Abstract
Objective
To examine the extent to which physician‐to‐system ownership transitions are associated with declines in practice‐reported patient responsiveness (PRPR).
Data Sources
A longitudinal cohort of practices (n = 897) from the National Survey of Large Physician Organizations/National Survey of Small‐ and Medium‐Sized Physician Organizations (2006/08) and the National Survey of All‐Size Physician Organizations (2012/13).
Study Design
Multivariable regression estimated the effect of ownership on changes in PRPR, controlling for practice size, specialty composition, other practice, and market characteristics.
Data Collection/Extraction Methods
Data were collected from three nationally representative surveys of physician organizations consisting of 40‐minute interviews with the medical director, president, or chief executive officer.
Principal Findings
Nine percent of organizations transitioned to system ownership. Compared to practices that were continuously physician‐owned, practices that switched to system ownership did not have significantly lower PRPR at baseline but continuously system‐owned practices did. Transitions to system ownership were associated with increased PRPR compared to continuously physician ownership. Increased practice size and changes in specialty composition, however, were associated with diminished PRPR.
Conclusions
Practices can maintain or improve strategies to address patient concerns when transferring ownership to systems with careful attention to the impact of increased size and changes in specialty composition.
Keywords: Health care systems, ownership, patient complaints, patient responsiveness, independent physicians
Medical practices in the United States are increasingly falling into one of two divergent types: small, single specialty practices owned by physicians and large, multispecialty practices owned by systems (Burns, Goldsmith, and Sen 2013). The trend toward increased system ownership (Liebhaber and Grossman 2007; Kocher and Sahni 2011) has many potential benefits. System ownership may improve a practice's bargaining power with payers, resulting in potentially greater resources for administrative structures and support. System ownership can also improve quality of care by providing a coordination framework and improve efficiency by reducing transaction costs (Mick and Shay 2016). Furthermore, given the implementation of the Medicare Access and Children's Health Insurance Program Reauthorization Act of 2015 (MACRA), physicians will be looking to systems for the infrastructure resources needed to succeed under the new value‐based payment incentives. There is concern, however, that as physician‐owned practices are acquired by hospitals and health care systems, patient‐centeredness will diminish, as system‐driven improvement initiatives will emphasize acute inpatient care at the expense of patient‐centered ambulatory care (Halley 2014). For example, system ownership has been found to be associated with decreases in physician engagement, which can compromise the quality of care (Keckley, Coughlin, and Stanley 2013). However, health care systems are met with many more compliance demands from accrediting bodies, such as the Joint Commission, and payers of health care, such as the Center for Medicare and Medicaid Services. These demands include the establishment of a formal system for receiving, documenting, and responding to patient complaints (Joint Commission on Accreditation of Healthcare Organizations 2000; Centers for Medicare & Medicaid Services 2004). This might carry over to hospital‐owned ambulatory primary care practices being more responsive to patients than physician‐owned practices.
To date, studies of the effect of system ownership on organizational performance have yielded mixed results. In a cross‐sectional study of California physician practices, system ownership was found to be associated with higher adjusted costs per patient compared to physician ownership (Robinson and Miller 2014). In another cross‐sectional study of a national sample of small‐ and medium‐sized practices (19 physicians or less), system‐owned practices had broader use of patient‐centered medical home (PCMH) processes, for example, electronic medical records, quality improvement initiatives, and nurse care managers (Rittenhouse et al. 2011). In a longitudinal study of a national sample of physician practices of all sizes, Bishop et al. (2016) found that practices which switched to hospital ownership had more chronic care management processes (CMPs), which are core PCMH processes and important to support the delivery of patient‐centered care (Wiley et al. 2015). However, Scott et al. (2016) found no evidence of improved patient care in four quality metrics when hospitals switched to an employment model with their physicians in a national, longitudinal study of acute care hospitals. We seek to expand on this literature by investigating the impact of ownership on practice strategies to respond to patient concerns and feedback because an organization's orientation to patients, particularly the extent to which patients’ needs are proactively assessed, may be more likely to be impacted by ownership changes compared to other PCMH processes or utilization.
