Abstract
OBJECTIVE
Reductions in heart attack and stroke hospitalizations are well documented in the U.S. population with diabetes. We extended trend analyses to other cardiovascular disease (CVD) conditions, including stroke by type, and used four additional years of data.
RESEARCH DESIGN AND METHODS
Using 1998–2014 National (Nationwide) Inpatient Sample data, we estimated the number of discharges having acute coronary syndrome (ACS) (ICD-9 codes 410–411), cardiac dysrhythmia (427), heart failure (428), hemorrhagic stroke (430–432), or ischemic stroke (433.x1, 434, and 436) as first-listed diagnosis and diabetes (250) as secondary diagnosis. Hospitalization rates for adults aged ≥35 years were calculated using estimates from the population with and the population without diabetes from the National Health Interview Survey and age-adjusted to the 2000 U.S. standard population. Joinpoint regression was used to analyze trends and calculate an average annual percentage change (AAPC) with 95% confidence limits (CLs).
RESULTS
From 1998 to 2014, in the population with diabetes, age-adjusted hospitalization rates declined significantly for ACS (AAPC −4.6% per year [95% CL −5.3, −3.8]), cardiac dysrhythmia (−0.7% [−1.1, −0.2]), heart failure (−3.6% [ −4.6, −2.7]), hemorrhagic stroke (−1.1% [−1.4, −0.7]), and ischemic stroke (−2.9% [−3.9, −1.8]). In the population without diabetes, rates also declined significantly for these conditions, with the exception of dysrhythmia. By 2014, rates in the population with diabetes population remained two to four times as high as those for the population without diabetes, with the largest difference in heart failure rates.
CONCLUSIONS
CVD hospitalization rates declined significantly in both the population with diabetes and the population without diabetes. This may be due to several factors, including new or more aggressive treatments and reductions in CVD risk factors and CVD incidence.
Diabetes is a major cause of cardiovascular disease (CVD) and a leading cause of blindness, kidney failure, and lower-limb amputations among adults (1–5). For every four adults with diagnosed diabetes, three have high blood pressure, a risk factor for CVD (1). Compared with people without diabetes, the risk for stroke is approximately two to four times as high and CVD death rates are about two times as high among people with diabetes (6,7).
Recent national data have documented reductions in mortality due to all-cause and CVD in the population with diabetes as well as improvements in several diabetes-related complications such as lower-limb amputations, kidney failure, acute myocardial infarction (AMI), and stroke (7,8). Of these complications, the largest absolute declines in rates between 1990 and 2010 were observed for AMI and stroke hospitalizations (8). These reports documenting improvements in diabetes-related morbidity and mortality are encouraging and may be due in part to improvements in the health of people with diabetes, including earlier diagnosis (9), better control of risk factors for complications (e.g., hyperglycemia and high blood pressure) (10,11), and improvements in quality of care and medical treatments (12). However, a recent study of CVD hospitalizations in the population with diabetes was limited in the number of CVD conditions examined (i.e., AMI and stroke) and did not examine stroke by type (8). We extended the analysis to other CVD conditions, including stroke by type, and used four additional years of data. We assessed whether disparities in rates between the population with diabetes and the population without diabetes were reduced or continued to persist, and in the population with diabetes, we looked at trends in hospitalizations by age, sex, and race/ethnicity.
RESEARCH DESIGN AND METHODS
We estimated the number of hospital discharges due to various CVD conditions among persons with and without diagnosed diabetes using 1998–2014 data from the National (Nationwide) Inpatient Sample (NIS) of the Agency for Healthcare Research and Quality (13,14). NIS contains information from >7 million hospital stays each year from 44 states participating in the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project, estimating >35 million hospitalizations nationally and representing >95% of the U.S. population. The NIS was redesigned in 2012; a more detailed description of the NIS is available (13,14). Data collected include information on patients’ age, race, sex, length of stay, and 15 diagnoses (one primary and 14 secondary diagnoses). Hospitalizations for all individuals were included regardless of discharge disposition (i.e., whether the patient was discharged alive or died during the hospitalization). We identified discharges for which the first-listed diagnosis was acute coronary syndrome (ACS) (ICD-9 codes 410–411), cardiac dysrhythmia (427), heart failure (428), or stroke (430–432, 433.x1, 434, and 436). Codes for ACS include AMI, angina, and coronary atherosclerosis; codes for cardiac dysrhythmia include cardiac arrest. Stroke discharges were subdivided into hemorrhagic stroke (430–432) and ischemic stroke (433.x1, 434, and 436); transient cerebral ischemia (435) was not included. The discharges were considered to be diabetes-related if diabetes (250) was listed as a secondary diagnosis.
Estimates of the population with and the population without diagnosed diabetes were obtained from the 1998–2014 National Health Interview Survey (NHIS). Conducted continuously since 1957, the NHIS is a health survey of the civilian, non-institutionalized, household population of the U.S. The multistage probability design of the survey has previously been described (15).The survey provides information on the health of the U.S. population, including information on the prevalence and incidence of disease, the extent of disability, and the use of health care services. For gathering information about diagnosed diabetes, respondents were asked whether they had ever been told by a doctor or health professional that they had diabetes or sugar diabetes (other than during pregnancy for women).
We calculated CVD-specific hospitalization rates per 1,000 population (with diabetes or without diabetes) by dividing the estimated number of discharges with and discharges without diagnosed diabetes from NIS by the estimated populations with and population without diagnosed diabetes from NHIS. We compared overall trends in hospitalization rates for ACS, heart failure, cardiac dysrhythmia, and hemorrhagic and ischemic stroke by diabetes status. Among those with diagnosed diabetes, we also examined trends by age (35–54, 55–74, and ≥75 years), sex, and race/ethnicity (non-Hispanic whites, non-Hispanic blacks, and Hispanics). We restricted our analysis to discharge records of patients aged ≥35 years because of the smaller sample size of these CVD conditions among people, <35 years old. People of “other races” and people with missing race/ethnicity data were excluded only from the race/ethnicity-specific analysis in the population with diabetes. In NIS, during the study period, missing race/ethnicity data in the population with diabetes ranged from 1 to 4%.
We used SUDAAN 11 (SAS callable) software (Research Triangle Institute, Research Triangle Park, NC) to obtain point estimates and SEs based on the Taylor series linearization method and to account for the complex sampling designs of the two surveys. We adjusted rates to the 2000 U.S. standard population using age-groups (35–54, 55–74, and ≥75 years), used the χ2 test to determine whether differences in hospitalization rates between various subgroups were significant, and calculated annual CVD-specific hospitalization rate ratios by dividing the diabetes-related rates by the non–diabetes-related rates.
To analyze trends in hospitalization rates, we used Joinpoint regression software (version 4.3.1.0; Statistical Methodology and Applications Branch and Data Modeling Branch, Surveillance Research Program, National Cancer Institute). Joinpoint regression uses permutation tests to identify points where linear trends change significantly in either direction or magnitude. Each trend segment is described by an annual percentage change (APC) and the trend for the entire study period is described by the average annual percentage change (AAPC), which is a summary measure of trend accounting for transitions within each trend segment. Both trend measures, with corresponding 95% confidence limits (CLs), were tested to determine whether the change was significantly different from 0, and results were considered statistically significant with a two-sided P value <0.05. The Figures show observed rates (symbols) and modeled trends (lines).
