Abstract
The occurrence of permanent patellar dislocation associated with severe osteoarthritis is considered rare and difficult to treat. Literature: The literature is quite controversial on the subject. The objective of the study is to report two rare cases of severe osteoarthritis with permanent dislocation of the patella that underwent total knee arthroplasty, in addition to a review of the literature on the subject and related surgical technique. Total knee arthroplasty with using the medial parapatellar approach associated with lateral release was a good surgical option in patients with permanent patellar dislocation associated with advanced osteoarthritis.
Keywords: Arthroplasty, replacement, knee; Patella; Dislocation
Resumo
A ocorrência de luxação permanente da patela associada a osteoartrite grave é considerada rara e de tratamento difícil. A literatura é bastante controversa sobre o assunto. O objetivo do trabalho é relatar dois raros casos de osteoartrite grave com luxação permanente da patela que foram submetidos a artroplastia total do joelho, além da técnica cirúrgica relacionada e de uma revisão da literatura. A artroplastia total do joelho com o acesso parapatelar medial associado a uma liberação lateral foi uma boa opção cirúrgica em pacientes com luxação permanente da patela associada a osteoartrite avançada.
Palavras-chave: Artroplastia do joelho, Patela, Luxação
Introduction
Total knee arthroplasty (TKA) is a highly complex surgical procedure, primarily indicated in patients with a diagnosis of knee osteoarthritis or rheumatologic diseases.1 It is a surgical procedure that has been constantly evolving since its inception. More modern implant models, which resemble as close as possible the anatomy of the knee, associated with increasingly precise and less traumatic instruments, have made surgical indications more and more widespread.1
Permanent patellar dislocation is a rare condition of congenital or acquired etiology.2 The literature that correlates TKA and osteoarthritis with the presence of permanent patellar dislocation is scarce.3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19 In this literature review, the authors observed that, among the various difficulties, surgical approach is one that deserves attention, as there is no consensus regarding which is the best option. This study is aimed at presenting two cases of permanent patellar dislocation in patients with osteoarthritis who underwent TKA. The authors also reviewed the literature and emphasized the controversy on the subject.
Case 1
A 65-year-old obese female patient presented severe pain in the right knee. On clinical examination, it was observed that the patient had suffered trauma on the same knee with three years of evolution. The patient did not seek medical attention because of the trauma, as she already had pain due to osteoarthritis. She reported having developed a marked edema in her right knee, that gradually disappeared. She also reported having developed greater difficulty in conducting her usual activities. Upon physical examination, she presented a fixed valgus deformity, a range of motion from 0° to 70°, and a painful crepitus in the joint. Minimal patellar mobility was observed during flexion and extension movements. No joint effusion was observed, nor any signs of instability or ligament deficiency.
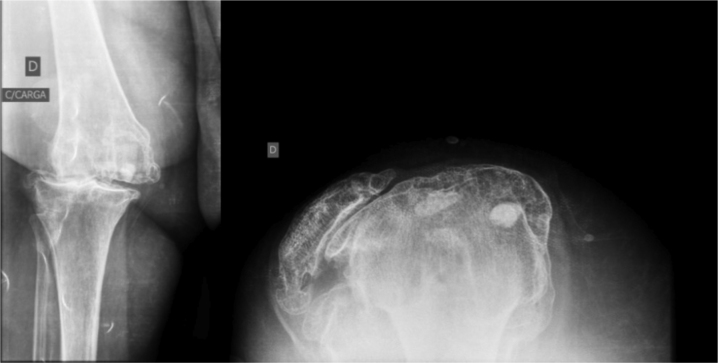
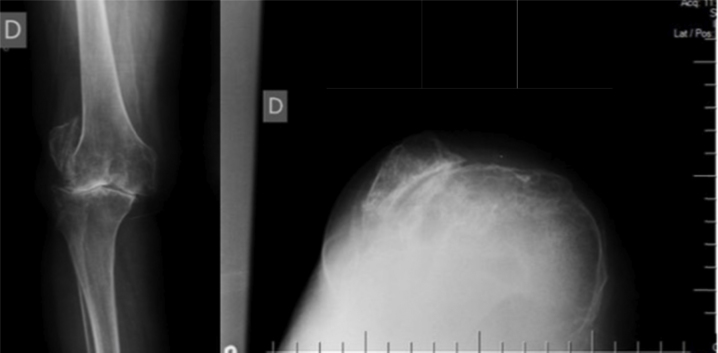
Weight-bearing anteroposterior, lateral, and Merchant axial views knee radiographs showed a valgus deformity, the presence of osteoarthritis in all compartments, and absence of the patella in the anterior compartment of the knee, i.e., a permanent lateral dislocation of the patella (Fig. 1).
