Abstract
Objective
(1) To examine usual source of care (USC) trends across four categories (No USC, Person USC, Person, in Facility USC, and Facility USC), and (2) to determine whether USC types are associated with emergency department (ED) visits and hospital admissions.
Data Source
1996–2014 Medical Expenditure Panel Surveys.
Study Design
We stratified each USC category, by age, region, gender, poverty, insurance, race/ethnicity, and education and used regression to determine the characteristics associated with USC types, ED visits, and hospital admissions.
Principal Findings
Those with No USC and Facility USCs increased 10 and 18 percent, respectively, while those with Person USCs decreased by 43 percent. Compared to those in the lowest income bracket, those in the highest income bracket were less likely to have a Facility USC. Among those with low incomes, individuals with No USC, Person, in Facility, and Facility USCs were more likely to have ED visits than those with Person USCs.
Conclusions
A growing number are reporting facilities as their USCs or none at all. The impact of these trends is uncertain, although we found that some USC types are associated with ED visits and hospital admissions. Tracking USCs will be crucial to measuring progress toward enhanced care efficiency.
Keywords: Primary care, access/demand/utilization of services, health policy/politics/law/regulation
Accessing the health care system can result in a wide spectrum of outcomes—from timely life‐saving interventions to fragmented care (Institute of Medicine 2013) to unnecessary, harmful tests (Brownlee 2008). Having a singular person or facility for navigating most health care needs, also known as a usual source of care (USC), can facilitate access to the right care (DeVoe et al. 2003) at the right place (Villani and Mortensen 2013; Liaw et al. 2014; Janke et al. 2015) at the right time (Grumbach, Keane, and Bindman 1993).
A USC is associated with myriad patient‐level benefits including higher quality, reduced unmet needs, and reduced health disparities (Corbie‐Smith et al. 2002; DeVoe et al. 2011, 2012; Kim et al. 2012). When patients have a trusted guide, they change their care‐seeking behavior, which has positive effects on the health care system. For example, studies have found that those with a USC rely less on emergency departments (EDs; Villani and Mortensen 2013; Liaw et al. 2014; Janke et al. 2015), although the relationship between having a USC and hospital admissions remains indeterminate (Spatz et al. 2014; Coller et al. 2015). While pairing a USC with insurance synergistically increases access, having a USC has been shown to be the more powerful predictor (Bindman et al. 1996; Sox et al. 1998; Dovey et al. 2003; Fryer et al. 2003; Bliss et al. 2004). Even for the uninsured, the act of establishing care with a point of contact facilitates access to doctor visits and preventive services (Lambrew et al. 1996; DeVoe et al. 2003).
Over the past decade, policy reforms have altered how patients interact with providers, calling into question whether these relationships have changed. The primary care medical home (PCMH) movement shifted control from individual physicians to teams of clinicians, working in high‐functioning clinics (Patient‐Centered Primary Care Collaborative 2007). While the Affordable Care Act (ACA) expanded insurance to millions (Congressional Budget Office 2014), it also fueled high deductible health plans (Collins et al. 2015), which have influenced how patients choose to access the system (Collins et al. 2014).
On the provider side, accountable care organizations (ACOs) and the Medicare Access and CHIP (Children's Health Insurance Program) Reauthorization Act (MACRA) are encouraging clinicians to transition to value‐based reimbursement and invest in enhanced services such as after‐hours care, data‐analytics, and care coordination. Practices have consolidated to distribute these costly, fixed expenses across larger numbers of clinicians (Liebhaber and Grossman 2007). These changes may affect patients’ relationships with clinics and clinicians, although the directionality of those changes is yet to be determined.
While we are unaware of reports documenting a rise in USCs that are facilities rather than individuals, the aforementioned forces portend just that. This shift from USCs that are people to ones that are places can be expected to have downstream effects as having a person USC has been shown to be superior in terms of accessing certain preventive services (Lambrew et al. 1996; Xu 2002). The type of USC also affects utilization. For example, those that identify that ED as their USC are more likely to have ED visits (O'Brien et al. 1997). In contrast, an analysis conducted in Korea found that having a person USC as opposed to a place was associated with fewer ED visits and hospitalizations (Kim, Jeon, and Lee 2017). Following a distinct but related line of inquiry, others have documented the relationship between practice size and utilization. Casalino found that practices with 1–2 physicians had fewer preventable admissions compared to larger practices and went on to hypothesize that patients and staff in smaller practices may know each other better and that these stronger relationships may prevent unnecessary hospitalizations (Casalino et al. 2014).
