Abstract
Among Black men who have sex with men (MSM), HIV incidence is disproportionately high and HIV care engagement is disproportionately low. There may be important opportunities to leverage the primary relationship to improve engagement in HIV care and treatment among Black MSM couples. Using dyadic qualitative analysis of semi-structured, one-on-one interviews, we explored dyadic aspects of HIV care engagement among 14 Black MSM couples in which at least one partner was HIV-positive and identified as a Black cisgender man. Findings showed that men varied in how involved they were in their HIV-positive partner’s care and treatment, and in how they reciprocated their partner’s involvement. Patterns of dyadic HIV care engagement supported a conceptual model of dyadic coordination that describes Black MSM relationships in terms of two conceptual dimensions of dyadic HIV care engagement, and guides future intervention designs with Black MSM couples.
Keywords: HIV, Black Men who have sex with Men, Primary Romantic Relationship, HIV care engagement, Couples, Dyadic Coordination
INTRODUCTION
Black men who have sex with men (MSM) are disproportionately affected by HIV/AIDS in the United States (US), representing approximately a quarter of all new HIV infections.1,2 Health disparities among MSM persist even after HIV infection, with lower proportions of Black MSM actively engaged in HIV care and treatment as compared to White MSM.3–5 An estimated 33% of Black MSM are retained in care as compared to 51% of White MSM and an estimated 16% of Black MSM achieved viral suppression as compared to 34% among White MSM.2
Social relationships can provide a range of physical and mental health benefits for men. Given that almost half of Black MSM living in the US reported being in a primary relationship,6 there may be important opportunities to leverage existing forms of social support to improve engagement in HIV care and treatment. With respect to HIV prevention, studies have demonstrated that MSM couples make joint decisions about relationship agreements,7,8 condom use,9 seroadaptation (e.g. sexual positioning, such as condom use based on each partner’s status,10 viral sorting (i.e., incorporating knowledge of partner’s viral load into safe sex decisions),11–13 HIV testing and counseling,14,15 and uptake of pre-exposure prophylaxis (PrEP).16 Evidence across a wide range of settings suggests that primary partners also play an important role in HIV care engagement.17–21 Primary partners provide key sources of social support for MSM living with HIV, which may have a positive impact on adherence and virologic control.22,23
However, less research has focused on understanding dyadic aspects of engagement in care among Black MSM couples. Black MSM are particularly vulnerable to poor engagement in care as a consequence of social and structural forces such as systemic racism and violence (e.g., police brutality, incarceration) that create challenging circumstances for those in primary relationships.2,24–26 While the primary partnership is often associated with favorable outcomes in care engagement, presumably via social support pathways, research with Black MSM showed conflicting results. A study with Black MSM found that, although partnered men were more likely than single men to have reported having a primary healthcare provider or receiving recent HIV care, they were less likely to have reported perfect adherence to antiretroviral therapy (ART).27 Moreover, those whose partner was HIV-negative tended to report better adherence to ART compared to men whose partner was HIV-positive.27 These findings highlight a need to better understand the dyadic aspects of HIV care engagement among Black MSM in primary relationships so that more effective interventions can be developed for Black MSM couples.
Prior research exploring how MSM in primary relationships engage in HIV care and treatment has focused primarily on individuals, rather than the couple, as the unit of analysis. Qualitative dyadic analyses of couple data better capture both sides of a two-way, dyadic interaction among couples and, as such, allow data triangulation in addressing differences in individual partners’ accounts.28 Dyadic analysis of couple data allows a richer, in-depth analysis to elucidate dyadic aspects of HIV care engagement. Thus, the goal of this study is to use qualitative dyadic analysis to explore the extent to which Black MSM in primary relationships may be involved in their partner’s HIV care and to describe these patterns of involvement.
METHOD
As part of a larger study exploring the use of mobile technology to increase engagement in HIV care with Black MSM in primary relationships, we explored how Black MSM couples engage in HIV care and treatment.
Recruitment and screening strategy
We used purposive sampling to recruit couples. Participants were recruited by trained recruiters who frequented and distributed study materials at social venues where men of color meet (e.g., local bars and cafes), as well as AIDS service and community-based organizations (CBOs) serving Black MSM in the Bay Area where we have established working relationships. Recruiters also announced the study at social gatherings at CBOs where social events are regularly held and provided interested individuals a contact number to call for eligibility screening.
