Abstract
Objective
To estimate whether the incidence of low birthweight and rates of infant mortality were associated with Massachusetts health reform in the overall population and for subgroups that are at higher risk for poor health outcomes.
Data Sources
Individual‐level data on birthweight were obtained from the National Center for Health Statistics detailed natality files, and aggregated county‐level mortality rates were generated from linked birth–death files. We used restricted versions of each file that had intact state and substate geographic identifiers.
Research Design
We employed a quasi‐experimental difference‐in‐differences design.
Principal Results
We found small and statistically nonsignificant associations between the reform and the incidence of low birthweight and infant mortality rates. Results were consistent across a number of subgroups and were robust to alternative comparison groups and alternative modeling assumptions.
Conclusions
We found no evidence that the Massachusetts reform was associated with improvements in individual low birthweights or county‐level infant mortality rates, despite increasing health insurance coverage rates for adult women of child‐bearing age. Because our mortality analysis was ecological, we are not able to draw conclusions about how an individual‐level health insurance intervention for uninsured pregnant women would affect the mortality outcomes of their infants.
Keywords: Health insurance, health reform, infant mortality, low birthweight
Since the 1960s, U.S. policy makers have sought to improve infant health outcomes by expanding access to health insurance, and they have done so with mixed results (Institute of Medicine 1985; Howell 2001; Goodman‐Bacon 2016). In this study, we examined whether the Massachusetts' 2006 health reform initiative was associated with changes in two infant health outcomes: low birthweight and the infant mortality rate. The Massachusetts example is a particularly important case to study both because it foreshadowed the Affordable Care Act (ACA) and, like the ACA, it featured a set of unique policy parameters that separated it from previous Medicaid expansions (e.g., an individual mandate and an outreach initiative that drove high take‐up, even among those previously eligible for public coverage). This is the first study, to our knowledge, to examine the associations of the Massachusetts reform with low birthweight and infant mortality rates.
Background
The production of infant health is a complex process involving many medical and social factors that play out over the course of a woman's life (Lu and Halfon, 2003). There are two primary pathways that could link health insurance expansion to infant health. The first is improved access to medical care. While the evidence is mixed, preconception, interconception, and prenatal care may improve health at birth by identifying and treating maternal risk factors and by modifying maternal health behaviors such as smoking that are known to be associated with poor health at birth (Badura et al. 2008; Simon and Handler 2008; Currie and Rossin‐Slater 2014). Improved access to medical technology at birth and during the first few months of life might improve health and survivability, conditional on health at birth (Phibbs et al. 2007). The second pathway through which expanded health insurance (and publicly subsidized insurance in particular) might improve infant health is by freeing up financial resources that would have otherwise gone to out‐of‐pocket medical expenses. Families may reallocate such resources to activities known to be associated with infant health (e.g., nutrition) and/or improved financial conditions might reduce stress.
Previous evaluations of Medicaid have indeed found that health insurance expansions reduce infant mortality. For example, Goodman‐Bacon (2016) found that the introduction of Medicaid in the late 1960s led to sizable decreases in infant mortality. Currie and Gruber (1996) found similar evidence stemming from the expansions of the 1980s. In both cases, mortality effects appeared to be driven by improved access to hospital care after birth, rather than improved health at birth as measured by birthweight. Despite plausible conceptual models linking health insurance, access to care during pregnancy, and the eventual health of infants, both studies found small to null effects on the incidence of low birthweight. These findings are consistent with other state‐specific studies of Medicaid expansion (Howell 2001).
The policy parameters of previous Medicaid expansions might account for small to null effects on health at birth and larger effects on survival. At its inception and during the expansionary period of the 1980s and 1990s, Medicaid eligibility for low‐income adult women was conditioned on parenting or pregnancy and the application process was burdensome and time consuming. The combination of restrictive categorical‐based eligibility and low take‐up may have delayed entry into prenatal care and/or reduced access to preconception care. These barriers may have attenuated potential effects on health at birth and subsequent mortality (Currie and Gruber 1996; Currie and Grogger 2002; Rosenberg et al. 2007). Despite less than perfect take‐up during early periods of pregnancy or the preconception period, uninsured women and their infants qualifying for Medicaid were very likely to obtain coverage at the point of delivery because hospitals faced strong incentives to enroll otherwise uninsured women (via presumptive eligibility). Access to Medicaid at the time of birth may have improved infants' access to life‐saving hospital services (Currie and Gruber 1996, 1997; Currie and Grogger 2002).
The policy characteristics of the Affordable Care Act (ACA), and the 2006 Massachusetts reforms that preceded it, differed from prior Medicaid expansions in ways that might be important for infant health outcomes. Public health insurance was expanded to low‐income populations regardless of family structure. The individual market was reformed through guaranteed issue and community rating. Low‐ and middle‐income consumers not eligible for Medicaid were given tax credits to offset the costs of private coverage. Importantly, coverage options for adults were not conditional on parenting or pregnancy status, many residents were required to obtain coverage or face a penalty, and the reforms were accompanied by large outreach efforts. In Massachusetts, the result of the 2006 reform was high take‐up of insurance coverage even among groups that were previously eligible, but had not enrolled in Medicaid (Sonier, Boudreaux, and Blewett 2013). A similar “welcome mat” effect is now being observed for the ACA (Frean, Gruber, and Sommers 2016). As a result of more timely take‐up, some women may have gained coverage or obtained more generous coverage early in pregnancy or been covered during the interconception period. As a consequence, the Massachusetts reform may have affected infant health differently than previous Medicaid expansions. On the other hand, the Massachusetts reform may have had a more modest effect on outcomes compared to Medicaid's introduction or expansion in the 1980s, given that it targeted a less disadvantaged population.
