Abstract
Background
We compared direct and daily cumulative energy expenditure (EE) differences associated with reallocating sedentary time to physical activity in adults for meaningful EE changes.
Methods
Peer-reviewed studies in PubMed, Medline, EMBASE, CINAHL, PsycINFO, Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews were searched from inception to March 2017. Randomized and non-randomized interventions with sedentary time and EE outcomes in adults were included. Study quality was assessed by the National Heart Lung and Blood Institute tool, and summarized using random-effects meta-analysis and meta-regression.
Results
In total, 26 studies were reviewed, and 24 studies examined by meta-analysis. Reallocating 6–9 h of sedentary time to light-intensity physical activity (LIPA) (standardized mean difference [SMD], 2.501 [CI: 1.204–5.363]) had lower cumulative EE than 6–9 h of combined LIPA and moderate-vigorous intensity physical activity (LIPA and moderate-vigorous physical activity [MVPA]) (SMD, 5.218 [CI: 3.822–6.613]). Reallocating 1 h of MVPA resulted in greater cumulative EE than 3–5 h of LIPA and MVPA, but <6–9 h of LIPA and MVPA.
Conclusions
Comparable EE can be achieved by different strategies, and promoting MVPA might be effective for those individuals where a combination of MVPA and LIPA is challenging.
Keywords: health promotion, physical activity, public health
Background
Sedentary behaviours are increasingly ubiquitous in today’s society, with the average person spending more than half of their waking day expending little energy (≤1.5 resting metabolic equivalents [METs]) in sitting or reclining postures.1,2 Mounting evidence suggests that prolonged sedentary time (i.e. too much sitting) can increase an adult’s risk for cardio-metabolic diseases and mortality independent of moderate to vigorous physical activity (MVPA).3 Accordingly, sedentary lifestyles are recognized as a distinct public health concern.4 Since sedentary behaviours are associated with low energy expenditure (EE), it may be beneficial to focus on interrupting or reallocating sedentary time to increase EE. For example, postural changes when transitioning from a sedentary state to a light-intensity physical activity (LIPA) such as standing elicits musculoskeletal changes that influence metabolic health benefits5 and may increase EE. However, it is still unclear from existing evidence whether one method of time-reallocation to increase cumulative caloric expenditures (e.g. sedentary time to LIPA) is superior to another (e.g. sedentary time to MVPA). Based on the FITT principle, the former would presumably require a longer time commitment consisting of lower workload intensity, while the latter may allow for shorter time commitments, but would require greater effort and higher workload intensities.6
Studies examining the reallocation of sedentary behaviours to LIPA and/or MVPA have increasingly used isotemporal substitution modeling.7,8 However, conclusions based on this approach can be confusing as they utilize cross-sectional study designs and not a true temporal substitution. In addition, they focus on associations with long-term health risks such as mortality, of which the risks may be difficult to delineate from other potential confounding factors. Alternatively, determining the cumulative EE benefits of reallocating sedentary time to physical activity over a waking day helps to answer the more relevant causal and public health question of how to spend our sedentary time for immediate health benefits. The objectives of this systematic review and meta-analysis were to first, compare the direct EE differences reported by interventions where sedentary time was reallocated to physical activity and second, to evaluate the daily cumulative EE differences (EE scaled and compared over a waking day) associated with these interventions. We hypothesized that LIPA-based interventions, by reallocating a greater daily duration of sedentary time, will result in greater cumulative EE than those interventions reallocating to MVPA alone.
Methods
Electronic data sources and searches
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed.9 The Medline literature search strategy was designed in consultation with a research librarian, utilizing the PICO method (see Supplementary Table 1). Adapting the subject headings as necessary, each of the following medical databases were searched from inception to March 2017: Medline (Ovid), PubMed (excluding Medline records), Embase, CINAHL, PsycINFO, the Cochrane Central Register of Controlled Clinical Trials and the Cochrane Database of Systematic Reviews. Duplicate records were removed prior to applying the inclusion/exclusion criteria.
The aim of the search strategy was to extract peer-reviewed studies and/or abstracts providing adequate data on the effect of physical activity interventions on sedentary behaviour with outcomes related to EE or metabolic health in adults. Studies conducted in free-living or controlled conditions were both considered. No restrictions were placed on search results with respect to publication year, length of follow-up, population, geographic origin, outcome measurement or language, but minor publication types and non-peer reviewed articles (‘grey’ literature, newspaper articles, personal narratives, legal cases, etc.) were excluded to maximize the comparison of studies with suitable methodological quality. Reference lists were manually examined to supplement the electronic searches.
