Abstract
Community–academic research partnerships aim to build stakeholder trust in order to improve the reach and translation of health research, but there is limited empirical research regarding effective ways to build trust. This multisite study was launched to identify similarities and differences among stakeholders’ perspectives of antecedents to trust in research partnerships. In 2013–2014, we conducted a mixed-methods concept mapping study with participants from three major stakeholder groups who identified and rated the importance of different antecedents of trust on a 5-point Likert-type scale. Study participants were community members (n = 66), health care providers (n = 38), and academic researchers (n = 44). All stakeholder groups rated “authentic communication” and “reciprocal relationships” the highest in importance. Community members rated “communication/methodology to resolve problems” (M = 4.23, SD = 0.58) significantly higher than academic researchers (M = 3.87, SD = 0.67) and health care providers (M = 3.89, SD = 0.62; p < .01) and had different perspectives regarding the importance of issues related to “sustainability.” The importance of communication and relationships across stakeholders indicates the importance of colearning processes that involve the exchange of knowledge and skills. The differences uncovered suggest specific areas where attention and skill building may be needed to improve trust within partnerships. More research on how partnerships can improve communication specific to problem solving and sustainability is merited.
Keywords: collaboration, community-based participatory research, translational research, trust
Community–academic research partnerships are recommended for addressing a wide spectrum of health issues (Boutin-Foster et al., 2008; Carney, Maltby, Mackin, & Maksym, 2011; Lesser & Oscós-Sánchez, 2007; Masuda, Creighton, Nixon, & Frankish, 2011). These partnerships engage multiple stakeholder groups in research that aims to combine knowledge and action to achieve sustainable social change (Israel, Schulz, & Parker, 2005; Lesser & Oscós-Sánchez, 2007). Stakeholders in these partnerships note that trust is a critical factor for efficient collaboration and achievement of desired outcomes (Dalal, Skeete, Yeo, Lucas, & Rosenthal, 2009; Minkler, 2005; Parrill & Kennedy, 2011; Pivik & Goelman, 2011; Plowfield, Wheeler, & Raymond, 2005; Strand, Marullo, Cutforth, Stoecker, & Donohue, 2003; Suarez-Balcazar, Harper, & Lewis, 2005), yet there is little empirical research on the conceptualization of factors that promote trust within research partnerships.
Trust is a complex and multidimensional phenomenon (Khodyakov, 2007; Lewicki & Wiethoff, 2000; Lewis & Weigert, 2012). It has a context-specific cognitive dimension (i.e., we have beliefs and make decisions about who to trust and when; Khodyakov, 2007). For example, the specific actions that individuals believe contribute to trust in the context of business relationships are different from those in the context of personal relationships (Lewicki, Tomlinson, & Gillespie, 2006). Research needs to consider cognitive dimensions of trust, such as stakeholder opinions and thoughts about the antecedents of trust within the specific context of research partnerships.
Trust is bidirectional—a result of interaction between individuals, groups of individuals, and/or institutions. It involves a level of vulnerability for at least one of the parties involved (Deutsch, 1958). In many relationships, trust is perceived differently among the involved parties due to imbalanced levels of vulnerability. For example, compared to physicians, patients likely feel a greater need for trust-building processes since they experience a higher level of vulnerability and dependence on physicians for their personal health (Hall, Dugan, Zheng, & Mishra, 2001). There are likely complex differences in vulnerability among stakeholders involved in community–academic research partnerships. For example, community partners may feel vulnerable due to reliance on academic partner’s research funding for employment, and academic partners may feel vulnerable due to reliance on community partners to recruit research participants.
In community–academic research partnerships, there are often challenging power differentials between stakeholders who come from a wide range of socioeconomic and cultural backgrounds and frequently have divergent priorities and goals (Minkler, 2005). Developing trust is noted as an important factor to overcome power differentials (Brush, Baiardi, & Lapides, 2011; Cargo et al., 2008; Dalal et al., 2009; Gilbert, Quinn, Ford, & Thomas, 2010; Lowe, Riggs, & Henson, 2011; Merzel et al., 2007; Moreno, Rodríguez, Lopez, Bholat, & Dowling, 2009; Norris et al., 2007; Parrill & Kennedy, 2011; Wolff & Maurana, 2001); however, to date, there is limited empirical investigation of how diverse stakeholders differ in the perceived importance of potential contributors to trust.
We conducted a multisite concept mapping study to identify the major antecedents of trust within research partnerships (Frerichs et al., 2015). The aim of this article was to identify similarities and differences between stakeholder groups’ perspectives regarding the importance of these antecedents in order to generate new insight about what contributes to creating and maintaining trust in research partnerships. Stakeholder perspectives studied included community members, health care providers, and academic researchers. Specifically, among stakeholder groups, we aimed to (1) compare and contrast the relative level of importance placed on antecedents of trust, (2) identify if there were absolute differences in the level of importance placed on the antecedents, and (3) assess congruence and disagreement in the level of importance placed on specific statements related to each antecedent.