The Context in Massachusetts
In 2005, one year before Massachusetts enacted reform, 7.8 percent of Massachusetts infants were born with low birthweight (<2,500 g), 10 percent were deemed in less than excellent health based on 5‐minute Apgar scores, and the infant mortality rate was 5.1 per 1,000 deliveries (Centers for Disease Control and Prevention 2014). Infant health outcomes in Massachusetts were only slightly better than the average across the 50 states and the District of Columbia. Poor infant health outcomes in Massachusetts, like the rest of the United States, were not equally distributed. For example, in 2005, the African American infant mortality rate (IMR) in Massachusetts was 2.3 times the state average and the Hispanic IMR was 1.4 times that of the state average (Caceres, Orejuela‐Hood, and West 2016).
Despite an already robust health care system that included ambulatory and hospital care that was higher than average in quality and despite high levels of prereform insurance coverage, previous studies of child and adult outcomes have found that the reform led to reductions in unmet medical needs and increased use of preventative services (Long et al. 2010; Kolstad and Kowalski 2012; Agency for Health Care Research and Quality, 2016). Self‐reported health improved and all‐cause adult mortality for adults declined by 3 percent (Courtemanche and Zapata 2013; Sommers, Long, and Baiker 2014). Not only did the Massachusetts reform increase health care access and improve health, but it also reduced medical debt (Mazumder and Miller 2016).
The reform could have also impacted access to contraceptive care which may have affected rates of low birthweight and infant mortality by extending birth intervals. Evidence on the impact of the reform on contraceptive care is thin, but one focus group study suggested that the reform did improve access for low‐income women utilizing family planning clinics (Dennis et al. 2012). Another paper found that the reform reduced fertility among unmarried women, but not married women (Apostolava‐Mihaylova and Yelowitz 2017).
The effects of reform were broadly felt. Although relative measures of racial and socioeconomic disparities were not erased, the reform improved outcomes (in absolute terms) for racial minorities and socioeconomically disadvantaged populations (Zhu et al. 2010; Van Der Wees, Zaslavsky, and Ayanian 2013).
In this study, we examined whether the 2006 reform in Massachusetts was associated with changes in the incidence of low birthweight and rates of infant mortality. The Massachusetts reform is an important bellwether for the rest of the country because it occurred over 10 years ago and we can now examine its impact on longer run trends.
Methods
Data
Data on infant health outcomes came from two sources compiled by the National Center for Health Statistics (NCHS). To study infant mortality rates, we used the 2001–2012 period linked birth–death files (mortality data, hereafter). These data are compiled from death certificates for all infants in the United States that died prior to their first birthday. Records are matched to corresponding birth certificates to obtain information about circumstances at birth. The linked birth data include only deceased cases so we had to aggregate the data to obtain an appropriate denominator. We generated infant mortality counts and rates (deaths per 1,000 live births) at the county‐race‐year level. Our mortality data formed an unbalanced panel given that there were not live births in every county‐by‐race‐by‐year cell. Because our mortality analysis is conducted at an aggregated level, we cannot draw conclusions about the association of reform with individual mortality.
Our primary measure of health at birth was an indicator of low birthweight (<2,500 g) obtained from the 2001 to 2012 Natality Detailed Files (birth data, hereafter). We also examined four secondary outcomes from the birth data, including very low birthweight (<1,500 g), 5‐minute Apgar scores, prematurity (<37 weeks' gestation at the time of birth), and small‐for‐gestational age. While our main focus is on low birthweight and infant mortality rates, results concerning the secondary outcomes are discussed below and presented in the Appendix SA2. The birth data contain a (nearly) complete census of all births in the United States. We utilized a number of demographic characteristics associated with health insurance and birth outcomes, including mother's race, age, and marital status and the birth order and gender of the infant. We included only singleton births. The birth data are at the individual level, and because of the large number of observations even small, nonrelevant differences were often statistically significant at the p < .05 level.
We used restricted versions of both data that have state and county of residence indicators. Using the county indicators, we merged the data with county‐level poverty and unemployment to control for fluctuations in macro‐economic conditions, including effects of the Great Recession.
The birth and mortality data had two important limitations. The first is that birth certificates collect an important set of demographic covariates, but they lack other important predictors like income. The second limitation is that in 2003, a new birth certificate form was issued, but states were given the option about when to implement it. Massachusetts adopted the new birth certificate in 2011. Thus, we were confined to using only the subset of variables that were consistently measured in the old and revised form. Key variables that are not comparable over time are educational attainment, the timing of prenatal care initiation, physical activity, and smoking status. NCHS reports that while the old and revised certificates collected these variables, they did so in different ways which prevent comparability across state and year. Beginning in 2010, NCHS sets these variables to missing in states that use the old certificate, even in the restricted file. In some analyses, we used education, but we could only do so for the 2001–2009 data.
The final dataset we utilized was the 2002–2013 Annual Social and Economic Supplement to the Current Population Survey (CPS). We used the CPS to examine how unadjusted uninsured rates for women of child‐bearing age changed from pre‐ to postreform. More complete analyses of the reform's effect on coverage are provided elsewhere (e.g., Long et al. 2010; Sonier, Boudreaux, and Blewett 2013).
Analysis
Our approach followed previous evaluations of Massachusetts reform (Love and Seifert 2016). Using a difference‐in‐differences design, we compared pre–postchanges in Massachusetts to pre–postchanges in a set of comparison states. The comparison states included four other New England states that neighbored Massachusetts: Maine, New Hampshire, Vermont, and Rhode Island. We did not include Connecticut because it expanded Medicaid in the postperiod. In the Appendix SA2, we show the results of sensitivity tests in which we include both Connecticut and New York. Using indicator variables, we divided the study period into three policy periods: a preperiod (2002–2005), an implementation period (2006 and 2007) in which some but not all of the policy had been implemented, and a postperiod (2008–2012). These period indicators were set in reference to year of birth, and in a robustness test, we explored whether our results changed when setting the policy indicators in reference to approximate date of conception (estimated using gestational age at birth).