Fig. 1.
Preoperative radiological evaluation.
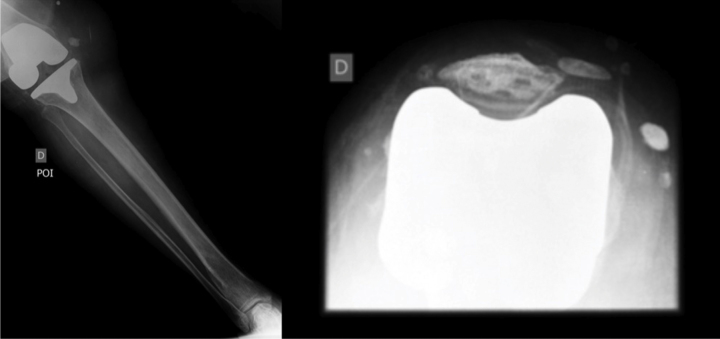
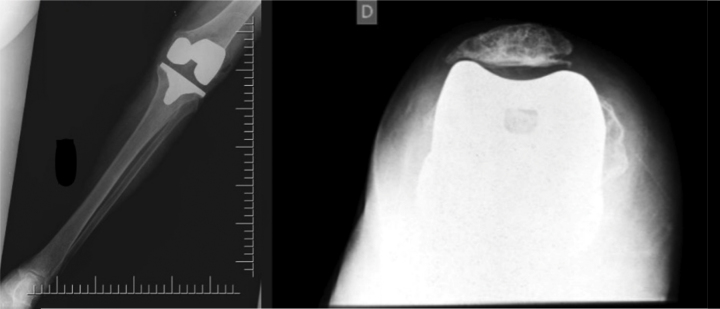
In August 2014, the patient underwent right TKA. A posterior-stabilized implant model was chosen, and patellar replacement (PFC Sigma® DePuy Synthes) was also performed (Fig. 2). A medial parapatellar approach was chosen, associated with an extensive lateral retinacular release (Fig. 3).
Fig. 2.
Postoperative radiological evaluation.
Fig. 3.
Intraoperative evaluation.
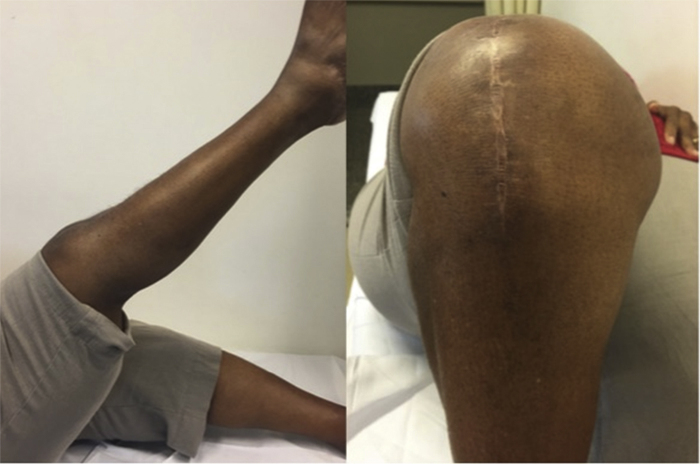
In the immediate postoperative period, the patient showed improvement of pain and knee function. She returned to her usual activities and was satisfied with the surgical procedure. The patient's function was assessed using the Knee Society Score (KSS),20 which improved from 42 in the preoperative period to 91 in the postoperative period with two years of clinical follow-up (Fig. 4).
Fig. 4.
Postoperative clinical evaluation.