Method
Setting
The study was conducted from 2013 to 2014 with Community Engagement programs at four Clinical and Translational Science Award (CTSA) Institutes: the University of North Carolina at Chapel Hill, University of Florida, University of Arkansas, and University of California at Los Angeles. The University of Pittsburgh CTSA served as the coordinating data center. The study was reviewed and approved by the institutional review boards at each site.
Sampling and Participants
Four CTSA sites recruited participants from three major stakeholder groups: (1) community members, (2) health care providers (clinicians and lay health professionals with primary employment in nonacademic settings), and (3) academic researchers (individuals with research or clinical degrees with primary employment in academic settings). Each CTSA site used respondent-driven and snowball sampling methods to identify participants through existing research network contact lists and participant pools that corresponded to each stakeholder group. Health care providers and academic researchers who self-identified as having at least some experience conducting community-engaged research and community members with varying levels of community-engaged research experience were included.
Concept Mapping Procedures
Concept mapping is a mixed-methods and participatory research method used to solicit, structure, and prioritize ideas (Kane & Trochim, 2007) that has been applied to health research to understand a range of topics, including minority participation in health research (Robinson & Trochim, 2007) and health disparities (Risisky et al., 2008). For our study, research teams comprising community and academic researchers at each CTSA conducted three activities: brainstorming, sorting and rating, and interpretation sessions (Kane & Trochim, 2007). Each site conducted a brainstorming session with each stakeholder group separately to generate lists of statements (e.g., activities, concepts) participants viewed as contributing to trust in research partnerships (125 unique statements were generated). Next, during sorting and rating sessions, all participants independently sorted the statements into piles based on how they perceived the items related to each other. The sorted data was analyzed using multidimensional scaling analyses (Kane & Trochim, 2007), which resulted in the identification of five main trust antecedents (i.e., clusters of statements). The participants also completed either online or paper-based surveys (the method varied by site) to rate each of the 125 statements by importance. During interpretation sessions (held by stakeholder group at each site), participants labeled the antecedents through a consensus-building and voting process. Specifically, participants in each session reviewed the statements for the five clusters of trust antecedents, brainstormed labels in small groups, and then discussed potential labels amongst the whole group to reach a consensus. Each site submitted their proposed labels to the data coordinating center, who compiled and removed duplicate labels, which were then submitted to research teams at each CTSA site for final voting. The final labels were (1) communication, credibility, and methodology to anticipate and resolve problems (27 statements; e.g., “memorandums of understanding outlining roles, responsibilities, data sharing/ownership . . .”); (2) authentic, effective, and transparent communication (37 statements; e.g., “honesty and full disclosure”); (3) mutually respectful and reciprocal relationships (31 statements; e.g., “assuring a mutual “win” for all at the table”); (4) committed partnerships (17 statements; e.g., “institutional concern for greater community”); and (5) sustainability (13 statements; e.g., “availability of funding”). A list of all statements by antecedent can be found in the online supplemental materials.
Measures
Importance Rating
To measure perceived level of importance of each of the 125 statements, participants were provided the following prompts, “How important is each item for creating trust between community and academic partners in research?” and “How important is each item for maintaining trust . . .?” with 5-point Likert-type scale response options (1 = not at all important, 5 = extremely important).
Analysis
We conducted analysis in Concept Systems Global Max (Concept Systems, Inc, Ithaca, NY) and SAS 9.4 (SAS Institute, Cary, NC). We used two analysis functions in Concept Systems Global Max: pattern matching and go-zones (Kane & Trochim, 2007), and conducted additional analyses in SAS 9.4.
First, we used adapted pattern matching (Kane & Trochim, 2007). The analysis results in graphs that qualitatively illustrate the relative level (or ranking) of trust antecedents between participants. To create our graphs, we calculated the stakeholder groups’ mean ratings of each antecedent (Kane & Trochim, 2007; Robinson & Trochim, 2007), which were placed on separate vertical axes of the graphs. Analysis of variance (ANOVA) determined if a stakeholder group’s mean importance ratings of the five antecedents were significantly different from each other (e.g., within the community member stakeholder group, were there statistically significant differences between how they rated each of the five antecedents). The Bonferonni procedure was used for post hoc comparisons between each pair of the five antecedents.
We conducted ANOVA for each of the five antecedents to assess significant differences in stakeholder group’s absolute mean importance ratings (i.e., across the stakeholder groups, were there statistically significant differences between their ratings of the same antecedents). The Bonferonni procedure was used for post hoc comparisons between each pair of stakeholder groups.
Finally, we used modified go-zones (Kane & Trochim, 2007) to identify which trust antecedents had the greatest congruence and disagreement between stakeholder groups in importance ratings of the antecedents’ individual statements. This allowed us to identify if there were differences potentially masked by the Aims 1 and 2 analyses due to the use of ratings averaged across statements (e.g., the average rating of the 13 statements of “sustainability” may appear similar between two stakeholder groups; however, each stakeholder group could potentially rate different statements related to sustainability with higher/lower importance). For each antecedent and between each pair of stakeholder groups, go-zones categorized importance ratings of individual statements into four categories: (1) high by both stakeholder groups, (2) low by both stakeholder groups, (3) high by the first and low by the second stakeholder group, and (4) low by the first and high by the second stakeholder group. Go-zones benchmark high and low ratings based on the mean for each group (i.e., a statement is considered “high” if it is above the stakeholder group’s mean rating of all statements). Categories 1 and 2 indicated that the stakeholder groups rated the statement similarly, and categories 3 and 4 indicated that the stakeholder groups rated the statements differently. We then calculated the percentage of statements related to each antecedent for the four categories, and summed the percentage in the similar (and different) categories between each pair of stakeholder groups.
