Abstract
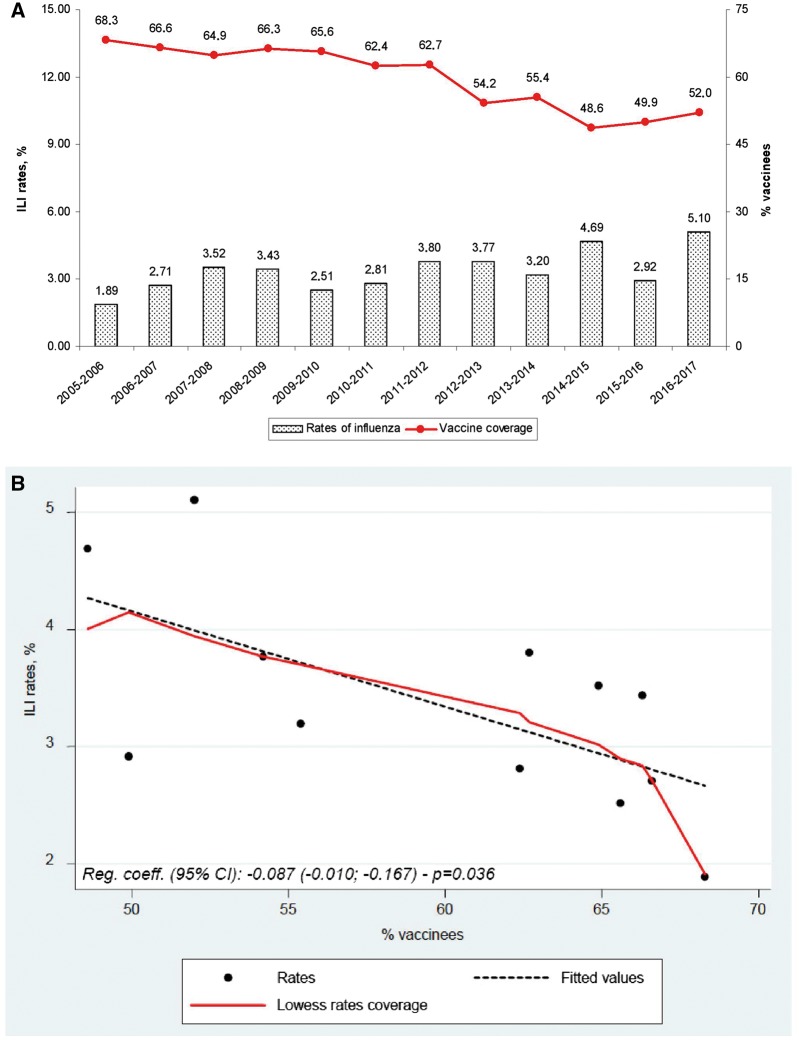
After a peak of 68.3% during the 2005–06 season, influenza vaccine coverage among Italian elderly showed an unprecedented, prolonged decline. According to the National surveillance network, the vaccination coverage was ≤50% during two of the last three seasons (2014–17). In parallel, influenza-like illness (ILI) rates increased from 2.71% in the triennium 2005–08, to 4.24% in the last triennium. A significant association was found between ILI rise and vaccine coverage decline (P = 0.036), and according to a conservative estimation, each 1% increase in coverage may prevent ≥2690 ILI cases among the elderly. A reinforcement of influenza immunization policies is strongly needed in Italy.
Introduction
As a crucial instrument to control epidemics,1 influenza vaccination is recommended for the elderly in all European countries since decades.2 In Italy, the vaccine coverage showed a prolonged ascending trend, up to 68.7% during the years 2005–06. After that season, the proportion of vaccinated elderly continuously decreased, falling below 50% during two of the last three seasons.3
A few studies evaluated the relationship between vaccine coverage and influenza-like illness (ILI) incidence using large, real-world datasets, and all analyses were performed in countries with increasing coverage trend.4–7 We analysed the potential association between vaccine coverage and attack rates among the elderly during a wide, protracted decline, which represents a unique scenario among high-income European countries.