Study selection
Eligible studies included were randomized and non-randomized intervention investigations (trials and observational studies) that assessed adult populations (aged ≥18 years), with sedentary time and a measure of EE (and broadly as metabolic health) as an outcome. Two authors independently screened study titles and abstracts for inclusion. We operationally distinguished sedentary behaviours as a distinct class of waking activity characterized by low EE (≤1.5 METs) in a sitting or reclined position1 and excluded studies that defined sedentary behaviour as a category of physical activity or as inadequate physical activity.10 LIPA was predefined as activities such as standing and walking at a pace of 1.7–2.5 miles per hour (1.6–2.9 METs); MVPA was predefined as activities such as calisthenics, bicycling, walking at a pace greater than 3 miles per hour, or jogging (≥3 METs).11
Data extraction and quality assessment
Data were extracted from all studies that were flagged for review by at least one author. Details of individual studies were collected and characterized on the basis of authors and year of publication; study design; sample size and characteristics; data collection methods (exposure and outcome), follow-up length, attrition and mean differences. Included studies were assessed for risk of bias using the criteria outlined by the National Heart Lung and Blood Institute’s Controlled Intervention Studies and the Observational Cohort Quality Assessment Tools.12 These tools were selected over others given their ability to assess the internal validity of a range of observational and interventional study designs. Two authors independently assessed articles for quality and any scoring inconsistencies were discussed with an additional reviewer. An intra-class correlation coefficient of 0.92 [95% CI: 0.82–0.97] indicated excellent reviewer agreement during the scoring process.
Data synthesis and analysis
All included studies were qualitatively analyzed to directly compare mean differences in equivalent EE associated with reallocating sedentary time to physical activity. Studies with comparable outcome data were quantitatively analyzed by meta-analysis, where standardized mean differences (SMD) were used to estimate pooled EE effect sizes. Efforts were made to contact study authors when suitable data were not reported or available (four authors provided additional unpublished data from eight contacted). Statistical heterogeneity was assessed using Cochran’s Q statistic and the I2 statistic of the proportion of total variation because of heterogeneity.13 An I2 value of 25–50% indicated a low degree of heterogeneity, 50–75% a moderate degree of heterogeneity and more than 75% a high degree of heterogeneity. If a small number of studies were available for meta-analysis or we saw substantial heterogeneity, we considered a Knapp–Hartung modified random-effects model to yield more conservative effects.14 For the summary estimate, we considered a P < 0.05 as statistically significant. We graphically explored the potential for small study effects such as publication bias using Egger test of asymmetry of funnel plots and quantitatively by the Egger linear regression method.15 The meta-analyses and the generation of forest plots were conducted using Comprehensive Meta-analysis, version 2 (Biostat), and the R statistical software (R Foundation for Statistical Computing).16,17 For our second objective, we compared the EE of interventions by their daily duration of exertion (cumulative EE). We found several LIPA intervention studies were conducted over short trial periods to detect direct rather than EE accumulated over a day. In this case, we calculated projected estimations by extrapolating the direct EE (in kcal/h) over a 12-h period (to standardize the typical duration of a waking day). This method and time frame has been used in other studies extrapolating EE and other outcomes over a waking day.18,19
Subgroup analysis was explored using meta-regression (‘method of moments’ random-effects model) to investigate whether associations with EE varied according to sex, acute (<1 day) vs. long duration studies (>1 day), risk of bias, and measures of EE (e.g. indirect calorimetry vs. accelerometer).20 To assess the robustness of our findings, we also examined the effect of individual studies on pooled effect estimates.
