Abstract
Malaria remains widespread throughout the planet and increasing global travel continues to lead to imported cases of malaria in travelers, including children. This article provides an overview of pediatric malaria, including its epidemiology, clinical features, diagnosis, treatment, and prevention in travelers.
Keywords: Malaria, Travel medicine, Fever, Diagnostics, Antiparasitic therapy, Chemoprophylaxis
Key points
-
•
Malaria is common worldwide and travel to malaria-endemic destinations is increasing.
-
•
Travel history should be obtained for all children presenting with fever.
-
•
Antigen-based malaria tests can provide rapid malaria diagnosis, although blood smears are still necessary.
-
•
Treatment of malaria depends on severity of illness, species of malaria parasite, and epidemiologic likelihood of drug resistance.
Introduction
A century ago, malaria was a major public health threat in the United States, with ongoing transmission in 13 Southeastern states as late as the 1930s.1 Although extensive efforts ultimately eliminated local malaria in North America, this mosquito-borne infection remains endemic throughout much of the world. Indeed, more than half of the children on our planet live in malaria-endemic countries. Despite continued success in malaria control, there are more than 200 million new infections each year and nearly half a million deaths, mostly in infants and children younger than 5 years old.2 Importantly, in our increasingly global society, malaria and other imported infectious diseases remain of particular concern to the North American traveler, with nearly all American malaria cases acquired abroad.3, 4, 5, 6
This article offers a brief overview of the Plasmodium parasite responsible for malaria, the epidemiology of infection, clinical features associated with uncomplicated and severe malaria presentations, preventative measures for travelers, and current treatment strategies for childhood malaria infections.
Description of the pathogen
Malaria is caused by infection with intracellular protozoan parasites of the genus Plasmodium, transmitted by the bite of a female Anopheles spp mosquito.7, 8 While feeding, the infected mosquito leaves behind sporozoites, the infectious motile form of the parasite. Sporozoites then migrate to the liver, asymptomatically invade hepatocytes, and amplify infection through the release of tens of thousands of daughter parasites. This release initiates the asexual erythrocytic replication stage of the parasite life cycle, the stage of parasite responsible for the malaria pathogenesis. Two species of Plasmodium, P vivax and P ovale, uniquely develop dormant parasite forms called hypnozoites, which may remain in the liver for months or years after primary infection before causing relapse and recurrent symptomatic disease.9, 10
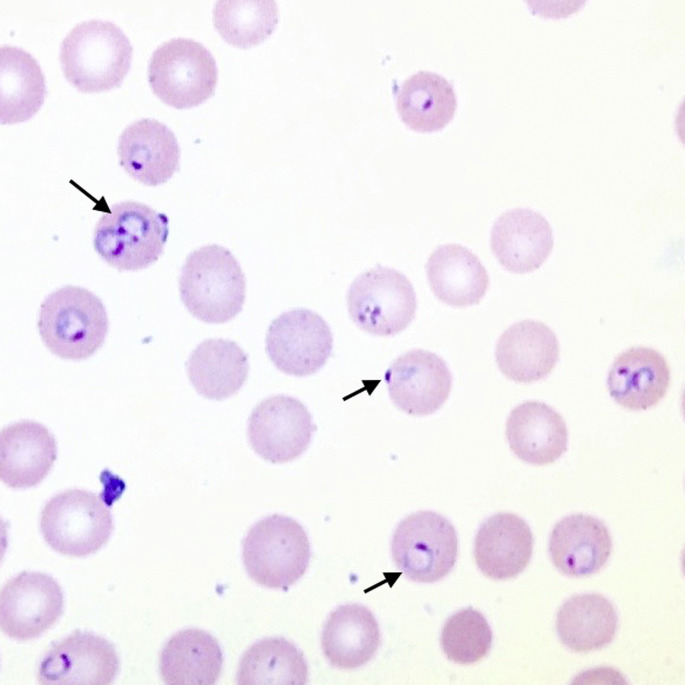
The clinical symptoms of malaria are due to cycles of asexual replication within red blood cells (Fig. 1 ). Fever is a hallmark symptom, triggered by erythrocyte rupture and parasite release every 2 to 3 days, depending on Plasmodium species.7 Severe, life-threatening malaria may result from high parasite burdens, causing hemolysis and severe anemia, or from end-organ damage due to vascular adherence of infected erythrocytes and microocclusion.11, 12 Person-to-person transmission is mediated by mosquitoes, in which the sexual form of the parasite (gametocytes) infects a feeding mosquito to thus complete the parasite’s complex life cycle.7, 8
Fig. 1.
