Abstract
Background
Particulate matter<2.5μm in diameter (PM2.5) and heat are strong predictors of morbidity, yet few studies have examined the effects of long-term exposures on non-fatal events, or assessed the short and long-term effect on health simultaneously.
Objective
We jointly investigated the association of short and long-term exposures to PM2.5 and temperature with hospital admissions, and explored the modification of the associations with the short-term exposures by one another and by temperature variability.
Methods
Daily ZIP code counts of respiratory, cardiac and stroke admissions of adults ≥65 (N=2,015,660) were constructed across New-England (2001-2011). Daily PM2.5 and temperature exposure estimates were obtained from satellite-based spatio-temporally resolved models. For each admission cause, a Poisson regression was fit on short and long-term exposures, with a random intercept for ZIP code. Modifications of the short-term effects were tested by adding interaction terms with temperature, PM2.5 and temperature variability.
Results
Associations between short and long-term exposures were observed for all of the outcomes, with stronger effects of long-term exposures to PM2.5. For respiratory admissions, the short-term PM2.5 effect (percent increase per IQR) was larger on warmer days (1.12% versus −0.53%) and in months of higher temperature variability (1.63% versus −0.45%). The short-term temperature effect was higher in months of higher temperature variability as well. For cardiac admissions, the PM2.5 effect was larger on colder days (0.56% versus −0.30%) and in months of higher temperature variability (0.99% versus −0.56%).
Conclusions
We observed synergistic effects of short-term exposures to PM2.5, temperature and temperature variability. Long-term exposures to PM2.5 were associated with larger effects compared to short-term exposures.
Keywords: particulate matter, temperature, hospitalizations, respiratory, cardiac
Graphical abstract
1. INTRODUCTION
Particulate matter air pollution and heat are strong predictors of cardiovascular (1–9) and respiratory (2, 8, 10, 11) morbidity and mortality. It is, therefore, important to correctly identify their joint effect on health outcomes, especially in light of the ongoing process of climate change (12, 13). In most studies that assessed the effects of temperature and particulate matter smaller than 2.5μm in diameter (PM2.5) on health, temperature was treated as a confounder rather than a modifier (13). Those that did assess modification by temperature mostly focused on the estimation of short-term PM effects with stratification by temperature or season. Very little evidence is currently available on synergism (that is, on the joint effects of temperature, temperature variability and air pollution) (14). In addition, examination of the health effects of temperature has been almost exclusively focused on short-term exposures (days to a few weeks). However, recent studies of mortality cohorts have indicated that there are chronic effects of longer-term temperature exposure, and that temperature variability is a key predictor of health (15–19). Such exposures have not, to our knowledge, been studied for hospital admissions for acute events.
The underlying mechanism explaining the interaction between temperature and PM may be related to different exposure patterns to PM across the range of temperature (i.e. different PM composition in warmer and colder temperatures) (20) or to physiological stress that may increase susceptibility (21). Regarding temperature variability, there is strong evidence of adaptation to usual temperatures (22), and because the effect of climate change is seen both in the increases of the average values and the variability of temperature (23), it is important to investigate the health impacts of unstable weather and its interaction with PM.
The majority of studies that examined the interaction between temperature and PM focused on mortality (13, 18, 20, 21, 24–33). The evidence regarding hospital admissions, emergency room visits or other measures of morbidity are scarce, and the direction of the interaction varies by the outcome tested and the geographic location. A study by Pan et al assessed the modification of the association between temperature and measures of cerebrovascular hemodynamics, by PM2.5. The authors found significantly weaker effects of temperature on resting blood flow velocity at higher PM2.5 concentrations (34). A recent study has found an increased risk of stroke associated with PM2.5 on the day of the event, with stronger associations on warmer days (35). A study in New York, which included hospital admissions due to cardiovascular diseases, found stronger associations with PM2.5 in the winter and in low temperatures (36). For respiratory admissions, a study of 204 US urban counties found stronger effects of PM2.5 in warmer regions (37). Another study, however, found stronger short-term PM2.5 effects in the winter (10).
Another gap is that most previous research examined either acute or chronic exposure rather than investigating the effect of both exposures simultaneously (14). Examining the simultaneous effect of both exposures will provide the effect of each exposure independently from the other. Kloog and colleagues addressed this in a series of studies, where they investigated both acute and chronic effect of air pollution on several health outcomes and found increases of short and long-term exposure to PM2.5 to be associated with increases in cardiovascular, respiratory and stroke admissions rate (2, 32, 38), but further examination of the potential interactions of these effects is clearly needed.
In this study, we aim to investigate the association between short and long-term exposures to PM2.5 and temperature simultaneously, with cardiac, stroke and respiratory hospital admissions, while using spatio-temporally resolved satellite based exposure models (39, 40). In addition, we aim to explore the modification of the associations with the short-term exposures by one another and by temperature variability, which may limit physiological adaptation to temperature.
2. METHODS
2.1. Study population and main outcomes
This study was approved by the Harvard School of Public Health Institutional Review Board. The study population comprised New England residents between the years 2000 and 2011, 65 years or older, who were Medicare beneficiaries and enrolled in the fee-for-service program. For each eligible subject, individual-level data on gender, age, race, country of residence, Medicaid eligibility, dates of hospital admissions, the International Classification and Disease, Ninth Revision (ICD 9) code for the primary cause of hospitalization and the date of death were extracted. Cases were defined as emergency admissions with a principal discharge code of all respiratory diseases (ICD 9: 460-519), all cardiac diseases (ICD 9: 390-429) or ischemic stroke (ICD 9: 432-435). From this data, we constructed daily counts of the number of hospital admissions for each admission cause and each zip code.
2.2. Exposure
Temperature data
Temperature data were obtained from a spatiotemporally resolved prediction model generating predictions of daily average temperatures at a 1×1 KM spatial resolution, described previously in detail (40). In brief, daily MODIS (Moderate resolution imaging spectroradiometer) land surface temperatures (LST) data, in grid cells where both air temperature and LST were available for that day, were calibrated using mixed effect models. The model covariates included LST, land use regression (LUR) variables (percent urban, elevation, normalized difference vegetation index) and a random intercept and slope for surface temperature for each day. Information from neighboring grid cells was used to estimate air temperature when no surface temperature data are available. Out-of-sample ten-fold cross-validation was used to quantify the accuracy of the model predictions, showing excellent model performance for both days with available satellite data (mean out-of-sample R2 = 0.947) and days without satellite observations (mean out-of-sample R2 = 0.940). For more in depth information refer to Kloog et al (2014) (40).