Our analysis adds to the existing literature in several ways. First, we use a broad time frame, encompassing the release of the PCMH joint principles, the passage of the Health Information Technology for Economic and Clinical Health Act which expanded the adoption of electronic health records (EHRs), and the passage of the ACA. Second, we use different categories to delineate the types of USC in order to capture heterogeneity. The objectives of our study were fourfold: to determine (1) the percentage of people in the United States with (a) No USC, (b) Person, (c) Person, in Facility, and (d) Facility USC; (2) how these percentages have changed over time; (3) the characteristics of people within each USC category; (4) whether these USC categories are associated with ED visits and hospital admissions.
Methods
Data Sources
We conducted a trend analysis assessing the types of USCs, using cross‐sectional data from the 1996–2014 Medical Expenditure Panel Survey (MEPS), which estimates health services use and medical expenditures by following patients over two‐and‐a‐half‐year periods. This anonymous, publicly available dataset is weighted, allowing for estimation of national results.
Variables
Usual source of care was determined by the following question: “Is there a particular doctor's office, clinic, health center, or other place that you usually go to if you are sick or need advice about your health?” Those responding yes were then asked two additional questions which clarified whether the patient perceived the USC to be a person, a facility, or person embedded within a facility (Figure S1). Of note, in 2008, an additional probing question was added for persons identifying a facility as the USC, asking the respondent to declare whether or not he/she sees a particular individual within the facility. If so, the USC was coded as a Person, in Facility (Agency for Healthcare Research and Quality and Quality 2008). Using this protocol, we created four mutually exclusive USC categories: (1) No USC, (2) Person (e.g., a solo physician), (3) Person, in Facility (e.g., a physician working within a primary care clinic), or (4) Facility (e.g., a primary care clinic or an emergency department). USC responses are collected in rounds 2 and 4 within a MEPS panel, each of which lasts 2.5 years. Round 2 occurs in the first year while round 4 occurs in the second; therefore, our annual figures include responses from two different panels. We did not capture USC changes at the individual level, but rather, used cross‐sectional data to calculate estimates by survey year.
For each type of USC, we assessed patient age, region of the country, gender, poverty level, insurance coverage, race/ethnicity, and highest educational degree completed. We categorized age into five groups: (1) 0–17 years of age, (2) 18–34, (3) 35–49, (4) 40–64, and (5) 65 years of age or older. Household poverty was categorized as (1) less than 100 percent of the federal poverty level (FPL), (2) 100–124 percent FPL, (3) 125–199 percent FPL, (4) 200–399 percent FPL, and (5) 400 percent FPL or greater.
We categorized insurance as private, Medicare, Medicaid, other public insurance, dually eligible, or uninsured. Individuals were considered privately insured if they were covered by private insurance at any point in the year. They were classified as Medicare, Medicaid, or other public insurance (such as Tricare) if they were covered by Medicare, Medicaid, or other public insurance, respectively, at some point in the year but not private insurance. They were classified as dually eligible if they were covered by both Medicare and Medicaid at some point in the year but not private insurance. The uninsured were neither covered by public nor private insurance at any point in the year. For highest level of education completed, we created three categories: (1) <12 years of education, (2) a high school diploma or general education development (GED), and (3) posthigh school degree. To understand the impact of USC changes, we created dichotomous variables identifying individuals with any ED visits or hospital admissions. In MEPS, hospital admissions and ED visits are reported for each survey year, rather than across the 2.5‐year panel period.
In general, those lacking USCs are seldom sick and consume fewer health care resources compared to those with USCs (Pancholi 2004; Phillips et al. 2009). In our analysis of the association between USC type and ED visits and hospitalizations, we adjusted for this self‐selection bias by including two variables that account for baseline health and utilization and have been linked to ED visits (Weber et al. 2005). First, we included reported physical health status, which has five categories: excellent, very good, good, fair, and poor. Second, we accounted for the number of office‐based visits, which we grouped into four categories: 0, 1–3, 4–9, and 10 or more.
Statistical Analysis
Using STATA 14.0 (StataCorp. 2015; Stata Statistical Software: Release 14; StataCorp LP, College Station, TX), we conducted bivariate analyzes by USC type and used chi‐squared tests for categorical variables. To obtain valid national estimates for USC, we included complex MEPS survey design variables (primary sampling units and strata) and sampling weights in our analysis using survey commands in STATA. To assess the characteristics associated with the USC types, we created two models. In the first model, we performed logistic regression. The dependent variable was whether or not the individual had a USC, while MEPS year, region, gender, poverty, insurance, education, and age were the independent variables. Restricting the sample to those with a USC, we also conducted a multinomial regression where the dependent variable was USC type, while the independent variables were the same as above.