Potential participants were invited to a phone screening to determine eligibility during which they were informed of the purpose of the study and of the types of questions that they would be asked, such as questions regarding their HIV-status, their partner’s HIV-status, healthcare service providers, and medications, in addition to other questions to determine eligibility. Couples were eligible if at least one partner: identified as Black or African American; identified as a cisgender man at the time of the study; reported having a primary partner of three months or longer; reported being HIV-positive; was between the ages of 18 and 65; reported having a personal mobile phone; and resided in the San Francisco Bay Area. Participants were excluded from the study if their partner declined to participate. Inclusion criteria for the primary partners of the participants were: identified as a cisgender man; reported the referring participant as their primary partner of three months or longer; was between the ages of 18 and 65; and resided in the San Francisco Bay Area. HIV-status was verified by a letter of diagnosis or a labeled HIV medicine pill bottle.
A total of 51 individuals were screened for the study. Of these, 23 were ineligible for the following reasons: Did not identify as Black/African American (n=2); neither partner was HIV-positive (n=2); single relationship status (n=2); no-show (n=2); the relationship ended at the time of screening or interview (n=4); or primary partner declined to participate (n=9). One couple (n=2) was excluded from analyses due to one partner identifying as a trans woman upon arriving at the interview. A total of 28 men (14 couples) participated in the study.
Individual interviews
Upon determining their eligibility, participants were enrolled and assigned a unique identification number that linked them with their partner. Participants and their primary partner were scheduled for an in-person interview. The interviews were conducted in private rooms at the study site that was centrally located and easily accessible via public transportation. Each member of a couple was scheduled to arrive at the same time and place and was interviewed individually in separate rooms at the same time.
At the study interview site, the couple was greeted and led by research staff into separate interview rooms. Each participant was informed of his voluntary participation. Informed consent was obtained from the participant prior to each interview, which lasted approximately 1.5 to 2 hours. There was a private waiting area for participants who finished the study before their partner.
The lead author and co-author (JYT, RSK) conducted semi-structured, one-on-one interviews. Each couple member was interviewed separately to allow him to freely narrate and discuss his unique experiences.28,29 Among seroconcordant-positive couples where both partners were engaged in HIV care and treatment, interviews specifically explored how their own engagement in HIV care and treatment may have influenced their partner’s care engagement (e.g., “How has taking care of your HIV impacted [your relationship/partner/your partner’s care engagement]?”). Because all of HIV-negative partners of the serodiscordant couples in this study reported receiving PrEP, interviews explored how each couple member navigated his respective care engagement and the mutual influence each perceived having on the other’s care engagement.
To allow for both individual- and dyadic level analyses, interview questions were designed so that the HIV-positive Black man in each couple was assigned to be the “index” participant; if both couple members were HIV-positive Black men, then the index participant was randomly assigned within the couple. Interview questions were designed to explore the index participant’s HIV care engagement in the context of the primary romantic relationship. For example, interview guide topics covered how the index participant engaged in HIV care (e.g., “How often do you see your medical provider for your HIV?”), and how his partner may be involved in his care, (e.g., “In what ways does [your significant other] support you to take care of your HIV?”). Each member of the couple was asked identical questions in order to allow us to explore overlaps and contrasts between each couple member’s narratives.
Analysis
Interviews were audio-recorded and transcribed verbatim. We analyzed the data at the individual and dyadic levels using an inductive approach in which we identified themes first by reading all transcripts and developed a codebook based on emergent themes in the data. Similar to the qualitative dyadic analysis approach outlined in Eisikovits and Koren,28 we compared and contrasted each individual’s account of HIV care engagement with that of his partner. This process allowed us to discover overlaps between individual narratives and to identify points of corroboration and contradiction between relationship partners, with the couple as the “unit of analysis.” We cross-analyzed significant statements, sentences, and quotes, formulating themes based on both partners’ perspectives on their relationship, health and care engagement, and respective roles in their own and each other’s healthcare.28 Comparing both partners’ perspectives allowed triangulation to derive a fuller, more contextualized understanding of the nature of HIV care engagement in the context of the dyadic relationship.
After examining the data at the dyadic level, we then conducted individual-level analysis. The first, second, and third authors developed the codebook by reading all transcripts and iteratively generating and revising codes based on group discussions of major themes that emerged. We applied the codes to the transcripts of one couple to verify code definitions and consistency in code application. After reviewing the coded transcripts and comparing code application between coders, we revised the codebook. We repeated this process. Upon reaching consensus on code definitions and agreement on code application, we independently coded the remaining transcripts. We coded using Dedoose version 7.6.21, a qualitative data software package.30
RESULTS
A total of 11 seroconcordant-positive and three serodiscordant couples (14 couples; 28 men) participated in the study (Table 1). The mean age of the sample was 48.79 years. The majority of couples were comprised of partners who both self-identified as Black (10 couples); the remaining couples were of mixed race. The annual personal income of the sample ranged from less than $10K to $55K, with half of the sample (n=14) reporting an annual personal income of less than $20K. The intra-couple age difference ranged from 0 to 36 years (M=10.71 years). Relationship length ranged from three months to over 20 years (M=6.56 years). Of the 14 couples, eight reported living together at the time of the study. Quotes are followed by a pseudonymous name, the participant’s age, race, HIV serostatus and whether he is in a concordant positive (C) or discordant (D) partnership (e.g., Daniel, 35, Black, HIV+, D).
