (Table 1). There were neither intraoperative nor postoperative complications. One patient had ureteral mucosal damage (Grade 1) after using a ureteral access sheath. Both srURS and fURS had a working length of 630 mm and maximum deflection of 270º bilaterally. The outer diameter was 9F with a working cannel of 3.6F.
Table 1.
Demographics
| Variable | Result |
|---|---|
| n | 10 |
| Age (years) | 58.9 +14.1 (42–89) |
| Laterality Right Left |
40% 60% |
| Surgeon 1 2 |
20% 80% |
| Device fURS srURS |
5 5 |
| Catheterization prior to surgery (2J) | 50% |
| Stone features Longer diameter Shorter diameter Unique Multiple |
9.6 mm ±4.7 (1.6–20) 7.2 mm +5.2 (1.6–20) 70% 30% |
| Lithiasis site Superior calix Medium calix Inferior calix Pelvis Proximal urether |
1 2 3 3 2 |
Flexible ureteroscope
The preoperative image quality rating was 8.4 (8-10), compared with 6.8 (4–9) during surgery. The preoperative ratings for deflection and maneuverability were 9.6 (8–10) and 9.2 (7–10), respectively. The deflection rating decreased somewhat to 8.0 (6–10) during surgery; while it was maintained when using a basket 9.5 (9–10), it was markedly reduced when using a laser fiber 6.0 (4–8). A high score (8–10) was recorded for irrigation in all evaluations. All five surgeries with the fURS were completed with the same disposable scope as was used from the outset. Results are summarized in Table 2.
Table 2.
Ratings with the flexible ureteroscopes before, during, and after surgery
| Scale | Before | During | After |
|---|---|---|---|
| Vision | 8.4 ±0.5 (8–10) | 6.8 ±1.8 (4–9) | 7.0 ±2.1 (4–10) |
| Deflection | 9.6 ±0.9 (8–10) | 8.0 ±1.6 (6–10) | 8.4±1.1 (7–10) |
| Deflection laser | 6.0 ±2.3 (4–8) | ||
| Deflection basket | 9.5 ±0.7 (9–10) | ||
| Maneuverability | 9.2 ±1.3 (7–10) | 7.2 ±2.2 (4–10) | 8.4 ±0.5 (8–9) |
| Maneuverability with laser | 7.3 ±1.5 (6–9) | ||
| Maneuverability with basket | 7.0 ±4.2 (4–10) | ||
| Irrigation | 9.6 ±0.9 (8–10) | 9.4 ±0.9 (8–10) | 9.6 ±0.9 (8–10) |
Semirigid ureteroscope
The preoperative image quality rating of 9.2 (8–10) decreased to 7.6 (6–9) while using the scope, although there was a small improvement in the rating after surgery, to 8.4 (8–9). Deflection and maneuverability decreased progressively from the preoperative ratings of 9.4 (7–10) and 9.6 (8–10), respectively, to the postoperative ratings of 7 (1–10) and 7.4 (1–10), respectively. Lower ratings during surgery, compared with before surgery, were seen with the use of a basket and the laser fiber. Three out of five interventions with the srURS were completed with the same disposable scope as was used from the outset. Results are summarized in Table 3.
Table 3.
Ratings with the semirigid ureteroscopes before, during, and after surgery
| Scale | Before | During | After |
|---|---|---|---|
| Vision | 9.2 ±1.1 (8–10) | 7.6 ±1.1 (6–9) | 8.4 ±0.5 (8–9) |
| Deflection | 9.4 ±1.3 (7–10) | 8.5 ±1.3 (7–10) | 7.0 ±3.7 (1–10) |
| Deflection laser | 8.5 ±0.7 (8–9) | ||
| Deflection basket | 8.7 ±0.6 (8–9) | ||
| Maneuverability | 9.6 ±0.9 (8–10) | 8.8 ±1.0 (8–10) | 7.4 ±3.7 (1–10) |
| Maneuverability with laser | 9.0 ±1.4 (8–10) | ||
| Maneuverability with basket | 8.3 ±0.6 (8–9) | ||
| Irrigation | 10 | 8.6 ±0.5 (8–9) | 8.0 ±3.9 (1–10) |
Overall evaluation
Two of the surgeries with the srURS had to be completed with reusable scopes, and all five cases with fURS were finished with the same scope. The ureteroscopy was considered standard, as described by Giusti [6], in four of the fURS and three of the srURS procedures. The mean overall satisfaction rating was 6. In regards to scope quality, one fURS leaked from the handle–shaft junction.