Examining the impact of practice ownership is challenging because transitions to system ownership also involve increases in practice size and changes in specialty mix, which may have independent impacts on practice strategies and organizational performance. Previous studies have not distinguished between the relative impacts of changes in practice ownership and associated changes, including increased practice size and specialty composition, on the quality and efficiency of health care. Increased practice size can improve operational efficiency by allowing physicians to pool resources, negotiate with payers, and distribute risk from variations in volume and complexity in the patient population (Shortell et al. 2005; Besanko et al. 2009). However, the benefits of increasing size are limited, as communication and coordination have been found to suffer from increasing size (Wheelan 2009). Changes in specialty composition may also affect the quality of care as multispecialty groups are challenged to coordinate care for complex cases. While there is the potential for improved care coordination in health care systems (Rittenhouse et al. 2004; Mehrotra, Epstein, and Rosenthal 2006; Rodriguez et al. 2009), prior studies have found mixed evidence of decreased costs among multispecialty groups compared to single specialty groups (Pauly 1996). As multispecialty groups have been found to be structurally complex (Kralewski, Pitt, and Shatin 1985), care coordination and practice responsiveness may also decrease with increased diversification of services.
To advance evidence on the impact of physician practice transitions to system ownership, we use a national cohort of physician organizations to disentangle the relative association of practice ownership, size, and specialty composition on the extent to which practices report the use of strategies for responding to patient concerns, feedback, and developing new services.
Methods
Data
Three nationally representative surveys of physician organizations were linked: the National Study of Small‐ and Medium‐sized Physician Practices (NSSMPP) and waves 2 and 3 of the National Survey of Physician Organizations (NSPO2 and NSPO3). These surveys focus on medical practices that provide care for patients with at least one of four chronic conditions: asthma, congestive heart failure, depression, and diabetes. These surveys consisted of 40‐minute interviews with the person most knowledgeable about the processes of the practice, usually the medical director, president, or chief executive officer. NSSMPP focused on practices with 19 or fewer physicians, while NSPO2 focused on large practices with 20 or more physicians. These two surveys were conducted in 2006 (NPSO2) and 2008 (NSMPP) and served as the baseline for our study. NSPO3 sampled practices of all sizes nationally, in 2012 and 2013, and serves as the follow‐up period for the study. These surveys have been previously described elsewhere (Shortell et al. 2009, 2014; Rodriguez et al. 2016).
Analytic Sample
There were 557 practices that responded to the NSPO2 survey (60.3 percent response rate), 1,931 practices that responded to the NSSMPP survey (63.2 percent response rate), and 1,398 practices that responded to the NSPO3 survey (49.1 percent response rate). We were interested in analyzing a cohort of practices longitudinally, so we focused on 1,048 practices that had both baseline and follow‐up survey responses. We were interested in physician ownership compared to systems ownership, so we excluded 104 practices that were owned by community health centers at either or both time points. Finally, we excluded 47 practices that were missing key variables for this study. The final analytic sample includes 897 physician organizations.
Measures
System ownership is defined as ownership by a hospital, hospital system, health care system, health management organization, or insurance entity. Because we are interested in the impact of change in ownership over time, we distinguish between practices that were continuously physician‐owned (n = 703), continuously system‐owned (n = 86), physician then system‐owned (n = 83), and system then physician‐owned (n = 25). We were also interested in the impact of practice size, which was categorized as small (1–2 physicians), medium (3–19 physicians), and large (20 or more physicians). A change in practice size was accordingly defined as an increase or decrease in a number of physicians that resulted in a change in size categories. Specialty composition was categorized as 100 percent primary care practitioners (PCPs), 33 percent to 99 percent primary care practitioners, or less than 33 percent primary care practitioners. A change in specialty composition was likewise defined as an increase or decrease in the percentage of primary care practitioners that resulted in changes in specialty mix categories.
A composite measure of practice‐reported patient responsiveness (PRPR) was constructed using practice‐reported responses to five questions adapted from the Malcolm Baldrige National Quality Award criteria (α = 0.76)(Shortell et al. 2004). The questions assessed the extent to which (1) the practice does a good job assessing patient needs and expectations, (2) the staff promptly resolves patient complaints, (3) patient complaints are studied to identify patterns and prevent reoccurrence, (4) practice uses data from patients to improve care, and (5) practice uses data on patient expectation and satisfaction to develop new services. Answers to each of these statements ranged from strongly disagree (1) to strongly agree (5) for a final average score on PRPR that likewise ranged from lowest (1) to highest (5). The focus here is the practice's use of responsive strategies for addressing patient complaints and feedback as opposed to the patient‐centeredness of care, as reported by the patients.
We further included NSPO3 data on the percent revenue from Medicaid patients as a proxy for patient socioeconomic vulnerability, the care management process index as this can contribute to PRPR regardless of ownership, and the Herfindahl‐Hirschman Index as calculated from the American Hospital Association Annual Survey of Hospitals (“AHA Annual Survey|American Hospital Association's Annual Survey Database|AHA Data Online,” n.d.; Connor et al. 1997; Cuellar and Gertler 2003; Spang, Bazzoli, and Arnould 2001) to account for county‐level hospital competition for 2009, the closest available year of data to the physician practice survey date, to account for heterogeneity in market environments.