Methods
We correlated vaccine coverage and influenza incidence in the 12 influenza seasons following the peak in 2005–06, up to the last available data (2016–17). The information on vaccine coverage and ILI incidence among Italian elderly (≥65 years) were extracted from the official online databases of the Italian Ministry of Health and National Institute of Health, respectively (www.iss.it/flue/index.php).3 The National vaccine coverage is collected annually from the Regions, while ILI attack rates are collected from ≈1200 general practitioners (in charge of ≈2% of the Italian population) by the Influenza epidemiological and virological surveillance Network (InfluNet). Attack rates are reported weekly during the 28-week typical influenza season, and have been combined to obtain the overall ILI incidence for each season (dividing the total number of cases by the mean number of elderly observed per week—Supplementary Material). Using these data, we provided quantitative estimates of the decrease in influenza cases following a hypothetical 1% increase in vaccine coverage, and assuming an overall vaccine effectiveness of 50%.1
A scatter plot was used to display the proportion of vaccinated elderly vs. ILI attack rates, and a locally weighted scatter-plot smoother (LOWESS) curve was built to capture the potential nonlinearities of the relationship. The potential association between the two variables was initially evaluated using Spearman correlation coefficient, then fitting a multivariate regression adjusted for vaccine match.6 Matching information were extracted from WHO and CDC websites, and defined according to WHO criteria (Supplementary Material for web-links and specifications). All analyses were performed using Stata 13.1.
Results
A mean of 260 407 elderly (min. 214, 420; max. 322, 071) were included in the Italian surveillance system during the 28-week influenza seasons 2005–17 (Supplementary Material). Of them, an average of 8838 experienced a case of ILI, corresponding to a mean annual rate of 3.39%.
After the peak of 68.3% in 2005–06, the vaccination coverage decreased up to a minimum of 48.6% during the season 2014–15 (−28.8%; Figure 1A), slightly rising to 52.0% in the last observed season (2016–17). In absolute terms, if the latter values are applied to the entire Italian population, the overall number of Italian vaccinated elderly decreased from ≈9 240 000 to ≈7 035 000, with more than 2.2 million citizens left uncovered.
Figure 1.
(A) Rates of influenza and percentage of vaccine coverage among Italian elderly during influenza seasons 2005–17 (sources: Italian National Institute of Health and Ministry of Health) (B) Scatter-plot (and regression lines) of the overall influenza rates among Italian elderly during influenza seasons 2005–17 vs. the percentage of elderly that were vaccinated for influenza
ILI attack rate typically varies across seasons, depending on virus characteristics and vaccine matching (6). The highest rates were however observed during two of the last three seasons (Figure 1A), and the average rate of the last 6 years (3.91%) was significantly higher than that of the first (2.81%).
Both Spearman test and multivariate regression showed a significant, inverse association between vaccine coverage and ILI rates (both P < 0.05; regression coefficient −0.087; 95% CI: −0.010; −0.167; Figure 1B). In addition, despite the wide variability of seasonal ILI rates, the relationship between ILI rates and vaccine coverage was quite linear (as shown by LOWESS curve in Figure 1B).
Discussion
In the last decade, Italy has faced a decline in the coverage for all vaccines at all age-groups, with most regions falling below the targets established by the Ministry of Health.3 The drop was so substantial to propel a major change in the National immunization strategy, which increased the number of vaccines mandatory for all infants from four to ten, and established a set of actions to reinforce immunization campaigns and awareness.8
Potential explanations that have been proposed for the increased vaccine hesitancy are the underestimation of infection-related severe harms by physicians, and an increased perception of vaccines risks by the general population,9 which was fueled by the growing use of the web and mass-media by anti-vaccination movements.10 In addition, influenza vaccination was particularly penalized as a consequence of two events: first, the termination of dedicated incentives to general practitioners in several regions in 2013 (when the largest drop was registered)11; second, a widespread mass-media alert during the 2014 season, when a causal relationship between three post-vaccination deaths was initially claimed, and only 2 weeks later disproved.10 Indeed, during these 2 weeks, the uptake of influenza vaccination dropped by 80% (10).
Clearly, the scientific community warned that a loss of public confidence in vaccination would have had detrimental consequences on vaccines uptake, especially among high-risk subjects.9 Indeed, three of the four analyses published to date found a significant correlation between increasing vaccine coverage and descending ILI rates,4–6 and the fourth study still achieved significance when the analyses were restricted to the seasons with A(H3) dominant virus subtype (7).
Although a rise in influenza incidence was thus expected, no quantitative analyses were available from countries with a descending coverage, and no estimates of the amount of additional ILI were thus possible. Our data substantially confirm previous findings, showing a strong correlation between the decrease in vaccine coverage and the rise in ILI rates among Italian elderly, and provide a basis for the quantification of the harms of vaccine hesitancy.