DISCUSSION
Single-use ureteroscopes have been developed to improve unfavorable features of reusable ureteroscopes. The cost of the purchase and repair of reusable flexible ureteroscopes can restrict the performance of ureteroscopy in some centers; this is especially true in low-volume centers, where using single-use may be cost beneficial [7]. Pusen's fURS device costs may be approximately $600 U.S. The price of a reusable digital device could reach $25,000 [8]. The average repair cost of has been estimated to be $325 [9]. Accounting only for the purchase cost of the reusable device, 41 surgical procedures could be performed with a Pusen single use fURS for the price of a reusable fURS. Sterilization has also become a matter of debate as the process can damage the ureteroscope, and some centers consequently use highly decontaminated, but not sterile scopes [10, 11]. Single-use ureteroscopes also have the advantage of being immediately available, and the surgeon gets a brand new device for each procedure.
Some disposable scopes already on the market have been studied. The initial Polyscope (Lumenis, Israel; Polydiagnost, Germany), a catheter-like scope, at first showed good results, but was subsequently abandoned [12]. To date, the LithoVue (Boston Scientific, Massachusetts, USA) is the only disposable fURS to have been well studied [13]. It demonstrated a comparable performance (in terms of access, digital imaging, maneuverability, and deflection) to digital and fiber optic reusable fURS in cadaveric, in vitro, and swine models [14, 15, 16]. Also a prospective clinical study in 40 patients showed an overall performance satisfaction rating of ‘very good’ in 70% of cases, ‘good’ in 17.5%, and ‘acceptable’ in 12.5% [17]. In a study by Marchini [18], they evaluated in vitro different types of single use fURS. They described Pusen as superior in terms of weight and water flow without instruments in place; however, when assessing optical resolution, field of view, deflection capacity and irrigation flow with instrument in place LithoVue outperformed the rest of the devices.
It is of paramount importance that other, newer disposable scopes on the market are properly evaluated since high quality and outcomes as good as those achieved with reusable scopes should be minimum requirements.
In the present study, both scopes had some features, such as the plug and play system and easy opening of the instruments, which made preparation of the surgical table simple. The irrigation systems used with a manual pump were found to be of good quality during the whole procedure. The radio-opacity of the scopes also had a good rating.
Flexible ureteroscope
The handle is ergonomic and similar to that of regular ureteroscopes. The 9-Fr shaft allows the scope to fit correctly into 10.7/12.7 ureteral access sheath (UAS). The insertion in the UAS was rated (8–10). The single-site working channel was placed as in regular scopes, making it easy to plug port seals or manual pumps.
The digital vision was provided by a CMOS system. The image quality was initially good. During the procedure this quality was maintained with respect to the urothelial walls, which were close to the scope, but structures farther away were not clearly defined, with the bladder and renal pelvis appearing dim. A similar effect was seen when using a basket and approaching a stone; moreover, when using the laser dim spots appeared in the corners of the image. A better lighting source could be helpful. When using the laser, image interference was only seen when a high energy (>1.5 J per pulse) was used and this was not disruptive.
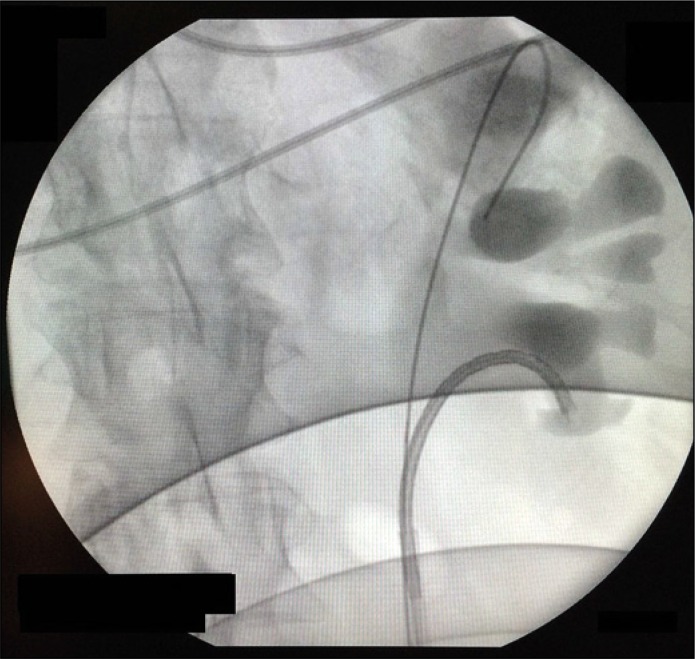
The deflection was adequate before the procedure. As reported above, it decreased in quality over time as the deflection was not exactly reproduced at the tip. However, deflection of the device permitted to reach most of intrarenal locations (Figure 3). In one case the scope had to be straightened every time an instrument was inserted, including the ball tip fiber.