Our difference‐in‐differences approach controlled for any trends or contemporaneous shocks that were common to the treatment and control states. Controlling for these trends is clearly important, given a context of contemporaneous but unrelated improvements in infant health (Mathews, MacDorman, and Thoma 2015). The assumption of our design is that changes in the comparison states represented the changes that would have occurred in Massachusetts had the reform not taken place. To assess the appropriateness of this assumption, we graphically and statistically inspected the data for differential temporal trends during the preperiod. We also examined whether our results changed using alternative comparison states.
We implemented the difference‐in‐differences analysis using multivariable regressions. In the mortality analysis, we controlled for race (non‐Hispanic white, non‐Hispanic black, all other race/ethnic groups), county‐by‐year unemployment and poverty. In the birth data, we had access to more covariates. We controlled for maternal age in years (<21, 21–34, ≥35), race (white, non‐hispanic; black, non‐hispanic; other, non‐Hispanic; Hispanic), infant's gender, birth order, and county‐by‐birth year poverty and unemployment. All models included birth year fixed effects to control for cohort‐specific patterns and state fixed effects to control for unique state attributes.
We modeled mortality (a count variable) using negative binomial regression where the number of births per cell was used as the exposure variable. We transformed the coefficients so that they represent incidence rate ratios. Low birthweight (a 0/1 indicator) was modeled using linear probability models at the individual level as is common in state health policy research, and in Appendix SA2 we show that the linear probability results are similar to the average marginal effects from logistic regression. In both models, we clustered standard errors on state. While we were concerned that our inference strategy might tend to over‐reject the null given a small number of clusters, we show in Appendix SA2 that key results are robust to using a studentized wild‐cluster bootstrap (McKinnon 2014).
Subgroup Analyses
Consistent with previous research on the Massachusetts reform, our main analysis considered all women, not just women who were uninsured prior to reform (cf. Long et al. 2010). However, some women were more likely than others to be affected by the policy change (e.g., the uninsured or underinsured), so we examined the association of reform on infant mortality rates and low birthweight overall and for a set of predefined subgroups that were more likely to benefit. Unfortunately, insurance status was not consistently measured in either dataset and would otherwise be endogenous (e.g., a family might choose their insured status based on the infant's expected health). In the birth data, we examined associations by mother's age and race, marital status, and educational attainment (for 2001–2009 only). Minority and lower SES women had lower insured rates prior to reform and lower SES women experienced larger gains in coverage, access, and use of care as the result of reform (Long et al. 2010). Therefore, associations between reform and infant health may have varied across these strata. In the mortality analysis, we were limited by cell size and thus examined only the overall population and non‐Hispanic black and non‐Hispanic white deaths separately.
Results
In the analytic birth data, we observed a total of 1.5 million births over the 12‐year study period. Baseline (2001–2005) composition of Massachusetts and the comparison states are presented in Table 1. Massachusetts births were to older mothers, on average, compared to the comparison state births (p < .05). Massachusetts births were also less likely to be white, non‐Hispanic and less likely to be born into an unmarried parent household compared to their counterparts (p < .05). Massachusetts had lower poverty and unemployment (p < .05). The large sample sizes in the birth data mean that even clinically irrelevant differences in Table 1 are statistically significant. Nonetheless, the imbalance of covariates at baseline underscores the need for our quasi‐experimental approach and our use of state fixed effects, which controlled for both observed and unobserved time‐invariant differences between Massachusetts and the comparison states.
Table 1.
Baseline Characteristics, 2001–2005 Birth Data
| Comparison States | Massachusetts | |||
|---|---|---|---|---|
| % | SE | % | SE | |
| Male | 51.37 | 0.10 | 51.15 | 0.08 |
| Live birth order | ||||
| 1st | 43.52 | 0.10 | 44.79a | 0.08 |
| 2nd–3rd | 48.75 | 0.11 | 48.42a | 0.08 |
| 4th or later | 7.74 | 0.06 | 6.79a | 0.04 |
| Maternal age | ||||
| Less than 21 | 10.41 | 0.06 | 7.87a | 0.04 |
| 21–34 | 72.96 | 0.09 | 69.55a | 0.08 |
| 35+ | 16.63 | 0.08 | 22.58a | 0.07 |
| Maternal race/ethnicity | ||||
| White, non‐Hispanic | 82.19 | 0.08 | 71.37a | 0.07 |
| Black, non‐Hispanic | 3.09 | 0.04 | 8.41a | 0.05 |
| Other, non‐Hispanic | 8.07 | 0.06 | 7.68a | 0.04 |
| Hispanic | 6.66 | 0.05 | 12.54a | 0.05 |
| Maternal marital status | ||||
| Unmarried | 31.99 | 0.10 | 28.56a | 0.07 |
| County economic characteristics | ||||
| Poverty rate | 9.57 | 0.01 | 9.50a | 0.01 |
| Unemployment rate | 4.46 | 0.00 | 5.01a | 0.00 |
Indicates a significant difference from the comparison states, p < .05.
Source: 2001–2005 Natality Detail File and Area Health Care Resources File.
Panel A of Figure 1 displays uninsured rates from the CPS and demonstrates the relevance of the reform to health insurance coverage. The figure suggests that reform was associated with substantial declines in the uninsured rates for adult women of child‐bearing age (age 19–44). The uninsured rate fell from a peak of about 12 percent in the preperiod to a low of about 4 percent in the postperiod.