Table 1.
Participants’ Race/Ethnicity, Age, HIV Status.
| Index (n=14) | Partner (n=14) | ||||
|---|---|---|---|---|---|
| n | M (SD) | n | M (SD) | ||
| Age (year) | - | 48.9 (12.84) | - | 43.6 (13.74) | |
| ≤ 24 | 1 | - | 0 | - | |
| 25–35 | 2 | - | 3 | - | |
| 36–45 | 1 | - | 4 | - | |
| 46–55 | 4 | - | 3 | - | |
| 56–64 | 5 | - | 1 | - | |
| ≥ 65 | 1 | - | 3 | - | |
|
| |||||
| Race | Black | 13 | - | 10 | - |
| Mixed, Black | 1 | - | 2 | - | |
| Hispanic | 0 | - | 1 | - | |
| White | 0 | - | 1 | - | |
|
| |||||
| HIV Status | HIV+ | 14 | - | 11 | - |
| HIV− | 0 | - | 3 | - | |
Note. Index denotes the HIV-positive Black man in each couple; if both couple members were HIV-positive Black men, one was randomly assigned as the Index.
Findings indicated that dyadic HIV care engagement varied across couples along the dimensions of partner involvement and reciprocity. On the dimension of involvement, most men described being actively involved in their partner’s HIV care, some described being peripherally involved, and a few described being uninvolved. Men in about half of the sample described being actively involved in their partner’s HIV care and overall health. For example:
“[I take him] to drop in therapy, and to my doctor’s appointments. I go to his doctor’s appointments. He’s met my doctor, I’ve met his doctor… Oh, I know every last bit of that man’s deal.”
Daniel, 35, Black, HIV+, C
While some described playing an active role in their partner’s healthcare, men in half of the couples in the study described playing a more passive or peripheral role. Men described being “on-call,” rising to the occasion if and when needed. Finally, men in a few couples described being completely uninvolved in their partner’s HIV care and treatment, because “neither one of us has issues that we really need to dwell on.” For example:
“Well, neither of us is sick. I guess we focus on the fun times. We don’t talk about what’s bothering us except for my cold, or if something should be bothering Wayne right at the moment, which doesn’t really happen very often. But as far as our HIV, we just don’t talk about it.”
Shawn, 67, Black, HIV+, C
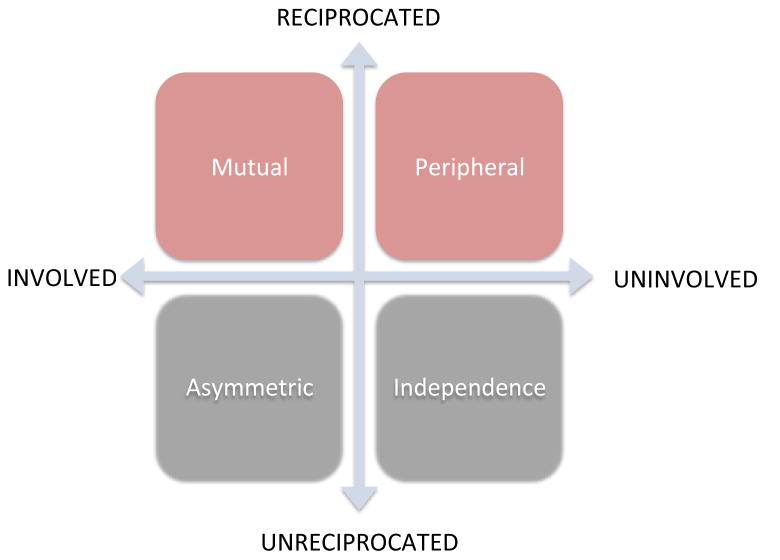
At the dyadic level, some men reciprocated their partner’s involvement, while others did not. Thus, dimensions of involvement and reciprocity are not mutually exclusive (Table 2). Some couples described mutual involvement, whereby both partners are directly involved to the same extent in the other’s HIV care. Other couples discussed peripheral involvement, whereby both partners are involved to the same extent in the other’s HIV care. Some patterns of involvement and reciprocity illustrated an asymmetric involvement pattern, whereby one’s level of involvement in his partner’s care is unreciprocated; and (d) independence, where there is a lack of involvement and reciprocity. The dimensions of involvement and reciprocity illustrate dyadic coordination of HIV care and treatment (Figure 1). In the following, we characterize couples based on the extent to which partners’ involvement was reciprocated, using the nomenclature derived from the two-dimensional model of dyadic coordination.