Figure 3.
Deflection of the flexible ureteroscopes allowed the surgeon to work in the inferior calix. Scope visibility of the device was good.
Semirigid ureteroscope
The handle has a joystick-like deflection device that we found to be adequate after becoming accustomed to it. The working channel does not have a seal port, and some leakage could be seen. Also the surgeon had to control the laser fiber with one hand to make it stable.
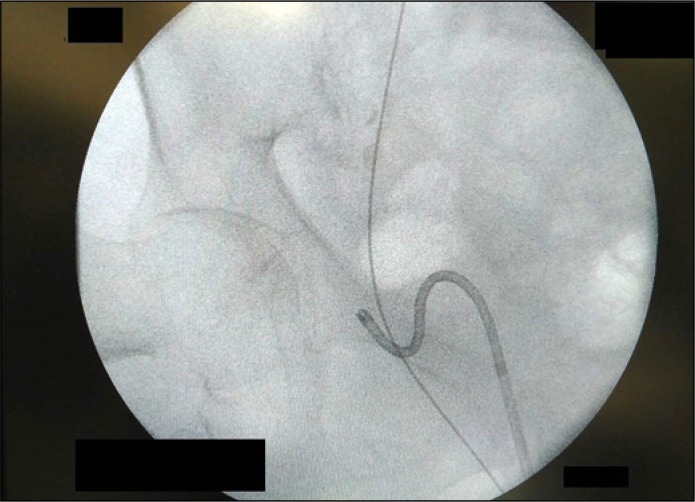
Insertion of the scope through the ureteral meatus and distal ureter was performed as with any other flexible ureteroscope. Unfortunately, however, two of the surgeries with the srURS had to be completed with reusable scopes. In these two cases we found it difficult to progress to the mid-ureter (in one case the scope broke at the semirigid–flexible junction) as the flexible tip bent, losing strength (Figure 4). This is the reason why the postoperative ratings regarding deflection and maneuverability decreased significantly. On this basis we suggest that the srURS should be used in conjunction with a small 10/12 UAS.
Figure 4.
Flexible tip of the semirigid ureteroscope bent at distal ureter before passing through the iliac constriction.
The digital vision was provided by a complementary metal-oxide semiconductor (CMOS) system. Regarding the light system, the urothelial walls close to the scope were well viewed, but structures farther away were not clearly defined, with the bladder and renal pelvis appearing dim. The subjective evaluation showed the same experience with the light source as with the fURS. The srURS did, however, have better image quality ratings during surgery than the fURS 7.6 (6–9) vs. 6.8 (4–9) respectively, and showed greater improvement in the postoperative rating. The reduction in image quality during surgery with the srURS could be explained by the dim intrarenal vision and the impact of some small amounts of bleeding.
Introduction of instruments into the working channel was found to be difficult. We consequently suggest use of a guidewire introducer to facilitate insertion or removal of the black cap (although this results in leaking).
Overall evaluation
As mentioned above, the ureteroscopy was considered as standard in four fURS and three srURS (i.e., seven of ten procedures), and the mean overall satisfaction rating was 6. The dim light source, the two srURS that failed during insertion, and the one fURS that leaked from the handle–shaft junction were the cases with lower ratings.
Limitations of our study are the low volume of patients, with only 10 cases, and having only 2 surgeons to perform the surgeries, with one surgeon performing 2 surgeries. Also the evaluation of the devices was mostly subjective according to each surgeon’s experience.
Overall, the results led us to consider that the quality of the device and the achievement of a comparable image quality are paramount if single-use scopes are to be accepted as replacements for the existing reusable instruments. For the time being, the Pusen scopes may be considered suitable for simple cases. The study was intended to evaluate the devices themselves, while more studies are necessary to determine clinical outcomes.