We calculated recommended measures to assess reliability of the concept mapping sorting and rating data (Rosas & Kane, 2012; Trochim, 1993). We randomly divided our participants into two groups and calculated the split-half reliability coefficient (rSHT) by correlating the two groups’ sorting data (i.e., similarity matrices) and applying the Spearman–Brown correction. We calculated Cronbach’s alpha for importance rating data across all 125 statements.
Results
A total of 148 individuals participated in the sorting and rating activities (n = 66 community members, n = 38 health care providers, and n = 44 academic researchers). Community members were more likely than their counterparts to be female, be African American, and have fewer years working in health-related areas (see Table 1). Reliability and internal consistency of concept mapping data were high: rSHT = .95 and α > .90)
Table 1.
Demographics of Participants by Stakeholder Group.
| Characteristics | Community members (n = 66), % (n) | Health care providers (n = 38), % (n) | Academic researchers (n = 44), % (n) |
|---|---|---|---|
| Gender | |||
| Female | 81.8 (54) | 65.8 (25) | 66.0 (29) |
| Male | 18.2 (12) | 34.2 (13) | 34.1 (15) |
| Race/ethnicity | |||
| Non-Hispanic White | 10.9 (7) | 55.3 (21) | 77.3 (34) |
| Hispanic | 7.8 (5) | 7.9 (3) | 2.3 (1) |
| Black | 75.0 (48) | 30.0 (11) | 9.1 (4) |
| Other | 5.2 (4) | 7.9 (3) | 11.4 (5) |
| Experience working in academic–community research partnerships, years | |||
| <1 | 34.4 (22) | 5.3 (2) | 2.3 (1) |
| 1–3 | 12.5 (8) | 15.8 (6) | 13.6 (6) |
| 3–5 | 10.9 (7) | 15.8 (6) | 15.9 (7) |
| 5–7 | 3.1 (2) | 15.8 (6) | 9.1 (4) |
| >7 | 39.1 (25) | 47.4 (18) | 59.1 (26) |
Relative Importance of Trust Antecedents
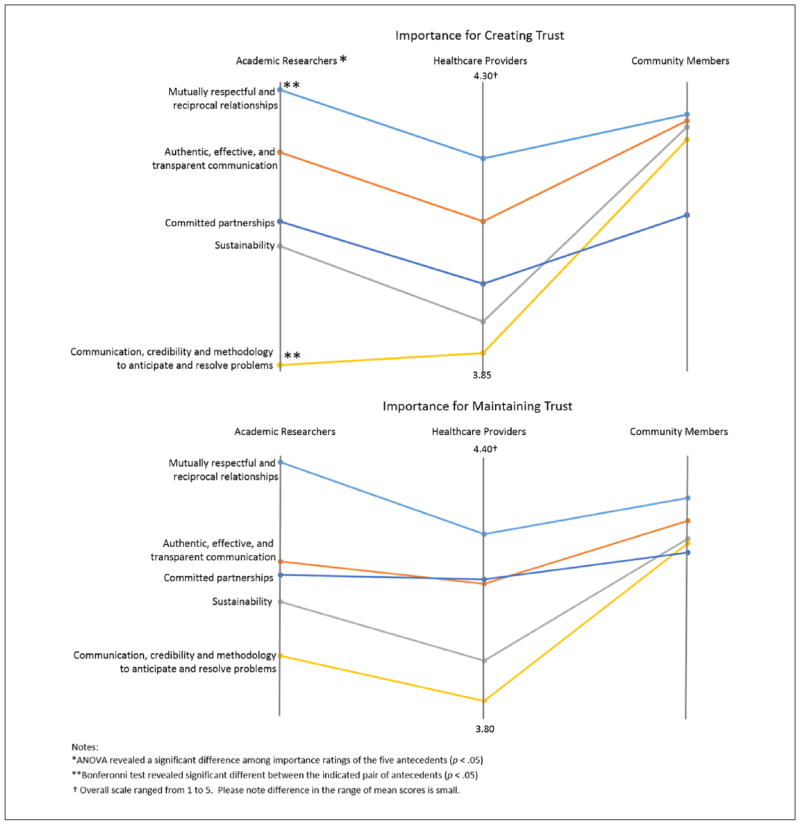
Pattern matching graphs in Figure 1 present the mean importance ratings of each of the five antecedents along three vertical axes—one for each stakeholder group. Across all stakeholder groups, the mean importance ratings for both creating and maintaining trust were highest for the antecedents of “authentic, credible, and transparent communication” and “mutually respectful and reciprocal relationships”; however, the ranking was different for the other three antecedents. Academic researchers’ and health care providers’ mean ratings of “communication and credibility to anticipate and resolve problems” and “sustainability” were the lowest of the five antecedents; whereas community members’ mean ratings of these two antecedents were higher than that of “committed partnerships.” ANOVA revealed that among academic researchers, there was a significant difference among their ratings of the five antecedents (p < .01). Specifically, the mean importance rating of “communication and credibility to anticipate and resolve problems” (M = 3.87, SD = 0.67) was significantly lower than that of “mutually respectful and reciprocal relationships” (M = 4.31, SD = 0.53). Among health care providers and community members, their mean ratings of the antecedents were not found to be significantly different.