Table 2.
Dyadic Coordination in HIV Care and Treatment.
| Dyadic Coordination | Description |
|---|---|
| Mutual | Both partners describe being actively involved in the other’s HIV care and treatment. |
| Peripheral | Both partners describe being peripherally involved (e.g., on an “as- needed” basis) in the other’s HIV care and treatment. |
| Asymmetric | One partner describes being more involved in the other’s care while the other denies it. |
| Independent | Both partners indicate being uninvolved in the other’s HIV care and treatment. |
Figure 1.
Two-Dimensional Model of Dyadic Coordination of HIV Care and Treatment
Mutual Involvement
Some couples described relationships in which both partners are directly involved in each other’s HIV and healthcare management. One man described coordinating his and his partner’s schedules so that they are able to attend medical appointments together and be mutually involved:
“We try to make [our appointments] on the same day so that it’s kind of convenient to go with each other. But if need be, one or the other, we - I’ll still go with him, or he’ll come with me to my appointment.”
Matthew, 44, Black, HIV+, C
Both Matthew and his partner, Tyler, corroborated that they involved in the other’s healthcare—their support is mutual and reciprocated. Tyler indicated how Matthew’s involvement in his care plays an intricate role in his being retained in care:
“He always makes sure I make my appointment. Am I going to keep my appointment? He’ll go with me to make sure I keep my appointment and stuff like that.”
– Tyler, 38, Black, HIV+, C
Both partners were mutually knowledgeable about the other’s treatment regimen and felt mutually responsible for the other’s health. Tyler indicated that this feeling of responsibility is not one-sided:
| Interviewer: | How responsible do you feel for his health? |
| Tyler: | I feel very responsible…And the way I help him, [I] remind him. |
| Interviewer: | How responsible does he feel for your health? |
| Tyler: | Very responsible. |
| Interviewer: | How much does he know about your HIV treatment? |
| Tyler: | He knows everything. |
| Interviewer: | How often does he need to take his meds? |
| Tyler: | Every day…once a day. |
| Interviewer: | Do you know any of the names of the medicines he takes? |
| Tyler: | Yes. He takes Prezcobix. He takes Truvada. |
Peripheral Involvement
Other couples described dynamics in which both partners are only peripherally involved in the other’s healthcare. Martin and Jose each recognize that there is a limit to how much they can help the other, that at the end of the day, it is up to the individual to help himself. Jose, a 49-year-old Black/mixed race man living with HIV, expressed that he doesn’t want to be a “nag,” while his partner, Martin, a 56-year-old Latino man living with HIV, admits, “I can’t be with [him] 24/7.” They are “stand-by,” peripherally involved in the other person’s health, both contending that being too involved would create conflict, and expressing that being co-dependent is not their respective style. Ben explained that he and his partner are supportive, but are nevertheless independent:
“I’m not his mother. I’m not his caretaker. He’s not my mother or caretaker. We’re just - we take care of our own stuff and then we share with what we have. So, it’s the mentality.”
– Ben, 55, White, HIV+, C
Asymmetric Involvement
In some couples, partners described a lack of reciprocity. Men expressed that their involvement in their partner’s healthcare is unreciprocated, and had different reasons for why. Some men described their partner as helpless and in need for care:
“I just tell him that he has an appointment to go to and he goes. I help him with everything… I help him with his…appointments - a reminder on his calendar. I feed him. I clothe him. I do his nails. I cut his hair. I do everything for him. Like seriously. I mean, I dress him. I go buy his clothes and I make sure he has the right stuff on. I iron his clothes for him… I went to his first day of school and made sure about his classes. I do everything for him… Literally everything. Because he can’t be without me.”