Statistical Analyses
First, for each of the model variables, ownership categories were compared to the reference category of continuously physician‐owned practices. We used Wilcoxon rank‐sum test for categorical variables and Fisher's exact test for continuous variables (Table 1).
Table 1.
Medical Practice Characteristics at Baseline (2006/08) and over Follow‐up (2006/08 to 2012/13), by Ownership Status
| Continuously Physician‐Owned (N = 703; 78%) | Physician‐ to System‐Owned (N = 83; 9%) | Continuously System‐Owned (N = 86; 10%) | System‐ to Physician‐Owned (N = 25; 3%) | ||||
|---|---|---|---|---|---|---|---|
| Baseline PRPR | 4.2 (3.8, 4.6) | 4.2 (3.6, 4.6) | 0.3 | 4.0 (3.6, 4.4) | 0.013 | 4.2 (3.4, 4.2) | 0.048 |
| Change in PRPR | 0.0 (−0.6, 0.4) | −0.2 (−0.6, 0.2) | 0.3 | 0.0 (−0.6, 0.4) | 0.6 | 0.0 (−0.2, 0.8) | 0.043 |
| Baseline size | <0.0001 | <0.0001 | 0.016 | ||||
| 1–2 MDs | 382 (54%) | 19 (23%) | 23 (27%) | 11 (44%) | |||
| 3–19 MDs | 274 (39%) | 50 (60%) | 44 (51%) | 8 (32%) | |||
| 20+ MDs | 47 (6.7%) | 14 (17%) | 19 (22%) | 6 (24%) | |||
| Change in size | <0.0001 | <0.0001 | 0.12 | ||||
| Decrease | 41 (5.8%) | 4 (4.8%) | 3 (3.5%) | 2 (8.0%) | |||
| Increase | 47 (6.7%) | 20 (24%) | 19 (22%) | 4 (16%) | |||
| No change | 615 (87%) | 59 (71%) | 64 (74%) | 19 (76%) | |||
| Baseline composition | 0.10 | <0.0001 | 0.001 | ||||
| 100% PCP | 478 (68%) | 47 (57%) | 64 (74%) | 17 (68%) | |||
| 33–99% PCP | 78 (11%) | 12 (14%) | 18 (21%) | 8 (32%) | |||
| <33% PCP | 147 (21%) | 24 (29%) | 4 (4.7%) | 0 (0%) | |||
| Change in composition | 0.038 | <0.0001 | 0.021 | ||||
| Decrease PCP | 62 (8.8%) | 15 (18%) | 25 (29%) | 5 (20%) | |||
| Increase PCP | 14 (2.0%) | 1 (1.2%) | 1 (1.2%) | 2 (8.0%) | |||
| No change | 627 (89%) | 67 (81%) | 60 (70%) | 18 (72%) | |||
| Baseline Medicaid revenue (%) | 5.0 (1.0, 10.0) | 5.0 (0.0, 10.0) | 0.9 | 10.0 (5.0, 18.0) | <0.0001 | 7.0 (0.7, 15.0) | 0.082 |
| Change in Medicaid revenue | 0.0 (−2.0, 3.0) | 1.0 (−1.0, 5.0) | 0.023 | 0.5 (−3.0, 5.0) | 0.057 | 0.0 (−5.0, 4.3) | 0.7 |
| Baseline CMP index (%) | 15.0 (5.0, 30.0) | 15.0 (0.0, 35.0) | 0.7 | 20.0 (5.0, 40.0) | 0.026 | 20.0 (5.0, 65.0) | 0.10 |
| Change in CMP index | 0.0 (−10.0, 20.0) | 5.0 (−10.0, 25.0) | 0.2 | 7.5 (−5.0, 25.0) | 0.11 | 10.0 (0.0, 25.0) | 0.079 |
| Baseline HHI | 3298 (2049, 5056) | 2382 (1960, 4556) | 0.079 | 4199 (2554, 7473) | 0.002 | 3425 (2353, 6241) | 0.7 |
Data are presented as medians (interquartile range) or frequency (percentages) using Fisher's exact test or Wilcoxon rank‐sum test, respectively.