Figure 1.
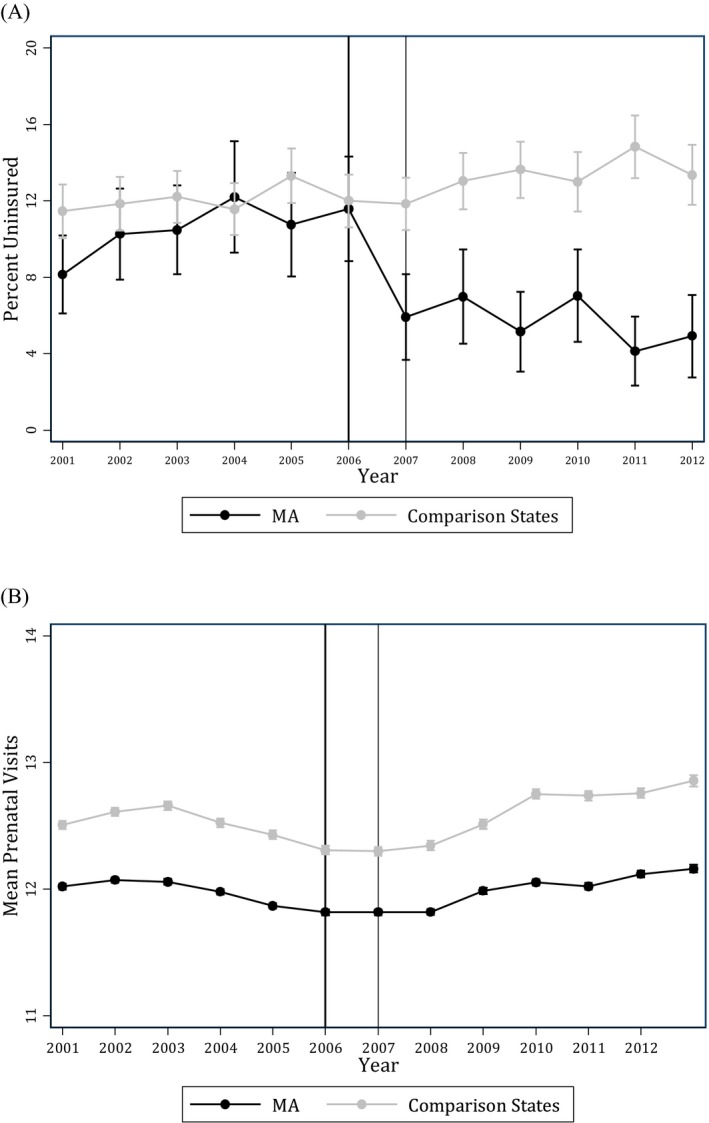
Health Insurance and Prenatal Visits in Massachusetts and Four Comparison States. (A) Uninsured Rates among Women Aged 19–44; (B) Average Number of Prenatal Visits Source: 2002–2013 Current Population Survey, Annual Social and Economic Supplement and 2001–2012 birth data. The vertical lines indicate the implementation period. Error bars are 95% confidence intervals.
Another useful source for gauging how many births were potentially impacted directly by the reform comes from the Massachusetts' Pregnancy Risk Factor Surveillance System (PRAMS; National Center for Chronic Disease Prevention and Health Promotion 2017). In 2007, the earliest year of available data, 16.2 percent of births (or about 12,630 births) occurred among women who were uninsured just prior to their pregnancies. An additional 15.9 percent of deliveries (about 12,396) occurred among mothers who received Medicaid financed prenatal care but were not covered by Medicaid just prior to pregnancy and thus may have entered prenatal care relatively late in pregnancy and/or had disruptions in care during the pre‐ or interconception periods. By 2011, the prepregnancy uninsured rate was a third the size of that in 2007 (5.4 percent or 4,210 births) and 8.7 percent of women receiving Medicaid prenatal care did not have Medicaid prior to pregnancy (6,365 births). Given that the earliest year of PRAMS data occurs during the implementation year of the reform, these estimates provide a rough lower‐bound sense of the number of deliveries that were likely to be directly affected.
Panel B of Figure 1 plots the average number of prenatal visits, obtained from the birth data. Prenatal care is one of several mechanisms described in the introduction that might connect health insurance to infant health. In the prereform period, Massachusetts women averaged about a half visit less than comparison state mothers. There was a slight decline in the number of visits in Massachusetts during the preperiod and then a slight increase in the postperiod. However, women in the comparison states also experienced an increase during the postperiod, suggesting that change in the number of prenatal visits in Massachusetts may not be attributable to the reforms. Unfortunately, the birth data available to us do not consistently track the timing and adequacy of prenatal care initiation over state and year—a more relevant metric for measuring appropriate prenatal care use.
Figure 2 plots the incidence of low birthweight and infant mortality rates in Massachusetts and the comparison states over time. For both outcomes the preperiod trends appeared similar in Massachusetts and the comparison states, a key assumption of the difference‐in‐differences design. Results from a more formal test of this assumption are reported in Appendix SA2. Using the preperiod birth data (years 2001–2005), we regressed the indicator of low birthweight on continuous year, indicator for Massachusetts, and the interaction of year and Massachusetts. The interaction term was near zero and nonsignificant (p = .165), suggesting similar linear time trends in the treatment and comparison states prior to the introduction of reforms. Returning to Figure 2, the incidence of low birthweight decreased in Massachusetts and the comparison states in the postperiod. Between 2007 and 2012, there was a steady decline in infant mortality in both Massachusetts and the comparison states.
Figure 2.