Blood smear from patient with P falciparum malaria. Intraerythrocytic parasite forms are visible in nearly 20% of red blood cells, some of which are doubly-infected. Arrows: typical signet ring, headphones, and appliqué forms of the parasite.
(Courtesy of Amruta Padhye MD, Columbia, MO.)
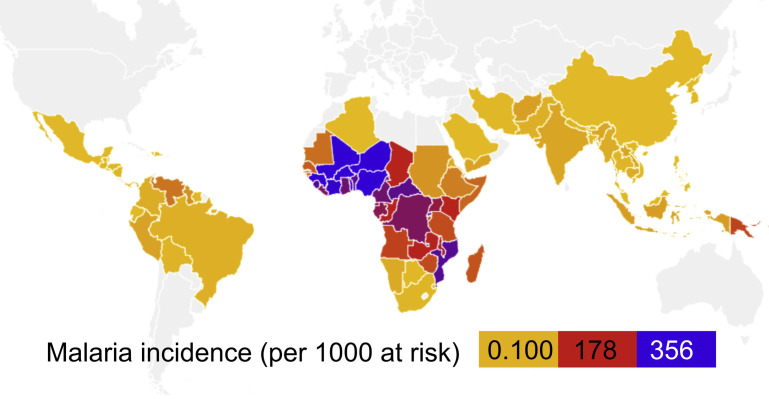
Epidemiology
More than half the world’s population lives in areas where malaria transmission occurs, and the disease continues to cause a major public health burden to populations in areas of Africa, Asia, and Central and South America (Fig. 2 ).2 In 2015, more than 200 million cases of malaria were reported, resulting in nearly half a million deaths, an estimate 3 times higher than the number of people lost to armed conflicts that same year.2, 13 Most of malaria-associated deaths are caused by P falciparum species in sub-Saharan Africa, which kills about 1200 African children younger than the age of 5 years daily.14
Fig. 2.
Malaria incidence in 2015. Incidence of malaria per 1000 population at risk. Map created using OpenHeatMap (www.openheatmap.com).
(Data from World Health Organization. World malaria report 2015. Geneva (Switzerland): World Health Organization; 2016. Available at: http://www.who.int/malaria/publications/world-malaria-report-2015/report/en/.)
Global malaria control efforts have focused on both mosquito vector control strategies and improved access to effective antimalarial therapies. There have been tremendous gains in the last decade; from 2000 to 2015, the incidence of malaria has dropped by 37%, and deaths have decreased by 60% globally.2, 15 However, drug resistance continues to hamper control efforts worldwide, with widespread resistance to the former first-line agents chloroquine and sulfadoxine-pyrimethamine.16 The remarkable discovery of artemisinin by Nobel Laureate Youyou Tu ultimately led to development of rapidly parasiticidal artemisinin-based combination therapies (ACTs), powerful weapons in the face of rising resistance to older antimalarials.17, 18 Unfortunately, the emergence of artemisinin-resistant P falciparum in Southeast Asia, only a few years after ACT implementation, emphasizes the importance of sustaining control measures and the ongoing need for antimalarial development.19, 20
Though malarial transmission remains possible in areas of the United States where anopheline mosquitoes are found, nearly all of the 1500 or so annual reported cases of malaria in the United States are infections acquired abroad.3, 5, 21 Rare and unusual modes of transmission have also been reported, which include inadvertent airplane transport of mosquitos from endemic areas, congenital transmission, transfusion-associated malaria, and contaminated needles and syringes.22, 23, 24, 25, 26
Clinical features of malaria
Uncomplicated malaria infection typically manifests as a nonspecific febrile illness, similar in presentation to influenza and other common viral infections.27, 28 Travelers with acute malaria most often present within 7 days to 3 months following an infected mosquito bite, and malaria should be suspected in any febrile traveler.3 Malaria symptoms are highly variable, and may include chills, rigors, sweating, headaches, lethargy, myalgias, and cough. Gastrointestinal symptoms may be prominent, including nausea, emesis, diarrhea, and abdominal pain.29 In addition to fever, physical findings may reflect end-organ involvement, including pallor, tachycardia, hepatosplenomegaly, jaundice, and increased respiratory rate, as well as, in the case of cerebral malaria, altered mental status.30 The course of disease may be indolent or fulminant, and delays in or lack of treatment beyond 24 hours following onset of clinical symptoms may result in rapid progression to life-threatening, severe malarial disease.31
Children younger than 18 years of age tend to present sooner and are more likely to develop severe malaria. Of note, the classic cyclical fever patterns described for malaria may not be present in travelers and young children because parasite life cycles may not have synchronized by the time treatment is sought.27, 28 Unsurprisingly, travelers are more likely to present with severe malaria, compared with the semi-immune residents of endemic areas.3, 5 Additional risk factors for development of severe malaria include recent travel to P falciparum–endemic regions (especially sub-Saharan Africa), age older than 65 years or younger than 18 years, pregnancy, existing medical conditions, lack of malaria prophylaxis, and treatment delay.5, 30
Severe malaria may manifest as 1 or more of the following syndromes30, 32:
-
1.