RESULTS
CVD-Specific Hospitalization Rates by Diabetes Status
From 1998 to 2014, in both the population with and the population without diabetes, trends in age-adjusted hospitalization rates declined significantly for ACS, heart failure, and hemorrhagic and ischemic stroke (Table 1). However, throughout the period, rates for cardiac dysrhythmia hospitalization declined significantly only in the population with diabetes (AAPC −0.7% per year [95% CL −1.1, −0.2], P = 0.004) (Table 1).
Table 1.
Age-adjusted hospital discharge rates and trend analysis of selected CVD conditions among people aged ≥35 years with and without diagnosed diabetes (U.S., 1998–2014)
| Rate (95% CL)* | Rate difference (95% CL) |
Overall trend | Trend segment 1† | Trend segment 2/3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| 1998 | 2014 | AAPC (95% CL) | P | Period | APC (95% CL) | P | Period | APC (95% CL) | P | ||
| ACS | |||||||||||
| Diabetes | 19.2 (17.5, 20.9) | 9.4 (8.8, 10.0) | −9.9 (−11.7, −8.0) | −4.6 (−5.3, −3.8) | <0.001 | 1998–2009 | −6.8 (−7.5, −6.1) | <0.001 | 2009–2014 | 0.5 (−1.6, 2.7) | 0.60 |
| No diabetes | 5.6 (5.2, 6.0) | 2.7 (2.6, 2.8) | −2.8 (−3.2, −2.4) | −4.4 (−5.4, −3.4) | <0.001 | 1998–2001 | −1.8 (−5.8, 2.4) | 0.34 | 2001–2007 | −6.8 (−8.8, −4.9) | <0.001 |
|
| |||||||||||
| 2007–2014 | −3.3 (−4.3, −2.3) | <0.001 | |||||||||
|
| |||||||||||
| Cardiac dysrhythmia | |||||||||||
| Diabetes | 7.4 (6.8, 8.0) | 6.7 (6.3, 7.1) | −0.7 (−1.4, 0.1) | −0.7 (−1.1, −0.2) | 0.004 | 1998–2014 | −0.7 (−1.1, −0.2)‡ | 0.004 | |||
| No diabetes | 4.1 (3.8, 4.3) | 3.3 (3.1, 3.4) | −0.8 (−1.1, −0.6) | −1.2 (−3.1, 0.8) | 0.23 | 1998–2001 | 4.8 (−0.4, 10.1) | 0.06 | 2001–2004 | −3.6 (−13.3, 7.3) | 0.44 |
|
| |||||||||||
| 2004–2011 | −0.0 (−1.9, 2.0) | 1.00 | |||||||||
|
| |||||||||||
| 2011–2014 | −7.2 (−10.3, −4.0) | 0.002 | |||||||||
|
| |||||||||||
| Heart failure | |||||||||||
| Diabetes | 25.9 (23.8, 28.0) | 14.5 (13.7, 15.4) | −11.4 (−13.7, −9.1) | −3.6 (−4.6, −2.7) | <0.001 | 1998–2003 | −1.7 (−3.7, 0.4) | 0.10 | 2003–2010 | −6.3 (−7.8, −4.9) | <0.001 |
| 2010–2014 | −1.3 (−3.5, 1.1) | 0.25 | |||||||||
| No diabetes | 5.4 (5.1, 5.8) | 3.5 (3.4, 3.7) | −1.9 (−2.2, −1.6) | −2.6 (−3.2, −2.0) | <0.001 | 1998–2004 | −1.1 (−2.5, 0.3) | 0.12 | 2004–2014 | −3.5 (−4.1, −2.9) | <0.001 |
|
| |||||||||||
| Hemorrhagic stroke | |||||||||||
| Diabetes | 1.4 (1.3, 1.6) | 1.1 (1.0, 1.2) | −0.3 (−0.5, −0.1) | −1.1 (−1.4, −0.7) | <0.001 | 1998–2014 | −1.1 (−1.4, −0.7)‡ | <0.001 | |||
| No diabetes | 0.8 (0.8, 0.9) | 0.6 (0.6, 0.7) | −0.2 (−0.3, −0.1) | −1.5 (−1.8, −1.1) | <0.001 | 1998–2014 | −1.5 (−1.8, −1.1)‡ | <0.001 | |||
|
| |||||||||||
| Ischemic stroke | |||||||||||
| Diabetes | 10.6 (9.7, 11.4) | 6.6 (6.2, 7.0) | −4.0 (−4.9, −3.0) | −2.9 (−3.9, −1.8) | <0.001 | 1998–2005 | −7.0 (−7.9, −6.0) | <0.001 | 2005–2009 | −2.8 (−6.9, 1.5) | 0.17 |
| 2009–2014 | 3.1 (1.6, 4.7) | 0.001 | |||||||||
| No diabetes | 3.1 (2.9, 3.2) | 2.1 (2.0, 2.2) | −1.0 (−1.2, −0.8) | −2.3 (−2.7, −1.9) | <0.001 | 1998–2006 | −4.5 (−5.1, −3.8) | <0.001 | 2006–2014 | −0.1 (−0.7, 0.6) | 0.80 |
Per 1,000 population with diabetes for diabetes-related discharge rates or per 1,000 population without diabetes for non–diabetes-related discharge rates and age-adjusted based on the 2000 U.S. standard population.
Trend segment identified by Joinpoint regression.
APC = AAPC (i.e., trend had 0 joinpoints).
Although throughout the period, with the exception of cardiac dysrhythmia rates in the population without diabetes, hospitalization rates for these CVD conditions declined significantly in both populations, in several instances the trend in the latter part of the period was different from the overall trend (Table 1). In the population with diabetes, rates leveled off for ACS (from 2009 to 2014) and for heart failure (from 2010 to 2014). Rates for ischemic stroke increased significantly (APC 3.1% per year [95% CL 1.6, 4.7], P = 0.001) in the population with diabetes (from 2009 to 2014) and leveled off in the population without diabetes (from 2006 to 2014). On the other hand, in the population without diabetes, although rates for cardiac dysrhythmia showed no significant change from 1998 to 2014, rates from 2011 to 2014 declined significantly (APC −7.2% per year [−10.3, −4.0], P = 0.002) (Table 1).
From 1998 to 2014, the AAPCs in hospitalization rates were similar between the population with diabetes and the population without diabetes: for ACS, −4.6% per year (95% CL −5.3, −3.8) vs. −4.4% (−5.4, −3.4), respectively; for cardiac dysrhythmia, −0.7% per year (−1.1, −0.2) vs. −1.2% (−3.1, 0.8); for heart failure −3.6% per year (−4.6, −2.7) vs. −2.6% (−3.2, −2.0); for hemorrhagic stroke, −1.1% per year (−1.4, −0.7) vs. −1.5% (−1.8, −1.1); and for ischemic stroke, −2.9% per year (−3.9, −1.8) vs. −2.3% (−2.7, −1.9). However, despite these similar average rates of decline in both populations, compared with 1998, hospitalization rates in 2014 for these CVD conditions continued to be approximately two to four times higher in the population with diabetes than in the population without diabetes, with the largest relative difference (4.1 times) in heart failure rates.