Results
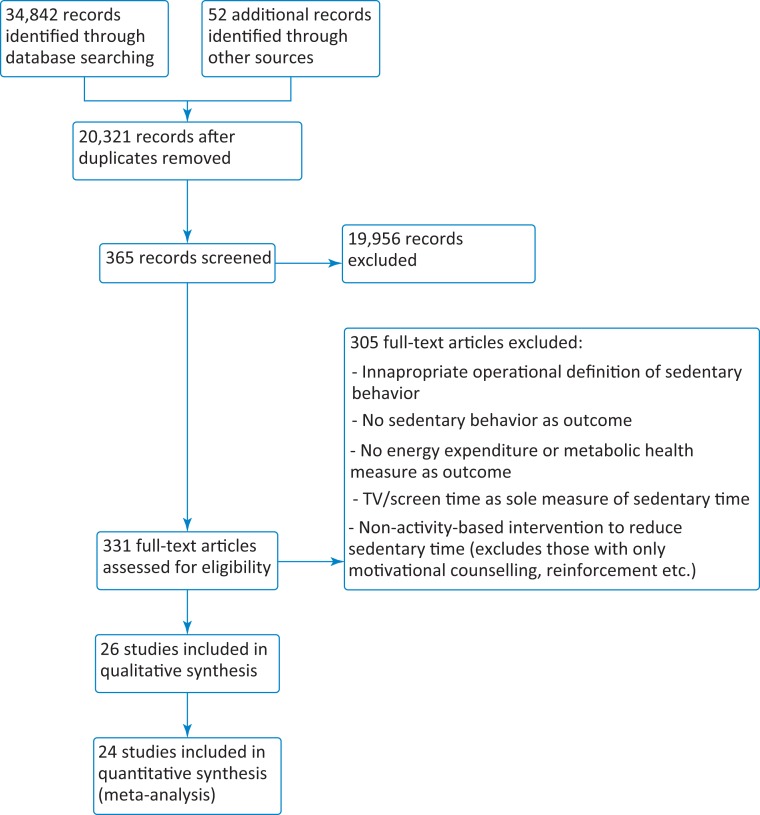
A total of 34 842 studies were identified through database searching (PubMed [excluding Medline]: 2 809; Medline: 11 899; EMBASE: 13 728; CINAHL: 721; PsycINFO: 2 655; the Cochrane Central Register of Controlled Trials: 3006, and the Cochrane Database of Systematic Reviews databases: 204) and 52 were added after hand searching in-text citations (Fig. 1). In total, 26 studies (949 participants) were qualitatively analyzed, of which, 24 studies (869 participants) were included in the meta-analysis.
Fig. 1.
Summary of evidence search and selection.
Study characteristics
The risk of bias of the included studies and an overview of study characteristics are summarized in Supplementary Table 2. Overall, 10 studies had a high risk of bias,21–30 12 had a moderate risk of bias,18,31–41 and 4 studies had low risk of bias.42–45 Four studies were randomized controlled trials21,27,38,42; 20 were randomized and non-randomized crossover trials with three to five treatment conditions18,22–24,26,28–31,33–37,39,41,43–46; and the remaining two studies utilized repeated-measures or quasi-experimental study designs.25,32 Studies were all conducted in the high-income countries of the United States, Australia, New Zealand, United Kingdom, Canada, Spain and The Netherlands. The majority of studies (n = 15) utilized objective measurement methods to assess sedentary time and physical activity (by accelerometer and/or inclinometer devices) and objective methods to assess EE via indirect calorimetric and accelerometer estimates (n = 25). A total of 20 studies featured conditions where the focus was on limiting and/or replacing bouts of sedentary time with LIPA (LIPA interventions)21,23,24,26–41,45; 10 studies featured conditions where sedentary time was replaced with MVPA (MVPA interventions)18,23,26,29,33,35–37,41,42,45; and four studies featured a combination of both (LIPA and MVPA interventions).23,27,35,43 The majority of studies were conducted over a short duration (<1 week), with five studies conducted from 5 weeks to 24 months.
Publication bias and heterogeneity
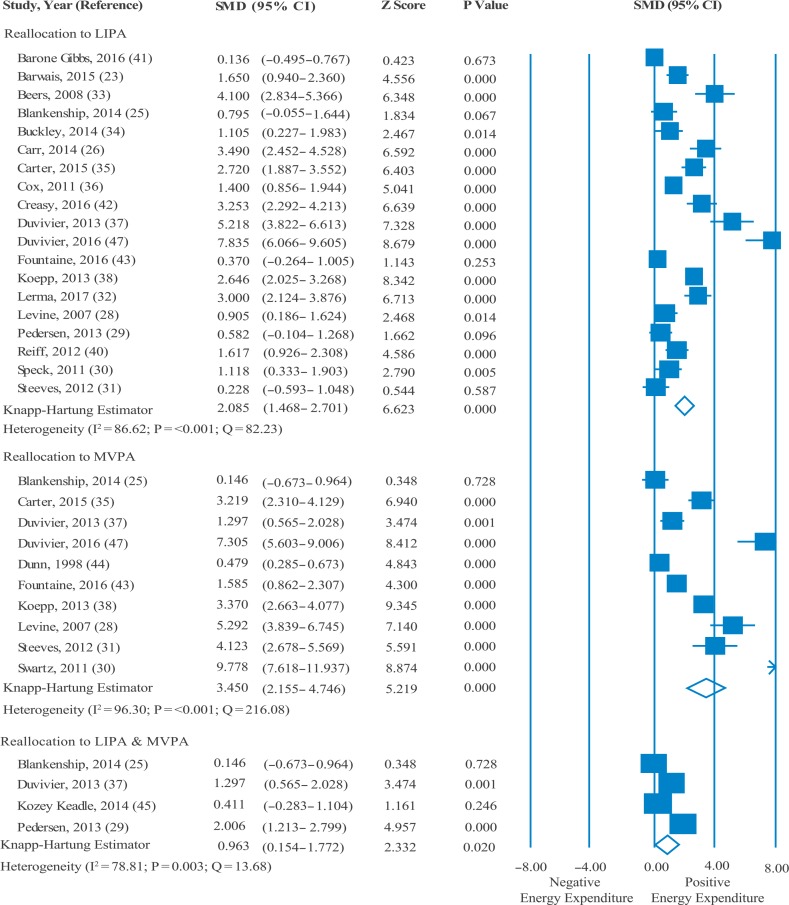
There was significant publication bias among studies utilizing LIPA (Egger’s regression intercept, 7.30 [P = 0.020]) and MVPA (Egger’s regression intercept, 6.24 [P = 0.003]), while combined LIPA and MVPA studies were found to have non-significant, moderate publication bias (Egger’s regression intercept, 4.66 [P = 0.834]). As per Higgins and Thompson’s13 classification, heterogeneity within LIPA, MVPA and LIPA and MVPA interventions was found to be high (Fig. 2).