Then, to examine the association between ownership changes and changes in PRPR, multivariable linear regression models were estimated, controlling for practice size, specialty composition, proportion of Medicaid revenue, care management processes (CMP) index, PRPR at baseline, and market competition, near baseline in 2009. Because ownership change may be accompanied by changes in these control variables, analyses also controlled for change in practice size, change in the proportion of PCP, change in proportion of Medicaid revenue, and change in the CMP index.
We also examined the impact of ownership status on the change in use of each of the five individual PRPR items in regression analyses. Because the change in the use of individual components is dichotomous, we classified these changes as improvements (positive change) or not (negative change or no change) and multivariable logistic regression models were estimated using the same control variables as our main model.
We anticipated that some control variables might be highly correlated, so the variance inflation factor (VIF) was calculated for each control variable to assess the extent to which the multivariable models were overfit using a criterion of VIF ≤ 2.0.
Sensitivity Analyses
Change over time analyses with two points in time can be susceptible to floor or ceiling effects (Nunnally and Bernstein 1978). As a result, we repeated the analysis excluding practices with baseline PRPR scores at the minimum of 1 or the maximum of 5. We adjust for the baseline CMP index and in change over time in the CMP index to account for a potentially confounding effect on estimating the association between ownership change and PRPR. However, the ownership effect of interest may be attenuated with these controls because the use of care management processes may provide a foundation for practices to implement strategies to improve patient responsiveness because patients with chronic conditions can provide helpful information for improving practice responsiveness to patients. As an additional sensitivity analysis, we removed the CMP control variable from our models to assess whether the effect size for ownership status changed substantially.
Results
Descriptive Statistics
Practice characteristics are shown in Table 1. Compared to practices that were physician‐owned at both baseline and follow‐up, practices that transitioned from physician ownership to system ownership were more likely to increase in size (6.7 percent vs. 24 percent, p < .0001) and more often decreased in their proportion of PCPs (8.8 percent vs. 18 percent, p = .038). However, compared to practices that were continuously physician‐owned, practices that switched from physician‐owned to system‐owned did not have significantly different PRPR at baseline (median = 4.2, interquartile range (IQR) = 3.8, 4.6 vs. median = 4.2, IQR = 3.6, 4.6, p = .3), and continuously system‐owned practices had significantly lower PRPR at baseline (median = 4.2, IQR = 3.8, 4.6, vs. median = 4.0, IQR = 3.6, 4.4, p = .013).
Adjusted Analyses
Results of the multivariable linear regression are shown in Table 2, where a positive coefficient indicates an increase in PRPR and a negative coefficient indicates a decrease in PRPR. In adjusted analyses (Figure 1), a transition from physician ownership to system ownership was associated with increased PRPR (β = 0.31, 95 percent CI = 0.05, 0.57, p = .018). Decreases in the proportion of PCPs and increases in practice size were associated with declines in PRPR (β = −0.25, 95 percent = CI −0.36, −0.14, p < .0001; β = −0.38, 95 percent CI = −0.51, −0.25, p < .0001, respectively).
Table 2.
The Association of Ownership Change on PRPR
| Variable | Coefficient | 95% CI | p‐Value |
|---|---|---|---|
| Ownership | |||
| Continuously physician‐owned | Ref | Ref | Ref |
| Continuously system‐owned | 0.10 | −0.19, 0.38 | .5 |
| Physician‐owned | 0.31 | 0.05, 0.57 | .018 |
| Changed to system‐owned | |||
| System‐owned | 0.05 | −0.15, 0.24 | .6 |
| Changed to physician‐owned | |||
| Baseline practice size | |||
| 1–2 MDs | Ref | Ref | Ref |
| 3–19 MDs | −0.17 | −0.22, −0.12 | <.0001 |
| 20+ MDs | −0.43 | −0.69, −0.17 | .002 |
| Change in practice size | |||
| No Change | Ref | Ref | Ref |
| Decrease | −0.19 | −0.49, 0.11 | .2 |
| Increase | −0.38 | −0.51, −0.25 | <.0001 |
| Baseline composition | |||
| 100% PCP | Ref | Ref | Ref |
| 33–99% PCP | −0.04 | −0.18, 0.10 | .6 |
| <33% PCP | 0.11 | 0.06, 0.15 | <.0001 |
| Change in composition | |||
| No change | Ref | Ref | Ref |
| Decrease PCP | −0.25 | −0.36, −0.14 | <.0001 |
| Increase PCP | −0.20 | −0.73, 0.33 | .4 |
| Baseline Medicaid revenue per 5% | 0.02 | −0.00, 0.05 | .10 |
| Change in Medicaid revenue per 5% | −0.01 | −0.02, 0.00 | .10 |
| Baseline CMP index per 5% | 0.07 | 0.06, 0.08 | <.0001 |
| Change in CMP index per 5% | 0.05 | 0.05, 0.06 | <.0001 |
| Baseline HHI per 100 | −0.00 | −0.01, 0.00 | .059 |
| Baseline PRPR | −0.83 | −0.86, −0.80 | <.0001 |
Change in practice‐reported patient responsiveness (PRPR) ranges from −4 to 4.