Figure 1.
Relative comparison of mean ratings of dimensions by importance for creating and maintaining trust across stakeholder groups.
Note. The figure visualizes the relative importance ratings each stakeholder group placed on the five trust dimensions for creating and maintaining trust. Two dimensions, “mutually respectful and reciprocal relationships” and “authentic, effective, and transparent communication,” were rated highest across all groups. “Communication, credibility, and methodology to anticipate and resolve problems” was rated relatively higher by community members than health care providers and academic researchers.
Absolute Importance Levels of Trust Antecedents
There were no statistically significant differences between academic researcher and health care provider mean importance ratings (Table 2). Community members’ mean importance rating for creating trust of “communication, credibility, and methodology to anticipate and resolve problems” (M = 4.23, SD = 0.58) was significantly higher than academic researchers’ (M = 3.87, SD = 0.67) and health care providers’ ratings (M = 3.89, SD = 0.62; p < .01; Table 2). Community members’ mean importance rating of “sustainability” for creating trust (M = 4.25, SD = 0.70) was marginally higher (p < .10) than academic researchers’ (M = 3.94, SD = 0.56) and health care providers’ ratings (M = 4.06, SD = 0.69; p < .10). Also, community members’ mean importance rating of “communication, credibility, and methodology to anticipate and resolve problems” for maintaining trust (M = 4.16, SD = 0.72) was significantly higher (p < .05) than that of academic researchers’ (M = 3.81, SD = 0.60) and health care providers’ ratings (M = 3.91, SD = 0.69; p < .05).
Table 2.
Mean Ratings of Importance of Dimensions for Creating and Maintaining Trust Between Stakeholder Groups.
| Dimension | Community members, M (SD) | Health care providers, M (SD) | Academic researchers, M (SD) | Analysis of variance, pa |
|---|---|---|---|---|
| Importance for creating trust | ||||
| Mutually respectful and reciprocal relationships | 4.27 (0.69) | 4.20 (0.51) | 4.31 (0.53) | .682 |
| Authentic, effective, and transparent communication | 4.26 (0.59) | 4.10 (0.55) | 4.21 (0.47) | .333 |
| Sustainability | 4.25 (0.70) | 3.94 (0.56) | 4.06 (0.69) | .064 |
| Communication, credibility, and methodology to anticipate and resolve problems | 4.23 (0.58)a | 3.89 (0.62) | 3.87 (0.67) | .004 |
| Committed partnerships | 4.11 (0.70) | 4.00 (0.51) | 4.10 (0.57) | .660 |
| Importance for maintaining trust | ||||
| Mutually respectful and reciprocal relationships | 4.26 (0.71) | 4.18 (0.53) | 4.34 (0.53) | .545 |
| Authentic, effective, and transparent communication | 4.21 (0.67) | 4.07 (0.52) | 4.12 (0.57) | .531 |
| Sustainability | 4.17 (0.78) | 3.90 (0.59) | 4.03 (0.66) | .189 |
| Communication, credibility, and methodology to anticipate and resolve problems | 4.16 (0.72)a | 3.81 (0.60) | 3.91 (0.69) | .035 |
| Committed partnerships | 4.14 (0.75) | 4.08 (0.52) | 4.09 (0.56) | .908 |
Mean was significantly different (p < .05) compared to both health care providers and academic researchers in post hoc comparisons.
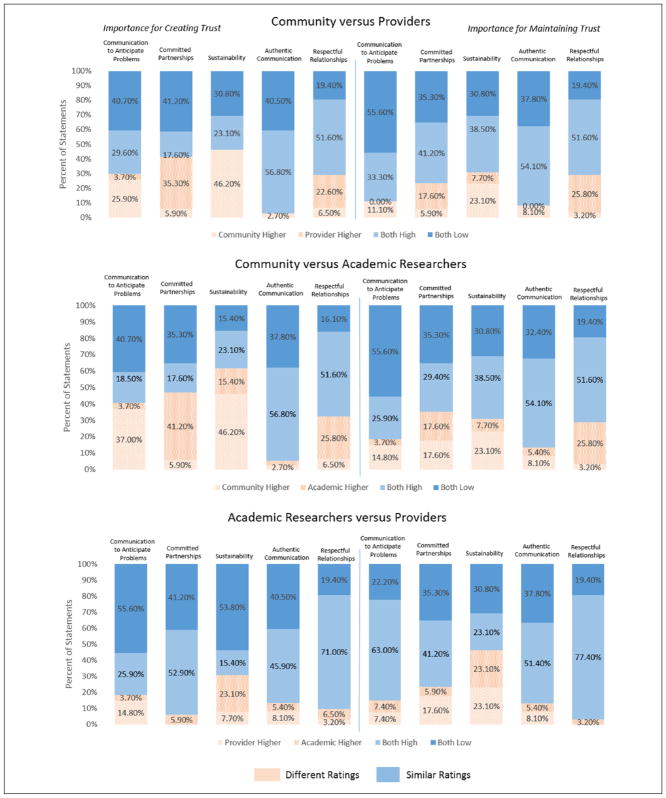
Congruence and Disagreement of Trust Antecedent Statements
Figure 2 indicates the percentage of statements related to each antecedent that were rated either similarly and differently between each pair of stakeholder groups. In general, health care providers and academic researchers rated statements related to the antecedents most similarly. Stakeholder groups rated the greatest percentage of statements similarly for the “authentic, credible, and transparent communication” antecedent—over 89% of statements between all pairs of stakeholder groups had similar ratings (Figure 2). The least similar ratings of statements were found related to “sustainability”—the average percentage rated differently across pairs of stakeholders was 43.1%. For example, over half (61.5%) of statements related to sustainability were rated differently between community members and academic researchers.