We also examined whether the USC categories were associated with differences in ED visits and hospitalizations. The dependent variable was whether or not the individual had an ED visit or hospital admission. The independent variables were the same as above in addition to the USC categories, reported health, and office‐based visits. We estimated logistic regression models for each outcome. Due to the possibility that the impact of USC type varies by income level (Kangovi et al. 2013), we also estimated models that included an interaction between low income and USC type as well as bifurcated the sample into low‐income (<200 percent of the FPL) and high‐income (≥200 percent of the FPL) categories. To quantify changes in utilization associated with changes in USC between 1996 and 2014, we first calculated the unadjusted means for the USC categories by income group. Based on the regression coefficients calculated above and variable means, we determined adjusted rates of ED visits and hospitalizations. We then examined the overall rate using first the 1996 observed distribution and then the 2014 distribution.
As our analysis was restricted to a publicly available dataset, institutional review board approval was neither required nor obtained.
Results
We included 559,762 respondents in the analysis. In 2014, across the age categories, respondents most commonly identified Facility USCs (Table 1). Within the Facility USC category, the percentage was highest among respondents <18 years of age. Within the No USC category, the percentage was highest among the 18–34 year olds while the highest percentage for Person USC was among the oldest respondents. Overall, 14 percent of our sample had an ED visit while 6 percent had a hospital admission.
Table 1.
Demographic Characteristics of Study Population, by Type of Usual Source of Care (USC), 2014
| Characteristics | All | No USC | Person | Person, in Facility | Facility | p‐Valuea | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | % | Number | % | Number | % | Number | % | Number | % | ||
| Total | 32,389 | 100 | 7,271 | 22.4 | 4,749 | 14.7 | 6,021 | 18.6 | 14,258 | 44.0 | |
| Gender | |||||||||||
| Male | 15,376 | 48.9 | 4,025 | 23.3 | 2,145 | 14.7 | 2,629 | 20.4 | 6,577 | 41.6 | <.001 |
| Female | 16,913 | 51.1 | 3,246 | 16.5 | 2,604 | 16.2 | 3,392 | 23.9 | 7,671 | 43.3 | |
| Age | |||||||||||
| Less than 18 years old | 9,036 | 23.2 | 826 | 7.9 | 1,340 | 13.6 | 1,584 | 20.6 | 5,286 | 57.9 | <.001 |
| 18–34 years old | 7,553 | 23.0 | 3,134 | 38.5 | 709 | 10.5 | 876 | 14.4 | 2,834 | 36.6 | |
| 35–49 years old | 6,084 | 18.8 | 1,970 | 27.5 | 778 | 14.6 | 963 | 18.9 | 2,373 | 39.0 | |
| 50–64 years old | 5,775 | 20.2 | 1,066 | 15.5 | 1,006 | 18.1 | 1,322 | 25.6 | 2,381 | 40.8 | |
| 65 or older | 3,841 | 14.8 | 275 | 5.9 | 916 | 23.6 | 1,276 | 36.5 | 1,374 | 34.0 | |
| Age missing | 27 | 0.1 | 17 | 64.1 | 0 | 0 | 3 | 12.9 | 7 | 23.0 | |
| Education | |||||||||||
| Less than high school | 13,956 | 33.8 | 2,409 | 14.2 | 1,990 | 14.2 | 2,285 | 19.8 | 7,272 | 51.8 | <.001 |
| High school diploma/GED | 6,337 | 19.9 | 1,878 | 25.2 | 890 | 15.5 | 1,144 | 21.8 | 2,425 | 37.4 | |
| Post high school | 11,836 | 45.9 | 2,919 | 21.5 | 1,840 | 16.3 | 2,577 | 24.3 | 4,500 | 37.8 | |