Case 2
Female patient, 77 years old, overweight and with intense pain in her right knee. On clinical examination, the patient mentioned having suffered trauma in the same knee with six years of evolution. The patient did not seek medical attention because of the trauma, as she already had pain due to osteoarthritis. She reported a significant swelling in her right knee after the trauma, which progressively improved. After the trauma, she observed a greater difficulty in performing her usual activities. Upon physical examination, she presented a fixed varus deformity, a range of motion from 0° to 60°, and a painful crepitus in the joint. Minimal patellar mobility was observed during flexion and extension movements. No joint effusion was observed, nor any signs of instability or ligament deficiency.
Weight-bearing anteroposterior, lateral and Merchant axial views knee radiographs showed a varus deformity, the presence of tricompartmental osteoarthritis, and absence of the patella in the anterior compartment of the knee, i.e., it was dislocated, in direct contact with the external border of the lateral femoral condyle (Fig. 5).
Fig. 5.
Preoperative radiological evaluation.
In March 2014, the patient underwent a right TKA. A posterior-stabilized implant model was used, with a patellar replacement (PFC Sigma® DePuy Synthes) (Fig. 6). A medial parapatellar approach was chosen, associated with an extensive lateral retinacular release.
Fig. 6.
Postoperative radiological evaluation.
In the immediate postoperative period, the patient presented pain relief and functional improvement of the knee. She returned to her daily activities and was satisfied with the surgical procedure. The patient's function was evaluated using the KSS,20 which improved from 25 in the preoperative period to 82 in the postoperative period with two years of clinical follow-up (Fig. 7).
Fig. 7.
Postoperative clinical evaluation.
Discussion
Irreducible patellar dislocation is a rare condition, usually presenting a congenital origin, although some cases have acquired etiology.13 Acquired patellar dislocation is usually secondary to knee trauma.13 In the present report, the two cases presented a history of prior trauma. However, the presence of dysplastic trochlea was observed intraoperatively. This indicates the multifactorial etiology of these cases. Hudson et al.15 stated that post-traumatic permanent patellar dislocation is often confused with congenital patellar dislocation. Nonetheless, the present authors consider that regardless of the etiology, the main objective is the patellofemoral alignment after TKA.
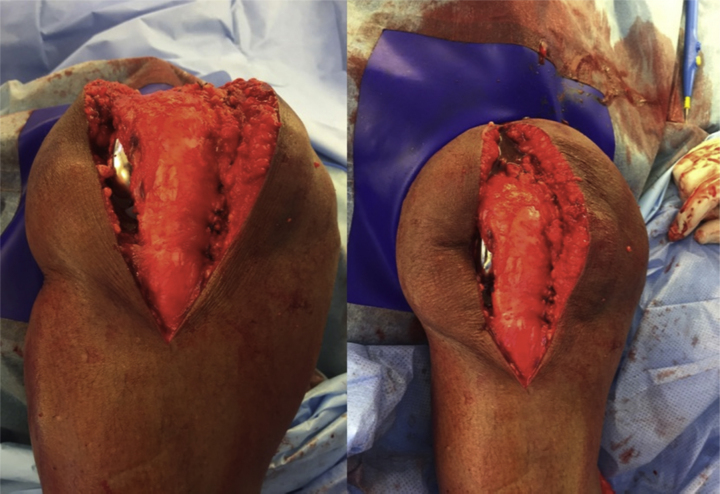
Knee anatomy, in this type of pathology, presents a hypoplastic patella and femoral condyle, as well as a flat femoral groove.13 In the present series, anatomical alterations of the trochlea were observed (Fig. 8). Hudson et al.15 reported an adaptive change of the trochlear cartilage, besides that of the lateral femoral condyle and articular surface of the patella.
Fig. 8.