Figure 2.
Percentage of statements within each dimension with different and similar importance ratings between stakeholder groups.
Note. Concept mapping go-zone analyses were used to assess different and similar ratings of statements within each dimension between stakeholder groups. The darker portion of the bar graphs indicates the percentage of statements rated similarly, and the lighter portion reflects the percentage rated differently. Statements within the dimension of sustainability had the greatest proportion of dissimilar ratings, especially between community members and academic researchers. Authentic communication had the highest proportion of statements rated similarly.
Discussion
To our knowledge, this study is one of the first to investigate similarities and differences among stakeholder groups’ perspectives about the most important contributors to trust within research partnerships. The most significant differences across stakeholder groups were between community members and academic researchers, in particular with regard to creating trust (differences for maintaining trust appeared to attenuate). All three stakeholder groups viewed antecedents of “authentic, effective, and transparent communication” and “mutually respectful and reciprocal relationships” as highly important. However, significant differences were found related to “communication, credibility, and methodology to anticipate and resolve problems” and “sustainability.” Our findings indicate potential areas where attention may be needed to improve trust within partnerships.
The two antecedents that all stakeholder groups rated as relatively most important (i.e., “authentic, effective, and transparent communication” and “mutually respectful and reciprocal relationships”) both relate to colearning processes involving transactions between parties in terms of information, experiences, or services. Qualitative research has found that effective communication and positive interpersonal interactions are important facilitators of trust and successful community–academic research partnerships (Barnett, Anderson, Houle, Higginbotham, & Gatling, 2010; White-Cooper, Dawkins, Kamin, & Anderson, 2009). Our study strengthens empirical evidence that communication and relationships are perceived as most important to trust across stakeholder groups, and indicates the importance of co-learning within research.
There were also differences in the relative ratings of the antecedents. It appeared that academic researchers placed slightly less importance on, “communication, credibility, and methodology to anticipate and resolve problems” for creating trust, whereas community members rated it equally important to other antecedents. One study using focus groups found that community partners provided specific examples of barriers to developing trust more often than academic partners (White-Cooper et al., 2009). Another study found that community partners were less satisfied with the quality of communication and decision-making processes (e.g., expressing views, bringing up new ideas) than academic partners (Allen, Culhane-Pera, Pergament, & Call, 2011). Our study indicates that these differing perspectives may be related to the relative importance stakeholders place on this antecedent of trust.
In absolute terms, community members rated the antecedent of “communication, credibility, and methodology to anticipate and resolve problems” with higher mean importance than academic researchers. Ours is the first study to our knowledge to statistically assess differences in trust in the context of community–academic partnerships. A larger proportion of our community member participants were female and non-White, which was expected given the underrepresentation of women and minorities in academia and health care professions (Committee on Opportunities to Address Clinical Research Workforce Diversity Needs for 2010, 2006). Community members’ higher valuations in the importance of creating trust are possibly due, in part, to women’s and racial/ethnic minorities’ lower levels of general trust in health care institutions and providers (Armstrong et al., 2006; Boulware, Cooper, Ratner, LaVeist, & Powe, 2003; Corbie-Smith, Thomas, & St. George, 2002; Doescher, Saver, Franks, & Fiscella, 2000; Halbert, Armstrong, Gandy, & Shaker, 2006). Our findings indicate that gender and race likely contribute to differences in perceptions of trust in research partnerships and should be explored by future studies.
Finally, we found that participants appeared to have the most divergent perspectives regarding the importance of statements related to sustainability. There is a substantial body of conceptual and theoretical literature about sustainability, yet there remains a lack of consensus regarding the definition and determinants of it (Luke, 2014; Scheirer, 2005; Shediac-Rizkallah & Bone, 1998). A recent concept mapping study identified nine separate domains of sustainability of public health programs (e.g., funding stability, partnerships, organizational capacity; Schell et al., 2013). Through the concept mapping process, participants in our study identified statements related to sustainability that included a similar range of activities and concepts (e.g., funding, staffing, capacity building, and training opportunities). Enhancing sustainability is a major challenge of community–academic research partnerships (Alexander et al., 2003; Israel et al., 2006; Moreno et al., 2009; Pivik & Goelman, 2011). Our findings indicate that more detailed exploration of ideas and concepts related to sustainability may be of value to understand the best processes to address the challenges. For example, academic researchers who rely on community partners to conduct on-the-ground research activities may view strategies to sustain financial resources to employ staff as more important, whereas community partners who have less access to educational opportunities than academic partners may view training strategies to sustain their long-term research capacity as more important.