Fig. 2.
The energy expenditure directly associated with interventions where sedentary time was reallocated to physical activity.
Effect of sedentary interventions on EE
Figure 2 describes the direct EE associated with reallocating sedentary time to varying intensities of physical activity. LIPA, MVPA and LIPA and MVPA interventions were all associated with increased EE. MVPA interventions were attributed to a larger increase in EE (pooled SMD, 3.45 [CI: 2.16–4.75]) than LIPA (pooled SMD, 2.09 [CI: 1.47–2.70]). Combined LIPA and MVPA interventions were associated with a significant but lower increase in EE (pooled SMD, 0.96 [CI: 0.15–1.77]) than LIPA and MVPA. The pooled EE estimates for the three groups did not change substantially with the exclusion of any study.
Table 1 outlines the daily cumulative EE associated with reallocating sedentary time to LIPA, MVPA and LIPA and MVPA. Reallocating 6–9 h of sedentary time to LIPA (pooled SMD, 2.509 [CI: 1.204–5.363]) had less than half of the cumulative EE than reallocating 6–9 h of sedentary time to LIPA and MVPA (pooled SMD, 5.218 [CI: 3.822–6.613]). Reallocating 1 h of sedentary time to MVPA resulted in greater cumulative EE than the reallocation of 3–5 h of LIPA and MVPA, but less EE than 6–9 h of LIPA and MVPA reallocation.
Table 1.
Estimated cumulative energy expenditure associated with reallocating sedentary time to varying intensities of physical activity in a 12-h waking day
| Total duration of physical activity time | Pooled SMD (95% CI) | P-value |
|---|---|---|
| Reallocating sedentary time to LIPA | ||
| 1–2 h26,30,31,33,35,36 | 1.974 (0.723, 3.224) | 0.01 |
| 3–5 h28,34,42,43,47,48 | 2.305 (0.153, 4.241) | 0.03 |
| 6–9 h23,29,37,40 | 2.501 (1.204, 5.363) | 0.01 |
| Reallocating sedentary time to LIPA and MVPA | ||
| 1–2 h45 | 0.411 (−0.314, 1.136) | 0.25 |
| 3–5 h48 | 0.795 (−0.055, 1.644) | 0.73 |
| 6–9 h37 | 5.218 (3.822, 6.613) | <0.001 |
| Reallocating sedentary time to MVPA | ||
| ≤30 min35,43,44 | 1.715 (−1.703, 5.133) | 0.02 |
| 1 h20,31,37,47,48 | 4.443 (3.113, 9.433) | 0.01 |
LIPA, light-intensity physical activity; MVPA, moderate-to-vigorous-intensity physical activity; SMD, standardized mean difference of estimated cumulative energy expenditure.
A subgroup analysis using meta-regression (Table 2) showed that estimates of EE significantly varied by sex for reallocation to LIPA, and MVPA; by study duration for reallocation to MVPA; and by measure of EE for reallocation to LIPA. No variations were found when comparing study quality.
Table 2.
The association between individual covariates and physical activity-related energy expenditure examined using method of moments, random-effects meta-regression
| Variable | Physical activity | Coefficient, B | 95% CI | P-value |
|---|---|---|---|---|
| Risk of bias | LIPA | −0.455 | 2.309, 1.400 | 0.63 |
| LIPA and MVPA | 1.473 | −0.703, 3.649 | 0.18 | |
| MVPA | 2.924 | −1.287, 7.135 | 0.17 | |
| Sex | LIPA | 1.124 | 0.354, 2.112 | <0.001 |
| LIPA and MVPA | 0.453 | −0.434, 1.325 | 0.12 | |
| MVPA | 2.132 | 1.623, 2.879 | <0.001 | |
| Study duration | LIPA | 2.071 | 1.403, 6.074 | <0.001 |
| LIPA and MVPA | 0.713 | −0.760, 2.186 | 0.34 | |
| MVPA | 3.980 | 2.412, 4.975 | <0.001 | |
| Measure of EE | LIPA | 5.772 | 2.914, 8.629 | <0.001 |
| LIPA and MVPA | 0.620 | −2.433, 3.673 | 0.69 | |
| MVPA | 4.920 | −1.477, 11.317 | 0.13 |
EE, energy expenditure; LIPA, light-intensity physical activity; MVPA, moderate-to-vigorous-intensity physical activity.