Cerebral malaria: Caused by parasite adherence to cerebral vasculature, symptoms may include altered mental status, coma, seizures, and evidence of increased intracranial pressure
-
2.
Blackwater fever: Acute renal failure and hemoglobinuria caused by intravascular hemolysis
-
3.
Severe anemia: Defined as hemoglobin less than 7 g/dL and caused by high parasite burden and hemolysis of infected erythrocytes
-
4.
Acute respiratory distress syndrome
-
5.
Hyperparasitemia: Typically defined as malaria parasite infection of greater than 5% of circulating red blood cells
-
6.
Metabolic complications: Common abnormalities include severe metabolic acidosis and life-threatening hypoglycemia.
Although fever is an almost universal symptom of malaria, infections with different Plasmodium species may have somewhat variable clinical presentations (Table 1 ). Severe malaria is most often due to infection with P falciparum, which can reach higher parasite levels than other species.8 P falciparum accounts for 80% of United States malaria cases seen in child travelers.2 In contrast, P vivax and P ovale infections are rarely fatal but carry the risk of reactivation of dormant liver-stage parasites.9, 10 Chronic asymptomatic bloodstream infection may result from P malariae infection, which can also cause a nephrotic syndrome from immune complex deposition in the kidney.33 Less often seen in travelers, P knowlesi is a zoonotic malaria parasite of long-tailed macaques, increasingly recognized as a cause of severe human infections that may be misdiagnosed as the less harmful P malariae species.34
Table 1.
Species of human malaria parasites
| Plasmodium Species | Endemic Regions | Typical Drug Resistance |
|---|---|---|
| P falciparum |
|
|
| P vivax |
|
|
| P ovale |
|
— |
| P malariae | Less common Wide global distribution |
— |
| P knowlesi | Rare Cases in forested regions of Southeast Asia, associated with long-tailed macaques |
— |
Malaria prevention for travelers: awareness and bites
Protective strategies against malaria infection are strongly recommended for all travelers to malaria-endemic regions. Because there is no approved vaccine for malaria, malaria prevention requires awareness of the risks of malaria infection, preventing mosquito bites and encouraging adherence to antimalarial chemoprophylactic regimens.35
A health care provider must first help to assess a traveler’s risk of contracting malaria by determining the endemicity of a particular locale and the season of travel. Urban areas, air-conditioned locations, and geographic regions above 3300 m are typically free of malaria.35 Clinicians who provide pretravel counseling should consult the most current and detailed information on health risks, including malaria, which may be found on the Centers for Disease Control and Prevention (CDC) Web site (www.CDC.gov/malaria), as well the World Health Organization Web site (http://www.who.int/malaria/travellers/en/). Parents and guardians are strongly cautioned against taking very young children to high endemicity areas, in part because it is challenging to provide a suitable preventative chemotherapeutic regimen that is approved for use in small infants (Table 2 ). Furthermore, malaria may be rapidly fatal in young pediatric patients, in whom early symptoms of P falciparum infection may go unrecognized.36
Table 2.
