Health disparities are a major problem in the United States: many conditions, including cardiovascular disease, diabetes, and Alzheimer’s disease, disproportionately affect racial and ethnic minorities and the socioeconomically disadvantaged.1–5 Few interventions have successfully reduced these disparities.
Poor and minority populations often live in socioeconomically disadvantaged neighborhoods, and neighborhood context directly affects access to food, safety, education, health behaviors, and stress levels. 1–5 Living in a disadvantaged neighborhood has been linked to higher rates of diabetes, cardiovascular disease, and other diseases; increased utilization of health services; and earlier death. 1–5 Moreover, neighborhood disadvantage may influence health independently of a person’s socioeconomic status: studies have suggested that poor people who live in wealthier neighborhoods may have better health outcomes than poor people who live in extremely disadvantaged neighborhoods.2,5
Health interventions and policies that don’t account for neighborhood disadvantage may be ineffective or provide only limited benefit.1 For example, a diabetes education program will do little to reduce disparities in diabetes control if participants live in substandard housing and lack access to a refrigerator for insulin storage. In such cases, the most effective solution involves addressing the fundamental issue of neighborhood disadvantage — and improving housing quality — rather than merely providing education about diabetes.
There is increasing interest in assessing neighborhood disadvantage on a national scale to support research, policy, and health interventions. Better understanding of variations in neighborhood disadvantage could lead to improved insight into the sociobiologic mechanisms that underlie health disparities, which could, in turn, facilitate the development of improved therapeutics and interventions. Neighborhood disadvantage is difficult to quantify, however, particularly for people who lack the necessary technical skills to make use of the complex national geospatial data sources that house this information. Until now, access to such information has largely been limited to geospatial analysts and has been out of practical reach for most other researchers, policymakers, patients, caregivers, and frontline health and social service personnel.
To improve access and facilitate broad application, a neighborhood-disadvantage metric should be inclusive of all U.S. neighborhoods, regularly updated, rigorously tested for validity, easily accessible, and constructed to meet the needs of a range of possible users. Data should be available on the neighborhood or Census block-group level. Such a metric might be applicable to a wide variety of research and health policy efforts, including research into fundamental sociobiologic mechanisms of disease and initiatives to better align resources with needs.
One measure that meets these criteria is the area deprivation index (ADI). Originally created by the U.S. Health Resources and Services Administration nearly 3 decades ago, the ADI is composed of 17 education, employment, housing-quality, and poverty measures originally drawn from long-form Census data and updated by our team to incorporate more recent American Community Survey (ACS) data.3 The ADI has the same limitations as ACS and Census data, including limited accounting for undocumented-immigrant populations. However, there has been extensive research on the ADI, and our updated index has now been validated for a range of health outcomes and disease domains for use at the neighborhood level.3,4
To make neighborhood-disadvantage metrics more accessible to policymakers, researchers, patients, caregivers, and clinicians, we are making the ACS-derived ADI for the United States and Puerto Rico freely available to the public. We have constructed a detailed cross reference of over 69 million nine-digit Zip Codes to allow this index to be merged with a wide variety of other data resources in an attempt to promote increased understanding of the ways in which neighborhood disadvantage affects health. Data are available for download on the University of Wisconsin School of Medicine and Public Health’s Neighborhood Atlas website (www.neighborhoodatlas.medicine.wisc.edu). The Neighborhood Atlas will be maintained and regularly updated with funding provided by the school and the National Institutes of Health (NIH Grants R01MD010243 and RF1AG057784).
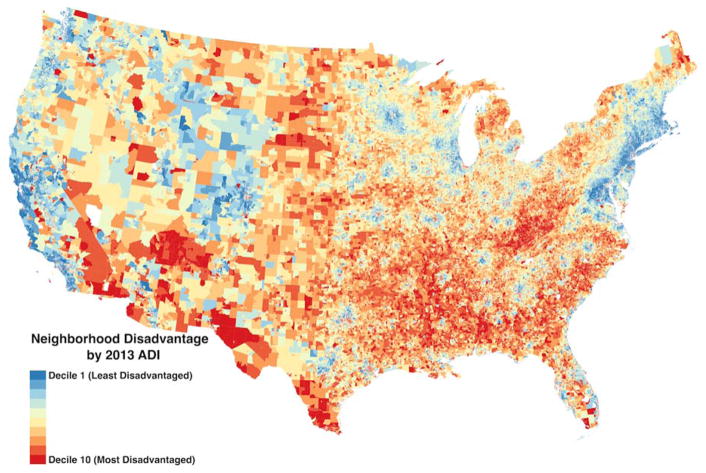
This new online platform allows users to visualize neighborhood disadvantage on a local, city, state, or national level by means of a customized mapping interface similar to that used in many popular smartphone navigation apps. The neighborhood disadvantage of a particular area can be ranked against that of other areas in the same state or throughout the country. Addresses can be entered directly into the tool to elucidate neighborhood disadvantage around specific geographic points. An advanced degree is not required to download, understand, or use this information. The map shows the distribution of neighborhood disadvantage throughout the United States (inner-city neighborhoods are difficult to see because of their relatively small geographic size).
U.S. Neighborhood Disadvantage in 2013, by Area Deprivation Index Deciles.
Multiple academic, health system, and state and federal collaborators are already using the Neighborhood Atlas and the granular data it contains to inform research, outreach, and policy. Going forward, health systems and payers could use Atlas data to better understand and invest in social factors that affect health in their populations. For example, the Everyone with Diabetes Counts program, a national disparities-reduction program within the Centers for Medicare and Medicaid Services, is using Atlas data to inform ground-level operations and strategies for more efficiently reaching disadvantaged populations. The tool could also be used to catalyze new partnerships among communities, health systems, and governments to advocate for policies addressing the social factors that influence health — such as affordable and safe housing, residential segregation, and transportation — in specific highly disadvantaged neighborhoods. Multiple state-based public health organizations and health systems are already employing Neighborhood Atlas data for this purpose.
Policymakers and payers could use Atlas data to inform risk-adjustment strategies, financial incentives, payment reform, infrastructure targeting, benefits decisions, and program eligibility. For example, the Maryland Health Services Cost Review Commission, the state’s all-payer hospital rate-setting authority, is using these metrics in its decisions regarding hospital-level quality measurement and policy. The Atlas could also be harnessed to advance disparities-focused research. Data could be used to inform study design, recruitment and retention of participants, and analysis and dissemination of results for translational, clinical, and community-based research.
The Neighborhood Atlas makes neighborhood-disadvantage metrics accessible to everyone. We hope that improving the accessibility of these data will catalyze the kinds of policy efforts, research studies, resource alignment, and clinical interventions that are desperately needed in order to eliminate health disparities in the United States.
Supplementary Material
Footnotes
Disclosure forms provided by the authors are available at NEJM.org.
References
- 1.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995:80–94. [PubMed] [Google Scholar]
- 2.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes — a randomized social experiment. N Engl J Med. 2011;365:1509–19. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kind AJ, Jencks S, Brock J, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765–74. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lantos PM, Hoffman K, Permar SR, Jackson P, Hughes BL, Kind A, Swamy G. Neighborhood disadvantage is associated with high cytomegalovirus seroprevalence in pregnancy. J Racial Ethn Health Disparities. 2017:1–5. doi: 10.1007/s40615-017-0423-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu J, Kind AJ, Nerenz D. Area deprivation index predicts readmission risk at an urban teaching hospital. Am J Med Qual. 2018 doi: 10.1177/1062860617753063. doi:1062860617753063. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.