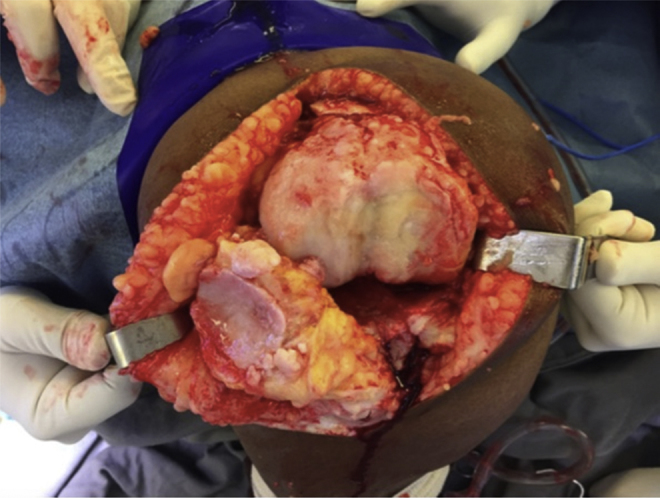
Intraoperative knee anatomy.
Chronic patellar dislocation is correlated with a valgus deformity in knee osteoarthritis.10 The present study presented one case of valgus deformity and another with varus deformity, emphasizing the rarity of this case series. In their report, Hudson et al.15 also observed varus deformity.
TKA is a valid procedure for adult patients with patellar dislocation associated with osteoarthritis and absence of the femoral sulcus.3 These anatomical deformities make the surgical procedure more intricate. Preoperative planning is fundamental to achieve patellar alignment.11 In order to minimize possible complications, a thorough clinical and radiological evaluation is essential.
There is controversy regarding realignment of the extensor apparatus.16 The authors who defend non-realignment of the extensor apparatus claim that patients are able to adapt to this situation.8, 9, 16 In contrast, In et al.2 stated that in TKA with patellar dislocation, realignment of the extensor mechanism is mandatory. The present authors consider the realignment of the extensor apparatus to be fundamental to gain of range of motion and for prosthesis survival. Tunay et al.3 stated that the realignment of the extensor mechanism restores the strength of the quadriceps and aids the biomechanics of the knee, besides being able to prevent complications.
Most surgeons are more familiar with the medial parapatellar approach. However, the lateral parapatellar approach may be the most appropriate for this condition.19 The lateral access allows a release of the retracted structures of this compartment and, consequently, patellar alignment.19 The preference of the surgeon should be respected, but the analysis of the knee deformity and of the contractured structures facilitates the choice of the apt access route.
Some studies have used the medial parapatellar approach with extensive lateral release.3, 5, 6, 7, 9, 13, 15, 16, 17 Rozell et al.17 emphasize the importance of adequate lateral release. Likewise, the present authors believe that a gradual lateral release can generate correct patellar alignment. In the present study, the lateral release was initiated by opening the retinaculum to the level of the patella. At that moment, knee flexion and extension movements were performed to evaluate the patellofemoral alignment. In the persistence of patellofemoral imbalance, the release was progressively extended to the proximal and distal regions of the patella. The no thumb test was repeated successively until the correct patellar alignment was achieved. The vastus lateralis was not stretched, thereby preserving the arterial supply of the superior lateral genicular artery.
Tunay et al.3 advocate the use of the medial parapatellar approach with extensive lateral release. These authors observed a shortening of the extensor mechanism that, consequently, hindered patellar reduction.3 Thus, quadriceps elongation was added using the Vulpius technique.3 The authors reaffirm that good patellofemoral congruence is key to success, thus justifying the use of any surgical technique for this purpose.
The medial parapatellar approach associated with lateral release may lead to loss of blood supply to the patella.2, 18 Because of this, some defend the subvastus approach, associated with lateral release.2, 18 In et al.2 observed one case of patellar tilt in their series with this surgical approach. In turn, Junqueira et al.14 reported a good result in their published case. However, those authors did not present an axial patellar radiograph. Baldini et al.18 reported that a lower limb panoramic view and the axial patellar view radiographs are fundamental in the assessment of this condition. The present authors consider the axial patellar view to be paramount for evaluating patellofemoral congruence, and that patellar tilt may cause pain and early implant wear.