Commonly used agents for antimalarial prophylaxis
| Treatment Recommendations | Contraindications | Target Population | |
|---|---|---|---|
| Atovaquone-proguanil | Prevention and treatment of chloroquine-resistant P falciparum | Not recommended for pregnant or breastfeeding women, children <11 kg, or patients with impaired renal function | Last-minute travelers or travelers with short-term exposure to endemic regions Well-tolerated but may be more expensive than other options |
| Doxycycline | Can be used for prophylaxis but not treatment | Contraindicated in children <8 y old and pregnant women Gastrointestinal discomfort and sun sensitivity are common |
Daily dosing, inexpensive option, suitable for last-minute travelers |
| Mefloquine | Effective against chloroquine-resistant parasites | Safe during pregnancy but not approved by the US Food and Drug Administration for children weighing <5 kg or younger than 6 mo Neuropsychiatric effects can be pronounced, contraindicated in patients with seizure disorders or cardiac conduction abnormalities |
Weekly dosing regimen, preferred for long-term travelers |
| Primaquine | Recommended for prophylaxis in areas with P vivax malaria | Cannot be taken by pregnant or breast-feeding women Testing is necessary to exclude patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency |
Daily dosing |
| Chloroquine | Limited use due to widespread resistance | Safe for infants, young children, and pregnant women | Weekly dosing, must be started 1–2 wk before travel |
All species of malaria are mosquito-transmitted and, therefore, the first line of protection against infection is to prevent bites from Anopheles spp. Insect repellents containing DEET, picaridin, or IR3535 are recommended to protect exposed skin and should be reapplied every few hours in warmer climates. Protective clothing should be worn, with long sleeves and pants tucked into socks with appropriate footwear. A helpful tip is to treat clothing with repellent or long-lasting insecticides such as permethrin (readily available from online retailers), which lasts through several clothing washes. Finally, travelers are strongly recommended to use insecticide-treated mosquito bed nets with mesh sizes smaller than 1.5 mm, which are particularly effective against the night-feeding A gambiae vector.36
Malaria prevention for travelers: chemoprophylaxis
In addition to barrier protection, chemoprophylaxis should be offered to adults and children traveling to endemic malaria regions. Specific regimens are dictated by a traveler’s risk of acquiring malaria and local antimalarial-resistance patterns, and providers are encouraged to follow country-specific recommendations from the CDC (https://www.cdc.gov/malaria/travelers/country_table/a.html). In the United States, approved malaria chemoprophylaxis options include atovaquone-proguanil, chloroquine, doxycycline, mefloquine, and primaquine (see Table 2).37
Most cases of P falciparum malaria infection result from inadequate adherence to prophylactic regimens or failure to take precautions against mosquitoes, with self-reported adherence rates in American military personnel of less than 50%.38, 39 Proper education about the risks of malaria and the efficacy of prevention methods has been shown to improve adherence to preventative measures, and this is particularly important with rising rates of international travel.6, 36 In summary, the ABCs of malaria prevention are as follows36:
A: Awareness of the risks of malaria. This can include understanding incubation periods, the possibility of delayed onset symptoms, and symptoms, especially fever.
B: Bites. Efforts to reduce the likelihood of mosquito bites.
C: Chemoprophylaxis. Using antimalarial drugs that target blood and liver-stage parasites to prevent progression of infection to disease.
D: Diagnosis. Prompt diagnosis and treatment is key to prevent complications of disease caused by malaria infection.
Diagnosis of malaria infection
Because the symptoms of malaria can be highly variable, clinicians should maintain a high index of suspicion for all returning travelers presenting with fever. Clinicians should continue to consider routine pediatric infections, such as viral and bacterial respiratory tract infections, infectious diarrhea, and urinary tract infections. In patients with fever and altered mental status or seizure, cerebral malaria may mimic bacterial meningitis, which is of particular concern in young children who may not have completed routine vaccinations and in travelers returning from the Hajj or other parts of the meningitis belt of sub-Saharan Africa. Important additional considerations in travelers include typhoid fever (especially in children younger than 5 years) and dengue, both of which are common in malaria-endemic regions.35 Clinicians should maintain awareness of any ongoing global infectious disease outbreaks, such as Ebola and severe acute respiratory syndrome (SARS), which may have immediate infection control implications.