CVD-Specific Hospitalizations in the Population With Diabetes
By Age
In 2014, in the population with diabetes, hospitalization rates for all CVD conditions studied were higher in the older population than in the younger population (Table 2). The greater differences between those older and those younger were in rates for cardiac dysrhythmia (6.6 times) and for heart failure (6.0 times).
Table 2.
Hospital discharge rates and trend analysis of selected CVD conditions among people aged ≥35 years with diagnosed diabetes, by age-group, sex, and race/ethnicity (U.S., 1998–2014)
| Rate (95% CL)* | Rate difference (95% CL) |
Overall trend | Trend segment 1† | Trend segment 2/3/4 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| 1998 | 2014 | AAPC (95% CL) | P | Period | APC (95% CL) | P | Period | APC (95% CL) | P | ||
| ACS | |||||||||||
| Age (years) | |||||||||||
| 35–54 | 11.3 (9.9, 12.7) | 6.9 (6.2, 7.6) | −4.4 (−6.0, −2.8) | −3.2 (−4.3, −2.0) | <0.001 | 1998–2009 | −5.6 (−6.7, −4.4) | <0.001 | 2009–2014 | 2.4 (−1.1, 6.0) | 0.16 |
| 55–74 | 24.4 (21.9, 26.9) | 10.3 (9.6, 11.0) | −14.1 (−16.7, −11.5) | −5.2 (−6.0, −4.5) | <0.001 | 1998–2009 | −7.6 (−8.4, −6.9) | <0.001 | 2009–2014 | 0.3 (−2.0, 2.5) | 0.80 |
| ≥75 | 44.8 (38.3, 51.3) | 19.5 (17.3, 21.6) | −25.3 (−32.2, −18.5) | −5.5 (−6.6, −4.4) | <0.001 | 1998–2010 | −7.1 (−8.0, −6.2) | <0.001 | 2010–2014 | −0.6 (−4.9, 3.9) | 0.77 |
| Sex | |||||||||||
| Men | 22.9 (20.4, 25.4) | 11.4 (10.5, 12.4) | −11.5 (−14.2, −8.8) | −4.2 (−5.1, −3.4) | <0.001 | 1998–2009 | −6.5 (−7.4, −5.7) | <0.001 | 2009–2014 | 1.1 (−1.4, 3.6) | 0.36 |
| Women | 15.9 (14.3, 17.6) | 7.4 (6.8, 7.9) | −8.6 (−10.3, −6.9) | −4.6 (−6.2, −3.0) | <0.001 | 1998–2002 | −2.9 (−5.5, −0.1) | 0.04 | 2002–2005 | −12.3 (−19.5, −4.6) | 0.009 |
| 2005–2010 | −5.1 (−7.8, −2.3) | 0.005 | |||||||||
| 2010–2014 | 0.4 (−2.0, 2.8) | 0.73 | |||||||||
| Race/ethnicity | |||||||||||
| NH white | 16.7 (14.6, 18.7) | 10.0 (9.2, 10.8) | −6.7 (−8.9, −4.5) | −3.2 (−4.9, 1.6) | <0.001 | 1998–2005 | −9.1 (−10.5, −7.6) | <0.001 | 2005–2009 | −1.9 (−8.4, 5.0) | 0.54 |
| 2009–2014 | 4.5 (2.1, 6.9) | 0.002 | |||||||||
| NH black | 11.7 (8.8, 14.5) | 7.9 (6.8, 8.9) | −3.8 (−6.8, −0.8) | −2.0 (−4.3, 0.2) | 0.08 | 1998–2007 | −6.2 (−9.3, −2.9) | 0.002 | 2007–2014 | 3.5 (−0.5, 7.7) | 0.08 |
| Hispanic | 11.6 (8.2, 15.0) | 6.3 (5.3, 7.3) | −5.2 (−8.8, −1.7) | −4.0 (−5.3, −2.6) | <0.001 | 1998–2014 | −4.0 (−5.3, −2.6)‡ | <0.001 | |||
|
| |||||||||||
| Cardiac dysrhythmia | |||||||||||
| Age (years) | |||||||||||
| 35–54 | 2.8 (2.4, 3.1) | 3.2 (2.8, 3.5) | 0.4 (−0.1, 0.9) | 0.8 (0.1, 1.5) | 0.03 | 1998–2014 | 0.8 (0.1, 1.5)‡ | 0.03 | |||
| 55–74 | 10.1 (9.1, 11.1) | 8.0 (7.5, 8.5) | −2.1 (−3.3, −1.0) | −1.3 (−1.8, −0.9) | <0.001 | 1998–2014 | −1.3 (−1.8, −0.9)‡ | <0.001 | |||
| ≥75 | 23.3 (20.0, 26.6) | 21.0 (18.7, 23.3) | −2.3 (−6.3, 1.8) | −0.8 (−1.5, −0.2) | 0.02 | 1998–2014 | −0.8 (−1.5, −0.2)‡ | 0.02 | |||
| Sex | |||||||||||
| Men | 8.1 (7.2, 9.0) | 7.4 (6.9, 8.0) | −0.6 (−1.7, 0.5) | −0.2 (−0.7, 0.2) | 0.31 | 1998–2014 | −0.2 (−0.7, 0.2)‡ | 0.31 | |||
| Women | 6.9 (6.2, 7.5) | 6.0 (5.5, 6.4) | −0.9 (−1.7, −0.1) | −1.1 (−3.2, 1.1) | 0.31 | 1998–2002 | 3.0 (−0.9, 7.0) | 0.11 | 2002–2005 | −6.4 (−16.5, 5.0) | 0.21 |
| 2005–2011 | 1.3 (−1.5, 4.1) | 0.31 | |||||||||
| 2011–2014 | −5.6 (−9.9, −1.1) | 0.02 | |||||||||
| Race/ethnicity | |||||||||||
| NH white | 6.4 (5.6, 7.1) | 7.3 (6.7, 7.8) | 0.9 (0.0, 1.8) | 0.4 (−1.0, 1.9) | 0.58 | 1998–2005 | −3.2 (−5.0, −1.4) | 0.003 | 2005–2011 | 5.9 (2.5, 9.4) | 0.003 |
| 2011–2014 | −1.6 (4 −5.9, 3.0) | 0.45 | |||||||||
| NH black | 5.3 (4.0, 6.6) | 6.1 (5.3, 6.8) | 0.7 (−0.8, 2.3) | 2.2 (0.9, 3.5) | 0.002 | 1998–2014 | 2.2 (0.9, 3.5)‡ | 0.002 | |||
| Hispanic | 3.4 (2.4, 4.4) | 3.9 (3.2, 4.6) | 0.5 (−0.7, 1.7) | 0.2 (−1.1, 1.5) | 0.77 | 1998–2014 | 0.2 (−1.1, 1.5)‡ | 0.77 | |||
|
| |||||||||||
| Heart failure | |||||||||||
| Age (years) | |||||||||||
| 35–54 | 9.7 (8.5, 11.0) | 7.7 (6.9, 8.6) | −2.0 (−3.5, −0.5) | −1.3 (−3.2, 0.6) | 0.17 | 1998–2003 | 2.3 (−1.5, 6.3) | 0.20 | 2003–2009 | −6.2 (−9.8, −2.4) | 0.005 |
| 2009–2014 | 1.0 (−2.4, 4.6) | 0.51 | |||||||||
| 55–74 | 34.5 (31.3, 37.7) | 15.4 (14.4, 16.4) | −19.1 (−22.5, −15.8) | −5.0 (−5.8, −4.1) | <0.001 | 1998–2003 | −3.4 (−5.3, −1.5) | 0.003 | 2003–2010 | −7.7 (−9.0, −6.4) | <0.001 |