In TKA with permanent patellar dislocation, reinforcement with the medial patellofemoral ligament is a useful alternative.4, 12 Two studies have used the lateral parapatellar approach associated with reconstruction of the medial patellofemoral ligament. Matsushita et al.12 concluded that, in cases of patellar dislocation, after ligamentous balancing, a proximal realignment or an anterior tibial tuberosity (ATT) osteotomy should be performed. In turn, Yamanaka et al.11 believe that the lateral parapatellar access should be made associated with ATT osteotomy during TKA. These authors also advocate the use of a tibial stem in the knee prosthesis when performing ATT osteotomy.11 Due to the occurrence of tibial fracture during the procedure, ATT osteotomy was avoided on the contralateral side.11 The authors believe that, in special situations, the reconstruction of the medial patellofemoral ligament or ATT osteotomy are alternatives that contribute to the patellofemoral balance.
Dao et al.10 performed the turndown approach in the quadriceps and a medial advancement. One case of patellar tilt was observed in their series.10 A turndown-type access may be considered unnecessary for this condition.
Some authors have opted for a greater external rotation of the femoral and tibial components.12 They state that in this way there was better patellar sliding. In contrast, In et al. used the pre-established classical patterns of external rotation of the femoral component and tibial alignment.2 The present authors believe that the soft tissue balance should be considered in order to achieve correct patellar alignment. Component rotation is considered to be another factor of postoperative complications.
Hau and Newman19 state that tibiofemoral instability can occur in these cases. Because of this, some authors recommend the use of a more constricted prosthesis.7, 8, 9, 13, 16 Hudson et al.15 used an implant with minor constriction, believing that the degree of deformity or instability was minimal. They concluded that the choice of prosthesis constriction depends on the case. The present authors agree with this statement and consider that more constricted implants have shorter survival.
Patellar replacement should always be performed in the same surgical procedure that corrects the hypoplastic surface of the patella.3 The present authors are in agreement with this theory and contraindicate its use only in cases of patellar thickness less than 12 mm.
The matter is controversial. The literature is scarce and is primarily composed of case reports, which justifies and increases the relevance of the present literature review, which can help the orthopedist in conducting adequate planning when faced with this condition.
TKA by medial parapatellar approach associated with lateral release was a good option for patients with permanent patellar dislocation associated with advanced osteoarthritis.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at the Instituto Nacional de Traumatologia e Ortopedia, Centro de Cirurgia do Joelho, Rio de Janeiro, RJ, Brazil.
References
- 1.Barretto J.M., Malta M., Albuquerque R.P., Assis D.P., Campos A.S. Avaliação a médio prazo da artroplastia total de joelho com implante de fabricação nacional. Rev Bras Ortop. 2011;46(5):540–545. [Google Scholar]
- 2.In Y., Kong C.G., Sur Y.J., Choi S.S. TKA using the subvastus approach and lateral retinacular release in patients with permanent post-traumatic patellar dislocation: a report of two cases. Knee Surg Sports Traumatol Arthrosc. 2009;17(3):254–259. doi: 10.1007/s00167-008-0676-x. [DOI] [PubMed] [Google Scholar]
- 3.Tunay S., Ozkan H., Köse O., Atik A., Basbozkurt M. Total knee arthroplasty in a patient with neglected congenital patellar dislocation. Orthopedics. 2009;32(10) doi: 10.3928/01477447-20090818-22. [DOI] [PubMed] [Google Scholar]
- 4.Sato H., Ishibashi Y., Tsuda E., Sasaki K., Toh S. Total knee arthroplasty for gonarthrosis with patellar dislocation. J Orthop Sci. 2005;10(6):656–660. doi: 10.1007/s00776-005-0948-y. [DOI] [PubMed] [Google Scholar]