When malaria is suspected, thick and thin blood films of peripheral blood should be examined.31 Thick blood films provide for more sensitive detection of malaria parasites, whereas thin blood films permit speciation and quantification of parasitemia. Blood films should be repeated every 12 to 24 hours during the initial 72 hours of suspected malaria infection, regardless of whether parasites are observed.37
Lateral flow-based rapid diagnostic tests (RDTs) have recently become available to provide initial screening for malaria infection, especially for smaller facilities that may not have trained microscopists on staff at all times. Beginning in 2007, the US Food and Drug Administration (FDA) approved the BinaxNOW malaria RDT for use in commercial laboratories and hospitals. This antigen detection kit has high sensitivity and specificity for P falciparum and P vivax infection, with reduced sensitivity for P ovale and P malariae.40, 41 Because both false-positive and false-negative results have been reported with RDTs worldwide, suspected malaria should continue to be evaluated by blood smears, regardless of the results of rapid testing.42, 43, 44
Nucleic acid testing for malaria remains the gold standard, with the highest sensitivity and specificity42, 45; however, such testing is unavailable at most North American facilities. Polymerase chain reaction testing for diagnostic confirmation and species identification is provided free-of-charge for referring facilities in the United States.3
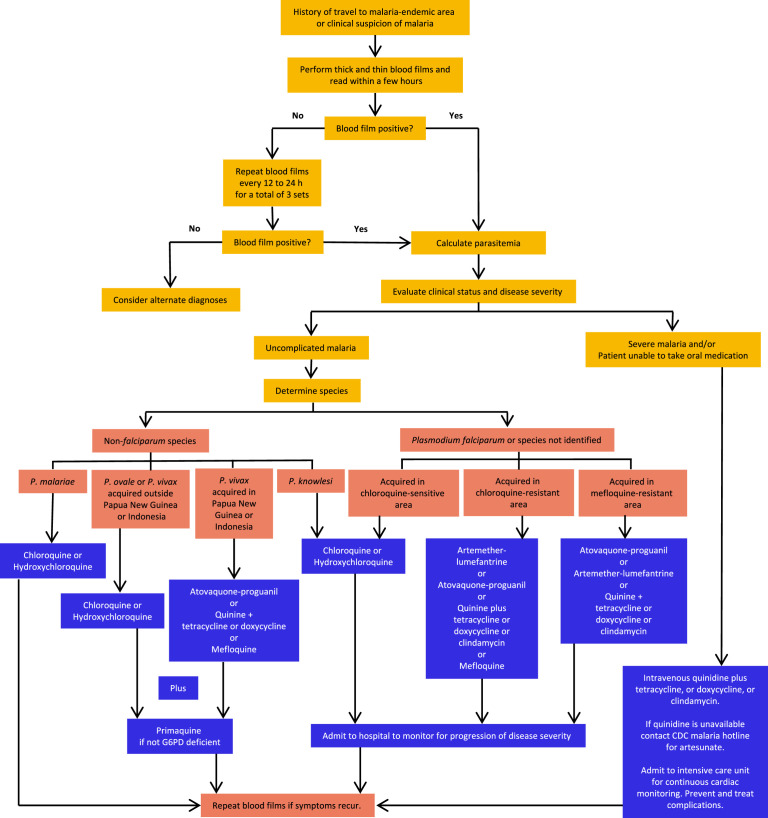
Treatment of malaria infection
Single-agent (monotherapy) approaches to malaria treatment are a major contributor to drug resistance and are not recommended.32 In general, antimalarial decision-making is based on severity of symptoms, parasite species, and likelihood of drug resistance (Fig. 3 ). Uncomplicated P falciparum (or unknown malaria species) infection is effectively treated with a 3-day regimen of ACT, which combines the fast-acting artemisinin derivative with a longer-acting antimalarial partner drug. In the United States, artemether-lumefantrine (Coartem), a single orally available ACT for treatment of uncomplicated malaria, is commercially available.46
Fig. 3.
Decision-tree for malaria treatment. G6PD, glucose 6-phosphatase.
(Courtesy of CDC, Atlanta, GA. Available at: https://www.cdc.gov/malaria/resources/pdf/algorithm.pdf.)
P vivax, P ovale, P malariae, and P knowlesi infections acquired in chloroquine-susceptible endemic areas may be treated with chloroquine, otherwise treatment with an ACT is recommended.31 Importantly, for radical cure and elimination of latent liver stages, P vivax and P ovale infections must additionally be treated with a 14-day course of primaquine to prevent future relapse. Note that patients must be evaluated for the presence of glucose 6-phosphatase (G6PD) deficiency before initiation of primaquine, which can precipitate hemolytic crisis.37
Patients with severe malaria will require intensive supportive care and parenteral treatment with intravenous antimalarial treatment. Worldwide, intravenous artesunate is strongly recommended because evidence suggests improved survival compared with quinine.47 However, artesunate is not commercially available in the United States and, therefore, intravenous quinidine gluconate is the most commonly available treatment for severe malaria. Due to its arrhythmogenic cardiotoxicity, quinidine treatment requires cardiac telemetry and QTc monitoring.31 As of 2007, intravenous artesunate, produced following Good Manufacturing Practices, has been made available on an emergency basis, through an investigational new drug protocol (FDA IND protocol # 76,725) for the treatment of severe malaria in the United States. Clinicians treating pediatric patients with severe malaria are encouraged to consult the CDC Malaria Hotline, which provides expert clinical advice and release of intravenous artesunate with severe malaria patients in whom quinidine is not appropriate.48 Additional malaria treatment guidelines and dosing specifications can be found on the CDC Web site (https://www.cdc.gov/malaria/diagnosis_treatment/treatment.html). Monotherapy for malaria is not recommended and, therefore, all cases of severe malaria require a second agent, such as tetracycline, doxycycline, or clindamycin (intravenous or oral).32, 37 There is no consensus about the efficacy of exchange blood transfusion for severe disease.32, 49, 50
A few pediatric-specific treatment modifications may be necessary for treatment of malaria in children. Pyrimethamine should be avoided in the first few weeks of life because it competes with bilirubin and may aggravate neonatal hyperbilirubinemia. Data are limited on the safety and tolerability of primaquine in young infants, which is, therefore, contraindicated in children younger than 6 months of age, and tetracyclines are contraindicated for children younger than 8 years of age. Parenteral antimalarial treatment may be required for treatment of uncomplicated malaria in children with prominent gastrointestinal symptoms, until oral administration is possible.32, 37
Best Practices.