| 2010–2014 | −2.1 (−4.1, −0.0) | 0.048 | |||||||||
| ≥75 | 83.8 (72.0, 95.6) | 46.0 (41.0, 51.0) | −37.8 (−50.6, −25.0) | −4.4 (−5.0, −3.8) | <0.001 | 1998–2014 | −4.4 (−5.0, −3.8)‡ | <0.001 | |||
| Sex | |||||||||||
| Men | 26.3 (23.5, 29.2) | 15.7 (14.5, 17.0) | −10.6 (−13.7, −7.5) | −2.9 (−5.3, −0.5) | 0.02 | 1998–2007 | −2.6 (−3.8, −1.3) | 0.001 | 2007–2010 | −8.0 (−20.1, 6.1) | 0.22 |
| 2010–2014 | 0.1 (−3.2, 3.6) | 0.94 | |||||||||
| Women | 25.8 (23.2, 28.4) | 13.3 (12.4, 14.3) | −12.5 (−15.2, −9.7) | −4.3 (−5.9, −2.6) | <0.001 | 1998–2002 | 0.7 (−4.0, 5.7) | 0.74 | 2002–2008 | −8.5 (−11.7, −5.2) | <0.001 |
| 2008–2014 | −3.2 (−5.4, −1.0) | 0.009 | |||||||||
|
| |||||||||||
| Race/ethnicity | |||||||||||
| NH white | 19.6 (17.4, 21.7) | 12.9 (12.0, 13.9) | −6.6 (−9.0, −4.3) | −2.8 (−3.5, −2.1) | <0.001 | 1998–2007 | −5.6 (−6.6, −4.6) | <0.001 | 2007–2014 | 0.9 (−0.4, 2.2) | 0.14 |
| NH black | 25.1 (19.3, 30.8) | 22.1 (19.3, 24.9) | −3.0 (−9.4, 3.4) | −0.7 (−1.7, 0.2) | 0.12 | 1998–2014 | −0.7 (−1.7, 0.2)‡ | 0.12 | |||
| Hispanic | 14.9 (10.4, 19.3) | 9.7 (8.0, 11.3) | −5.2 (−10.0, −0.5) | −2.7 (−5.3, 0.0) | 0.053 | 1998–2003 | 6.6 (−2.3, 16.3) | 0.13 | 2003–2014 | −6.7 (−8.6, −4.7) | <0.001 |
|
| |||||||||||
| Hemorrhagic stroke | |||||||||||
| Age (years) | |||||||||||
| 35–54 | 0.6 (0.5, 0.8) | 0.7 (0.6, 0.8) | 0.0 (−0.1, 0.2) | 0.5 (−0.3, 1.3) | 0.22 | 1998–2014 | 0.5 (−0.3, 1.3)‡ | 0.22 | |||
| 55–74 | 1.7 (1.5, 1.9) | 1.1 (1.1, 1.2) | −0.6 (−0.8, −0.4) | −2.3 (−3.2, −1.4) | <0.001 | 1998–2001 | −7.3 (−12.0, −2.4) | 0.008 | 2001–2014 | −1.1 (−1.6, −0.6) | <0.001 |
| ≥75 | 4.5 (3.8, 5.1) | 3.2 (2.8, 3.6) | −1.2 (−2.0, −0.5) | −1.8 (−2.4, −1.2) | <0.001 | 1998–2014 | −1.8 (−2.4, −1.2)‡ | <0.001 | |||
| Sex | |||||||||||
| Men | 1.8 (1.6, 2.0) | 1.3 (1.1, 1.4) | −0.5 (−0.8, −0.3) | −1.8 (−3.3, 0.3) | 0.02 | 1998–2001 | −7.7 (−15.2, 0.4) | 0.06 | 2001–2014 | −0.4 (−1.2, 0.4) | 0.29 |
| Women | 1.2 (1.0, 1.3) | 1.0 (0.9, 1.1) | −0.2 (−0.4, 0.0) | −1.1 (−1.4, −0.7) | <0.001 | 1998–2014 | −1.1 (−1.4, −0.7)‡ | <0.001 | |||
| Race/ethnicity | |||||||||||
| NH white | 1.0 (0.9, 1.1) | 0.9 (0.8, 1.0) | −0.1 (−0.2, 0.1) | −0.5 (−1.3, 0.2) | 0.17 | 1998–2002 | −9.5 (−12.2, −6.7) | <0.001 | 2002–2014 | 2.6 (2.1, 3.2) | <0.001 |
| NH black | 1.4 (1.0, 1.8) | 1.4 (1.2, 1.6) | 0.0 (−0.4, 0.4) | 1.0 (−0.1, 2.2) | 0.08 | 1998–2014 | 1.0 (−0.1, 2.2)‡ | 0.08 | |||
| Hispanic | 1.0 (0.7, 1.3) | 1.0 (0.8, 1.2) | 0.0 (−0.4, 0.3) | 0.3 (−2.3, 2.8) | 0.84 | 1998–2003 | 7.7 (−0.5, 16.6) | 0.06 | 2003–2014 | −3.0 (−4.9, −1.0) | 0.006 |
|
| |||||||||||
| Ischemic stroke | |||||||||||
| Age (years) | |||||||||||
| 35–54 | 3.6 (3.2, 4.1) | 4.0 (3.6, 4.4) | 0.1 (−0.6, 0.7) | 0.5 (−0.8, 1.7) | 0.45 | 1998–2009 | −2.0 (−3.2, −0.8) | 0.003 | 2009–2014 | 6.2 (2.6, 10.0) | 0.003 |
| 55–74 | 15.2 (13.8, 16.6) | 7.3 (6.8, 7.8) | −6.5 (−7.9, −5.2) | −3.9 (−4.6, −3.2) | <0.001 | 1998–2005 | −8.6 (−9.4, −7.8) | <0.001 | 2005–2010 | −2.2 (−4.3, −0.1) | 0.04 |
| 2010–2014 | 2.6 (1.0, 4.3) | 0.005 | |||||||||
| ≥75 | 32.4 (27.8, 37.0) | 17.8 (15.8, 19.7) | −17.2 (−22.5, −11.9) | −4.6 (−5.8, −3.3) | <0.001 | 1998–2006 | −8.8 (−10.8, −6.8) | <0.001 | 2006–2014 | −0.1 (−2.1, 2.0) | 0.93 |
| Sex | |||||||||||
| Men | 11.1 (9.9, 12.3) | 6.9 (6.3, 7.4) | −4.2 (−5.6, −2.9) | −2.9 (−4.3, −1.6) | <0.001 | 1998–2001 | −11.7 (−17.1, −6.1) | 0.001 | 2001–2009 | −3.8 (−5.3, −2.2) | 0.001 |
| 2009–2014 | 4.2 (1.8, 6.6) | 0.003 | |||||||||
| Women | 10.2 (9.2, 11.2) | 6.3 (5.9, 6.8) | −3.9 (−5.0, −2.8) | −3.3 (−4.1, −2.6) | <0.001 | 1998–2007 | −6.9 (−7.9, −5.9) | <0.001 | 2007–2014 | 1.5 (0.1, 2.9) | 0.04 |
| Race/ethnicity | |||||||||||
| NH white | 7.8 (7.0, 8.7) | 6.1 (5.6, 6.5) | −1.8 (−2.8 −0.8) | −1.8 (−3.6, 0.1) | 0.06 | 1998–2003 | −11.3 (−14.0, −8.6) | <0.001 | 2003–2007 | −3.1 (−9.9, 4.1) | 0.34 |
| 2007–2014 | 6.5 (4.8, 8.2) | <0.001 | |||||||||
| NH black | 11.0 (8.5, 13.5) | 9.0 (7.9, 10.1) | −2.0 (−4.7, 0.7) | −0.9 (−3.3, 1.7) | 0.51 | 1998–2006 | −6.0 (−10.1, −1.7) | 0.01 | 2006–2014 | 4.6 (1.0, 8.3) | 0.02 |
| Hispanic | 6.1 (4.4, 7.8) | 4.5 (3.8, 5.2) | −1.6 (−3.4, 0.2) | −2.0 (−4.3, 0.3) | 0.08 | 1998–2009 | −3.8 (−6.2, −1.4) | 0.005 | 2009–2014 | 2.0 (−4.0, 8.5) | 0.49 |
NH, non-Hispanic.