– Chris, 47, Black, HIV+, C
In this couple, Chris described that his partner, Jayden, a 36-year-old Black man living with HIV, would be lost without him. By and large, Jayden corroborated Chris’ account. Jayden readily admitted that Chris takes care of him “in every way” while he does not reciprocate. As shown in the following exchange, Jayden acknowledged the asymmetry in the relationship and admitted wanting it to continue:
| Interviewer: | Does he cook for you? |
| Jayden: | Yes. |
| Interviewer: | Do you cook for him? |
| Jayden: | I wish. |
| Interviewer: | What would you like him to keep doing? |
| Jayden: | Being on my back. |
| Interviewer: | About what? |
| Jayden: | Everything. Taking meds. |
| Interviewer: | So, you want him to keep doing that. |
| Jayden: | Yeah. |
| Interviewer: | What do you want him to stop doing? |
| Jayden: | What do I want him to stop doing? Nothing. |
In the above example, not only did Jayden and Chris both agree that asymmetry exists, they also agreed that Chris was more involved as a partner than Jayden was for Chris. They saw eye-to-eye regarding who was provided care and who received it. For other couples, the partners may agree that asymmetry exists, but disagree regarding the direction of the asymmetry. That is, both partners believe that they are more involved in the other’s HIV care and treatment than the other, as exemplified in the following couple. For example, Justin perceived being more involved in his partner’s care than his partner is in his:
“I’m involved with his HIV care more than he is [in my or his own care]…Because I take him to [Name of Clinic]. I know his nurse, I know the doctor. And just, like, I know who to go to if I need information for him. I know like what pills he’s taking… but then he takes that as, like, as I said, like I’m supposed to just do it already… I know everything about his HIV care, you know, but… Like, right now, he didn’t even tell me, like, he was on Hep C medicine for the 12 - eight weeks or whatever. And, like, that…affects me, so what didn’t he tell me? He gets his medicine mailed to him, so I know like the medicine list. I know, like, this is new medicine – ‘You don’t want tell me about this new medicine?’ I knew about it - like, it affects me, so… Yeah, so, I know everything about his care, yes.” -
Justin, 24, Black, HIV+, C
Justin expressed some resentment toward his partner for not acknowledging the care he provides him. Justin’s partner, Henry, contended that Justin does help him, but nevertheless insisted that he does more for Justin:
“We remind each other about taking the pills. Right now, he does want to be helping me out with my issue with my health. He does want to be driving me around…[But] I do [call to make medical appointments] more than he does. I’m the one who call the [Name of Clinic] for his appointments…For his appointments and my appointments.”
– Henry, 42, Hispanic, HIV+, C
It is worthwhile to note that although neither Justin nor Henry appeared satisfied with their relationship, dyadic coordination of HIV care and treatment nevertheless occurred. Both appeared to benefit from their partner’s involvement, even as both partners claimed to have done more or as much as the other partner. In other words, both partners appeared to be able to meet their respective needs in HIV care and treatment engagement because their partner was involved.
Independence: Lack of Involvement and Reciprocity
The remainder of the couples indicated a mutual lack of involvement in HIV care and treatment. Because partners are uninvolved in the other’s HIV care and treatment, there is nothing to reciprocate. Shawn and Wayne are in a concordant-positive relationship in which both described a mutual lack of involvement. While both insisted that they feel responsible for the other’s health, each had a different reason for his lack of involvement. Shawn reasoned that their mutual lack of involvement is due to the fact that they are both healthy and neither of them wants to dwell on “the negatives”:
“We talk about it, but we don’t help each other as far as - no. Well, neither one of us has issues that we really dwell on. And like I said, I see my doctor twice a year. Actually, I’ve seen Wayne at UC before when I was there. But not because we were going together. Well, neither of us is sick. I guess we focus on the fun times. Neither one of us dwells on - because we never talk about what’s bothering us except for my cold, or if something should be bothering Wayne right at the moment, which doesn’t really happen very often. But as far as our HIV, we just don’t talk about it.”
– Shawn, 67, Black, HIV+, C
Wayne stayed uninvolved in Shawn’s HIV care to maintain his and Shawn’s autonomy and as a way to show mutual respect:
“Some things I leave it up to him because I don’t want to come off as this controlling type person. And that would affect our respect for each other… We don’t get too much into that because I know he is very concerned about his health.”
– Wayne, 58, Black, HIV+, C
DISCUSSION
Primary partnerships are often associated with favorable HIV-related outcomes, presumably via supportive dynamics in primary relationships. However, recent evidence among Black MSM suggests that the association between the primary relationship and HIV care engagement might not always be consistently positive.27 These findings warrant a closer look into the dyadic nature of care engagement and treatment adherence in order to explore whether and how supportive dynamics in HIV care engagement could occur among Black MSM couples. Dyadic analysis of overlaps and contrasts of couple members’ narratives illuminated two dimensions of dyadic HIV care engagement, involvement and reciprocity, which together describe the extent and patterns of dyadic coordination in HIV care and treatment. Patterns of involvement showed that while some men were actively involved in their partner’s HIV care and treatment, others were only peripherally involved, and still others were uninvolved. Reciprocity illustrated the extent to which partner involvement was mutual, with patterns that ranged from a mutual give-and-take to asymmetric patterns of care-giving and care-receiving that were more one-sided.
Partners who were mutually involved in each other’s care and treatment had intimate knowledge of each other’s HIV medication regimen as well as the occurrence and frequency of medical appointments. It was common among mutually involved partners to attend each other’s appointments. Partners in some couples were mutually uninvolved in and independent from each other’s care, using terms like “mother” that ascribed caregiving and involvement as a feminine role, something these men do not want to play. This suggests that masculinity among Black men could be a barrier to couple involvement in HIV care engagement, as demonstrated elsewhere.31,32 Other men described getting involved only when their partner was very sick or otherwise compromised and therefore needed their help—a contingent and peripheral “stand-by” type of involvement. Finally, mutual involvement in HIV care and treatment not only occurred in seroconcordant-positive relationships but also in serodiscordant relationships where the HIV-negative partner is on PrEP in the current sample.