What is the current practice?
- Pediatric malaria infection
- Best practice, guideline, and care path objectives
-
•Counsel travelers to malaria-endemic regions on the ABCs of protective measures against infection, including limiting mosquito contact and chemoprophylaxis.
-
•Consider malaria in the differential for any infant or child presenting with nonspecific febrile illness, particularly in returning travelers.
-
•Rapid recognition and diagnosis of malaria infection is necessary to prevent disease progression.
-
•Treatment of malaria depends on disease severity, Plasmodium species, and likelihood of antimalarial resistance.
-
•
What changes in current practice are likely to improve outcomes?
-
•
Improve adherence to antimalarial regimens and other prevention techniques through proper traveler education.
-
•
A travel history should be obtained for all pediatric patients presenting with fever or flu-like symptoms.
-
•
Monotherapeutic regimens that promote development of drug resistance should be avoided.
- Treatment recommendations
-
•Diagnosis depends on microscopic analysis of rapid antigen testing and thick and thin blood smears.
-
•Combination malaria treatment is based on disease severity, parasite species, and likelihood of drug resistance.
-
•For P vivax and P ovale, primaquine treatment (following G6PD testing) is necessary to prevent relapse from latent liver stages.
-
•
Summary
Properly informing travelers to malaria-endemic regions about preventative measures for infection is the most effective means of promoting adherence and preventing transmission. In the event of malaria infection, a high index of suspicion, rapid diagnosis, and immediate treatment is critical to prevent the morbidity and mortality associated with disease progression, particularly in pediatric patients.
Footnotes
Disclosures: Research funding: NIH/NIAID (AI103280, AI123808), Bill and Melinda Gates Foundation, Children’s Discovery Institute, and Dr A.R.O. John is a Burroughs Wellcome Fund Investigator in the Pathogenesis of Infectious Disease. Scientific advisory board member, Pluton Biosciences LLC (A.R.O. John).
References
- 1.Bleakley H. Malaria eradication in the Americas: A retrospective analysis of childhood exposure. Am Econ J Appl Econ. 2010;2(2):1–45. doi: 10.1257/app.2.2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva (Switzerland): 2016. World malaria report 2016. [Google Scholar]
- 3.Mace K.E., Arguin P.M. Malaria surveillance—United States, 2014. MMWR Surveill Summ. 2017;66:1–24. doi: 10.15585/mmwr.ss6612a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Armed Forces Health Surveillance Branch Update: malaria, US armed forces, 2015. MSMR. 2016;23(1):2. [PubMed] [Google Scholar]
- 5.Hwang J., Cullen K.A., Kachur S.P. Severe morbidity and mortality risk from malaria in the United States, 1985–2011. Open Forum Infectious Diseases. 2014;1(1):ofu034. doi: 10.1093/ofid/ofu034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Tourism Organization . World Tourism Organization; Madrid (Spain): 2015. UNWTO World Tourism Highlights, 2015 edition.https://www.e-unwto.org/doi/book/10.18111/9789284416899 Available at: [Google Scholar]
- 7.Phillips M.A., Burrows J.N., Manyando C. Malaria. Nat Rev Dis Primers. 2017;3:17050. doi: 10.1038/nrdp.2017.50. [DOI] [PubMed] [Google Scholar]
- 8.Cowman A.F., Healer J., Marapana D. Malaria: biology and disease. Cell. 2016;167(3):610–624. doi: 10.1016/j.cell.2016.07.055. [DOI] [PubMed] [Google Scholar]
- 9.Markus M.B. Malaria relapse. In: Mehlhorn H., editor. Encyclopedia of parasitology. Springer-Verlag; Berlin: 2016. pp. 1–3. [Google Scholar]
- 10.Chu C.S., White N.J. Management of relapsing Plasmodium vivax malaria. Expert Rev Anti Infect Ther. 2016;14(10):885–900. doi: 10.1080/14787210.2016.1220304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dondorp A.M., Kager P.A., Vreeken J. Abnormal blood flow and red blood cell deformability in severe malaria. Parasitol Today. 2000;16(6):228–232. doi: 10.1016/s0169-4758(00)01666-5. [DOI] [PubMed] [Google Scholar]