Per 1,000 population with diabetes.
Trend segment identified by Joinpoint regression.
APC = AAPC (i.e., trend had 0 joinpoints).
From 1998 to 2014, among those aged ≥55 years, trends in hospitalization rates declined significantly for all CVD conditions (Table 2). However, among those aged 35–54 years, overall trends declined only for ACS (AAPC −3.2% per year [95% CL −4.3, −2.0], P < 0.001); remained unchanged for heart failure, hemorrhagic stroke, and ischemic stroke; and increased for cardiac dysrhythmia (AAPC 0.8% per year [0.1, 1.5], P = 0.03). Although in all age-groups the rates for ACS declined throughout the period, in the last 4–5 years of the study period the rates in all age-groups leveled off (Table 2). For ischemic stroke, rates increased in the last 4–5 years of the study period among those aged 35–74 years (APC 6.2% per year [2.6, 10.0], P = 0.003, for those aged 35–54 years and APC 2.6% [1.0, 4.3], P = 0.005, for those aged 55–74 years) and leveled off beginning in 2006 among those aged ≥75 years.
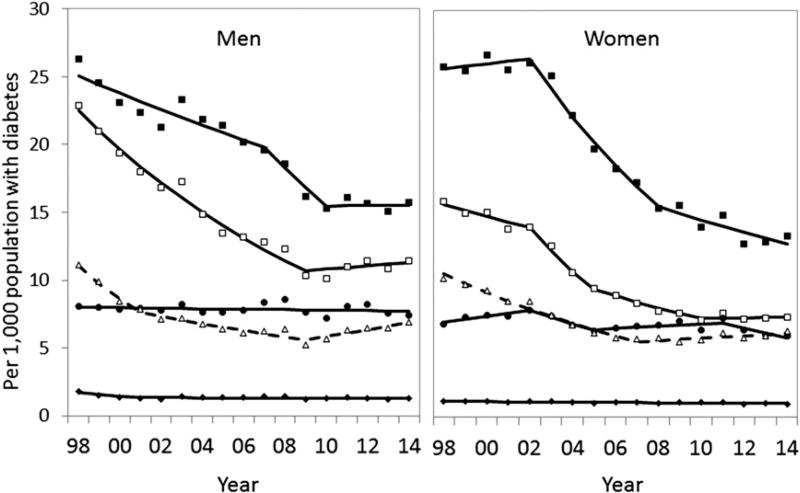
By sex
In 2014, in the population with diabetes, hospitalization rates for ACS, cardiac dysrhythmia, heart failure, and hemorrhagic stroke (but not for ischemic stroke) were higher in men than in women (Table 2). From 1998 to 2014, hospitalization rates for ACS, heart failure, and hemorrhagic and ischemic stroke declined significantly in both men and women and rates in cardiac dysrhythmia remained unchanged in both men and women (Table 2; Fig. 1). However, similar to what was seen with the age-specific hospitalization rates, the patterns of decline within the period differed between men and women.
Figure 1.
Age-adjusted hospitalization rates for selected CVD conditions among people aged ≥35 years with diagnosed diabetes, by sex (U.S., 1998–2014). Per 1,000 population with diabetes and age-adjusted based on the 2000 U.S. standard population. Symbols represent observed hospitalization rates, and lines represent modeled trends using Joinpoint regression. ■, heart failure; □, ACS; △, ischemic stroke; ●, cardiac dysrhythmia; ◆, hemorrhagic stroke.
Although throughout the period hospitalization rates for ACS and for heart failure declined in both men and women, the rates for ACS leveled off in both men and women in the last 4–5 years of the study period and the rates for heart failure leveled off in men beginning in 2007 (Table 2; Fig. 1). For cardiac dysrhythmia, even though the rates during the study period remained unchanged in both men and women, rates in women declined significantly from 2011 to 2014 (APC −5.6% per year [95% CL −9.9, −1.1], P = 0.02). For ischemic stroke, although rates throughout the period declined in both men and women, rates in the latter part of the period increased in both men (APC 4.2% per year [1.8, 6.6], P = 0.003) and women (APC 1.5% [0.1, 2.9], P = 0.04).
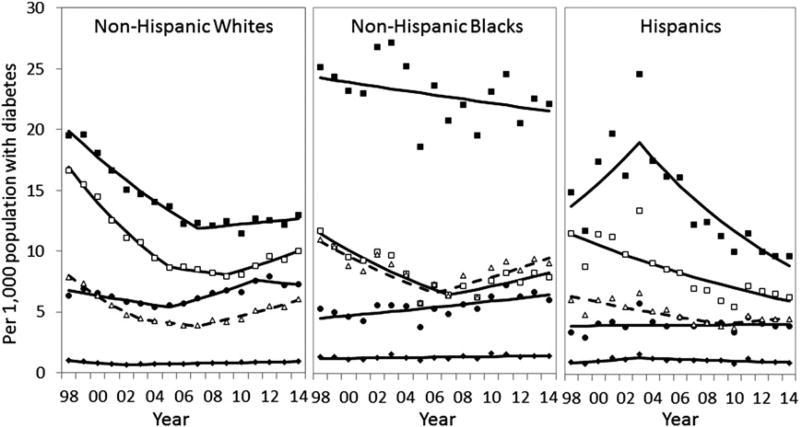
By Race/Ethnicity
In 2014, in the population with diabetes, in contrast with what was seen in rates by age and sex, racial/ethnic differences in hospitalization rates varied by CVD condition (Table 2). Compared with the other race/ethnicity groups, non-Hispanic whites had higher hospitalization rates for ACS (10.0 per 1,000 [95% CL 9.2, 10.8] vs. 7.9 [6.8, 8.9] for non-Hispanic blacks and 6.3 [5.3, 7.3] for Hispanics) and for cardiac dysrhythmia (7.3 per 1,000 [6.7, 7.8] vs. 6.1 [5.3, 6.8] for non-Hispanic blacks and 3.9 [3.2, 4.6] for Hispanics). On the other hand, non-Hispanic blacks had higher hospitalization rates for heart failure (22.1 per 1,000 [19.3, 24.9] vs. 12.9 [12.0, 13.9] for non-Hispanic whites and 9.7 [8.0, 11.3] for Hispanics), hemorrhagic stroke (1.4 per 1,000 [1.2, 1.6] vs. 0.9 [0.8, 1.0] for non-Hispanic whites and 1.0 [0.8, 1.2] for Hispanics), and ischemic stroke (9.0 per 1,000 [7.9, 10.1] vs. 6.1 [5.6, 6.5] for non-Hispanic whites and 4.5 [3.8, 5.2] for Hispanics). In contrast, compared with the other groups, Hispanics had lower hospitalization rates for cardiac dysrhythmia, heart failure, and ischemic stroke.