PM2.5 data
PM2.5 data were obtained from a hybrid satellite based model incorporating daily satellite remote sensing data and classic LUR methodologies at 1×1 km spatial resolution. In brief, in days where both monitor PM data and Aerosol Optic Depth (AOD) values were co-located, mean daily PM2.5 concentrations in each grid cell were estimated by calibrating the AOD-PM relationship using mixed effect models with a random slope for day and nested regions, in addition to the spatial and temporal predictors such as in a classic LUR. Then, a second model was built to estimate exposures on days when AOD measures were not available using calibration fits. The model used the regional mean of PM2.5 monitoring stations, with a smooth function of latitude and longitude and a random intercept for each cell that takes advantage of associations between grid cell AOD values and PM data from monitors located elsewhere, and associations with available AOD values in neighboring grid cells. Again, Out-of-sample “ten-fold” cross-validation was used to quantify the accuracy of the model predictions, showing excellent model performance for both days with available satellite data (mean out-of-sample R2 = 0.88) and days without satellite observations (mean out-of-sample R2 = 0.87). For more in depth description please refer to Kloog et al (2014) (39).
The exposure values of all grid cells located within each of the 1823 ZIP codes and their 500 meters buffer surrounding, were averaged daily and exposure data was assigned to ZIP codes using ArcGIS based on spatial location and date.
2.3. Covariates
The following ZIP code level socioeconomic variables were obtained through the U.S. Census Bureau from the US Census 2000 and the American Community Survey (ACS) 5-year estimates of 2009–2013: median household income, percent black, percent Hispanic, percent living in poverty and percent of residents with no high school education. Using both Census and ACS data we applied a linear interpolation obtaining yearly values for each variable.
2.4. Statistical methods
Associations between cause-specific admissions and short and long-term exposure to PM2.5 and temperature were assessed using Poisson regression with proportional hazard model with a piecewise constant hazard for each day (41) and a random intercept for each ZIP code. This model combines the classic Poisson time series analysis with proportional hazard model where the hazard is allowed to vary each time period, allowing its estimation using a Poisson regression. This allows the simultaneous assessment of the associations with both short and long-term exposures. Each time interval in the model has a separate hazard, allowing the baseline hazard to vary with time, and an offset representing the person-time at risk in that ZIP code. Since the time intervals are small, the time-interval intercepts approaches a smooth function of time, and therefore can be replaced with a smooth function of time incorporated in the Poisson model (2).
Previous work done by our team found stronger associations with PM2.5 measured over the current and previous day of hospitalization, compared to same day exposure (2). We, therefore, used the moving average of PM2.5 at lag days 0-1 for the calculation of the short-term exposure to PM2.5. For temperature, previous studies found stronger effects of colder temperatures at lag 1-5 (42) and of warmer temperatures at lag 0 (43), we therefore a priori defined three potential exposure windows (lag 0, lag 0-1 and lag 1-5) and tested the associations with each. Moreover, the association with temperature is commonly nonlinear. To assess the linearity of the associations with the four main exposures, we regressed the cause specific admissions rate against the aforementioned exposures using penalized splines. Then, we compared the Akaike’s and Bayesian information criteria between the models to assess the best fit.
To ensure that the short-term effect estimates only capture short-term variation within ZIP code and not spatial differences between ZIP code, the short-term exposures were defined as the difference between the defined exposure window and the average ZIP code exposure across the entire study period. This also assures that the short-term effects cannot be confounded by spatially varying population characteristics. Long-term exposure was defined as the annual average of exposures (2). To capture temperature variability, we computed the monthly standard deviation of daily temperatures, separately for each ZIP code.
All models were built off of a base model, which included the short and long-term exposures to PM2.5 and temperature, with adjustment for a smoothed function of time (using natural cubic splines with 5 degrees of freedom per year)(2), day of the week, and ZIP code level socioeconomic variables (age, percent minorities, median household income, percent poverty and percent people with no high school education). We then fit a series of separate models, which each added additional terms to the base model as follows: (1) base model plus interaction terms between the two short-term exposures, (2) base model plus interaction terms between short-term exposure to PM2.5 and the measure of temperature variability, and (3) base model plus interaction terms between short-term temperature and the measure of temperature variability. Since the variation in the long-term exposures is smaller, a longer follow-up period was needed to examine interactions of long-term exposures. Because of the limited number of years of follow-up in our study (10 years), we did not examine these interactions in our analysis.
Results are presented as percent change for inter-quartile range (IQR) increase of the exposures. The effect of the long-term exposure to temperature was modeled using penalized splines, we therefore computed the percent change in admissions rate per IQR increase (and 95% Confidence Intervals (CI)) in the 10th (8 °C) and 90th (12 °C) percentile of temperature.
For the effect modification analysis, the results are presented as percent change in cause-specific admissions for an IQR increase in the exposure at the 10th and 90th percentile of the distribution of the modifier.
3. RESULTS
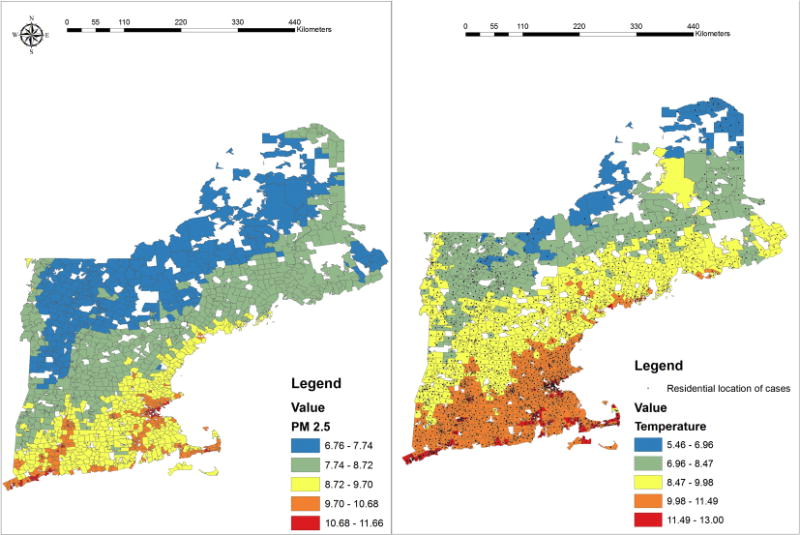
Descriptive statistics of the 2,015,660 admissions included in the study are presented in Table 1. The patient population was about 80 years old on average, 44.6% were males and the majority was white. Table 2 shows the summary statistics of short and long-term exposures to PM2.5 and temperature across the study area. The two-day average concentration of PM2.5 was 8.92μg/m3 on average (IQR = 5.65-11.05), and the two-day temperature average was 9.94 °C (IQR = 7.62-12.83). Supplementary Figure 1 shows the mean annual PM2.5 and temperature predictions generated by our models averaged within ZIP codes. For PM2.5, the mean annual concentrations in the study period ranged between 6.7 and 11.6 μg/m3, with higher values in urban areas. Hence, any association is entirely below the current National Ambient Air Quality Standard for PM2.5. The average temperature ranged between 5.5 and 13.0 °C. The standard deviation of monthly temperature ranged between 0.15 and 7.9 °C with the highest variability observed between December-January and lowest variability observed between July-September. The correlation between the exposures was low to moderate with the highest correlation observed between long-term exposures to temperature and PM2.5 (r=0.46, p<0.001).