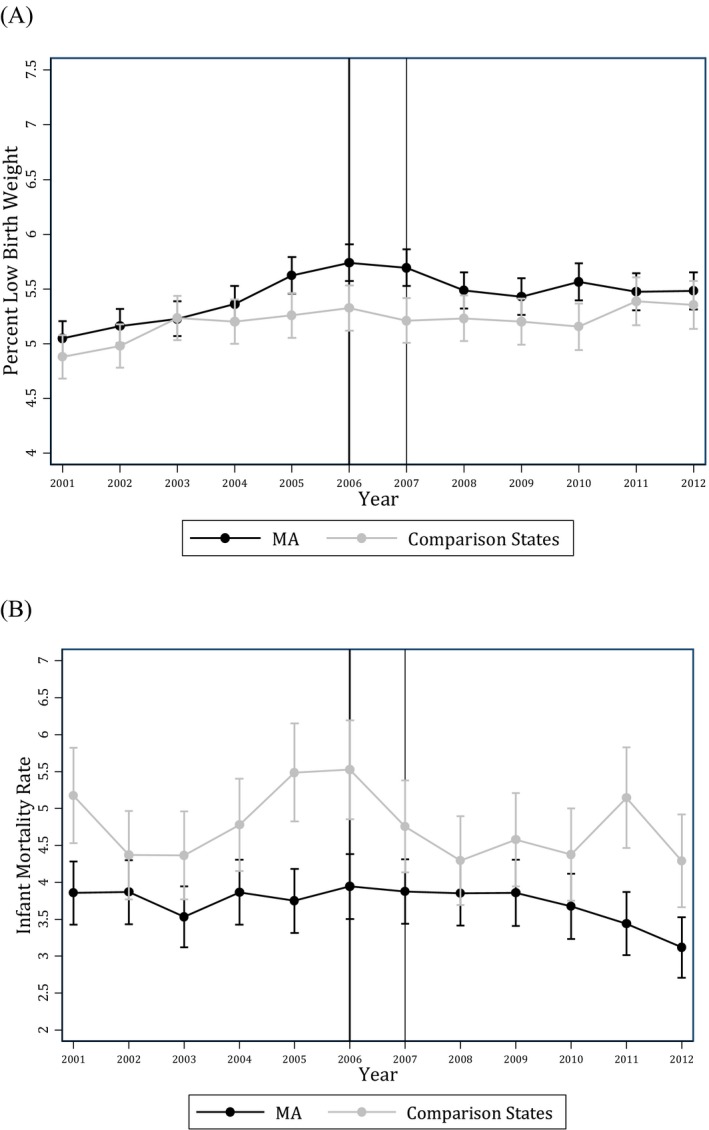
Low Birthweight and Infant Mortality in Massachusetts and Four Comparison States, Singleton Births. (A) Incidence of Low Birthweight (<2,500 g); (B) Infant Mortality per 1,000 Live Births Source: 2001–2012 birth and death files. The vertical lines indicate the implementation period. Error bars indicate 95% confidence intervals. Interval estimates for the IMRs are based only on the variance of the numerator. The denominator is assumed to be given.
Table 2 presents the regression adjusted difference‐in‐differences estimates from the low birthweight analysis, which was based on individual‐level data. Estimates are for the overall population and for subgroups of women described above. The coefficients have been scaled by 100 to represent percentage point change. We present only the coefficients of interest, but full model results are available in Appendix SA2. In the overall population, the reform was associated with a small, but statistically significant increase in low birthweight during the implementation period. The association was small (a 0.25 percentage point change) and it appeared to be driven by a larger decline in low birthweight in the comparison group than in Massachusetts (Figure 2). The association faded out in the postperiod. This pattern of results was generally consistent for each of the prespecified subgroups. While the point estimates for Non‐Hispanic African Americans, Hispanics, and unmarried mothers were negative, suggesting a reduction in low birthweight, the estimates were not statistically significant.
Table 2.
The Association of Massachusetts Health Reform with the Incidence of Low Birthweight (Percentage Point Change), Overall and by Subgroup
| Est. | SE | p‐Value | |
|---|---|---|---|
| Overall population | |||
| Treat × Implementation | 0.25 | 0.04 | .004 |
| Treat × Post | 0.10 | 0.14 | .527 |
| Baseline mean in MA | 5.28 | 0.04 | |
| Non‐Hispanic white mothers | |||
| Treat × Implementation | 0.32 | 0.09 | .020 |
| Treat × Post | 0.22 | 0.11 | .133 |
| Baseline mean in MA | 4.40 | 0.03 | |
| Non‐Hispanic African American mothers | |||
| Treat × Implementation | 0.07 | 0.25 | .801 |
| Treat × Post | −0.34 | 0.23 | .220 |
| Baseline mean in MA | 9.30 | 0.01 | |
| Hispanic mothers | |||
| Treat × Implementation | 0.32 | 0.28 | .324 |
| Treat × Post | −0.33 | 0.22 | .208 |
| Baseline mean in MA | 6.91 | 0.12 | |
| Unmarried mothers | |||
| Treat × Implementation | 0.13 | 0.08 | .166 |
| Treat × Post | −0.23 | 0.14 | .168 |
| Baseline mean in MA | 7.90 | 0.08 | |
| High school education or less (2001–2009) | |||
| Treat × Implementation | 0.10 | 0.05 | .102 |
| Treat × Post | 0.07 | 0.17 | .703 |
| Baseline mean in MA | 7.00 | 0.07 | |
All estimates are from separate regressions. Coefficients and standard errors have been scaled by 100 to represent percentage point change. Models adjust for mother's age, race, and marital status, birth order, county‐level poverty and unemployment, and state and year fixed effects. Source: 2001–2012 Birth Files and Area Health Resources Files.