From 1998 to 2014, hospitalization rates for ACS declined significantly for non-Hispanic whites and Hispanics (AAPC −3.2% per year [95% CL −4.9, −1.6] and −4.0% [−5.3, −2.6], respectively, both P < 0.001) and showed no significant change for non-Hispanic blacks (Table 2; Fig. 2). For heart failure, rates decreased significantly for non-Hispanic whites only (AAPC −2.8% per year [−3.5, −2.1], P < 0.001) and remained unchanged for the other two groups. However, for cardiac dysrhythmia, rates throughout the period increased significantly for non-Hispanic blacks (AAPC 2.2% per year [0.9, 3.5], P = 0.002) and remained level for the other two groups. For hemorrhagic and ischemic stroke, rates during the study period showed no significant change in all three race/ethnicity groups. However, similar to the trends in the other demographic groups, patterns of decline within the study period differed by race/ethnicity group.
Figure 2.
Age-adjusted hospitalization rates for selected CVD conditions among people aged ≥35 years with diagnosed diabetes, by race/ethnicity (U.S., 1998–2014). Per 1,000 population with diabetes and age-adjusted based on the 2000 U.S. standard population. Symbols represent observed rates, and lines represent modeled trends. ■, heart failure; □, ACS; △, ischemic stroke; ●, cardiac dysrhythmia; ◆, hemorrhagic stroke.
Although throughout the period hospitalization rates for ACS and for heart failure declined significantly in non-Hispanic whites, in this group the rates of ACS increased (APC 4.5% per year [95% CL 2.1, 6.9], P = 0.002) from 2009 to 2014 and the rates of heart failure leveled off beginning in 2007 (Table 2; Fig. 2). In contrast, among Hispanics, the rates for heart failure declined from 2003 to 2014 (APC −6.7% per year [−8.6, −4.7], P < 0.001). Even though throughout the period rates for hemorrhagic and ischemic stroke showed no consistent change for all three race/ethnicity groups, rates for hemorrhagic stroke in the latter part of the period increased for non-Hispanic whites (APC 2.6% per year [2.1, 3.2], P < 0.001), and rates for ischemic stroke also increased for non-Hispanic whites (APC 6.5% per year [4.8, 8.2], P < 0.001) and for non-Hispanic blacks (APC 4.6% per year [1.0, 8.3], P = 0.02).On the other hand, from 2003 to 2014, hospitalization rates for hemorrhagic stroke among Hispanics declined (APC −3.0% per year [−4.9, −1.0], P = 0.006).
CONCLUSIONS
Heart disease and stroke are leading causes of death in the U.S. (16). In this analysis of nationally representative data, we documented from 1998 to 2014 significant declines in hospitalization rates for ACS, heart failure, and hemorrhagic and ischemic stroke, in both the population with diabetes and the population without diabetes, and a significant decline in cardiac dysrhythmia rates in the population with diabetes only. The average rate of decline for the entire period was similar in both populations. However, compared with the population without diabetes, and with the exception of cardiac dysrhythmia and hemorrhagic stroke, rate differences between 1998 and 2014 were greater in the population with diabetes. Thus, despite these encouraging trends, hospitalization rates in 2014 for these CVD conditions remained 2–4 times as high in the population with diabetes than in the population without diabetes, with the largest difference in heart failure rates.
Other population-based studies—three international and one of a U.S. state—have reported declining trends in hospitalization rates in the population with diabetes for AMI (which is a condition within ACS) (17–19), heart disease (including ischemic heart disease, cardiac dysrhythmia, and heart failure) (20), and stroke (17,19,20). Two studies compared trends in AMI and stroke hospitalization rates by diabetes status (17,18). One study of the population of Ontario, Canada, found that AMI and stroke rates declined more in the population with diabetes than in the population without diabetes between 1992 and 2000 (17). The second study, in England, found no difference in AMI and stroke trends by diabetes status between 2004 and 2010, consistent with our findings in trends of ACS and hemorrhagic and ischemic stroke (18). In both of these international studies (17,18), similar to our findings, hospitalization rates at the end of the study period were still greater in the population with diabetes than in the population without diabetes. Our findings of decreasing trends in ACS, cardiac dysrhythmia, heart failure, and both hemorrhagic and ischemic stroke hospitalization rates in the population with diabetes in the U.S. are also consistent with a study that found remarkable improvements in CVD death rates from 1997 to 2006 among U.S. adults with diabetes (40% decrease) (7).
Declining trends in AMI and stroke hospitalization and mortality rates in the U.S. general population (i.e., populations with diabetes and without diabetes combined) are well-documented (21–25). Our findings showing that hospitalization rates for heart failure declined significantly from1998 to 2014 in both the population with diabetes and the population without diabetes are in contrast with a study indicating that overall hospitalization rates from 2000 to 2010 showed no significant change for congestive heart failure (26) but are consistent with another study showing that overall death rates for heart failure decreased from2000 to 2012 (27). Furthermore, a study based on NIS data (28) reported an increase from 2000 to 2010 in the overall hospitalization rate for atrial fibrillation—the most common arrhythmia leading to hospitalization—in seeming contrast to our findings showing that hospitalization rates for cardiac dysrhythmia declined from 1998 to 2014 in the population with diabetes and showed no consistent trend in the population without diabetes from 1998 to 2011. However, when we looked at atrial fibrillation alone (data not shown), we found that rates increased throughout the study period in the population with diabetes and from 2004 to 2011 in the population without diabetes. This suggests that dysrhythmia hospitalizations for causes other than atrial fibrillation differed from trends in atrial fibrillation.