Although the estimation of how many ILI cases would be prevented with increasing vaccination coverage remains complex, given the relatively scarce number of seasons available for statistical modeling, and the variability in seasonal ILI attack rates, even an approximate, conservative quantification may help the discussion among all stakeholders on the strategies to reduce vaccine hesitancy. Conservatively assuming an average ILI rate of 3.0%, and a vaccine effectiveness of 50%,1 since the proportion of vaccinated subjects was close to 50% in the last biennium, we may hypothesize that the overall incidence among vaccinated and unvaccinated elderly were 2.0 and 4.0%, respectively. Thus, increasing the coverage by 1%, which equals to vaccinating 134 492 more elderly (computed from the mean population of the last biennium—source: National Institute for Statistics), would imply a reduction of influenza incidence from 4.0% (n = 5380)—2.0%, preventing a total of 2690 ILI cases. This count is almost certainly underestimated, as both attack rates and vaccine effectiveness are usually higher,1 and herd immunity has not been considered. It can be affirmed, however, that no less than one influenza case would be prevented if 50 more elderly are vaccinated.
With some limitations to consider (a relatively short time span, the use of ILI as a proxy of laboratory-confirmed influenza cases, and the potential impact of other external factors such as viral pathogenicity), our findings provides evidence of the negative consequences of the decline in influenza vaccination rates among the elderly, supporting a reinforcement of immunization policies and their inclusion among the priorities of the public health agenda.
Supplementary data
Supplementary data are available at EURPUB online.
Conflicts of interest: G.G. received grants from GSK Biologicals SA, SPMSD, Novartis, Crucell/Janssen, Sequirus and Pfizer as consultant, advisory board member, expert, speaker, organizer of congresses/conferences or as investigator in clinical trials.
Key points
After a peak of 68.3% during the 2005–06 season, influenza vaccine coverage among Italian elderly showed an unprecedented decline, falling below 50% during two of the last three seasons.
All previous studies evaluating the relationship between vaccine coverage and influenza-like illness (ILI) were performed in countries with an increasing coverage trend.
This study investigates the potential association between vaccine coverage and attack rates among the elderly during a protracted decline, which represents a unique scenario among high-income European countries.
A significant, inverse correlation between the decline in vaccine coverage and the rise in ILI attack rates was found, providing quantitative evidence of the negative consequences of vaccination hesitancy among the elderly.
Further efforts are needed to increase influenza vaccine acceptance and uptake among Italian elderly, together with a reinforcement of the immunization policies.
Supplementary Material
References
- 1. Manzoli L, Ioannidis JP, Flacco ME, et al. Effectiveness and harms of seasonal and pandemic influenza vaccines in children, adults and elderly: a critical review and re-analysis of 15 meta-analyses. Hum Vaccin Immunother 2012; 8:851–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Rizzo C, Rezza G, Ricciardi W. Strategies in recommending influenza vaccination in Europe and US. Hum Vaccin Immunother 2017, 1–6, doi: 10.1080/21645515.2017.1367463 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Italian Ministry of Health. Influenza. Dati coperture vaccinali [Influenza vaccination coverage data] 2016 [September 2017]. Available at: http://www.salute.gov.it/portale/influenza/dettaglioContenutiInfluenza.jsp? lingua=italiano&id=679&area=influenza&menu=vuoto (17 March 2018, date last accessed).
- 4. Dijkstra F, Donker GA, Wilbrink B, et al. Long time trends in influenza-like illness and associated determinants in The Netherlands. Epidemiol Infect 2009; 137:473–9. [DOI] [PubMed] [Google Scholar]
- 5. Huang QS, Lopez LD, McCallum L, Adlam B. Influenza surveillance and immunisation in New Zealand, 1997-2006. Influenza. Other Respir Viruses 2008; 2:139–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Spruijt IT, de Lange MM, Dijkstra F, et al. Long-term correlation between influenza vaccination coverage and incidence of influenza-like illness in 14 European countries. PLoS One 2016; 11:e0163508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nunes B, Falcao I, Machado A, et al. Influenza vaccine coverage and the attack rate of influenza-like illness among the elderly in Portugal: is there a correlation? Euro Surveill 2007; 12:E070517 2. [DOI] [PubMed] [Google Scholar]
- 8. Signorelli C, Guerra R, Siliquini R, Ricciardi W. Italy’s response to vaccine hesitancy: an innovative and cost effective National Immunization Plan based on scientific evidence. Vaccine 2017; 35:4057–9. [DOI] [PubMed] [Google Scholar]
- 9. Larson HJ, Cooper LZ, Eskola J, et al. Addressing the vaccine confidence gap. Lancet 2011; 378:526–35. [DOI] [PubMed] [Google Scholar]
- 10. Signorelli C, Odone A, Conversano M, Bonanni P. Deaths after Fluad flu vaccine and the epidemic of panic in Italy. BMJ 2015; 350:h116. [DOI] [PubMed] [Google Scholar]
- 11. Odone A, Fara GM, Giammaco G, et al. The future of immunization policies in Italy and in the European Union: the Declaration of Erice. Hum Vaccin Immunother 2015; 11:1268–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.