| Education missing | 160 | 0.3 | 65 | 36.0 | 29 | 28.4 | 15 | 6.4 | 51 | 29.2 | |
| Race/ethnicity | |||||||||||
| Non‐Hispanic, White | 11,710 | 61.3 | 2,021 | 16.4 | 1,817 | 15.9 | 3,042 | 26.6 | 4,830 | 41.1 | <.001 |
| Non‐Hispanic, Black | 6,733 | 12.1 | 1,512 | 23.2 | 888 | 13.2 | 1,216 | 18.4 | 3,117 | 45.2 | |
| Non‐Hispanic, Other | 3,480 | 9.1 | 741 | 21.5 | 677 | 19.1 | 566 | 15.0 | 1,496 | 44.3 | |
| Hispanic | 10,366 | 17.5 | 2,997 | 28.8 | 1,367 | 13.6 | 1,197 | 13.3 | 4,805 | 44.3 | |
| Region | |||||||||||
| South | 5,768 | 21.3 | 1,029 | 16.2 | 705 | 13.1 | 1,547 | 29.1 | 2,487 | 41.6 | <.001 |
| Northeast | 12,102 | 37.2 | 3,255 | 23.8 | 1,883 | 16.0 | 1,961 | 18.6 | 5,003 | 41.7 | |
| Midwest | 4,931 | 17.3 | 787 | 14.7 | 1,014 | 22.5 | 1,051 | 26.0 | 2,079 | 36.9 | |
| West | 9,276 | 23.5 | 2,164 | 21.0 | 1,126 | 11.8 | 1,426 | 19.0 | 4,560 | 48.2 | |
| Region missing | 212 | 0.6 | 36 | 13.0 | 21 | 11.9 | 36 | 20.9 | 119 | 54.2 | |
| Federal poverty level | |||||||||||
| Less than 100% | 7,783 | 14.7 | 1,820 | 23.3 | 1,009 | 13.7 | 1,116 | 16.5 | 3,838 | 46.5 | <.001 |
| 101–124% | 2,054 | 4.6 | 502 | 21.0 | 299 | 14.3 | 288 | 19.5 | 965 | 45.1 | |
| 125–199% | 5,555 | 13.9 | 1,485 | 25.6 | 758 | 14.5 | 868 | 18.6 | 2,444 | 41.4 | |
| 200–399% | 8,993 | 28.9 | 2,160 | 21.4 | 1,304 | 14.3 | 1,815 | 22.9 | 3,714 | 41.4 | |
| 400% and greater | 7,904 | 37.9 | 1,304 | 15.1 | 1,379 | 17.6 | 1,934 | 25.6 | 3,287 | 41.7 | |
| Insurance coverage | |||||||||||
| Private | 13,926 | 54.4 | 2,866 | 18.6 | 2,090 | 15 | 2,870 | 22.4 | 6,100 | 43.9 | <.001 |
| Medicare | 3,442 | 14.4 | 235 | 5.8 | 770 | 23.1 | 1,202 | 36.7 | 1,235 | 34.4 | |
| Medicaid | 9,285 | 18.4 | 1,519 | 17.2 | 1,320 | 14.3 | 1,418 | 17.8 | 5,028 | 50.7 | |
| Dual | 1,081 | 2.4 | 92 | 8 | 254 | 21.1 | 292 | 29.3 | 443 | 41.7 | |
| Other public | 134 | 0.4 | 44 | 32 | 14 | 9.5 | 13 | 14.1 | 63 | 44.4 | |
| Not insured | 4,342 | 9.7 | 2,511 | 55.5 | 284 | 7.6 | 205 | 6.3 | 1,342 | 30.6 | |
| Any emergency department visits | |||||||||||
| Yes | 4,633 | 14 | 757 | 14.4 | 702 | 16.1 | 1,020 | 25.9 | 2,154 | 43.7 | <.001 |
| Any hospital admissions | |||||||||||
| Yes | 1,985 | 6.3 | 260 | 11.7 | 374 | 19.6 | 503 | 29.9 | 848 | 38.8 | <.001 |
Source: Authors’ analysis of the 2014 Medical Expenditure Panel Survey.
Tests of significance are across the four usual source of care categories.
N = 32,289.
Among those with No USC, the percentages were highest for those without insurance, Hispanics, and with a high school diploma. Among those with Person, in Facility USC, the percentages were highest for those with incomes at 400 percent of the FPL or greater, on Medicare, who are White, and with post–high school education. Among those with Facility USC, the percentages were highest for those with incomes at <100 percent of the FPL, on Medicaid, who are Black, and with less than a high school education.
Our regression results indicated that the odds of having a USC decreased over time (Table 2). Having a USC was associated with higher incomes and having insurance. Females were more likely to have a USC as were Whites. Eighteen to thirty‐four year olds were the age group least likely to have USCs.
Table 2.