Discussion
Main findings of this study
Interventions reallocating sedentary time to LIPA, MVPA or LIPA and MVPA increased EE in adults. When examined over a waking day, LIPA interventions required 6–9 h of sedentary time to generate an equivalent EE of 1 h of MVPA. While combined LIPA and MVPA interventions were expected to yield the greatest cumulative EE, reported yields were found to be similar to LIPA, which may be a result of the few studies available for comparison.
What is already known on this topic
Previous reviews have largely evaluated sedentary interventions on their success in modifying sedentary time.47,48 However, changes in sedentary time might reflect an individual’s motivation in engaging in lifestyle behaviours and provides little information on an individual’s daily activity patterns. Alternatively, daily cumulative EE provides a useful measure to compare the effect of displacing sedentary time over a day. As chronic diseases can take years to develop it is difficult to mechanistically link a transition of reduced activity to actual chronic disease risk. As more clinical studies are needed to elucidate the true pathways by which sedentary behaviours affect health, various mechanisms have been postulated such as influencing markers of inflammation.49 However, a comparison by EE offers a plausible outcome to interpret musculoskeletal contractions when breaking up sedentary time that evidence has shown can have an important role in modifying adiposity, insulin resistance and other disease risk markers.50,51
What this study adds
This review highlights the significance of focusing on increasing MVPA, particularly when transitioning between sedentary states and LIPA (in the form of bouts over the course of a day) can be difficult to adhere to. While Prince and colleagues had found MVPA interventions to be less effective at reducing sedentary time than interventions focused on sedentary time avoidance, they also found that MVPA was a more likely target for sedentary time reallocation.47 MVPA promotion has largely involved the targeting of controlled motivational processes such as intentions or self-efficacy, and engaging in sedentary behaviours are due to unconscious habits formed by environmental and behavioural cues.52 Increasing physical activity at any intensity is challenging with respect to physical and cognitive effort, and despite continuing efforts to increase MVPA and more recently LIPA levels, the global prevalence of populations achieving recommended MVPA and sedentary time levels remains suboptimal.53,54 As such, more research is still needed in order to learn how best to engage more individuals in regular MVPA and to overcome the subconscious decisions that lead to sedentary behaviours. The effort and burden required to combine both spectrums of physical activity may partly explain the lower direct EE found in the few studies that evaluated combined LIPA and MVPA interventions. Interventions seeking to reallocate time to MVPA or LIPA may require separate and distinctive behavioural strategies in order for participants to adhere to them.
This review has important public health and research implications. It is expected that replacing sedentary time with short periods of MVPA and frequent intervals of LIPA will yield the greatest cumulative EE. However, such interventions can be the most challenging to maintain as increasing activity participation poses many barriers to adherence such as motivation, cost, time and a built environment that may not always be facilitative.55 Thus, successful interventions are likely to be personalized to the individual. We found that similar EE can be achieved by different strategies, and a singular focus on promoting MVPA might be effective for individuals for whom a combined co-intervention has proven to be a challenge. Furthermore, being adherent to MVPA alone confers important health benefits, including cardiopulmonary fitness which is one of the most important modifiable prognostic determinants of health.56,57 In contrast, those unable to meet MVPA recommendations, older individuals and those with mobility limitations who are among the most sedentary and physically inactive populations, may benefit greatly from the lower workload and effort required to perform LIPA. As research in this area continues to progress, a focus on evaluating the feasibility of implementing MVPA and LIPA co-interventions can be an important step in reducing the health risks of sedentary behaviour and physical inactivity. However, the controlled conditions in which the majority of the reviewed interventions have been designed (such as randomized controlled/crossover trials) may not sufficiently determine the practicality of such interventions over an individual’s typical day and in the long-term. As such, high-quality intervention studies that determine the outcome benefits and behavioural preferences for individuals in their natural environment are necessary.