Declines in CVD hospitalization rates occurred despite the increased use of more sensitive laboratory tests (e.g., biomarkers) that have improved detection of heart attacks and strokes (29). Improvements in CVD morbidity and mortality might be due to several factors, including prevention or improved control of CVD risk factors (e.g., smoking, cholesterol, blood pressure); new or more aggressive treatments for CVD and its risk factors; improved detection and management of precursor conditions, such as subclinical atherosclerosis; better management of underlying diseases (including diabetes); and access to regular care, or other factors (11,12,29–32). We cannot determine from our surveillance data the reasons for the greater improvements (i.e., the larger rate differences) in ACS, heart failure, and ischemic stroke rates among those with diabetes. However, one potential explanation may be that adults with diabetes differentially benefited from new treatments and improvements to CVD risk factors either because they have higher levels of CVD risk factors than those without diabetes and thus have greater opportunity for improvement or because they were treated more aggressively owing to their high risk status. For example, although statin use has increased in the U.S. population (29,32–35), one study found the use of statins or other cholesterol-lowering medication to be higher and to have increased faster among people with diabetes than among those without diabetes (36), and population-based studies have found greater relative improvements in cholesterol and lipid levels among people with diabetes than in those without (32,37). In addition, between 1999 and 2010, the proportion of adults with diabetes achieving glycemic control and those achieving blood pressure control increased significantly (12).
Despite the encouraging trends in most of the CVD conditions studied, trends in several subgroups of the population with diabetes are of concern. In the latter years, after an initial period of decline, hospitalization rates leveled off for ACS in all age-groups, in men, in women, and in non-Hispanic blacks; for heart failure in men and in non-Hispanic whites; and for ischemic stroke in people aged ≥75 years and in Hispanics. In addition, throughout the period, hospitalization rates remained level for cardiac dysrhythmia in men, non-Hispanic whites, and Hispanics; for heart failure in those aged 35–54 years and non-Hispanic blacks; and for hemorrhagic stroke in those aged 35–54 years and non-Hispanic blacks. Reasons for why these rates are no longer declining in some population subgroups cannot be determined from our surveillance data; however, they may reflect demographic differences in treatment and uptake of treatments, a differential impact of preventive treatment or risk factor control, or other factors (38). Even more concerning, several trends in the population with diabetes showed a significant increase. In particular, in the latter part of the study period, ischemic stroke hospitalization rates increased in most of the subpopulations studied: in those aged 35–74 years, men, women, non-Hispanic whites, and non-Hispanic blacks. Increases were also seen for ACS in non-Hispanic whites (2009–2014), for cardiac dysrhythmia in people aged 35–54 years and in non-Hispanic blacks (1998–2014), and for hemorrhagic stroke in non-Hispanic whites (2002–2014). Reasons for these recent increases are unclear. Shifting patterns of case finding as a result of improved access to care may be underway, identifying a pool of higher-risk patients and changing the epidemiologic characteristics of the population with diabetes. Also, declines in diabetes incidence (39) and decreases in mortality (7,8,10) may have resulted in a population with diabetes that is older and has longer duration of disease and is therefore more susceptible to the development of diabetes complications. More years of data and continued surveillance of CVD hospitalizations in the population with diabetes will be needed to confirm these trends.
Our study has a major strength in that we used nationally representative surveys to examine trends in hospitalization of selected CVD conditions among people with and without diagnosed diabetes. However, it also has several limitations. First, although the CVD conditions studied are likely to result in hospital admissions, the findings need to be interpreted with caution given that health care practices have changed during the study period (29,31). Second, because NIS samples hospital discharges and not individual persons, NIS hospital discharge rates may not necessarily reflect rates per person; that is, persons who are hospitalized more than once in the same calendar year may be counted more than once. Although repeat hospitalizations overestimate the hospitalization rates, ratios of rates in the population with diabetes versus the population without diabetes with and without repeat hospitalizations may not be significantly affected (40). Third, we cannot distinguish persons with prior known CVD from those without and thus cannot determine whether CVD incidence rates are actually declining. Recent managed-care data show that reductions in death rates may be driven by people with prior history of CVD (41). Fourth, estimates of the population with diagnosed diabetes were based on self-report and did not include persons with undiagnosed diabetes or prediabetes or persons residing in nursing homes (15). Finally, new diagnostic criteria for diabetes in 1997 that lowered the threshold of the fasting glucose value from 140 to 126 mg/dL (9) may have resulted in a greater number of individuals with milder disease, detected earlier in the disease process, and contributed to the overall decline in CVD hospitalization rates. However, throughout the period, hospitalization rates for ACS, heart failure, and hemorrhagic and ischemic stroke declined significantly in both the population with diabetes and the population without diabetes.
Despite our encouraging findings, CVD remains a major preventable cause of morbidity and the most common cause of death for adults with diabetes (1,2). Furthermore, important disparities continue to persist, including greater CVD hospitalization rates for adults with diabetes than in adults without diabetes, among older people with diabetes compared with those younger, and among men with diabetes compared with women. Also, compared with non-Hispanic whites, non-Hispanic blacks with diabetes had higher hospitalization rates for heart failure and for stroke (both ischemic and hemorrhagic), as well as potentially geographical disparities that have previously been reported (24) but that we were unable to examine. In addition, our outcomes do not capture the full range of CVD morbidity, as data from the U.S. Renal Data System or from other sources suggest that very large differences between subgroups remain in other CVD outcomes, including cardiomyopathy, sudden cardiac arrest, and CVD associated with kidney failure (2,19,29,42). Although diabetes care in the U.S. has improved, broad opportunities remain to reduce rates of smoking, hyperglycemia, hyperlipidemia, and uncontrolled hypertension (12), particularly among people in younger age-groups and minority populations (38). Continued and additional efforts, such as promoting lifestyle changes that include increased physical activity and healthier eating (43), might be considered to improve CVD risk factor control, sustain and improve the declining hospitalization trends in CVD conditions in both the population with diabetes and the population without diabetes, and further reduce the excess risk for heart failure and stroke among non-Hispanic blacks with diabetes.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. N.R.B. researched data and wrote the manuscript. Y.L. analyzed data and contributed statistical support. E.W.G. and L.S.G. designed the study. Y.L., E.W.G., and L.S.G. critically reviewed and edited the manuscript and contributed to the discussion and interpretation of results. All authors approved the final manuscript. N.R.B. and Y.L. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 75th Scientific Sessions of the American Diabetes Association, Boston, MA, 5–9 June 2015.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 2.Bertoni AG, Goff DC., Jr . Diabetes and cardiovascular disease. In: Venkat Narayan KM, Williams D, Gregg EW, Cowie C, editors. Diabetes Public Health: From Data to Policy. New York, NY: Oxford University Press; 2011. pp. 173–194. [Google Scholar]
- 3.Zhang X, Saaddine JB, Chou CF, et al. Prevalence of diabetic retinopathy in the United States, 2005–2008. JAMA. 2010;304:649–656. doi: 10.1001/jama.2010.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burrows NR, Li Y, Geiss LS. Incidence of treatment for end-stage renal disease among individuals with diabetes in the U.S. continues to decline. Diabetes Care. 2010;33:73–77. doi: 10.2337/dc09-0343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y, Burrows NR, Gregg EW, Albright A, Geiss LS. Declining rates of hospitalization for nontraumatic lower-extremity amputation in the diabetic population aged 40 years or older: U.S., 1988–2008. Diabetes Care. 2012;35:273–277. doi: 10.2337/dc11-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Selvin E, Coresh J, Shahar E, Zhang L, Steffes M, Sharrett AR. Glycaemia (haemoglobin A1c) and incident ischaemic stroke: the Atherosclerosis Risk in Communities (ARIC) Study. Lancet Neurol. 2005;4:821–826. doi: 10.1016/S1474-4422(05)70227-1. [DOI] [PubMed] [Google Scholar]
- 7.Gregg EW, Cheng YJ, Saydah S, et al. Trends in death rates among U.S. adults with and without diabetes between 1997 and 2006: findings from the National Health Interview Survey. Diabetes Care. 2012;35:1252–1257. doi: 10.2337/dc11-1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370:1514–1523. doi: 10.1056/NEJMoa1310799. [DOI] [PubMed] [Google Scholar]
- 9.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Williams DE, Narayan KM, Geiss LS. Declining death rates from hyperglycemic crisis among adults with diabetes, U.S., 1985–2002. Diabetes Care. 2006;29:2018–2022. doi: 10.2337/dc06-0311. [DOI] [PubMed] [Google Scholar]
- 11.Wang J, Geiss LS, Cheng YJ, et al. Long-term and recent progress in blood pressure levels among U.S. adults with diagnosed diabetes, 1988–2008. Diabetes Care. 2011;34:1579–1581. doi: 10.2337/dc11-0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ali MK, Bullard KM, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med. 2013;369:287–288. doi: 10.1056/NEJMc1306652. [DOI] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality. [Accessed 6 July 2016];Overview of the National (Nationwide) Inpatient Sample (NIS) [Internet] 2016 Available from http://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 14.Agency for Healthcare Research and Quality. [Accessed 6 July 2016];NIS database documentation [Internet] 2015 Available from http://www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.