The dimension of reciprocity in dyadic relationships helped to elucidate patterns of symmetry or asymmetry in caregiving between relationship partners in the present study. Some men described being more involved in their partner’s care than their partner was in theirs. Among some of the asymmetric relationships where caregiving was one-sided, the caregiving partner commonly resented the asymmetry, and dissatisfaction between the two partners was typical. Interestingly, while some partners of these men denied such accounts, others corroborated them, appearing to be content with the caregiving asymmetry in their relationship. Indeed, dyadic coordination of HIV care nevertheless occurred even among couples where both partners’ disagreed on which partner was more of the caregiver than the other. These findings suggest that some men may still be involved in each other’s HIV care and treatment regardless of disagreements and relationship quality.
Patterns of involvement did not appear to be directly related to how HIV-positive men viewed their partner and/or their relationship, nor did it appear to be more or less common among men who cohabitated and/or have been together longer. Rather, active involvement appeared to be most directly related to how men saw their role as caregivers in the relationship and whether or not caregiving was reciprocal.33 Research suggests that positive relational factors such as high levels of relationship satisfaction and quality may be important for optimal HIV care engagement. Our findings suggest that dyadic coordination of HIV care and treatment occurred among “happy” and “unhappy” couples alike. Indeed, even as some partners expressed dissatisfaction in their relationship, dyadic coordination of HIV care and treatment still occurred as part of daily routines, having been incorporated into how partners interacted with each other to meet needs. This paradox is consistent with findings among other samples of couples living with HIV and suggests that for some couples, the provision of HIV-related support does not hinge on relationship dynamics such as satisfaction.34 Dyadic coordination of HIV care and treatment is an important way for individuals in couples to meet their needs, an explanation supported by a transactional, need-based perspective of interdependent relationships.35 Furthermore, needs may include the need to provide caregiving for a partner or perhaps the need to feel close to a partner by providing support.35–37 Future research should explore whether or not contingency of behavior and obligation continue over the course of the relationship irrespective positive relational dynamics (e.g., relationship satisfaction, trust, intimacy), and to examine the temporality of such dyadic coordination, that is, how dyadic coordination might continue over time.
As men age, the management of multiple chronic health conditions becomes more common. Caregiving in the context of the primary romantic relationship may encapsulate all aspects of healthcare—not just exclusively for HIV care and treatment. Comorbidity was common in the current sample, and our findings suggest that men did not differentiate between caregiving for HIV and caregiving for other chronic disease(s). Whether or not dyadic coordination of HIV care and treatment is more or less likely when other chronic health conditions are present is a topic for future research.
Limitations
The sample was comprised of mostly seroconcordant-positive couples, and all three serodiscordant couples reported PrEP uptake. As such, dyadic coordination of HIV care and treatment among discordant couples that do not use PrEP may not have been adequately represented. Our sample of couples is restricted to a geographic region of the country where HIV care and treatment services are relatively abundant and where Black MSM relationships may be less stigmatized than in other areas of the US.38,39
Research Implications
The present study aimed to examine how involved are primary relationship partners are and what patterns of involvement look like in HIV care engagement among Black MSM couples. There may be different types of interventions tailored to different patterns of dyadic coordination, depending on how couples differ along the dimensions of involvement and reciprocity. Just as some of these partnered men might benefit more from couple-focused interventions, some men may benefit more from individual-focused interventions. Interventions for HIV care engagement among Black MSM couples should determine both partners’ level of involvement and whether or not it is reciprocated in the relationship in tailoring the appropriate content for targeting that pattern of dynamics. The model may guide the design of interventions for improving HIV care engagement among couples by breaking down patterns of behavior into individual and dyadic aspects that may be better targeted for change. Intervention modules can be tailored to target or account for different dyadic coordination patterns in optimizing intervention effectiveness with couples.
Acknowledgments
J.Y. Tan was supported by a National Institute of Mental Health (NIMH) Mentored Research Scientist Award (K01 MH106416). A.A. Conroy was supported by a NIMH Mentored Research Scientist Award (K01 MH107331).
Footnotes
Compliance with Ethical Standards
JY Tan declares that she has no conflicts of interest. CK Campbell declares he has no conflicts of interest. AP Tabrisky declares that she has no conflicts of interest. R. Siedle-Khan declares he has no conflicts of interest. AA Conroy declares that she has no conflicts of interest. All procedures performed in this study were in accordance with the ethical standards of the UCSF Committee of Human Research/Institutional Review Board, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in this study.