Table 1.
Population characteristics
| Population characteristics | All respiratory (n=750,694) | All cardiac (n=1,053,731) | Ischemic stroke (n=211,235) |
|---|---|---|---|
| Male gender, %(n) | 44.50 (334,056) | 45.28 (477,170) | 41.40 (87,445) |
| Race, %(n) | |||
| White | 94.33 (708,106) | 94.35 (994,171) | 93.58 (197,677) |
| Black | 2.96 (22,196) | 3.13 (32,979) | 3.70 (7,806) |
| Other | 2.71 (20,392) | 2.52 (26,581) | 2.72 (5,752) |
| Age, Mean ± SD | 79.99±8.12 | 79.85±8.03 | 80.77±7.84 |
Table 2.
Summary statistics for hospitalization day, 2-day average and annual moving average of exposure to PM2.5 and temperature
| Exposure | Mean | SD | IQR |
|---|---|---|---|
| PM2.5 | |||
| Lag 0 | 8.92 | 5.38 | 5.22;11.31 |
| Lag 0-1 MA | 8.92 | 4.76 | 5.65;11.05 |
| Annual average | 8.92 | 1.63 | 7.82;10.08 |
| Temperature | |||
| Lag 0 | 9.94 | 6.17 | 5.63;14.80 |
| Lag 0-1 MA | 9.94 | 4.45 | 7.62;12.83 |
| Annual average | 9.94 | 1.55 | 8.88;11.13 |
MA=moving average; IQR=inter-quartile range; SD=standard deviation
Of the exposure windows tested, the average temperature at the same day yielded the best fit based on the Akaike’s and Bayesian information criteria. We therefore used the same day exposure for the calculation of the short-term exposure to temperature. As seen in supplementary figure 2, showing the associations between the smoothed functions of short and long-term exposures to temperature and hospital admissions, the association with short-term exposure to temperature was close to linear throughout most of the exposure distribution, with a slight curve only in the 98th percentile of short-term temperature (10 °C). For long-term exposure however, the dose-response curves for all three outcomes were nonlinear. We therefore treated the association with short-term exposure to temperature as linear and used penalized splines for the long-term exposure.
Table 3 presents the associations between short and long-term exposures to PM2.5 and temperature and each cause of admission estimated from the base model. Short-term exposure to temperature was associated with an 8.63% (95% CI: 7.88; 9.39) increase in respiratory admissions rate and 3.63% (95% CI: 3.01; 4.25) increase in cardiac admissions rate for an IQR (9.2 °C) increase in temperature, but not with stroke. Increases of long-term temperature in the 10th percentile were associated with higher admissions rate per IQR increase (2.2 °C), compared to the 90th percentile, for respiratory (6.24% and 1.37%, respectively), cardiac (−2.15% and −1.69%, respectively) and stroke (7.32% and 0.15%, respectively) admissions.
Table 3.
The association between short and long-term exposure to PM2.5 and temperature and cause specific admissions
| Cause | Exposure | Percent change (95% CI) |
|---|---|---|
| Respiratory | PM2.5 short term | 0.41% (0.16%; 0.65%)** |
| PM2.5, long term | 4.09% (3.31%; 4.87%)** | |
| Temperature, short term | 8.63% (7.88%; 9.39%)** | |
| Temperature, long term (10th p) | 6.24% (6.54%; 5.93%)** | |
| Temperature, long term (90th p) | 1.37% (1.28%;1.47%)** | |
| Cardiac | PM2.5, short term | 0.02% (−0.18%; 0.23%) |
| PM2.5, long term | 6.58% (5.90%; 7.26%)** | |
| Temperature, short term | 3.63% (3.01%; 4.25%)** | |
| Temperature, long term (10th p) | −2.15% (−2.36%; −1.93%)** | |
| Temperature, long term (90th p) | −1.69% (−1.77%; −1.60%)** | |
| Ischemic stroke | PM2.5 short term | 1.20% (0.71%; 1.69%)** |
| PM2.5, long term | 0.82% (−0.68%; 2.35%) | |
| Temperature, short term | −0.08% (−1.49%; 1.34%) | |
| Temperature, long term (10th p) | 7.32% (6.68%; 7.96%)** | |
| Temperature, long term (90th p) | 0.15% (−0.04%; 0.34%) |
Results are presented as percent change and 95% Confidence Intervals (CI) for an IQR increase in short term PM2.5 (5.4 μg/m3), long term PM 3, 2.5 (2.3 μg/m) short term temperature (9.2 °C) and long term temperature (2.2 °C). The effect of the long-term exposure to temperature was modeled using penalized splines, results are therefore presented as percent change and 95% Confidence Intervals (CI) for IQR increases in the 10th (8 °C) and 90th (10.2 °C) percentile of temperature. We used the moving average of PM2.5 at lag days 0-1 for the calculation of the short-term exposure to PM2.5, temperature ta lag day 0 for the calculation of short-term temperature and annual averages for the long-term exposures of PM2.5 and temperature.
p<0.05
For PM2.5, an IQR (5.4 μg/m3) increase in short-term exposure to PM2.5 was associated with a 0.41% (95% CI: 0.16; 0.65) increase in respiratory admissions and a 1.20% (95% CI: 0.71; 1.69) increase in stroke admissions rate. Larger and statistically significant associations with IQR (2.3 μg/m3) increases of long-term exposure to PM2.5 were observed for respiratory (4.09% increase (95% CI: 3.31; 4.87) and cardiac (6.58% increase (95% CI: 5.90; 7.26) admissions rate.