Table 3 presents incident rate ratios (IRRs) based on aggregated counts of infant mortality, adjusting for race, county‐level poverty and unemployment, and state and year fixed effects. Overall and for each subgroup considered, the IRRs for each outcome after implementation of the Massachusetts reform were near unity and not statistically significant. The exception was for infants born to mothers of other races. During the implementation of reform, there was a statistically significant decline in mortality rates, but the postperiod was associated with a nonsignificant increase, relative to the preperiod.
Table 3.
The Association of Massachusetts Health Reform with Aggregated Counts of Infant Mortality, Overall and by Subgroup
| IRR | SE | p‐Value | |
|---|---|---|---|
| Overall population | |||
| Treat × Implementation | 0.981 | 0.051 | .714 |
| Treat × Post | 1.049 | 0.089 | .572 |
| Baseline rate in MA (per 1,000 live births) | 3.73 | 0.25 | |
| Non‐Hispanic white mothers | |||
| Treat × Implementation | 1.044 | 0.065 | .494 |
| Treat × Post | 1.019 | 0.052 | .716 |
| Baseline mean in MA (per 1,000 live births) | 2.89 | 0.11 | |
| Non‐Hispanic African American mothers | |||
| Treat × Implementation | 1.039 | 0.167 | .811 |
| Treat × Post | 0.925 | 0.268 | .788 |
| Baseline mean in MA (per 1,000 live births) | 8.13 | 0.48 | |
| All other mothers | |||
| Treat × Implementation | 0.810 | 0.021 | .000 |
| Treat × Post | 1.653 | 0.488 | .089 |
| Baseline mean in MA (per 1,000 live births) | 4.90 | 0.265 | |
All estimates are from separate regressions. IRR represents incident rate ratios and SE are Hubert–White standard errors, clustered on state. Models control for race, county‐by‐year poverty, and unemployment and state and year fixed effects. See Appendix SA2 for complete regression results. For the overall analysis, n = 2,035. Source: 2001–2012 Mortality Files and Area Health Resources Files.
Sensitivity Analyses
In Appendix SA2, we present the results of several robustness tests. For example, we came to similar conclusions when we included Connecticut and New York and when we dropped Maine and Vermont (which implemented small insurance reforms in 2006). We also came to similar conclusions when defining the policy period indicators in reference to approximate date of conception rather than date of birth. We came to similar inferences when estimating average marginal effects from logistic regression and when estimating confidence intervals using a studentized wild‐cluster bootstrap. The reform had similar associations with other infant health outcomes that were measured in a consistent fashion across state and year. These secondary outcomes included very low birthweight, small‐for‐gestational age, premature birth, and 5‐minute Apgar scores. Finally, the mortality analysis was not affected by restricting the data to a balanced panel in which the same set of county‐by‐race cells are observed in every year.
Discussion
This study contributes new data about the association of health insurance expansions and infant health outcomes. Specifically, we examined if the 2006 Massachusetts reform was associated with changes in infant mortality rates or an infant's risk of low birthweight. We did not find compelling evidence that health reform in Massachusetts had an association with either of these indicators of infant health. Our 95% confidence intervals for a postperiod effect on low birthweight imply that we can exclude estimates larger than 0.3 percentage point decline for the full population and a 0.99 percentage point decline for non‐Hispanic African American infants (see Appendix SA2).
Our results differed in some respects from previous work on the Massachusetts reform. Despite a robust health system and high levels of insurance coverage prior to 2006, a large body of evidence suggests that the reform was associated with increased health care utilization, improved adult and child health, decreased adult mortality rates, and reduced measures of financial burden (see review in Love and Seifert 2016). Increased health care use, reduction in financial strain, and improvement in the general health of women of child‐bearing age may have important implications for infant health. However, in this study, we found no evidence that health reform in Massachusetts had an association with infant health, as measured by low birthweight and infant mortality rates. This finding was consistent across different subgroups that varied in their risk for poor outcomes and the likelihood that reform was a salient policy change given prereform levels of insurance coverage. However, it is important to recognize that our analysis measured the association of outcomes with the reform, not with insurance coverage per se. Our results were robust to different control groups and alternative modeling assumptions.
Our results are consistent with previous studies of Medicaid expansions that have found small to null associations with birthweight. Our mortality results are less consistent with previous research which has tended to find moderate‐to‐larger effects (Currie and Gruber 1996; Goodman‐Bacon 2016). Our mortality results also depart from some international universal coverage expansions. For example, Canada's universal coverage expansion was associated with reduced infant mortality rates (Hanratty 1996).
Our failure to find an association between health reform and infant health in Massachusetts could be attributed to several factors. One likely reason is that the safety net in Massachusetts could have already been delivering high‐quality and timely care to uninsured expectant mothers such that the dose of reform was not large enough to show up in the measures we examined. For example, since 1991, the state has supported a relatively extensive system of family planning clinics that deliver contraceptive care and other women's health services with sliding scale fees. In 2003, the state mandated that all FDA‐approved contraceptives be covered equally (Dennis et al. 2012, 2013).
Insurance reforms adopted as part of the ACA may have substantially different effects in states that did not share the baseline environments in Massachusetts. Unfortunately, our data did not allow us to examine whether the Massachusetts reform was associated with the proximate mechanisms that we postulated could link reform to infant outcomes: more timely care for women before and during pregnancy, improved financial resources, and improved hospital care for infants. This limitation dampens our ability to generalize our findings to other settings.