Figure 1.
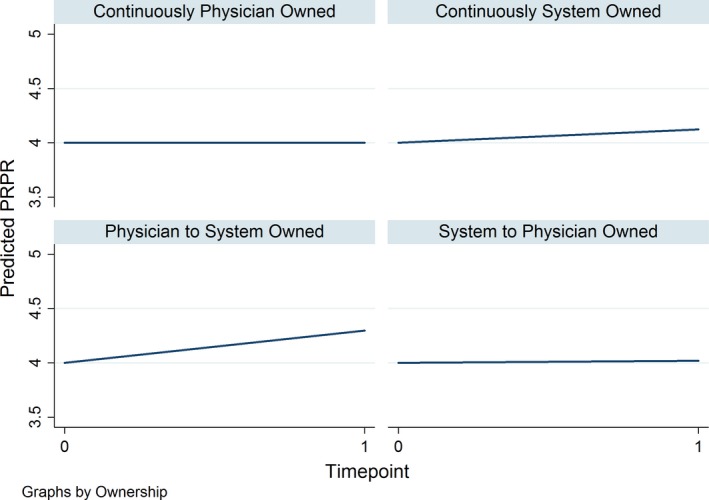
- Note. Data are as predicted from the main regression model shown in Table 2 for a practice with baseline PRPR of 4 on a range of 1–5, a constant practice size between 3 and 19 MDs and a constant specialty composition of 33 percent to 99 percent PCP.
When we examined each of the PRPR components individually using multivariable logistic regression, results were mostly consistent. Changing from physician ownership to systems ownership was still positively associated with improvements in PRPR components where statistically significant. The relationship between PRPR components and decreases in the proportion of PCP, however, was not robust. Analyses of individual PRPR components revealed that system ownership was primarily associated with improved PRPR primarily due to improved assessment of patient needs (odds ratio (OR) = 17.88, 95 percent CI = 2.50, 127.77, p = .005), although we also found that system ownership was associated with practices having systems to promptly resolve patient complaints (OR = 3.88, 95 percent CI = 1.02, 14.82, p = .047) and whether practices studied patient complaints to identity patterns (OR = 6.56, 95 percent CI = 3.35, 31.89, p = .021). Furthermore, while the effect of increasing practice size on overall PRPR was negative and statistically significant, the relationship was almost entirely driven by the decreased likelihood of larger practices to use data from patients to develop new services. This is the only PRPR item for which the relationship between increased practice size and PRPR was negative and significant (OR = 0.25, 95 percent CI = 0.07, 0.87, p = .023). Control variables in our final models all had variance inflation factors less than 2.0, indicating that collinearity was not a concern.
Sensitivity Analyses
While we were concerned about potential ceiling or floor effects impacting the level of over time change that was possible, excluding practices with PRPR scores at the extremes did not substantially change the overall results (data not shown). Removing CMP control variables also did not measurably change the impact of change in ownership from physician‐owned to system‐owned (β = 0.31, 95 percent CI = 0.08, 0.52, p = .010), the impact of increase in practice size (β = −0.43, 95 percent CI = −0.66, −0.20, p = .0004) or the impact of decrease in the proportion of PCP (β = −0.27, 95 percent CI = −0.038, −0.16, p < .0001).
Discussion
There is concern that ownership transitions of medical practices from physicians to large systems may negatively impact practices’ responsiveness to patient complaints and feedback (Halley 2014). Our results indicate that transitions from physician ownership to system ownership are actually associated with increased use of strategies to respond to patient complaints, feedback, and develop new services. This improvement may stem from the fact that compared to physician‐owned practices, system‐owned practices face greater pressure from accreditors and payers to develop a systematic process for receiving and responding to patient complaints. The perception that transitions to system ownership deteriorate practice responsiveness may be common, on the other hand, because increased practice size and changes in specialty composition often co‐occur with transitions to system ownership and these changes can reduce the use of practice strategies to respond to patients.