- 12.Miller L.H., Ackerman H.C., Su X.Z. Malaria biology and disease pathogenesis: insights for new treatments. Nat Med. 2013;19(2):156–167. doi: 10.1038/nm.3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Studies IIfS . Routledge; 2015. The IISS armed conflict survey: ACS, the Worldwide review of political, military and humanitarian trends in current conflicts.https://www.iiss.org/en/publications/acs/by%20year/armed-conflict-survey-2015-46e5 Available at: [Google Scholar]
- 14.Maitland K. Severe malaria in African children—the need for continuing investment. N Engl J Med. 2016;375(25):2416–2417. doi: 10.1056/NEJMp1613528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newby G., Bennett A., Larson E. The path to eradication: a progress report on the malaria-eliminating countries. Lancet. 2016;387(10029):1775–1784. doi: 10.1016/S0140-6736(16)00230-0. [DOI] [PubMed] [Google Scholar]
- 16.Olliaro P. Drug resistance hampers our capacity to roll back malaria. Clin Infect Dis. 2005;41(Supplement_4):S247–S257. doi: 10.1086/430785. [DOI] [PubMed] [Google Scholar]
- 17.Tu Y. Artemisinin—a gift from traditional Chinese medicine to the world (Nobel lecture) Angew Chem Int Ed. 2015;55:2–19. doi: 10.1002/anie.201601967. [DOI] [PubMed] [Google Scholar]
- 18.Bosman A., Mendis K.N. A major transition in malaria treatment: the adoption and deployment of artemisinin-based combination therapies. Am J Trop Med Hyg. 2007;77(6_Suppl):193–197. [PubMed] [Google Scholar]
- 19.Ashley E.A., Dhorda M., Fairhurst R.M. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371(5):411–423. doi: 10.1056/NEJMoa1314981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woodrow C.J., White N.J. The clinical impact of artemisinin resistance in Southeast Asia and the potential for future spread. FEMS Microbiol Rev. 2016;41(1):34–48. doi: 10.1093/femsre/fuw037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tatem A.J., Jia P., Ordanovich D. The geography of imported malaria to non-endemic countries: a meta-analysis of nationally reported statistics. Lancet Infect Dis. 2017;17(1):98–107. doi: 10.1016/S1473-3099(16)30326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mier-y-Teran-Romero L., Tatem A.J., Johansson M.A. Mosquitoes on a plane: Disinsection will not stop the spread of vector-borne pathogens, a simulation study. PLoS Negl Trop Dis. 2017;11(7):e0005683. doi: 10.1371/journal.pntd.0005683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Velasco E., Gomez-Barroso D., Varela C. Non-imported malaria in non-endemic countries: a review of cases in Spain. Malar J. 2017;16(1):260. doi: 10.1186/s12936-017-1915-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee E.H., Adams E.H., Madison-Antenucci S. Healthcare-Associated Transmission of Plasmodium falciparum in New York City. Infect Control Hosp Epidemiol. 2016;37(1):113–115. doi: 10.1017/ice.2015.236. [DOI] [PubMed] [Google Scholar]
- 25.Ruiz A.I.M., Bendicho A.I., Fuster J.L. Unexplained Anemia in a young infant due to congenital malaria. Pediatr Infect Dis J. 2016;35(4):468. doi: 10.1097/INF.0000000000001046. [DOI] [PubMed] [Google Scholar]
- 26.Holtzclaw A., Mrsic Z., Managbanag J. Transfusion-transmitted malaria not preventable by current blood donor screening guidelines: a case report. Transfusion. 2016;56(9):2221–2224. doi: 10.1111/trf.13680. [DOI] [PubMed] [Google Scholar]
- 27.Oakley M.S., Gerald N., McCutchan T.F. Clinical and molecular aspects of malaria fever. Trends Parasitol. 2011;27(10):442–449. doi: 10.1016/j.pt.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Ladhani S., Aibara R.J., Riordan F.A.I. Imported malaria in children: a review of clinical studies. Lancet Infect Dis. 2007;7(5):349–357. doi: 10.1016/S1473-3099(07)70110-X. [DOI] [PubMed] [Google Scholar]
- 29.Gutman J., Guarner J. Pediatric malaria: 8-year case series in Atlanta, Georgia, and review of the literature. J Travel Med. 2010;17(5):334–338. doi: 10.1111/j.1708-8305.2010.00434.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trampuz A., Jereb M., Muzlovic I. Clinical review: severe malaria. Crit Care. 2003;7(4):315. doi: 10.1186/cc2183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Griffith K.S., Lewis L.S., Mali S. Treatment of malaria in the United States: a systematic review. JAMA. 2007;297(20):2264–2277. doi: 10.1001/jama.297.20.2264. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization . World Health Organization; 2015. Guidelines for the treatment of malaria. [Google Scholar]