The findings of this study should be interpreted in light of the following limitations. First, like other studies of Medicaid's effect on mortality (Currie and Gruber 1996; Sommers, Long, and Baiker 2014; Goodman‐Bacon 2016), our study of infant mortality rates was ecological. Therefore, we cannot be certain that an individual‐level intervention of insurance coverage to uninsured pregnant women would not result in a change in the mortality of their infants. Second, this study relied on the assumption that the change in the control states was an accurate reflection of the change that would have occurred in Massachusetts had the reform not been implemented. There is no definitive test for the appropriateness of our comparison groups, but we found similar pretreatment trends and our results were consistent when using alternative comparison state groups. However, it is possible that some other change, such as a reduction in early elective delivery among comparison state hospitals that was correlated with the timing of reform but not a result of it, biased our results toward zero. Another limitation centers on our measurement of infant health. We focused on birthweight which is a limited proxy of infant health and infant mortality which is an extreme health state. It is possible that reform was associated with infant health outcomes that were not captured in our outcomes. A final limitation was that we clustered our standard errors on state to handle autocorrelation, yet clustered standard errors are known to be biased when the cluster size is small (Cameron and Miller 2015). However, the direction of the bias is typically to understate standard errors and over‐reject the null hypothesis. Given our null findings, our underestimation of standard errors is likely not an important concern and a more robust method did not change our conclusions (see Appendix SA2).
The Massachusetts reform foreshadowed many components of the ACA. Existing evidence on the ACA suggests that it is associated with a large change in health insurance coverage and use of medical care (French et al. 2016; Obama 2016). The results from our study do not preclude potential associations of the ACA with infant health. Not only is the ACA having a large effect on coverage, but it also includes specific maternal and infant health demonstrations that might have impacts that are independent of coverage gains (Center for Medicare and Medicaid Innovation 2015; Simmons et al. 2016). Improving infant health, especially for disadvantaged populations, remains an important public policy goal, and continued work is needed to identify evidence based and cost‐effective strategies. As previous work has suggested, effective strategies likely must include both health system and socially focused interventions (Lu and Halfon, 2003).
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Supplementary Appendix.
Acknowledgments
Joint Acknowledgement/Disclosure Statement: This project was supported in part by the AcademyHealth New Investigator Small Grant Program, the March of Dimes, and the Health Resources and Services Administration (R40MC28310). All errors and opinions are those of the authors and do not reflect the views of our funders. We thank the editors, two anonymous reviewers, and seminar participants at the University of Miami and the Agency for Health Care Research and Quality for helpful comments on a previous draft of this paper.
Disclosure: None.
Disclaimer: None.
References
- Agency for Health Care Research and Quality . 2016. “State Snapshots” [accessed on May 1, 2017]. Available at http://www.ahrq.gov/research/data/state-snapshots/index.html
- Apostolava‐Mihaylova, M. , and Yelowitz A.. 2017. “Health Insurance, Fertility, and the Wantedness of Pregnancies: Evidence from Massachusetts.” Contemporary Economic Policy. Available online ahead of print.
- Badura, M. , Johnson K., Hench K., and Reyes M.. 2008. “Healthy Start: Lessons Learned on Interconception Care.” Women's Health Issues 18 (6): S61–6. [DOI] [PubMed] [Google Scholar]
- Caceres, I. , Orejuela‐Hood M., and West J.. 2016. “Racial and Ethnic Health Disparities by EOHHS Regions in Massachusetts” Massachusetts Department of Health 2007 [accessed on March 1, 2016]. Available at http://www.mass.gov/eohhs/docs/dph/research-epi/disparity-report.pdf
- Cameron, C. , and Miller D.. 2015. “A Practitioner's Guide to Cluster‐Robust Inference.” Journal of Human Resources 50 (2): 317–73. [Google Scholar]
- Center for Medicare and Medicaid Innovation . 2015. “Strong Start for Mothers and Newborns Evaluation: Year 1 Annual Report” [accessed on September 20, 2016]. Available at https://innovation.cms.gov/Files/reports/strongstart-enhancedprenatal-yr1evalrpt.pdf
- Centers for Disease Control and Prevention . 2014. “VitalStats” National Center for Health Statistics [accessed on December 1, 2014]. Available at http://www.cdc.gov/nchs/VitalStats.htm
- Courtemanche, C. , and Zapata D.. 2013. “Does Universal Health Insurance Coverage Improve Health? The Massachusetts Experience.” Journal of Policy Analysis and Management 33 (1): 36–49. [DOI] [PubMed] [Google Scholar]
- Currie, J. , and Grogger J.. 2002. “Medicaid Expansions and Welfare Contractions: Offsetting Effects on Prenatal Care and Infant Health?” Journal of Health Economics 21 (2): 313–35. [DOI] [PubMed] [Google Scholar]
- Currie, J. , and Gruber J.. 1996. “Saving Babies: The Efficacy and Cost of Recent Changes in the Medicaid Eligibility of Pregnant Women.” Journal of Political Economy 104: 1263–96. [Google Scholar]
- Currie, J. , and Gruber J.. 1997. The Technology of Birth: Health Insurance, Medical Interventions, and Infant Health. National Bureau of Economic Research Work Paper, No. 5985.