CONCLUSIONS
The two new single-use ureteroscopes, one flexible and one semirigid, were considered to have allowed standard ureteroscopy in four and three out of five procedures for each scope, respectively. The preoperative rates regarding image quality, deflection, and maneuverability (all >8 of 10) decreased during the procedure for both scopes.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Türk C, Petřík A, Sarica K, et al. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 2.Somani BK, Al-Qahtani SM, de Medina SD, Traxer O. Outcomes of flexible ureterorenoscopy andlaser fragmentation for renal stones: comparison between digital and conventional ureteroscope. Urology. 2013;82:1017–1019. doi: 10.1016/j.urology.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Emiliani E, Traxer O. Single use and disposable flexible ureteroscopes. Curr Opin Urol. 2017;27:176–181. doi: 10.1097/MOU.0000000000000371. [DOI] [PubMed] [Google Scholar]
- 4.Traxer O, Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol. 2013;189:580–584. doi: 10.1016/j.juro.2012.08.197. [DOI] [PubMed] [Google Scholar]
- 5.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:20–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giusti G, Proietti S, Villa L, et al. Current Standard Technique for Modern Flexible Ureteroscopy: Tips and Tricks. Eur Urol. 2016;70:188–194. doi: 10.1016/j.eururo.2016.03.035. [DOI] [PubMed] [Google Scholar]
- 7.Martin CJ, McAdams SB, Abdul-Muhsin H, et al. The economic implications of a reusable flexible digital ureteroscope: a cost-benefit analysis. J Urol. 2017;197:730–735. doi: 10.1016/j.juro.2016.09.085. [DOI] [PubMed] [Google Scholar]
- 8.Gridley CM, Knudsen BE. Digital ureteroscopes: technology update. Res Rep Urol. 2017;9:19–25. doi: 10.2147/RRU.S104229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kramolowsky E, McDowell Z, Moore B, et al. Cost Analysis of Flexible Ureteroscope Repairs: Evaluation of 655 Procedures in a Community-Based Practice. 2016;30:254–256. doi: 10.1089/end.2015.0642. [DOI] [PubMed] [Google Scholar]
- 10.Ofstead CL, Heymann OL, Quick MR, Johnson EA, Eiland JE, Wetzler HP. The effectiveness of sterilization for flexible ureteroscopes: A real-world study. Am J Infect Control. 2017;45:888–895. doi: 10.1016/j.ajic.2017.03.016. [DOI] [PubMed] [Google Scholar]
- 11.Rutala WA, Weber DJ. Reprocessing semicritical items: Current issues and new technologies. Am J Infect Control. 2016;44:e53–62. doi: 10.1016/j.ajic.2015.12.029. [DOI] [PubMed] [Google Scholar]
- 12.Bader MJ, Gratzke C, Walther S, et al. The PolyScope: a modular design, semidisposable flexible ureterorenoscope system. J Endourol. 2010;24:1061–1066. doi: 10.1089/end.2010.0077. [DOI] [PubMed] [Google Scholar]
- 13.Butticè S, Sener TE, Netsch C, Emiliani E, Pappalardo R, Magno C. LithoVue™: A new single-use digital flexible ureteroscope. Cent European J Urol. 2016;69:302–305. doi: 10.5173/ceju.2016.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Proietti S, Dragos L, Molina W, Doizi S, Giusti G, Traxer O. Comparison of new single-use digital flexible ureteroscope versus nondisposable fiber optic and digital ureteroscope in a cadaveric model. J Endourol. 2016;30:655–659. doi: 10.1089/end.2016.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiseman O, Keeley F, Traxer O, Preminger G. A single-use disposable digital flexible ureteroscope (LithovueTM) compared to a nondisposable fibre-optic flexible ureteroscope in a live porcine model. Eur Urol Suppl. 2016;15:eV76. [Google Scholar]
- 16.Baghdadi M, Emiliani E, Talso M, et al. Comparison of laser fiber passage in ureteroscopic maximum deflection and their influence on deflection and irrigation: Do we really need the ball tip concept? World J Urol. 2017;35:313–318. doi: 10.1007/s00345-016-1873-8. [DOI] [PubMed] [Google Scholar]
- 17.Doizi S, Kamphuis G, Giusti G, et al. First clinical evaluation of a new single-use flexible ureteroscope (LithoVue™): a European prospective multicentric feasibility study. World J Urol. 2017;35:809–818. doi: 10.1007/s00345-016-1936-x. [DOI] [PubMed] [Google Scholar]
- 18.Marchini GS, Batagello CA, Monga M, et al. In Vitro evaluation of single-use digital flexible ureteroscopes: a practical comparison for a patient-centered approach. J Endourol. 2018;32:184–191. doi: 10.1089/end.2017.0785. [DOI] [PubMed] [Google Scholar]