- 33.Collins W.E., Jeffery G.M. Plasmodium malariae: parasite and disease. Clin Microbiol Rev. 2007;20(4):579–592. doi: 10.1128/CMR.00027-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox-Singh J., Davis T.M., Lee K.-S. Plasmodium knowlesi malaria in humans is widely distributed and potentially life threatening. Clin Infect Dis. 2008;46(2):165–171. doi: 10.1086/524888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hahn W.O., Pottinger P.S. Malaria in the traveler: how to manage before departure and evaluate upon return. Med Clin North Am. 2016;100(2):289–302. doi: 10.1016/j.mcna.2015.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization . World Health Organization; 2010. International travel and health: situation as on 1 January 2010. [Google Scholar]
- 37.Kimberlin D., Brady M., Jackson M. American Academy of Pediatrics; Elk Grove Village (IL): 2015. Red book. 2015 Report of the Committee on Infectious Diseases. [Google Scholar]
- 38.Itoh M., Arguin P.M. A conversation about chemoprophylaxis. Travel Med Infect Dis. 2016;14(5):434. doi: 10.1016/j.tmaid.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 39.Kotwal R.S., Wenzel R.B., Sterling R.A. An outbreak of malaria in US army rangers returning from Afghanistan. JAMA. 2005;293(2):212–216. doi: 10.1001/jama.293.2.212. [DOI] [PubMed] [Google Scholar]
- 40.Wiese L., Bruun B., Bæk L. Bedside diagnosis of imported malaria using the Binax Now malaria antigen detection test. Scand J Infect Dis. 2006;38(11–12):1063–1068. doi: 10.1080/00365540600818011. [DOI] [PubMed] [Google Scholar]
- 41.Stauffer W.M., Cartwright C.P., Olson D.A. Diagnostic performance of rapid diagnostic tests versus blood smears for malaria in US clinical practice. Clin Infect Dis. 2009;49(6):908–913. doi: 10.1086/605436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bell D., Wongsrichanalai C., Barnwell J.W. Ensuring quality and access for malaria diagnosis: how can it be achieved? Nat Rev Microbiol. 2006;4(9):682. doi: 10.1038/nrmicro1474. [DOI] [PubMed] [Google Scholar]
- 43.Bell D., Peeling R.W. WHO-Regional Office for the Western Pacific/TDR. Evaluation of rapid diagnostic tests: malaria. Nat Rev Microbiol. 2006;4:S34–S38. doi: 10.1038/nrmicro1524. [DOI] [PubMed] [Google Scholar]
- 44.Rubio J., Buhigas I., Subirats M. Limited level of accuracy provided by available rapid diagnosis tests for malaria enhances the need for PCR-based reference laboratories. J Clin Microbiol. 2001;39(7):2736–2737. doi: 10.1128/JCM.39.7.2736-2737.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Walk J., Schats R., Langenberg M.C. Diagnosis and treatment based on quantitative PCR after controlled human malaria infection. Malar J. 2016;15(1):398. doi: 10.1186/s12936-016-1434-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gray A.M., Arguin P.M., Hamed K. Surveillance for the safety and effectiveness of artemether-lumefantrine in patients with uncomplicated Plasmodium falciparum malaria in the USA: a descriptive analysis. Malar J. 2015;14(1):349. doi: 10.1186/s12936-015-0881-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dondorp A.M., Fanello C.I., Hendriksen I.C. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet. 2010;376(9753):1647–1657. doi: 10.1016/S0140-6736(10)61924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Twomey P.S., Smith B.L., McDermott C. Intravenous artesunate for the treatment of severe and complicated malaria in the United States: clinical use under an investigational new drug protocol intravenous artesunate for severe malaria. Ann Intern Med. 2015;163(7):498–506. doi: 10.7326/M15-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tan K.R., Wiegand R.E., Arguin P.M. Exchange transfusion for severe malaria: evidence base and literature review. Clin Infect Dis. 2013;57(7):923–928. doi: 10.1093/cid/cit429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shaz B.H., Schwartz J., Winters J.L. American society for apheresis guidelines support use of red cell exchange transfusion for severe malaria with high parasitemia. Clin Infect Dis. 2014;58(2):302–303. doi: 10.1093/cid/cit662. [DOI] [PubMed] [Google Scholar]