- Currie, J. , and Rossin‐Slater M.. 2014. “Early‐Life Origins of Life‐Cycle Well‐Being: Research and Policy Applications.” Journal of Policy Analysis and Management 34 (1): 208–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denis, A. , Clark J., Cordova D., McIntosh J., Edlund K., Wahlin B., Tsikitas L., and Blanchard K.. 2012. “Access to Contraception after Health Reform in Massachusetts: A Mixed‐Methods Study Investigating Benefits and Barriers.” Contraception 85 (2): 166–72. [DOI] [PubMed] [Google Scholar]
- Dennis, A. , Blanchard K., Cordova D., Wahlin B., Clark J., Edlund K., McIntosh J., and Tsiktas L.. 2013. “What Happens to Women Who Fall through the Cracks of Health Reform? Lessons from Massachusetts.” Journal of Health Politics, Policy and Law 38 (2): 373–99. [DOI] [PubMed] [Google Scholar]
- Frean, M. , Gruber J., and Sommers B.. 2016. “Premium Subsidies, the Mandate, Medicaid Expansion: Coverage Effects of the Affordable Care Act.” Journal of Health Economics 53: 72–86. [DOI] [PubMed] [Google Scholar]
- French, M. , Homer J., Gumus G., and Hickling L.. 2016. “Key Provisions of the Patient Protection and Affordable Care Act: A Systematic Review and Presentation of Early Research Findings.” Health Services Research 51(5): 1735–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman‐Bacon, A. 2016. “Public Insurance and Mortality: Evidence from Medicaid Implementation.” Journal of Political Economy. [Google Scholar]
- Hanratty, M. 1996. “Canadian National Health Insurance and Infant Health.” American Economic Review 86 (1): 276–84. [Google Scholar]
- Howell, E. 2001. “The Impact of Medicaid Expansions for Pregnant Women: A Synthesis of the Evidence.” Medical Care Research and Review 58 (1): 3–30. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . 1985. Preventing Low Birthweight. Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- Kolstad, J. , and Kowalski A.. 2012. “The Impact of Health Care Reform on Hospital and Preventive Care: Evidence from Massachusetts.” Journal of Public Economics 96: 909–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long, S. , Stockley K., Birchfield L., and Shulman S.. 2010. The Impacts of Health Reform: On Insurance Coverage and Health Care Access, Use, and Affordability for Women in Massachusetts. Washington, DC: The Urban Institute. [Google Scholar]
- Love, K. , and Seifert R.. 2016. “10 Years of Impact: A Literature Review of Chapter 58 of the Acts of 2006. Blue Cross Blue Shield Foundation of Massachusetts” [accessed on September 20, 2016]. Available at http://bluecrossfoundation.org/sites/default/files/download/publication/Impact_of_Ch58_final.pdf
- Lu, M. , and Halfon N.. 2003. “Racial and Ethnic Disparities in Birth Outcomes: A Life‐Course Perspective.” Maternal and Child Health Journal 7 (1): 13–30. [DOI] [PubMed] [Google Scholar]
- MacDorman, M. , Mathews T., Mohangoo A., and Zeitilin J.. 2014. “International Comparisons of Infant Health and Related Factors: United States and Europe, 2010.” National Vital Statistics Reports 63 (5): 1–7. [PubMed] [Google Scholar]
- Mathews, T. , MacDorman M., and Thoma M.. 2015. “Infant Mortality Statistics From the 2013 Period Linked Birth/Infant Death Data Set.” National Vital Statistics Reports 64 (9): 1–30. [PubMed] [Google Scholar]
- Mazumder, B. , and Miller S.. 2016. “The Effects of the Massachusetts Health Reform on Household Financial Distress.” American Economic Journal: Economic Policy 8 (3): 284–313. [Google Scholar]
- McKinnon, J. 2014. Wild Cluster Bootstrap Confidence Intervals. Queen's Economics Department Working Paper No. 1329. Kingston, Ontario: Queen's University. [Google Scholar]
- National Center for Chronic Disease Prevention and Health Promotion . 2017. “PRAMStat” Available at https://www.cdc.gov/prams/pramstat/index.html
- Obama, B. 2016. “United States Health Care Reform: Progress to Date and Next Steps.” Journal of the American Medical Association 316 (5): 525–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phibbs, C. , Baker L., Caughey A., Danielsen B., Schmitt S., and Phibbs R.. 2007. “Level and Volume of Neonatal Intensive Care and Mortality in Very‐Low‐Birth‐Weight Infants.” New England Journal of Medicine 356: 2165–75. [DOI] [PubMed] [Google Scholar]
- Rosenberg, D. , Handler A., Rankin K., Zimbeck M., and Adams K.. 2007. “Prenatal Care Initiation among Very Low‐Income Women in the Aftermath of Welfare Reform: Does Pre‐Pregnancy Medicaid Coverage Make a Difference?” Maternal and Child Health Journal 11 (1): 11–7. [DOI] [PubMed] [Google Scholar]
- Simmons, A. , Finegold J., Yarboff K., Gee R., and Chappel E.. 2016. “The Affordable Care Act: Promoting Better Health for Women.” ASPE Issue Brief [accessed on September 20, 2016]. Available at https://aspe.hhs.gov/sites/default/files/pdf/205066/ACAWomenHealthIssueBrief.pdf
- Simon, K. , and Handler A.. 2008. “Welfare Reform and Insurance Coverage during the Pregnancy Period: Implications for Preconception and Interconception Care.” Women's Health Issues 18 (6): S97–106. [DOI] [PubMed] [Google Scholar]
- Sommers, B. , Long S., and Baiker K.. 2014. “Changes in Mortality after Massachusetts Health Care Reform: A Quasi‐Experimental Study.” Annals of Internal Medicine 160 (9): 585–94. [DOI] [PubMed] [Google Scholar]
- Sonier, J. , Boudreaux M., and Blewett L.. 2013. “Medicaid ‘Welcome‐Mat’ Effect of Affordable Care Act Implementation Could Be Substantial.” Health Affairs 32 (7): 1319–25. [DOI] [PubMed] [Google Scholar]
- Van Der Wees, P. , Zaslavsky A., and Ayanian J.. 2013. “Improvements in Health Status after Massachusetts Health Care Reform.” Milbank Quarterly 91 (4): 663–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu, J. , Brawarsky P., Lipsitz S., Huskamp H., and Has J.. 2010. “Massachusetts Health Reform and Disparities in Coverage, Access and Health Status.” Journal of General Internal Medicine 25 (12): 1356–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Supplementary Appendix.