Figures 1 and 2 show the interaction of the short-term exposures and the modification of these exposures by monthly standard deviation of temperature. For respiratory admissions (Figure 1), the effect of short-term exposure to temperature was stronger on days of higher PM2.5 concentration (9.75%, 95% CI 8.91;10.60 in the 90th percentile) compared to days of lower concentration (7.68%, 95% CI 6.87;8.49 in the 10th percentile, interaction p <0.001); and in months of higher temperature variability (8.99%, 95% CI 8.19;9.80 in the 90th percentile) compared to lower temperature variability (7.55%, 95% CI 6.53;8.57 in the 10th percentile, interaction p <0.001). For cardiac admissions, the effect of short-term exposure to temperature was stronger on days of lower PM2.5 concentration (4.12%, 95% CI 3.44; 4.79 in the 10th percentile) compared to days of higher concentration (3.08%, 95% CI 2.40; 3.77 in the 90th percentile, interaction p <0.001).
Figure 1. The effect of short-term temperature across the range of short-term PM2.5 and monthly standard deviation (SD) of temperature.
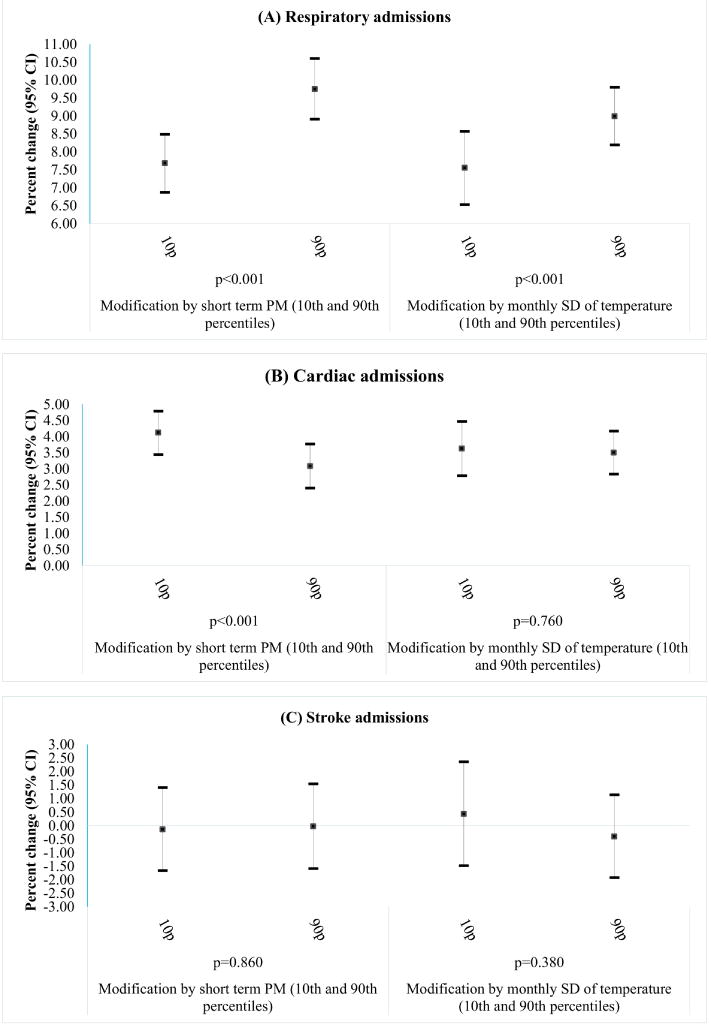
Results are presented as percent change and 95% Confidence Intervals (CI) for an IQR increase in temperature at the 10th and 90th percentiles of the distribution of short-term exposure to PM2.5and monthly standard deviation of temperature.
Figure 2. The effect of short-term PM2.5 across the range of short-term temperature and monthly standard deviation (SD) of temperature.
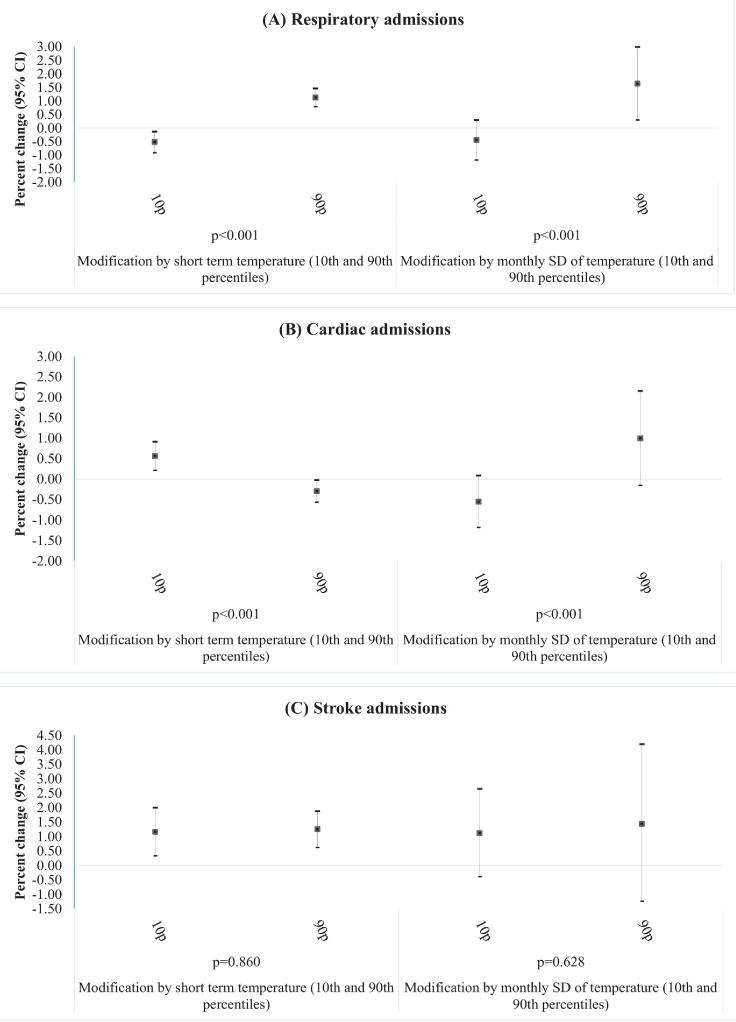
Results are presented as percent change and 95% Confidence Intervals (CI) for an IQR increase in short-term exposure to PM2.5 at the 10th and 90th percentiles of the distribution of short-term exposure to temperature and monthly standard deviation of temperature.