Logistic Regression: Patient Characteristics Associated with Usual Source of Care (USC), Compared to Having No USC
| Characteristics | Have a Usual Source of Care | |
|---|---|---|
| Odds Ratio | 95% Confidence Interval | |
| Year | ||
| 1996 | 1 | 1–1 |
| 1997 | 1.046 | 0.940–1.163 |
| 1998 | 0.928 | 0.839–1.027 |
| 1999 | 0.934 | 0.844–1.034 |
| 2000 | 0.922 | 0.824–1.031 |
| 2001 | 0.934 | 0.858–1.017 |
| 2002 | 0.920* | 0.844–1.002 |
| 2003 | 0.919* | 0.837–1.009 |
| 2004 | 0.900** | 0.825–0.981 |
| 2005 | 0.879*** | 0.804–0.960 |
| 2006 | 0.922* | 0.843–1.008 |
| 2007 | 0.834*** | 0.765–0.908 |
| 2008 | 0.799*** | 0.727–0.878 |
| 2009 | 0.830*** | 0.757–0.910 |
| 2010 | 0.875*** | 0.799–0.957 |
| 2011 | 0.887*** | 0.814–0.967 |
| 2012 | 0.832*** | 0.758–0.913 |
| 2013 | 0.840*** | 0.768–0.920 |
| 2014 | 0.831*** | 0.760–0.910 |
| Gender | ||
| Male | 1 | 1–1 |
| Female | 1.641*** | 1.609–1.674 |
| Age | ||
| Less than 18 years old | 1 | 1–1 |
| 18–34 years old | 0.198*** | 0.189–0.206 |
| 35–49 years old | 0.330*** | 0.316–0.345 |
| 50–64 years old | 0.561*** | 0.535–0.589 |
| 65 or older | 0.596*** | 0.545–0.652 |
| Education | ||
| Less than high school | 1 | 1–1 |
| High school diploma/GED | 1.062*** | 1.025–1.101 |
| Post high school | 1.017 | 0.987–1.048 |
| Race/Ethnicity | ||
| Non‐Hispanic, White | 1 | 1–1 |
| Non‐Hispanic, Black | 0.796*** | 0.762–0.831 |
| Non‐Hispanic, Other | 0.713*** | 0.663–0.767 |
| Hispanic | 0.640*** | 0.613–0.669 |
| Region | ||
| South | 1 | 1–1 |
| Northeast | 1.633*** | 1.530–1.742 |
| Midwest | 1.337*** | 1.258–1.421 |
| West | 1.064** | 1.007–1.125 |
| Federal poverty level | ||
| Less than 100% | 1 | 1–1 |
| 101–124% | 1.02 | 0.963–1.080 |
| 125–199% | 1.025 | 0.983–1.068 |
| 200–399% | 1.230*** | 1.178–1.284 |
| 400% and greater | 1.488*** | 1.423–1.556 |
| Insurance coverage | ||
| Private | 1 | 1–1 |
| Medicare | 1.900*** | 1.735–2.081 |
| Medicaid | 1.042 | 0.990–1.096 |
| Dual | 2.070*** | 1.864–2.300 |
| Other public | 0.749*** | 0.634–0.886 |
| Not insured | 0.280*** | 0.268–0.292 |
| Constant | 8.187*** | 7.444–9.003 |
Source: Authors’ analysis of the 1996 to 2014 Medical Expenditure Panel Surveys.
N = 559,762.
***p < .01, **p < .05, *p < .1.
After restricting to only those with USCs, relative to Person USC, the likelihood of having a Person, in Facility, or Facility USC increased over time (Table 3). Those with Facility USCs were less likely to have incomes in the highest bracket, while the converse was true for those with Person, in Facility USCs. Those with Facility USCs were also more likely to be uninsured and were more likely to be Black.
Table 3.