References
- 1.Sullivan PS, Peterson J, Rosenberg ES, et al. Understanding racial HIV/STI disparities in black and white men who have sex with men: A multilevel approach. PLoS One. 2014;9(3):e90514. doi: 10.1371/journal.pone.0090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rosenberg ES, Millett GA, Sullivan PS, del Rio C, Curran JW. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: A modelling study. Lancet HIV. 2014;1(3):e112–e118. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet. 2012;380(9839):341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan PS, Rosenberg ES, Sanchez TH, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: A prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–454. doi: 10.1016/j.annepidem.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011;25(8):1103–1112. doi: 10.1097/QAD.0b013e3283471efa. [DOI] [PubMed] [Google Scholar]
- 6.Koblin BA, Mayer KH, Eshleman SH, et al. Correlates of HIV acquisition in a cohort of black men who have sex with men in the United States: HIV prevention trials network (HPTN) 061. PloS One. 2013;8(7):e70413. doi: 10.1371/journal.pone.0070413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoff C. Negotiated safety agreements: Do they protect and how they protect. Focus. 2005;20(2):1–5. [PubMed] [Google Scholar]
- 8.Hoff CC, Beougher SC. Sexual agreements among gay male couples. Arch Sex Behav. 2010;39(3):774–787. doi: 10.1007/s10508-008-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campbell CK, Gomez AM, Dworkin S, et al. Health, trust, or “Just understood”: Explicit and implicit condom decision-making processes among black, white, and interracial same-sex male couples. Arch Sex Behav. 2014;43(4):697–706. doi: 10.1007/s10508-013-0146-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eaton LA, Kalichman SC, Cherry C. Sexual partner selection and HIV risk reduction among black and white men who have sex with men. Am J Public Health. 2010;100(3):503–509. doi: 10.2105/AJPH.2008.155903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conroy AA, Gamarel KE, Neilands TB, Dilworth SE, Darbes LA, Johnson MO. Relationship dynamics and partner beliefs about viral suppression: A longitudinal study of male couples living with HIV/AIDS (the DUO project) AIDS Behav. 2016;20(7):1572–1583. doi: 10.1007/s10461-016-1423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horvath KJ, Smolenski D, Iantaffi A, Grey JA, Rosser BS. Discussions of viral load in negotiating sexual episodes with primary and casual partners among men who have sex with men. AIDS Care. 2012;24(8):1052–1055. doi: 10.1080/09540121.2012.668168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prestage G, Mao L, Kippax S, et al. Use of viral load to negotiate condom use among gay men in Sydney, Australia. AIDS Behav. 2009;13(4):645. doi: 10.1007/s10461-009-9527-0. [DOI] [PubMed] [Google Scholar]
- 14.Neme S, Goldenberg T, Stekler JD, Sullivan PS, Stephenson R. Attitudes towards couples HIV testing and counseling among Latino men who have sex with men in the Seattle area. AIDS Care. 2015;27(10):1354–1359. doi: 10.1080/09540121.2015.1058894. [DOI] [PubMed] [Google Scholar]
- 15.Stephenson R, Sullivan PS, Salazar LF, Gratzer B, Allen S, Seelbach E. Attitudes towards couples-based HIV testing among MSM in three US cities. AIDS Behav. 2011;15(1):80–87. doi: 10.1007/s10461-011-9893-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell C, Hoff C, Kolber J, Chakravarty D, Neilands T, Grisham K. PrEP uptake, dyadic decision-making, and condom use among HIV-negative men in committed same-sex male relationships. Presented at: National HIV Prevention Conference; December 6–9, 2015; Atlanta, GA. [Google Scholar]
- 17.Johnson MO, Dilworth SE, Neilands TB. Partner reports of patients’ HIV treatment adherence. J Acquir Immune Defic Syndr. 2011;56(4):e117–8. doi: 10.1097/QAI.0b013e31820bd2ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stumbo S, Wrubel J, Johnson MO. A qualitative study of HIV treatment adherence support from friends and family among same sex male couples. Psychol Educ. 2011;2(4):318–322. doi: 10.4236/psych.2011.24050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wrubel J, Stumbo S, Johnson MO. Male same-sex couple dynamics and received social support for HIV medication adherence. J Soc Pers Relat. 2010;27(4):553–572. doi: 10.1177/0265407510364870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conroy A, Leddy A, Johnson M, Ngubane T, van Rooyen H, Darbes L. ‘I told her this is your life’: Relationship dynamics, partner support and adherence to antiretroviral therapy among South African couples. Cult Health Sex. 2017:1–15. doi: 10.1080/13691058.2017.1309460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conroy AA, McKenna SA, Leddy A, et al. “If she is drunk, I don’t want her to take it”: Partner beliefs and influence on use of alcohol and antiretroviral therapy in South African couples. AIDS Behav. 