The short-term effect of PM2.5 on respiratory and cardiac admissions was significantly modified by short-term exposure to temperature and temperature variability (Figure 2). For respiratory admissions, the effect of short-term exposure to PM2.5 was stronger on hotter days (1.12%, 95% CI 0.78;1.45 in the 90th percentile) compared to colder days (−0.53%, 95% CI −0.92; −0.14 in the 10th percentile, interaction p <0.001); and in months of higher temperature variability (1.63%, 95% CI 0.29;2.99 in the 90th percentile) compared to lower temperature variability (−0.45%, 95% CI −1.19;0.29 in the 10th percentile, interaction p <0.001). For cardiac admissions, the effect of short-term exposure to PM2.5 was stronger on colder days (0.56%, 95% CI 0.21;0.91 in the 10th percentile) compared to hotter days (−0.30%, 95% CI −0.57; −0.03 in the 90th percentile, interaction p <0.001); and in months of higher temperature variability (0.99%, 95% CI −0.16;2.15 in the 90th percentile) compared to lower temperature variability (−0.56%, 95% CI 0.21;0.91 in the 10th percentile, interaction p <0.001).
4. DISCUSSION
Our study shows associations between both short and long-term exposures to PM2.5 and temperature and increased risk of hospital admissions, and evidence of synergy between the short-term exposures. Increased risk for respiratory admissions was associated with the short and long-term exposures, with larger effects of short-term exposure to PM2.5 on warmer days, and larger effects of both short-term exposures to PM2.5 and temperature on days of higher temperature variability. Increased risk for cardiac admissions was associated with long-term exposure to PM2.5, and both short and long-term exposures to temperature, with smaller effects of short-term exposure to PM2.5 on warmer days, and larger effects on days of higher temperature variability. A significantly increased risk of ischemic stroke was associated with the short-term exposure to PM2.5 and long-term exposure to temperature, but the associations were not modified by PM2.5, temperature or temperature variability. The finding of substantially larger effect sizes for longer-term exposure to PM2.5 on incidence of ischemic stroke and on cardiac admissions than of shorter-term exposures is important, because it indicates that PM2.5 exposure does not simply advance the timing of these events, it increases the incidence rate. This is consistent with mortality studies, which show considerably larger effect size estimates for long-term PM2.5 exposure than for short-term exposure (44–46). Current risk assessments by the U.S. EPA and WHO only estimate the effect of short-term exposure to PM2.5 (or temperature) on these events, and the evidence from our study suggests these may be substantial underestimates. In addition, the PM2.5 associations we found were entirely below the current U.S. annual standard of 35 μg/m3(44), indicating those standards are inadequate to protect public health.
In recent decades, studies have suggested that extreme temperatures may have a significant health impact. Multiple studies have reported an excessive number of cardiac and respiratory hospitalizations during episodes of heat waves (9, 47, 48). Depending on the climate, episodes of extreme cold may also pose a threat to health in high latitude countries (49, 50). Studies of the associations between heat and hospital admissions show inconsistent results. A previous study performed among this study population (but for the entire country) found a higher risk for renal failure and heat stroke and a lower risk for congestive heart failure, associated with heat waves; no association was found with respiratory illness (51). Other studies did find, however, an increased risk for respiratory admissions in this elderly population associated with extreme heat or increased temperatures (43, 52). Regarding cardiac admissions, a recent meta-analysis reported an increase in the risk for hospitalizations associated with short-term exposures to both extreme heat and cold (49). Another review found heat exposure to be associated with increased risk of cardiac, cerebrovascular and respiratory mortality, but not cardiac or cerebrovascular morbidity (53). The evidence on the association between PM2.5 and hospital admissions is more consistent, with evidence of links to cardiac (37, 54, 55) respiratory (10, 56) and stroke admissions (1, 57).
All of the above studies assessed associations with either acute or chronic exposure. A key finding of this study is the independent effects of short and long-term exposures to PM2.5 and temperature while accounting for both windows of exposure simultaneously. For all the cause-specific admissions tested, the long-term effect estimate of PM2.5 was larger than the short-term effect. Interestingly, for respiratory and stroke admissions, the short-term effect was still present independently of the long-term effect. Both short and long-term effects of PM2.5 on health are biologically plausible. PM exposure can directly affect the airways, bronchiole, and alveolus through inhalation, decreasing lung function and inducing pulmonary inflammation and oxidative stress (58, 59). Cardiovascular symptoms can be directly induced through the effect of PM on receptors of the lungs, blood and cardiovascular system or indirectly mediated through inflammatory pathways and oxidative stress (4). The stronger effect of the long-term exposures can be explained by cumulative damage of these prolonged exposures (2).
Our findings show a larger increase in PM related respiratory admission rate on warmer days and days of higher temperature variability. Several theories were suggested to explain this synergistic effect with respect to cardiorespiratory morbidity and mortality. Stafoggia et al hypothesized that the modification, of PM-associated mortality, by temperature is mainly due to higher exposure to air pollution during warmer temperatures (20). Another theory is that temperature exposure can cause physiological stress and alter the response to the air pollutants, especially among more vulnerable individuals (21). We also observed a larger increase in temperature related respiratory admission rate on months of higher temperature variability. Unstable temperatures may modify the population response to temperature exposure by affecting heart rate, blood pressure, blood viscosity, peripheral vasoconstriction and the autonomic nervous system. Different countries may present different patterns of association with temperature variability depending on the climate (19).
For cardiac admissions, larger effects of PM2.5 were observed at lower temperatures. These results are in accordance with previous findings of larger PM2.5 related increases in cardiac disease admission rate during the winter season (10, 36). These findings may be explained by the extensive use of coal, oil, diesel or wood burn based heating during colder temperatures. This, alongside a tendency to stay indoors with poor ventilation, may increase the PM effect (36). Furthermore, the toxicity of PM2.5 may vary by its composition, which may vary seasonally and affect differently on human health (60), specifically on cardiac and respiratory outcomes. Interestingly, similar to respiratory admissions, larger PM2.5 effects were also observed on months of higher temperature variability. Which, again, may be related to the body response to unstable temperatures.