- 5.Kumagi M., Ikeda S., Uchida K., Ono T., Tsumara H. Total knee replacement for osteoarthritis of the knee with congenital dislocation of the patella. J Bone Jt Surg Br. 2007;89(11):1522–1524. doi: 10.1302/0301-620X.89B11.19598. [DOI] [PubMed] [Google Scholar]
- 6.Hanssen A.D., Rand J.A. Management of chronically dislocated patella during total knee arthroplasty. Tech Orthop. 1998;3(2):39–42. [Google Scholar]
- 7.Bergquist P.E., Baumann P.A., Finn H.A. Total knee arthroplasty in an adult with congenital dislocation of the patella. J Arthroplasty. 2001;16(3):384–388. doi: 10.1054/arth.2001.20545. [DOI] [PubMed] [Google Scholar]
- 8.Marmor L. Knee arthroplasty in a patient with congenital dislocation of the patella. Case report. Clin Orthop Relat Res. 1988;226:129–133. [PubMed] [Google Scholar]
- 9.Pradhan R.L., Watanabe W., Itoi E., Yamada S., Shimada Y., Sato K. Total knee arthroplasty in bilateral congenital dislocation of the patella – a case report. Acta Orthop Scand. 2001;72(4):422–424. doi: 10.1080/000164701753542113. [DOI] [PubMed] [Google Scholar]
- 10.Dao Q., Chen D.B., Scott R.D. Proximal patellar quadricepsplasty realignment during total knee arthroplasty for irreducible congenital dislocation of the patella: a report of two cases. J Bone Jt Surg Am. 2010;92(14):2457–2461. doi: 10.2106/JBJS.H.00812. [DOI] [PubMed] [Google Scholar]
- 11.Yamanaka H., Kawamoto T., Tamai H., Suzuki M., Kobayashi T., Eguchi Y. Total knee arthroplasty in a patient with bilateral congenital dislocation of the patella treated with a different method in each knee. Case Rep Orthop. 2015;2015:890315. doi: 10.1155/2015/890315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Matsushita T., Kuroda R., Kubo S., Mizuno K., Matsumoto T., Kurosaka M. Total knee arthroplasty combined with medial patellofemoral ligament reconstruction for osteoarthritic knee with preoperative valgus deformity and chronic patellar dislocation. J Arthroplasty. 2011;26(3) doi: 10.1016/j.arth.2010.01.101. 505.e17–20. [DOI] [PubMed] [Google Scholar]
- 13.Bullek D.D., Scuderi G.R., Insall J.N. Management of the chronic irreducible patellar dislocation in total knee arthroplasty. J Arthroplasty. 1996;11(3):339–345. doi: 10.1016/s0883-5403(96)80090-8. [DOI] [PubMed] [Google Scholar]
- 14.Junqueira J.J.M., Helito C.P., Bonadio M.B., Pécora J.R., Demange M.K. Artroplastia total de joelho por via subvasto em paciente com luxação crônica pós-traumática de patela. Rev Bras Ortop. 2016;51(5):614–618. doi: 10.1016/j.rboe.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hudson J., Reddy V.R., Krikler S.J. Total knee arthroplasty for neglected permanent post-traumatic patellar dislocation – case report. Knee. 2003;10(2):207–212. doi: 10.1016/s0968-0160(02)00144-8. [DOI] [PubMed] [Google Scholar]
- 16.Oh K.J., Yoon J.R., Yang J.H. Total knee arthroplasty in a pseudoachondroplastic dwarfism patient with bilateral patellar dislocation. Knee. 2013;20(1):45–48. doi: 10.1016/j.knee.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Rozell J.C., Voleti P.B., Israelite C.L. Patellar dislocation after total knee arthroplasty for neglected chronic post-traumatic patellar dislocation: a case report. UPOJ. 2015;25(1):75–78. [Google Scholar]
- 18.Baldini A., Castellani L., Traverso F., Balatri A., Balato G., Franceschini V. The difficult primary total knee arthroplasty: a review. Bone Jt J. 2015;97-B(Suppl. A):30–39. doi: 10.1302/0301-620X.97B10.36920. [DOI] [PubMed] [Google Scholar]
- 19.Hau R.C., Newman J.H. Knee replacement for osteoarthritis secondary to chronic patellar dislocation and trochlear dysplasia. Knee. 2008;15(6):447–450. doi: 10.1016/j.knee.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 20.Silva A.L., Demange M.K., Gobbi R.G., da Silva T.F., Pécora J.R., Croci A.T. Translation and validation of the Knee Society Score – KSS for Brazilian Portuguese. Acta Ortop Bras. 2012;20(1):25–30. doi: 10.1590/S1413-78522012000100005. [DOI] [PMC free article] [PubMed] [Google Scholar]