- 15.Design and estimation for the National Health Interview Survey, 1995–2004. Vital Health Stat 2. 2000;130:1–31. [PubMed] [Google Scholar]
- 16.Xu JQ, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2015. NCHS Data Brief, no. 267. Hyattsville, MD: National Center for Health Statistics; 2016. [PubMed] [Google Scholar]
- 17.Booth GL, Kapral MK, Fung K, Tu JV. Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care. 2006;29:32–37. doi: 10.2337/diacare.29.01.06.dc05-0776. [DOI] [PubMed] [Google Scholar]
- 18.Vamos EP, Millett C, Parsons C, Aylin P, Majeed A, Bottle A. Nationwide study on trends in hospital admissions for major cardiovascular events and procedures among people with and without diabetes in England, 2004–2009. Diabetes Care. 2012;35:265–272. doi: 10.2337/dc11-1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mountford WK, Lackland DT, Soule JB, Hunt KJ, Lipsitz SR, Colwell JA. Racial disparities in trends for cardiovascular disease and procedures among hospitalized diabetic patients. Ethn Dis. 2008;18:131–135. [PubMed] [Google Scholar]
- 20.Eurich DT, Gamble JM, Simpson SH, Johnson JA. The darkening cloud of diabetes: do trends in cardiovascular risk management provide a silver lining? Diabetes Care. 2008;31:2136–2142. doi: 10.2337/dc08-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang OJ, Wang Y, Chen J, Krumholz HM. Recent trends in hospitalization for acute myocardial infarction. Am J Cardiol. 2012;109:1589–1593. doi: 10.1016/j.amjcard.2012.01.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hall MJ, Levant S, DeFrances CJ. Hospitalization for stroke in U.S. hospitals, 1989–2009. NCHS Data Brief. 2012;95:1–8. [PubMed] [Google Scholar]
- 23.Tong X, George MG, Gillespie C, Merritt R. Trends in hospitalizations and cost associated with stroke by age, United States 2003–2012. Int J Stroke. 2016;11:874–881. doi: 10.1177/1747493016654490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeh RW, Normand SL, Wang Y, Barr CD, Dominici F. Geographic disparities in the incidence and outcomes of hospitalized myocardial infarction: does a rising tide lift all boats? Circ Cardiovasc Qual Outcomes. 2012;5:197–204. doi: 10.1161/CIRCOUTCOMES.111.962456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gillum RF, Kwagyan J, Obisesan TO. Ethnic and geographic variation in stroke mortality trends. Stroke. 2011;42:3294–3296. doi: 10.1161/STROKEAHA.111.625343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall MJ, Levant S, DeFrances CJ. Hospitalization for Congestive Heart Failure: United States, 2000–2010. NCHS Data Brief, no. 108. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 27.Ni H, Xu JQ. Recent Trends in Heart Failure-Related Mortality: United States, 2000–2014. NCHS Data Brief, no. 231. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 28.Sheikh A, Patel NJ, Nalluri N, et al. Trends in hospitalization for atrial fibrillation: epidemiology, cost, and implications for the future. Prog Cardiovasc Dis. 2015;58:105–116. doi: 10.1016/j.pcad.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 29.Go AS, Mozaffarian D, Roger VL, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fryar CD, Chen TC, Li X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief. 2012;103:1–8. [PubMed] [Google Scholar]
- 31.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 32.Ford ES. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013;61:2249–2252. doi: 10.1016/j.jacc.2013.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller GE, Stagnitti MN. Trends in Statin Use in the Civilian Noninstitutionalized Medicare Mopulation, 1997 and 2002. Statistical Brief #97. Agency for Healthcare Research and Quality; Rockville, MD: 2005. [Google Scholar]
- 34.National Center for Health Statistics. Health, United States, 2013: With Special Feature on Prescription Drugs. Hyattsville, MD: National Center for Health Statistics; 2014. [PubMed] [Google Scholar]
- 35.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42:1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 36.Robinson JG, Booth B. Statin use and lipid levels in older adults: National Health and Nutrition Examination Survey, 2001 to 2006. J Clin Lipidol. 2010;4:483–490. doi: 10.1016/j.jacl.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Preis SR, Pencina MJ, Hwang SJ, et al. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation. 2009;120:212–220. doi: 10.1161/CIRCULATIONAHA.108.846519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ali MK, Bullard KM, Gregg EW, Del Rio C. A cascade of care for diabetes in the United States: visualizing the gaps. Ann Intern Med. 2014;161:681–689. doi: 10.7326/M14-0019. [DOI] [PubMed] [Google Scholar]
- 39.Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312:1218–1226. doi: 10.1001/jama.2014.11494. [DOI] [PubMed] [Google Scholar]
- 40.Benjamin SM, Wang J, Geiss LS, Thompson TJ, Gregg EW. The impact of repeat hospitalizations on hospitalization rates for selected conditions among adults with and without diabetes, 12 US States, 2011. Prev Chronic Dis. 2015;12:E200. doi: 10.5888/pcd12.150274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Desai JR, Vázquez-Benítez G, Xu Z, et al. SUPREME-DM Study Group. Who must we target now to minimize future cardiovascular events and total mortality? Lessons from the Surveillance, Prevention and Management of Diabetes Mellitus (SUPREME-DM) Cohort Study. Circ Cardiovasc Qual Outcomes. 2015;8:508–516. doi: 10.1161/CIRCOUTCOMES.115.001717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.U.S. Renal Data System. USRDS 2017 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2017. [Google Scholar]
- 43.Zhang X, Devlin HM, Smith B, et al. Effect of lifestyle interventions on cardiovascular risk factors among adults without impaired glucose tolerance or diabetes: A systematic review and meta-analysis. PLoS One. 2017;12:e0176436. doi: 10.1371/journal.pone.0176436. [DOI] [PMC free article] [PubMed] [Google Scholar]