A major limitation of this study is its ecological nature, which did not allow us to control for individual level potential confounders such as age, diet, socioeconomic status etc. To minimize the potential confounding within the limits of this study, we have used area level socioeconomic variables. In addition, the assignment of exposure based on ZIP code rather than geocoded addresses may introduce some exposure misclassification into our study. To address that, we averaged the predictions obtained from our high spatially resolved satellite-based models, within the limits of each ZIP code.
In conclusion, our findings indicate associations between PM2.5, temperature and respiratory, cardiac and stroke admissions rate, with stronger effects of long-term exposure to PM2.5. We observed synergistic effects of the short-term exposures, and of PM2.5 and temperature and monthly temperature variability, with respect to respiratory and cardiac admissions. These findings emphasize the importance in assessing the joint effect of air pollution and climate parameters when investigating their effect on health.
Supplementary Material
Supplementary Figure 1. The mean annual PM2.5 and temperature predictions averaged within ZIP codes
Supplementary Figure 2. The association between short and long-term exposure to temperature and hospital admissions rate.
Supplementary figure 2 shows the association between short and long-term temperature exposures and respiratory, cardiac and stroke admissions rate, using penalized splines of temperature to allow for nonlinear relationship. All the models were adjusted for a smoothed function of time (using natural cubic splines with 5 degrees of freedom per year), day of the week, and ZIP code level socioeconomic variables (age, percent minorities, median household income and percent people with no high school education).
The two vertical lines represent the 2nd and 98th percentile of the short and long-term temperature distributions.
Figure 3.
Highlights.
Associations between short and long-term exposures were observed for all outcomes
Long-term exposures to particulate matter<2.5μm (PM2.5) had stronger effects than short-term exposures
Short-term PM2.5 related respiratory risk was larger on warmer days and
Short-term PM2.5 related cardiac in risk was larger on colder days
Short-term PM2.5 risks were larger in months of higher temperature variability
Acknowledgments
This study was supported by the NIH grant R01 ES024332-01A1, ES-000002, ES024012; HEI grant 4953-RFA14-3/16-4. This publication was made possible also by USEPA grant RD-835872-01. Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the USEPA. Further, USEPA does not endorse the purchase of any commercial products or services mentioned in the publication
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no competing financial interests to declare
References
- 1.Yitshak-Sade M, Novack V, Ifergane G, Horev A, Kloog I. Air Pollution and Ischemic Stroke Among Young Adults. Stroke. 2015;46(12):3348–53. doi: 10.1161/STROKEAHA.115.010992. [DOI] [PubMed] [Google Scholar]
- 2.Kloog I, Coull BA, Zanobetti A, Koutrakis P, Schwartz JD. Acute and Chronic Effects of Particles on Hospital Admissions in New-England. Plos One. 2012;7(4) doi: 10.1371/journal.pone.0034664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kloog I, Zanobetti A, Nordio F, Coull BA, Baccarelli AA, Schwartz J. Effects of airborne fine particles (PM2.5) on deep vein thrombosis admissions in the northeastern United States. Journal of Thrombosis and Haemostasis. 2015;13(5):768–74. doi: 10.1111/jth.12873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate Matter Air Pollution and Cardiovascular Disease An Update to the Scientific Statement From the American Heart Association. Circulation. 2010;121(21):2331–78. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 5.Barnett AG, Williams GM, Schwartz J, Best TL, Neller AH, Petroeschevsky AL, et al. The effects of air pollution on hospitalizations for cardiovascular disease in elderly people in Australian and New Zealand cities. Environmental Health Perspectives. 2006;114(7):1018–23. doi: 10.1289/ehp.8674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103(23):2810–5. doi: 10.1161/01.cir.103.23.2810. [DOI] [PubMed] [Google Scholar]
- 7.Ye XF, Wolff R, Yu WW, Vaneckova P, Pan XC, Tong SL. Ambient Temperature and Morbidity: A Review of Epidemiological Evidence. Environmental Health Perspectives. 2012;120(1):19–28. doi: 10.1289/ehp.1003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Michelozzi P, Accetta G, De Sario M, D’Ippoliti D, Marino C, Baccini M, et al. High Temperature and Hospitalizations for Cardiovascular and Respiratory Causes in 12 European Cities. American Journal of Respiratory and Critical Care Medicine. 2009;179(5):383–9. doi: 10.1164/rccm.200802-217OC. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz J, Samet JM, Patz JA. Hospital admissions for heart disease - The effects of temperature and humidity. Epidemiology. 2004;15(6):755–61. doi: 10.1097/01.ede.0000134875.15919.0f. [DOI] [PubMed] [Google Scholar]
- 10.Bell ML, Ebisu K, Peng RD, Walker J, Samet JM, Zeger SL, et al. Seasonal and Regional Short-term Effects of Fine Particles on Hospital Admissions in 202 US Counties, 1999-2005. American Journal of Epidemiology. 2008;168(11):1301–10. doi: 10.1093/aje/kwn252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kloog I, Nordio F, Zanobetti A, Coull BA, Koutrakis P, Schwartz JD. Short Term Effects of Particle Exposure on Hospital Admissions in the Mid-Atlantic States: A Population Estimate. Plos One. 2014;9(2) doi: 10.1371/journal.pone.0088578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McMichael AJ, Woodruff RE, Hale S. Climate change and human health: present and future risks (vol 367, pg 859, 2006) Lancet. 2006;368(9538):842. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- 13.Li J, Woodward A, Hou X-Y, Zhu T, Zhang J, Brown H, et al. Modification of the effects of air pollutants on mortality by temperature: A systematic review and meta analysis. Science of the total environment. 2017;575:1556–70. doi: 10.1016/j.scitotenv.2016.10.070. [DOI] [PubMed] [Google Scholar]