Limitations of this study
Some limitations should be considered when interpreting these findings. First, associations with specific health outcomes were not assessed given the challenges of attributing changes to sedentary behaviours. Nonetheless, our findings are consistent with a recent harmonized meta-analysis attributing increases in MVPA with reduced mortality risk.58 Second, cumulative estimates for combined LIPA and MVPA interventions were based on single study estimates and are likely to be imprecise. As advocacy towards combining exercise with LIPA builds,59 it is hoped that these estimates can be better refined with greater study of the effectiveness of combined interventions. Third, we found several studies had examined EE within short follow-up durations. While it would be ideal to compare all interventions by their cumulative effects over a day or in natural conditions, protocol-driven and controlled assessments are likely to generalize hourly and cumulative EE.20 Fourth, we did not further categorize EE differences between standing and low-pace walking as they were both within the commonly accepted operational definition of LIPA. Therefore, differences in cumulative EE may be attributed to activity type. As both standing and low-pace walking are likely to require different behaviours and yield different amounts of energy expended, further analysis across forms of LIPA is required. Fifth, as our meta-regression found and other reviews have reported,47,48,60 the large degree of study heterogeneity in the quantitative analysis may be attributed to the small sample sizes, study-by-study differences by sex, study duration and outcome measurement among the interventions reviewed. Such heterogeneity, while limiting interpretability, also reveals the need for better-designed interventional studies that clearly elucidate the effectiveness of sedentary behaviour interventions.
In conclusion, while a combination of LIPA and MVPA are expected to produce the greatest cumulative EE benefits in adults, our systematic review suggests that similar EE can be achieved by reallocating sedentary time to MVPA over a shorter duration of time. These findings reaffirm the need for individualized interventions and provide reassurance that similar EE can be achieved through different intervention strategies.
Supplementary Material
Acknowledgements
No further acknowledgements.
Supplementary data
Supplementary data are available at Journal of Public Health online.
Funding
This work was not supported by any specific grant from a funding agency in the public, commercial or not-for-profit sectors. AB is supported by a fellowship from the Institute for Work and Health. DAA is supported by a Chair in Cardiac Rehabilitation at the University Health Network-Toronto Rehabilitation Institute, and a Career Investigator Award from the Heart and Stroke Foundation of Canada. GEF is supported with a Canadian Institutes of Health Research-Public Health Agency of Canada (CIHR- PHAC) Chair in Applied Public Health. PIO is supported with a Goodlife Fitness Chair in Cardiovascular Rehabilitation and Prevention, University Health Network-Toronto Rehabilitation Institute.
Conflicts of interest
No potential conflicts of interest to disclose by any of the authors.
References
- 1. Barnes J, Behrens TK, Benden ME et al. . Letter to the Editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab 2012;37(3):540–2. [DOI] [PubMed] [Google Scholar]
- 2. Matthews CE, Chen KY, Freedson PS et al. . Amount of time spent in sedentary behaviors in the United States, 2003–04. Am J Epidemiol 2008;167(7):875–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Biswas A, Oh P, Faulkner G et al. . Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Ann Intern Med 2015;162(2):123–32. [DOI] [PubMed] [Google Scholar]
- 4. Dempsey PC, Owen N, Biddle SJ et al. . Managing sedentary behavior to reduce the risk of diabetes and cardiovascular disease. Curr Diab Rep 2014;14(9):1–11. [DOI] [PubMed] [Google Scholar]
- 5. Hamilton M, Healy G, Dunstan D et al. . Too little exercise and too much sitting: inactivity physiology and the need for new recommendations on sedentary behavior. Curr Cardiovasc Risk Rep 2008;2(4):292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. ACSM ACSM’s Guidelines for Exercise Testing and Prescription. Lippincott Williams & Wilkins; 2013.
- 7. Buman MP, Winkler EA, Kurka JM et al. . Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005–06. Am J Epidemiol 2013;179(3):323–34. [DOI] [PubMed] [Google Scholar]
- 8. Stamatakis E, Rogers K, Ding D et al. . All-cause mortality effects of replacing sedentary time with physical activity and sleeping using an isotemporal substitution model: a prospective study of 201,129 mid-aged and older adults. Int J Behav Nutr Phys Act 2015;12(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moher D, Liberati A, Tetzlaff J et al. . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151(4):264–9. [DOI] [PubMed] [Google Scholar]
- 10. Tremblay MS, Colley RC, Saunders TJ et al. . Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab 2010;35(6):725–40. [DOI] [PubMed] [Google Scholar]
- 11. Ainsworth BE, Haskell WL, Herrmann SD et al. . 2011 compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 2011;43(8):1575–81. [DOI] [PubMed] [Google Scholar]
- 12. NHLBI Development and Use of Quality Assessment Tools [cited 2016 April 2016]. http://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/background.htm.