2017:1–7. doi: 10.1007/s10461-017-1697-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wrubel J, Stumbo S, Johnson MO. Antiretroviral medication support practices among partners of men who have sex with men: A qualitative study. AIDS Patient Care STDS. 2008;22(11):851–858. doi: 10.1089/apc.2008.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson MO, Dilworth SE, Taylor JM, Darbes LA, Comfort ML, Neilands TB. Primary relationships, HIV treatment adherence, and virologic control. AIDS Behav. 2012;16(6):1511–1521. doi: 10.1007/s10461-011-0021-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Millett GA, Flores SA, Peterson JL, Bakeman R. Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS. 2007;21(15):2083. doi: 10.1097/QAD.0b013e3282e9a64b. [DOI] [PubMed] [Google Scholar]
- 25.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: A critical literature review. Am J Public Health. 2006;96(6):1007. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peterson JL, Bakeman R, Sullivan P, et al. Social discrimination and resiliency are not associated with differences in prevalent HIV infection in black and white men who have sex with men. J Acquir Immune Defic Syndr. 2014;66(5):538–543. doi: 10.1097/QAI.0000000000000203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan JY, Pollack L, Rebchook G, et al. The role of the primary romantic relationship in HIV care engagement outcomes among young HIV-positive black men who have sex with men. AIDS Behav. 2016:1–17. doi: 10.1007/s10461-016-1601-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eisikovits Z, Koren C. Approaches to and outcomes of dyadic interview analysis. Qual Health Res. 2010;20(12):1642–1655. doi: 10.1177/1049732310376520. [DOI] [PubMed] [Google Scholar]
- 29.Koren C, Eisikovits Z. Life beyond the planned script: Accounts and secrecy of older persons living in second couplehood in old age in a society in transition. J Soc Pers Relat. 2011;28(1):44–63. [Google Scholar]
- 30.Lieber E, Weisner T, Taylor J. Dedoose software. California: Sociocultural Research Consultants; 2011. [Google Scholar]
- 31.Skovdal M, Campbell C, Madanhire C, Mupambireyi Z, Nyamukapa C, Gregson S. Masculinity as a barrier to men’s use of HIV services in Zimbabwe. Globalization and health. 2011;7(1):13. doi: 10.1186/1744-8603-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siu GE, Seeley J, Wight D. Dividuality, masculine respectability and reputation: How masculinity affects men’s uptake of HIV treatment in rural eastern Uganda. Soc Sci Med. 2013;89:45–52. doi: 10.1016/j.socscimed.2013.04.025. [DOI] [PubMed] [Google Scholar]
- 33.Gamarel KE, Neilands TB, Golub SA, Johnson MO. An omitted level: An examination of relational orientations and viral suppression among HIV serodiscordant male couples. J Acquir Immune Defic Syndr. 2014;66(2):193–196. doi: 10.1097/QAI.0000000000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conroy A, Comfort M, Darbes LA, Johnson MO, Van Oosterhout JJG, Mkandawire J. Exploring linkages between couple functioning and adherence to ART in malawi: A dyadic perspective. Oral presentation to be given at the AIDS impact 13th international conference; Cape Town, South Africa. 13–15 november 2017. [Google Scholar]
- 35.Tan JY, Pratto F, Paul J, Choi K. A social-ecological perspective on power and HIV/AIDS with a sample of men who have sex with men of colour. Cult Health Sex. 2014;16(2):1–14. doi: 10.1080/13691058.2013.855821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pratto F, Lee I, Tan JY, Pitpitan E. Power basis theory: A psycho-ecological approach to power. In: Dunning D, editor. Social motivation. New York: Psychology Press; 2010. [Google Scholar]
- 37.Tan JY, Conroy AA, Lee IC, Pratto F. Leveraging power in intimate partner relationships: A power bases perspective. In: Agnew CR, Harman JJ, editors. Power in close relationships. Cambridge University Press; 2017. [Google Scholar]
- 38.Preston DB, D’Augelli AR, Kassab CD, Cain RE, Schulze FW, Starks MT. The influence of stigma on the sexual risk behavior of rural men who have sex with men. AIDS Educ Prevent. 2004;16(4):291–303. doi: 10.1521/aeap.16.4.291.40401. [DOI] [PubMed] [Google Scholar]
- 39.Schwartz SR, Nowak RG, Orazulike I, et al. The immediate effect of the same-sex marriage prohibition act on stigma, discrimination, and engagement on HIV prevention and treatment services in men who have sex with men in Nigeria: Analysis of prospective data from the TRUST cohort. Lancet HIV. 2015;2(7):e299–e306. doi: 10.1016/S2352-3018(15)00078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]