- 14.Zanobetti A, Peters A. Disentangling interactions between atmospheric pollution and weather. Journal of Epidemiology and Community Health. 2015;69(7):613–5. doi: 10.1136/jech-2014-203939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shi L, Liu P, Wang Y, Zanobetti A, Kosheleva A, Koutrakis P, et al. Chronic effects of temperature on mortality in the Southeastern USA using satellite-based exposure metrics. Sci Rep. 2016;6:30161. doi: 10.1038/srep30161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi L, Kloog I, Zanobetti A, Liu P, Schwartz J. Impacts of Temperature and its Variability on Mortality in New England. Nature Climate Change ip. Impacts of Temperature and its Variability on Mortality in New England. 2015;5:988–91. doi: 10.1038/nclimate2704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson BG, Bell ML. Weather-Related Mortality How Heat, Cold, and Heat Waves Affect Mortality in the United States. Epidemiology. 2009;20(2):205–13. doi: 10.1097/EDE.0b013e318190ee08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Breitner S, Wolf K, Devlin RB, Diaz-Sanchez D, Peters A, Schneider A. Short-term effects of air temperature on mortality and effect modification by air pollution in three cities of Bavaria, Germany: A time-series analysis. Science of the Total Environment. 2014;485:49–61. doi: 10.1016/j.scitotenv.2014.03.048. [DOI] [PubMed] [Google Scholar]
- 19.Guo YM, Gasparrini A, Armstrong B, Tawatsupa B, Tobias A, Lavigne E, et al. Temperature Variability and Mortality: A Multi-Country Study. Environmental Health Perspectives. 2016;124(10):1554–9. doi: 10.1289/EHP149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stafoggia M, Schwartz J, Forastiere F, Perucci CA, Group S Does temperature modify the association between air pollution and mortality? A multicity case-crossover analysis in Italy. American Journal of Epidemiology. 2008;167(12):1476–85. doi: 10.1093/aje/kwn074. [DOI] [PubMed] [Google Scholar]
- 21.Li Y, Ma ZQ, Zheng CJ, Shang Y. Ambient temperature enhanced acute cardiovascular-respiratory mortality effects of PM2.5 in Beijing, China. International Journal of Biometeorology. 2015;59(12):1761–70. doi: 10.1007/s00484-015-0984-z. [DOI] [PubMed] [Google Scholar]
- 22.Zanobetti A, O’Neill MS, Gronlund CJ, Schwartz JD. Summer temperature variability and long-term survival among elderly people with chronic disease. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(17):6608–13. doi: 10.1073/pnas.1113070109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stocker T. Climate Change 2013: The Physical Science Basis: Working Group I Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. New York: Cambridge University Press; 2014. [Google Scholar]
- 24.Kioumourtzoglou MA, Schwartz J, James P, Dominici F, Zanobetti A. PM2.5 and Mortality in 207 US Cities Modification by Temperature and City Characteristics. Epidemiology. 2016;27(2):221–7. doi: 10.1097/EDE.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun SZ, Cao PH, Chan KP, Tsang H, Wong CM, Thach TQ. Temperature as a modifier of the effects of fine particulate matter on acute mortality in Hong Kong. Environmental Pollution. 2015;205:357–64. doi: 10.1016/j.envpol.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 26.Li L, Yang J, Guo C, Chen PY, Ou CQ, Guo YM. Particulate matter modifies the magnitude and time course of the non-linear temperature-mortality association. Environmental Pollution. 2015;196:423–30. doi: 10.1016/j.envpol.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 27.Analitis A, Michelozzi P, D’Ippoliti D, de’Donato F, Menne B, Matthies F, et al. Effects of Heat Waves on Mortality Effect Modification and Confounding by Air Pollutants. Epidemiology. 2014;25(1):15–22. doi: 10.1097/EDE.0b013e31828ac01b. [DOI] [PubMed] [Google Scholar]
- 28.Burkart K, Canario P, Breitner S, Schneider A, Scherber K, Andrade H, et al. Interactive short-term effects of equivalent temperature and air pollution on human mortality in Berlin and Lisbon. Environmental Pollution. 2013;183:54–63. doi: 10.1016/j.envpol.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Kim SE, Lim YH, Kim H. Temperature modifies the association between particulate air pollution and mortality: A multi-city study in South Korea. Science of the Total Environment. 2015;524:376–83. doi: 10.1016/j.scitotenv.2015.03.137. [DOI] [PubMed] [Google Scholar]
- 30.Dholakia HH, Bhadra D, Garg A. Short term association between ambient air pollution and mortality and modification by temperature in five Indian cities. Atmospheric Environment. 2014;99:168–74. [Google Scholar]
- 31.O’Neill MS, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. American Journal of Epidemiology. 2003;157(12):1074–82. doi: 10.1093/aje/kwg096. [DOI] [PubMed] [Google Scholar]
- 32.Shi LH, Zanobetti A, Kloog I, Coull BA, Koutrakis P, Melly SJ, et al. Low-Concentration PM2.5 and Mortality: Estimating Acute and Chronic Effects in a Population-Based Study. Environmental Health Perspectives. 2016;124(1):46–52. doi: 10.1289/ehp.1409111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y, Shi LH, Lee M, Liu PF, Di Q, Zanobetti A, et al. Long-term Exposure to PM2.5 and Mortality Among Older Adults in the Southeastern US. Epidemiology. 2017;28(2):207–14. doi: 10.1097/EDE.0000000000000614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pan WC, Eliot MN, Koutrakis P, Coull BA, Sorond FA, Wellenius GA. Ambient Temperature and Cerebrovascular Hemodynamics in the Elderly. Plos One. 2015;10(8) doi: 10.1371/journal.pone.0134034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang FF, Luo YX, Guo YM, Tao LX, Xu Q, Wang C, et al. Particulate Matter and Hospital Admissions for Stroke in Beijing, China: Modification Effects by Ambient Temperature. Journal of the American Heart Association. 2016;5(7) doi: 10.1161/JAHA.116.003437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hsu W-H, Hwang S-A, Kinney PL, Linc S. Seasonal and temperature modifications of the association between fine particulate air pollution and cardiovascular hospitalization in NewYork state. Science of the Total Environment. 2017;578:626–32. doi: 10.1016/j.scitotenv.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dominici F, Peng RD, Bell ML, Pham L, McDermott A, Zeger SL, et al. Fine particulate air pollution and hospital admission for cardiovascular and respiratory diseases. Jama-Journal of the American Medical Association. 2006;295(10):1127–34. doi: 10.1001/jama.295.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kloog I, Ridgway B, Koutrakis P, Coull BA, Schwartz JD. Long- and Short-Term Exposure to PM2.5 and Mortality: Using Novel Exposure Models. Epidemiology. 2013;24(4):555–61. doi: 10.1097/EDE.0b013e318294beaa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kloog I, Chudnovsky AA, Just AC, Nordio F, Koutrakis P, Coull BA, et al. A new hybrid spatio-temporal model for estimating daily multi-year PM2.5 concentrations across northeastern USA using high resolution aerosol optical depth data. Atmospheric Environment. 2014;95:581–90. doi: 10.1016/j.atmosenv.2014.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kloog I, Nordio F, Coull BA, Schwartz J. Predicting spatiotemporal mean air temperature using MODIS satellite surface temperature measurements across the Northeastern USA. Remote Sensing of Environment. 2014;150:132–9. [Google Scholar]