- 13. Higgins J, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Stat Med 2002;21(11):1539–58. [DOI] [PubMed] [Google Scholar]
- 14. Knapp G, Hartung J. Improved tests for a random effects meta‐regression with a single covariate. Stat Med 2003;22(17):2693–710. [DOI] [PubMed] [Google Scholar]
- 15. Egger M, Smith GD, Schneider M et al. . Bias in meta-analysis detected by a simple, graphical test. Br Med J 1997;315(7109):629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Borenstein MHL, Higgins J, Rothstein H. Comprehensive Meta-Analysis Version 2. Englewood NJ: Biostat, 2005. [Google Scholar]
- 17. R Development Core Team R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing, 2012. [Google Scholar]
- 18. Swartz AM, Squires L, Strath SJ. Energy expenditure of interruptions to sedentary behavior. Int J Behav Nutr Phys Act 2011;8:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Reilly JJ, Kelly LA, Montgomery C et al. . Validation of Actigraph accelerometer estimates of total energy expenditure in young children. Int J Pediatr Obes 2006;1(3):161–7. [DOI] [PubMed] [Google Scholar]
- 20. Thompson SG, Higgins J. How should meta‐regression analyses be undertaken and interpreted? Stat Med 2002;21(11):1559–73. [DOI] [PubMed] [Google Scholar]
- 21. Barwais F, Cuddihy T. Empowering sedentary adults to reduce sedentary behaviour: success with a technology-based physical activity monitor. J Sci Med Sport 2014;18:e67. [Google Scholar]
- 22. Ben-Ner A, Hamann DJ, Koepp G et al. . Treadmill workstations: the effects of walking while working on physical activity and work performance. PLoS One 2014;9(2):e88620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Blankenship JM, Granados K, Braun B. Effects of subtracting sitting versus adding exercise on glycemic control and variability in sedentary office workers. Appl Physiol Nutr Metab 2014;39(11):1286–93. [DOI] [PubMed] [Google Scholar]
- 24. Carr LJ, Maeda H, Luther B et al. . Acceptability and effects of a seated active workstation during sedentary work: a proof of concept study. Int J Workplace Health Manag 2014;7(1):2–15. [Google Scholar]
- 25. Dewa CS, de Ruiter W, Chau N et al. . Walking for wellness: using pedometers to decrease sedentary behaviour and promote mental health. Int J Ment Health Promot 2009;11(2):24–8. [Google Scholar]
- 26. Levine JA, Miller JM. The energy expenditure of using a ‘walk-and-work’ desk for office workers with obesity. Br J Sports Med 2007;41(9):558–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pedersen SJ, Cooley PD, Mainsbridge C. An e-health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work 2014;49(2):289–95. [DOI] [PubMed] [Google Scholar]
- 28. Speck RM, Schmitz KH. Energy expenditure comparison: a pilot study of standing instead of sitting at work for obesity prevention. Prev Med 2011;52(3):283–4. [DOI] [PubMed] [Google Scholar]
- 29. Steeves JA, Thompson DL, Bassett DR Jr et al. . Energy cost of stepping in place while watching television commercials. Med Sci Sports Exerc 2012;44(2):330–5. [DOI] [PubMed] [Google Scholar]
- 30. Lerma NL, Swartz AM, Rowley TW et al. . Increasing the energy expenditure of seated activities in older adults with a portable elliptical device. J Aging Phys Act 2016;25(1):99–104. [DOI] [PubMed] [Google Scholar]
- 31. Beers EA, Roemmich JN, Epstein LH et al. . Increasing passive energy expenditure during clerical work. Eur J Appl Physiol 2008;103(3):353–60. [DOI] [PubMed] [Google Scholar]
- 32. Buckley JP, Mellor DD, Morris M et al. . Standing-based office work shows encouraging signs of attenuating post-prandial glycaemic excursion. Occup Environ Med 2013;71(2):109–11. [DOI] [PubMed] [Google Scholar]
- 33. Carter SE, Jones M, Gladwell VF. Energy expenditure and heart rate response to breaking up sedentary time with three different physical activity interventions. Nutr Metab Cardiovasc Dis 2015;25(5):503–9. [DOI] [PubMed] [Google Scholar]
- 34. Cox RH, Guth J, Siekemeyer L et al. . Metabolic cost and speech quality while using an active workstation. J Phys Act Health 2011;8(3):332–9. [DOI] [PubMed] [Google Scholar]
- 35. Duvivier BMFM, Schaper NC, Bremers MA et al. . Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS One 2013;8(2):e55542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Koepp GA, Manohar CU, McCrady-Spitzer SK et al. . Treadmill desks: a 1-year prospective trial. J Obes 2013;21(4):705–11. [DOI] [PubMed] [Google Scholar]