Our finding that transitions of practice ownership do not diminish and may, in fact, modestly increase practice use of strategies to respond to patients has important policy implications to fostering patient‐centered care as the Medicare Access and Children's Health Insurance Program Reauthorization Act of 2015 (MACRA) is implemented (“Education and Tools—Quality Payment Program,” n.d.). MACRA establishes value‐based payment incentives and quality of care targets, which require physicians to assume risk as well as upfront costs. In order to obtain the necessary resources to buffer against risk, physicians have a choice of either (1) joining an alternative payment model arrangement and assuming risk for potential losses or (2) becoming part of an incentive payment arrangement, which involves meeting quality and cost targets. As practice size is expected to increase under both system ownership and physician ownership under MACRA (Muhlestein and Smith 2016), it is important to identify strategies that can mitigate the negative impact of this increase in size on the responsiveness of practices to patients.
Results of the individual components of PRPR highlight that transitions to system ownership are associated with the improved assessment of patient needs, which appears to drive the positive relationship of transitions to system ownership and improved PRPR. Improved needs assessment may result from these transitions because systems tend to have more formalized planning of operations and management, including the processing and resolution of patient complaints. Improved needs assessment may also result from the increased consultation and referrals between hospitals and physician organizations within systems that are facilitated by organizational integration (Baker, Bundorf, and Kessler 2014). Our sensitivity analysis supports this proposition because we found that decreases in the proportion of primary care practitioners, that is, increases in the proportion of specialists, are positively associated with the use of strategies to assess patients’ needs.
Declines in PRPR appear to stem from increased practice size and not system ownership, per se. While modest, our results suggest that efforts to centralize resources should give thoughtful attention to retaining a certain level of decentralization. Physician organizations seeking to grow to improve their ability to assume risk may find that fostering local accountability for responding to patient concerns may be most effective in improving efficiency and quality. This might involve, for example, organizing physicians into pods or teams accountable for managing a defined and consistent patient population. This may help maintain more personalized and responsive relationships between patients and their medical teams as practices and systems become larger.
Limitations
Our findings should be considered in light of some limitations. First, the survey data were collected from a single practice respondent. This individual was identified as the most knowledgeable about practice operations, but resources were not available to independently assess the validity of the information provided. Second, while we addressed practice strategies for patient responsiveness, future research should also obtain patient assessments and assess the extent to which these strategies are correlated with patient‐centeredness. Nevertheless, we believe our data and findings provide insights central to understanding the impact of practice‐reported use of strategies to respond to patients. Third, selection effects are possible, as practices are not randomly acquired by systems. The selection and acquisition of practices may involve very different strategies for different types of practices in different contexts. To address potential selection, we account for heterogeneity in practice environments by including the Herfindahl‐Hirschman Index for county‐level hospital competition in our models. The sample size precluded the use of other methods to reduce selection effects such as propensity score matching. Despite these limitations, our findings provide the first empirical analysis of practice strategies for patient responsiveness within a large, national, longitudinal cohort of practices such that we can begin to untangle the nuanced and multifactorial impacts of practice characteristics on different aspects of the quality of care.
Conclusion
While we initially hypothesized that changes to system ownership may lead to declines in practice responsiveness to patient concerns, we found that system ownership of a physician organization is associated with increases in the use of strategies for responding to patient feedback. Transitions in practice ownership from physicians to systems, such as hospitals and health care systems, are not in and of itself associated with decreases in the use of these strategies. Practices that are transitioning to system ownership may be able to mitigate the impact of size and specialty mix by being attentive to administrative processes for patient responsiveness and initiating interventions that mitigate any negative effects.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We would like to thank Patricia Ramsay for her contribution in helping to conduct the NSSMPP, NSPO2, and NSPO3 studies and managing the data from these studies. We thank Larry Casalino for his participation in fielding the surveys and Richard Scheffler for acquiring the market data used in the analyses.
This study was supported by the Robert Wood Johnson Foundation (Award Nos. 35305, 68847, and 51573), the California HealthCare Foundation (Award No. 041109), the Commonwealth Fund (20050334), and by AHRQ's Comparative Health System Performance Initiative (Grant No. 1U19HS024075) which studies how health care delivery systems promote evidence‐based practices and patient‐centered outcomes research in delivering care. Ms. Poon's effort was supported by an Agency for Healthcare Research and Quality(AHRQ) National Research Service Award (NRSA) Institutional Research Training Grant (4T32HS022241).
The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from the following IMS Health information service(s): Healthcare Organizational Services (2007) IMS Health Incorporated. All rights reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IMS Health Incorporated or any of its’ affiliated or subsidiary entities. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of AHRQ.
Disclosures: None.
Disclaimer: None.