- 41.Laird N, Olivier D. Covariance analysis of censored survival data using log-linear analysis techniques. Journal of the American Statistical Association. 1981;76(374):231–40. [Google Scholar]
- 42.Nordio F, Zanobetti A, Colicino E, Kloog I, Schwartz J. Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environment International. 2015;81:80–6. doi: 10.1016/j.envint.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson GB, Dominici F, Wang Y, McCormack MC, Bell ML, Peng RD. Heat-related Emergency Hospitalizations for Respiratory Diseases in the Medicare Population. American Journal of Respiratory and Critical Care Medicine. 2013;187(10):1098–103. doi: 10.1164/rccm.201211-1969OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim KH, Kabir E, Kabir S. A review on the human health impact of airborne particulate matter. Environment International. 2015;74:136–43. doi: 10.1016/j.envint.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 45.Lu F, Xu DQ, Cheng YB, Dong SX, Guo C, Jiang X, et al. Systematic review and meta-analysis of the adverse health effects of ambient PM2.5 and PM10 pollution in the Chinese population. Environmental Research. 2015;136:196–204. doi: 10.1016/j.envres.2014.06.029. [DOI] [PubMed] [Google Scholar]
- 46.Zhao L, Liang HR, Chen FY, Chen Z, Guan WJ, Li JH. Association between air pollution and cardiovascular mortality in China: a systematic review and meta-analysis. Oncotarget. 2017;8(39):66438–48. doi: 10.18632/oncotarget.20090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Knowlton K, Rotkin-Ellman M, King G, Margolis HG, Smith D, Solomon G, et al. The 2006 California Heat Wave: Impacts on Hospitalizations and Emergency Department Visits. Environmental Health Perspectives. 2009;117(1):61–7. doi: 10.1289/ehp.11594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Empana JP, Sauval P, Ducimetiere P, Tafflet M, Carli P, Jouven X. Increase in out-of-hospital cardiac arrest attended by the medical mobile intensive care units, but not myocardial infarction, during the 2003 heat wave in Paris, France. Critical Care Medicine. 2009;37(12):3079–84. doi: 10.1097/CCM.0b013e3181b0868f. [DOI] [PubMed] [Google Scholar]
- 49.Phung D, Thai PK, Guo YM, Morawska L, Rutherford S, Chu C. Ambient temperature and risk of cardiovascular hospitalization: An updated systematic review and meta-analysis. Science of the Total Environment. 2016;550:1084–102. doi: 10.1016/j.scitotenv.2016.01.154. [DOI] [PubMed] [Google Scholar]
- 50.Shaposhnikov D, Revich B, Gurfinkel Y, Naumova E. The influence of meteorological and geomagnetic factors on acute myocardial infarction and brain stroke in Moscow, Russia. International Journal of Biometeorology. 2014;58(5):799–808. doi: 10.1007/s00484-013-0660-0. [DOI] [PubMed] [Google Scholar]
- 51.Bobb JF, Obermeyer Z, Wang Y, Dominici F. Cause-Specific Risk of Hospital Admission Related to Extreme Heat in Older Adults. Jama-Journal of the American Medical Association. 2014;312(24):2659–67. doi: 10.1001/jama.2014.15715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. Heat, Heat Waves, and Hospital Admissions among the Elderly in the United States, 1992-2006. Environmental Health Perspectives. 2014;122(11):1187–92. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Song XP, Wang SG, Hu YL, Yue M, Zhang TT, Liu Y, et al. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Science of the Total Environment. 2017;586:241–54. doi: 10.1016/j.scitotenv.2017.01.212. [DOI] [PubMed] [Google Scholar]
- 54.Luo CM, Zhu XX, Yao CJ, Hou LJ, Zhang J, Cao JY, et al. Short-term exposure to particulate air pollution and risk of myocardial infarction: a systematic review and meta-analysis. Environmental Science and Pollution Research. 2015;22(19):14651–62. doi: 10.1007/s11356-015-5188-x. [DOI] [PubMed] [Google Scholar]
- 55.Zanobetti A, Franklin M, Koutrakis P, Schwartz J. Fine particulate air pollution and its components in association with cause-specific emergency admissions. Environmental Health. 2009;8:12. doi: 10.1186/1476-069X-8-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between Air Pollutants and Asthma Emergency Room Visits and Hospital Admissions in Time Series Studies: A Systematic Review and Meta-Analysis. Plos One. 2015;10(9):24. doi: 10.1371/journal.pone.0138146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang Y, Eliot MN, Wellenius GA. Short-term Changes in Ambient Particulate Matter and Risk of Stroke: A Systematic Review and Meta-analysis. Journal of the American Heart Association. 2014;3(4):22. doi: 10.1161/JAHA.114.000983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ren CZ, Williams GM, Tong SL. Does particulate matter modify the association between temperature and cardiorespiratory diseases? Environmental Health Perspectives. 2006;114(11):1690–6. doi: 10.1289/ehp.9266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pope CA, Dockery DW. Health effects of fine particulate air pollution: Lines that connect. Journal of the Air & Waste Management Association. 2006;56(6):709–42. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 60.Peng RD, Bell ML, Geyh AS, McDermott A, Zeger SL, Samet JM, et al. Emergency Admissions for Cardiovascular and Respiratory Diseases and the Chemical Composition of Fine Particle Air Pollution. Environmental Health Perspectives. 2009;117(6):957–63. doi: 10.1289/ehp.0800185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1. The mean annual PM2.5 and temperature predictions averaged within ZIP codes
Supplementary Figure 2. The association between short and long-term exposure to temperature and hospital admissions rate.
Supplementary figure 2 shows the association between short and long-term temperature exposures and respiratory, cardiac and stroke admissions rate, using penalized splines of temperature to allow for nonlinear relationship. All the models were adjusted for a smoothed function of time (using natural cubic splines with 5 degrees of freedom per year), day of the week, and ZIP code level socioeconomic variables (age, percent minorities, median household income and percent people with no high school education).
The two vertical lines represent the 2nd and 98th percentile of the short and long-term temperature distributions.