Limitations
This study has several limitations. To reduce respondent burden, we obtained few demographic measures on our participants; this limited our ability to assess representation of our sample and consider additional potential confounders (e.g., age, education level). Also, “health care providers” in our study had experience with community-engaged research, and their responses may be different from health care providers who do not conduct community-engaged research. The respondent-driven procedures of the overall concept mapping approach helped purposively select participants with community-engaged research experience and facilitated identification of the major contributors perceived to create and maintain trust. However, using these methods meant that participants were not randomly selected, which may have introduced bias into the distribution and range of perspectives observed within each stakeholder group. Finally, although we detected statistically significant differences in mean ratings, the differences are small and their meaningfulness is unclear—however, it is notable that interpretation session facilitators noted they observed similar qualitative differences in how stakeholder groups discussed the importance of the antecedents.
Implications and Conclusions
Academic researchers may focus less on antecedents they perceive as less important, such as communication and methodology to resolve problems. Thus, partnerships should consider focused attention on this antecedent. For example, adaptations of collaborative problem-solving techniques such as the jigsaw (Aronson, Blaney, Stephan, Sikes, & Snapp, 1978) or think-pair-share method (Kagan & Kagan, 1994) may be valuable to apply within research partnerships. The jigsaw method is a technique to divide an overall project into segments, which are assigned to small groups of learners who work together as “experts” to complete their specific segment. The small groups then learn from each other about all segments to ensure completion and understanding of the final product across learners. Similarly a research project could be divided into important segments (e.g., participant recruitment, data analysis, etc.) and assigned to small groups that include a member from each stakeholder group to complete. Think-pair-share is a staged approach that involves time for learners to address a problem by (1) thinking about it individually, (2) discussing it in pairs, and (3) sharing ideas with the group. This may be an apt strategy to approach problem resolution in the context of research partnerships. Finally, project management software or online collaboration tools that allow community members to bring concerns to the attention of academic researchers should be considered and tested.
Our findings also highlight important areas for future empirical studies. Future research should develop instrumentation to measure trust. To improve understanding of specific strategies that improve trust, validated measures could be used within longitudinal research to assess trust development within and across partnerships in relation to the deployment of communication and relationship-building strategies. More research is merited to understand factors that shape divergent perspectives on how best to sustain community-engaged partnerships. Furthermore, studies should assess stakeholders’ perspectives regarding the optimal levels and distributions of types of resources (e.g., grant funding, in-kind support, community knowledge), and how these perspectives relate to trust.
Our study investigated an area with limited empirical study, yet consistently highlighted as a critical factor for effective community-engaged research. Our study generated insight about how different stakeholders view trust. We uncovered similarities across all stakeholders related to communication and to reciprocal relationships that provide an important foundation for building trust, but we also found differences related to sustainability and to communication and methodology to resolve problems. Future research to understand and develop strategies to address differences has potential to improve trust within community–academic research partnerships and generate more effective collaborations to address health.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Dr. Scott Rosas, senior consultant with Concept Systems, for his guidance on concept mapping validity and reliability measures.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a grants from the National Institutes of Health/ National Center for Advancing Translational Science through the Clinical & Translational Science Award Institutions of University of Arkansas for Medical Sciences (#UL1TR000039), University of California, Los Angeles (#UL1TR 000124), University of Florida (#UL1TR 000064), University of North Carolina (#UL1TR001111), and the University of Pittsburgh (#UL1TR000005). The study was also partially supported by Dr. Corbie Smith’s National Institutes of Health midcareer investigator award in patient-oriented research (K24 HL105493). The study sponsors did not have any role in study design; collection, analysis, and interpretation of data; writing the report, or the decision to submit the report for publication.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional supporting information is available at heb.sagepub.com/supplemental.