References
- AHA Annual Survey|American Hospital Association's Annual Survey Database|AHA Data Online . (n.d.). [accessed on November 25, 2016]. Available at https://www.ahadataviewer.com/book-cd-products/AHA-Survey/
- Baker, L. C. , Bundorf M. K., and Kessler D. P.. 2014. “Vertical Integration: Hospital Ownership of Physician Practices Is Associated with Higher Prices and Spending.” Health Affairs 33 (5): 756–63. [DOI] [PubMed] [Google Scholar]
- Besanko, D. , Dranove D., Shanley M., and Schaefer S.. 2009. Economics of Strategy. New York: John Wiley & Sons. [Google Scholar]
- Bishop, T. F. , Shortell S. M., Ramsay P. P., Copeland K. R., and Casalino L. P.. 2016. “Trends in Hospital Ownership of Physician Practices and the Effect on Processes to Improve Quality.” American Journal of Managed Care 22 (3): 172–6. [PMC free article] [PubMed] [Google Scholar]
- Burns, L. R. , Goldsmith J. C., and Sen A.. 2013. “Horizontal and Vertical Integration of Physicians: A Tale of Two Tails.” Advances in Health Care Management 15: 39–117. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services . 2004. The CMS Interpretive Guidelines for the Hospital Conditions of Participation. HC Pro, Inc; [accessed on July 9, 2017] Available at http://books.google.com/books?hl=en&lr=&id=BWowcjieej4C&oi=fnd&pg=PR7&dq=%22of+patient-focused+and+organizational+functions+and+processes.+The%22+%22is+the+means+used+to+assess+compliance+with+Federal+health,+safety,+and%22+%22and+Policy%22+%22Should+an+individual+or+entity+(hospital)+refuse+to+allow+immediate+access%22+&ots=UK1VlX8xJE&sig=fd9k5x_wmXMOufXpmL1u_0ISR6Q [Google Scholar]
- Connor, R. A. , Feldman R. D., Dowd B. E., and Radcliff T. A.. 1997. “Which Types of Hospital Mergers Save Consumers Money?” Health Affairs 16 (6): 62–74. [DOI] [PubMed] [Google Scholar]
- Cuellar, A. E. , and Gertler P. J.. 2003. “Trends in Hospital Consolidation: The Formation of Local Systems.” Health Affairs 22 (6): 77–87. [DOI] [PubMed] [Google Scholar]
- Education and Tools—Quality Payment Program . (n.d.). [accessed on November 23, 2016]. Available at https://qpp.cms.gov/education
- Halley, M. D. 2014. “Hospital‐Owned Medical Practices Gaining the Benefits without the Losses.” Healthcare Financial Management: Journal of the Healthcare Financial Management Association 68 (4): 90–4. [PubMed] [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations . 2000. Comprehensive Accreditation Manual for Hospitals: The Official Handbook. Oakbrook Terrace, IL: Joint Commission on Accreditation of Healthcare Organizations. [Google Scholar]
- Keckley, P. H. , Coughlin S. H., and Stanley E. L.. 2013. Deloitte 2013 Survey of US Physicians: Physician Perspectives about Health Care Reform and the Future of the Medical Profession. London: Deloitte Center for Health Solutions. [Google Scholar]
- Kocher, R. , and Sahni N. R.. 2011. “Hospitals’ Race to Employ Physicians — The Logic behind a Money‐Losing Proposition.” New England Journal of Medicine 364 (19): 1790–3. [DOI] [PubMed] [Google Scholar]
- Kralewski, J. E. , Pitt L., and Shatin D.. 1985. “Structural Characteristics of Medical Group Practices.” Administrative Science Quarterly 30 (1): 34–45. [PubMed] [Google Scholar]
- Liebhaber, A. , and Grossman J. M.. 2007. “Physicians Moving to Mid‐Sized, Single‐Specialty Practices.” Tracking Report/Center for Studying Health System Change 18: 1–5. [PubMed] [Google Scholar]
- Mehrotra, A. , Epstein A. M., and Rosenthal M. B.. 2006. “Do Integrated Medical Groups Provide Higher‐Quality Medical Care Than Individual Practice Associations?” [Product Page] [accessed on April 17, 2017]. Available at https://www.rand.org/pubs/external_publications/EP20061234.html [DOI] [PubMed]
- Mick, S. S. F. , and Shay P. D.. 2016. “Accountable Care Organizations and Transaction Cost Economics.” Medical Care Research and Review 73 (6): 649–59. [DOI] [PubMed] [Google Scholar]