- 37. Lopez-Fontana CM, Sanchez-Villegas A, Martinez-Gonzalez MA et al. . Daily physical activity and macronutrient distribution of low-calorie diets jointly affect body fat reduction in obese women. Appl Physiol Nutr Metab 2009;34(4):595–602. [DOI] [PubMed] [Google Scholar]
- 38. Reiff C, Marlatt K, Dengel DR. Difference in caloric expenditure in sitting versus standing desks. J Phys Act Health 2012;9(7):1009. [DOI] [PubMed] [Google Scholar]
- 39. Gibbs BB, Kowalsky R, Perdomo S et al. . Energy expenditure of deskwork when sitting, standing or alternating positions. Occup Med 2016;67(2):121–7. [DOI] [PubMed] [Google Scholar]
- 40. Creasy SA, Rogers RJ, Byard TD et al. . Energy expenditure during acute periods of sitting, standing, and walking. J Phys Act Health 2016;13(6):573–8. [DOI] [PubMed] [Google Scholar]
- 41. Fountaine CJ, Johann J, Skalko C et al. . Metabolic and energy cost of sitting, standing, and a novel sitting/stepping protocol in recreationally active college students. Int J Exerc Sci 2016;9(2):223. [PMC free article] [PubMed] [Google Scholar]
- 42. Dunn AL, Marcus BH, Kampert JB et al. . Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. J Am Med Assoc 1999;281(4):327–34. [DOI] [PubMed] [Google Scholar]
- 43. Kozey Keadle S, Lyden K, Staudenmayer J et al. . The independent and combined effects of exercise training and reducing sedentary behavior on cardiometabolic risk factors. Appl Physiol Nutr Metab 2014;39(7):770–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Rose-Peddie M, Bone J, Rehrer N et al. . Breaking prolonged sitting reduces postprandial glycemia & insulinemia in healthy adults. Med J Aust 2011;4(12):808. [Google Scholar]
- 45. Duvivier BM, Schaper NC, Hesselink MK et al. . Breaking sitting with light activities vs structured exercise: a randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia 2016;60(3):490–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Blankenship JM, Granados K, Braun B. Effects of subtracting sitting versus adding exercise on glycemic control and variability in sedentary office workers. Appl Physiol Nutr Metab 2014;39(11):1286–93. [DOI] [PubMed] [Google Scholar]
- 47. Prince S, Saunders T, Gresty K et al. . A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta‐analysis of controlled trials. Obes Rev 2014;15(11):905–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Martin A, Fitzsimons C, Jepson R et al. . Interventions with potential to reduce sedentary time in adults: systematic review and meta-analysis. Br J Sports Med 2015;49(16):1056–63. [DOI] [PubMed] [Google Scholar]
- 49. Henson J, Yates T, Edwardson CL et al. . Sedentary time and markers of chronic low-grade inflammation in a high risk population. PLoS One 2013;8(10):e78350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bergouignan A, Latouche C, Heywood S et al. . Frequent interruptions of sedentary time modulates contraction-and insulin-stimulated glucose uptake pathways in muscle: ancillary analysis from randomized clinical trials. Sci Rep 2016;6(32044):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lynch BM. Sedentary behavior and cancer: a systematic review of the literature and proposed biological mechanisms. Cancer Epidemiol Biomarkers Prev 2010;19(11):2691–709. [DOI] [PubMed] [Google Scholar]
- 52. Maher JP, Conroy DE. A dual-process model of older adults’ sedentary behavior. Health Psychol 2016;35(3):262. [DOI] [PubMed] [Google Scholar]
- 53. Colley R, Garriguet D, Janssen I et al. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009. Canadian Health Measures Survey. Statistics Canada Ottawa; 2011. [PubMed]
- 54. Troiano RP, Berrigan D, Dodd KW et al. . Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008;40(1):181–8. [DOI] [PubMed] [Google Scholar]
- 55. Owen N, Leslie E, Salmon J et al. . Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci 2000;28(4):153–8. [PubMed] [Google Scholar]
- 56. Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. Can Med Assoc J 2006;174(6):801–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Myers J. Exercise and cardiovascular health. Circulation 2003;107(1):e2–5. [DOI] [PubMed] [Google Scholar]
- 58. Ekelund U, Steene-Johannessen J, Brown WJ et al. . Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388(10051):1302–10. [DOI] [PubMed] [Google Scholar]
- 59. Franklin BA, Brinks J, Sternburgh L. Move more, sit less: a first‐line, public health preventive strategy? Prev Cardiol 2010;13(4):203–8. [DOI] [PubMed] [Google Scholar]
- 60. Shrestha N, Kukkonen-Harjula KT, Verbeek JH et al. Workplace interventions for reducing sitting at work. The Cochrane Library; 2016. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.