References
- Alexander JA, Weiner BJ, Metzger ME, Shortell SM, Bazzoli GJ, Hasnain-Wynia R, … Conrad DA. Sustainability of collaborative capacity in community health partnerships. Medical Care Research and Review. 2003;60(4 Suppl):130S–160S. doi: 10.1177/1077558703259069. [DOI] [PubMed] [Google Scholar]
- Allen ML, Culhane-Pera KA, Pergament S, Call KT. A capacity building program to promote CBPR partnerships between academic researchers and community members. Clinical and Translational Science. 2011;4:428–433. doi: 10.1111/j.1752-8062.2011.00362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self-reported health in the United States. Journal of General Internal Medicine. 2006;21:292–297. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aronson M, Blaney N, Stephan C, Sikes J, Snapp M. The jigsaw classroom. Beverly Hills, CA: Sage; 1978. [Google Scholar]
- Barnett M, Anderson J, Houle M, Higginbotham T, Gatling A. The process of trust building between university researchers and urban school personnel. Urban Education. 2010;45:630–660. [Google Scholar]
- Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Reports. 2003;118:358–365. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutin-Foster C, Phillips E, Palermo AG, Boyer A, Fortin P, Rashid T, … Love G. The role of community-academic partnerships: Implications for medical education, research, and patient care. Progress in Community Health Partnerships. 2008;2(1):55–60. doi: 10.1353/cpr.2008.0006. [DOI] [PubMed] [Google Scholar]
- Brush BL, Baiardi JM, Lapides S. Moving toward synergy: Lessons learned in developing and sustaining community–academic partnerships. Progress in Community Health Partnerships. 2011;5(1):27–34. doi: 10.1353/cpr.2011.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cargo M, Delormier T, Lévesque L, Horn-Miller K, McComber A, Macaulay AC. Can the democratic ideal of participatory research be achieved? An inside look at an academic–indigenous community partnership. Health Education Research. 2008;23:904–914. doi: 10.1093/her/cym077. [DOI] [PubMed] [Google Scholar]
- Carney JK, Maltby HJ, Mackin KA, Maksym ME. Community–academic partnerships: How can communities benefit? American Journal of Preventive Medicine. 2011;41(4 Suppl 3):S206–S213. doi: 10.1016/j.amepre.2011.05.020. [DOI] [PubMed] [Google Scholar]
- Committee on Opportunities to Address Clinical Research Workforce Diversity Needs for 2010. The status of women and underrepresented minorities and programs of support. In: Ommaya A, Hahm J, editors. Opportunities to address clinical research workforce diversity needs for 2010. Washington, DC: National Academies Press; 2006. pp. 33–54. [PubMed] [Google Scholar]
- Corbie-Smith G, Thomas SB, St George DMM. Distrust, race, and research. Archives of Internal Medicine. 2002;162:2458–2463. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- Dalal M, Skeete R, Yeo HL, Lucas GI, Rosenthal MS. A physician team’s experiences in community-based participatory research: Insights into effective group collaborations. American Journal of Preventive Medicine. 2009;37(6 Suppl 1):S288–S291. doi: 10.1016/j.amepre.2009.08.013. [DOI] [PubMed] [Google Scholar]
- Deutsch M. Trust and suspicion. Journal of Conflict Resolution. 1958;2:265–279. [Google Scholar]
- Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Archives of Family Medicine. 2000;9:1156–1163. doi: 10.1001/archfami.9.10.1156. [DOI] [PubMed] [Google Scholar]
- Frerichs L, Dave G, Kim M, Cheney A, Sullivan G, Varma D, … Corbie-Smith G. Engaging stakeholders in defining factors of building and sustaining trust in community-engaged research partnerships. Paper presented at the Society of General Internal Medicine Annual Meeting; Toronto, Ontario, Canada. 2015. Apr, [Google Scholar]
- Gilbert KL, Quinn SC, Ford AF, Thomas SB. The urban context: A place to eliminate health disparities and build organizational capacity. Journal of Prevention & Intervention in the Community. 2010;39:77–92. doi: 10.1080/10852352.2011.530168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halbert CH, Armstrong K, Gandy OH, Shaker L. Racial differences in trust in health care providers. Archives of Internal Medicine. 2006;166:896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: What is it, can it be measured, and does it matter? Milbank Quarterly. 2001;79:613–639. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Krieger J, Vlahov D, Ciske S, Foley M, Fortin P, … Palermo A. Challenges and facilitating factors in sustaining community-based participatory research partnerships: Lessons learned from the Detroit, New York City and Seattle Urban Research Centers. Journal of Urban Health. 2006;83:1022–1040. doi: 10.1007/s11524-006-9110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Schulz AJ, Parker EA. In: Methods in community-based participatory research for health. Israel B, Schulz AJ, Parker EA, editors. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- Kagan S, Kagan M. The structural approach: Six keys to cooperative learning. In: Sharan S, editor. Handbook of cooperative learning methods. Westport, CT: Greenwood Press; 1994. pp. 115–133. [Google Scholar]
- Kane M, Trochim WM. Concept mapping for planning and evaluation. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- Khodyakov D. Trust as a process: A three-dimensional approach. Sociology. 2007;41:115–132. [Google Scholar]
- Lesser J, Oscós-Sánchez MA. Community–academic research partnerships with vulnerable populations. Annual Review of Nursing Research. 2007;25:317–337. [PubMed] [Google Scholar]