- Muhlestein, D. B. , and Smith N. J.. 2016. “Physician Consolidation: Rapid Movement from Small to Large Group Practices, 2013–15.” Health Affairs 35 (9): 1638–42. [DOI] [PubMed] [Google Scholar]
- Nunnally, J. , and Bernstein I.. 1978. Psychometric Theory. New York: McGraw‐Hill. [Google Scholar]
- Pauly, M. V. 1996. “Economics of Multispecialty Group Practice.” Journal of Ambulatory Care Management 19 (3): 26–33. [DOI] [PubMed] [Google Scholar]
- Rittenhouse, D. R. , Grumbach K., O'Neil E. H., Dower C., and Bindman A.. 2004. “Physician Organization and Care Management in California: From Cottage to Kaiser.” Health Affairs 23 (6): 51–62. [DOI] [PubMed] [Google Scholar]
- Rittenhouse, D. R. , Casalino L. P., Shortell S. M., McClellan S. R., Gillies R. R., Alexander J. A., and Drum M. L.. 2011. “Small and Medium‐Size Physician Practices Use Few Patient‐Centered Medical Home Processes.” Health Affairs 30 (8): 1575–84. [DOI] [PubMed] [Google Scholar]
- Robinson, J. C. , and Miller K.. 2014. “Total Expenditures Per Patient in Hospital‐Owned and Physician‐Owned Physician Organizations in California.” Journal of the American Medical Association 312 (16): 1663–9. [DOI] [PubMed] [Google Scholar]
- Rodriguez, H. P. , Von Glahn T., Rogers W. H., and Safran D. G.. 2009. “Organizational and Market Influences on Physician Performance on Patient Experience Measures.” Health Services Research 44 (3): 880–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez, H. P. , McClellan S. R., Bibi S., Casalino L. P., Ramsay P. P., and Shortell S. M.. 2016. “Increased Use of Care Management Processes and Expanded Health Information Technology Functions by Practice Ownership and Medicaid Revenue.” Medical Care Research and Review: MCRR 73 (3): 308–28. [DOI] [PubMed] [Google Scholar]
- Scott, K. W. , Orav E. J., Cutler D. M., and Jha A. K.. 2016. “Changes in Hospital–Physician Affiliations in U.S. Hospitals and Their Effect on Quality of CareHospital–Physician Integration and Health Care Quality.” Annals of Internal Medicine 166: 1–8. 10.7326/M16-0125 [DOI] [PubMed] [Google Scholar]
- Shortell, S. M. , Marsteller J. A., Lin M., Pearson M. L., Wu S.‐Y., Mendel P., Cretin S., and Rosen M.. 2004. “The Role of Perceived Team Effectiveness in Improving Chronic Illness Care.” Medical Care 42 (11): 1040–8. [DOI] [PubMed] [Google Scholar]
- Shortell, S. M. , Schmittdiel J., Wang M. C., Li R., Gillies R. R., Casalino L. P., Bodenheimer T., and Rundall T. G.. 2005. “An Empirical Assessment of High‐Performing Medical Groups: Results from a National Study.” Medical Care Research and Review: MCRR 62 (4): 407–34. [DOI] [PubMed] [Google Scholar]
- Shortell, S. M. , Gillies R., Siddique J., Casalino L. P., Rittenhouse D., Robinson J. C., and McCurdy R. K.. 2009. “Improving Chronic Illness Care: A Longitudinal Cohort Analysis of Large Physician Organizations.” Medical Care 47 (9): 932–9. [DOI] [PubMed] [Google Scholar]
- Shortell, S. M. , Wu F. M., Lewis V. A., Colla C. H., and Fisher E. S.. 2014. “A Taxonomy of Accountable Care Organizations for Policy and Practice.” Health Services Research 49: 1883–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spang, H. R. , Bazzoli G. J., and Arnould R. J.. 2001. “Hospital Mergers and Savings For Consumers: Exploring New Evidence.” Health Affairs 20 (4): 150–8. [DOI] [PubMed] [Google Scholar]
- Wheelan, S. A. 2009. “Group Size, Group Development, and Group Productivity.” Small Group Research 40 (2): 247–62. [Google Scholar]
- Wiley, J. A. , Rittenhouse D. R., Shortell S. M., Casalino L. P., Ramsay P. P., Bibi S., Ryan A. M., Copeland K. R., and Alexander J. A.. 2015. “Managing Chronic Illness: Physician Practices Increased the Use of Care Management and Medical Home Processes.” Health Affairs (Project Hope) 34 (1): 78–86. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