- Lewicki RJ, Tomlinson EC, Gillespie N. Models of interpersonal trust development: Theoretical approaches, empirical evidence, and future directions. Journal of Management. 2006;32:991–1022. [Google Scholar]
- Lewicki RJ, Wiethoff C. Trust, trust development, and trust repair. In: Deutsche M, Coleman PT, editors. The handbook of conflict resolution: Theory and practice. San Francisco, CA: Jossey-Bass; 2000. pp. 86–107. [Google Scholar]
- Lewis JD, Weigert AJ. The social dynamics of trust: Theoretical and empirical research, 1985–2012. Social Forces. 2012;91:25–31. [Google Scholar]
- Lowe J, Riggs C, Henson J. Principles for establishing trust when developing a substance abuse intervention with a Native American community. Creative Nursing. 2011;17(2):68–73. doi: 10.1891/1078-4535.17.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luke DA. The Program Sustainability Assessment Tool: A new instrument for public health programs. Preventing Chronic Disease. 2014:11. doi: 10.5888/pcd11.130184. Retrieved from http://www.cdc.gov/pcd/issues/2014/13_0184.htm. [DOI] [PMC free article] [PubMed]
- Masuda JR, Creighton G, Nixon S, Frankish J. Building capacity for community-based participatory research for health disparities in Canada: The case of “partnerships in community health research. Health Promotion Practice. 2011;12:280–292. doi: 10.1177/1524839909355520. [DOI] [PubMed] [Google Scholar]
- Merzel C, Burrus G, Davis J, Moses N, Rumley S, Walters D. Developing and sustaining community—academic partnerships: Lessons from downstate New York healthy start. Health Promotion Practice. 2007;8:375–383. doi: 10.1177/1524839906289557. [DOI] [PubMed] [Google Scholar]
- Minkler M. Community-based research partnerships: Challenges and opportunities. Journal of Urban Health. 2005;82(Suppl 2):ii3–ii12. doi: 10.1093/jurban/jti034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno G, Rodríguez MA, Lopez GA, Bholat MA, Dowling PT. Eight years of building community partnerships and trust: The UCLA family medicine community-based participatory research experience. Academic Medicine. 2009;84:1426–1433. doi: 10.1097/ACM.0b013e3181b6c16a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris KC, Brusuelas R, Jones L, Miranda J, Duru OK, Mangione CM. Partnering with community-based organizations: an academic institution’s evolving perspective. Ethnicity & Disease. 2007;17(Suppl 1):S1–S27. [PubMed] [Google Scholar]
- Parrill R, Kennedy B. Partnerships for health in the African American community: Moving toward community-based participatory research. Journal of Cultural Diversity. 2011;18(4):150–154. [PubMed] [Google Scholar]
- Pivik JR, Goelman H. Evaluation of a community-based participatory research consortium from the perspective of academics and community service providers focused on child health and well-being. Health Education & Behavior. 2011;38:271–281. doi: 10.1177/1090198110372876. [DOI] [PubMed] [Google Scholar]
- Plowfield LA, Wheeler EC, Raymond JE. Time, tact, talent, and trust: Essential ingredients of effective academic-community partnerships. Nursing Education Perspectives. 2005;26:217–220. [PubMed] [Google Scholar]
- Risisky D, Hogan VK, Kane M, Burt B, Dove C, Payton M. Concept mapping as a tool to engage a community in health disparity identification. Ethnicity & Disease. 2008;18(1):77–83. [PubMed] [Google Scholar]
- Robinson JM, Trochim WM. An examination of community members’, researchers’ and health professionals’ perceptions of barriers to minority participation in medical research: An application of concept mapping. Ethnicity & Health. 2007;12:521–539. doi: 10.1080/13557850701616987. [DOI] [PubMed] [Google Scholar]
- Rosas SR, Kane M. Quality and rigor of the concept mapping methodology: A pooled study analysis. Evaluation and Program Planning. 2012;35:236–245. doi: 10.1016/j.evalprogplan.2011.10.003. [DOI] [PubMed] [Google Scholar]
- Scheirer MA. Is sustainability possible? A review and commentary on empirical studies of program sustainability. American Journal of Evaluation. 2005;26:320–347. [Google Scholar]
- Schell SF, Luke DA, Schooley MW, Elliott MB, Herbers SH, Mueller NB, Bunger AC. Public health program capacity for sustainability: A new framework. Implementation Science. 2013;8:15. doi: 10.1186/1748-5908-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shediac-Rizkallah MC, Bone LR. Planning for the sustainability of community-based health programs: Conceptual frameworks and future directions for research, practice and policy. Health Education Research. 1998;13:87–108. doi: 10.1093/her/13.1.87. [DOI] [PubMed] [Google Scholar]
- Strand K, Marullo S, Cutforth N, Stoecker R, Donohue P. Principles of best practice for community-based research. Michigan Journal of Community Service Learning. 2003;9:5–15. [Google Scholar]
- Suarez-Balcazar Y, Harper GW, Lewis R. An interactive and contextual model of community-university collaborations for research and action. Health Education & Behavior. 2005;32:84–101. doi: 10.1177/1090198104269512. [DOI] [PubMed] [Google Scholar]
- Trochim WMK. The reliability of concept mapping. Paper presented at the Annual Conference of the American Evaluation Association; Dallas, TX. 1993. Nov, [Google Scholar]
- White-Cooper S, Dawkins NU, Kamin SL, Anderson LA. Community-institutional partnerships: Understanding trust among partners. Health Education & Behavior. 2009;36:334–347. doi: 10.1177/1090198107305079. [DOI] [PubMed] [Google Scholar]
- Wolff M, Maurana CA. Building effective community–academic partnerships to improve health: A qualitative study of perspectives from communities. Academic Medicine. 2001;76:166–172. doi: 10.1097/00001888-200102000-00016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.