Multinomial Regression: Patient Characteristics Associated with Usual Source of Care (USC) Types, Compared to Having a Person USC
| Characteristics | Person, in Facility | Facility | ||
|---|---|---|---|---|
| Relative Risk Ratio | 95% Confidence Interval | Relative Risk Ratio | 95% Confidence Interval | |
| Year | ||||
| 1996 | 1 | 1–1 | 1 | 1–1 |
| 1997 | 0.922 | 0.795–1.069 | 1.013 | 0.870–1.180 |
| 1998 | 0.905 | 0.790–1.037 | 1.063 | 0.914–1.237 |
| 1999 | 0.880* | 0.768–1.008 | 1.063 | 0.917–1.232 |
| 2000 | 0.966 | 0.822–1.135 | 1.102 | 0.926–1.312 |
| 2001 | 0.922 | 0.808–1.052 | 1.188** | 1.027–1.373 |
| 2002 | 0.914 | 0.797–1.050 | 1.230*** | 1.058–1.429 |
| 2003 | 0.859** | 0.748–0.987 | 1.248*** | 1.074–1.451 |
| 2004 | 0.820*** | 0.706–0.951 | 1.273*** | 1.094–1.482 |
| 2005 | 0.738*** | 0.630–0.864 | 1.322*** | 1.135–1.541 |
| 2006 | 0.735*** | 0.636–0.851 | 1.442*** | 1.240–1.676 |
| 2007 | 0.725*** | 0.636–0.825 | 1.474*** | 1.292–1.683 |
| 2008 | 0.912 | 0.791–1.050 | 1.392*** | 1.201–1.612 |
| 2009 | 1.023 | 0.890–1.176 | 1.427*** | 1.236–1.647 |
| 2010 | 1.023 | 0.887–1.181 | 1.576*** | 1.374–1.807 |
| 2011 | 1.228*** | 1.057–1.427 | 1.707*** | 1.481–1.969 |
| 2012 | 1.376*** | 1.187–1.595 | 1.849*** | 1.609–2.124 |
| 2013 | 1.936*** | 1.673–2.241 | 1.838*** | 1.586–2.129 |
| 2014 | 2.081*** | 1.790–2.418 | 2.195*** | 1.899–2.539 |
| Gender | ||||
| Male | 1 | 1–1 | 1 | 1–1 |
| Female | 1.097*** | 1.073–1.122 | 0.994 | 0.976–1.012 |
| Age | ||||
| Less than 18 years old | 1 | 1–1 | 1 | 1–1 |
| 18–34 years old | 0.895*** | 0.841–0.953 | 1.017 | 0.967–1.070 |
| 35–49 years old | 0.929** | 0.873–0.989 | 0.842*** | 0.798–0.889 |
| 50–64 years old | 0.912*** | 0.856–0.972 | 0.656*** | 0.621–0.693 |
| 65 or older | 0.786*** | 0.712–0.867 | 0.490*** | 0.447–0.536 |
| Education | ||||
| Less than high school | 1 | 1–1 | 1 | 1–1 |
| High school diploma/GED | 1.050* | 0.999–1.103 | 1.116*** | 1.069–1.166 |
| Post high school | 1.078*** | 1.031–1.127 | 0.983 | 0.947–1.020 |
| Race/ethnicity | ||||
| Non‐Hispanic, White | 1 | 1–1 | 1 | 1–1 |
| Non‐Hispanic, Black | 0.840*** | 0.785–0.899 | 1.150*** | 1.077–1.229 |
| Non‐Hispanic, Other | 0.621*** | 0.563–0.685 | 0.801*** | 0.712–0.900 |
| Hispanic | 0.697*** | 0.635–0.765 | 0.948 | 0.883–1.018 |
| Region | ||||
| South | 1 | 1–1 | 1 | 1–1 |
| Northeast | 0.832*** | 0.746–0.929 | 0.765*** | 0.685–0.855 |
| Midwest | 1.671*** | 1.491–1.873 | 1.623*** | 1.412–1.865 |
| West | 1.200*** | 1.081–1.331 | 1.804*** | 1.615–2.016 |
| Federal poverty level | ||||
| Less than 100% | 1 | 1–1 | 1 | 1–1 |
| 101–124% | 1.025 | 0.943–1.114 | 0.947* | 0.889–1.009 |
| 125–199% | 1.028 | 0.962–1.097 | 0.953** | 0.909–0.999 |
| 200–399% | 1.103*** | 1.038–1.172 | 0.909*** | 0.866–0.953 |
| 400% and greater | 1.058* | 0.993–1.128 | 0.813*** | 0.770–0.859 |
| Insurance coverage | ||||
| Private | 1 | 1–1 | 1 | 1–1 |
| Medicare | 1.178*** | 1.074–1.292 | 0.949 | 0.877–1.028 |
| Medicaid | 0.871*** | 0.813–0.932 | 1.045 | 0.985–1.108 |
| Dual | 1.021 | 0.921–1.131 | 0.916* | 0.838–1.001 |
| Other public | 0.771 | 0.554–1.073 | 1.514*** | 1.197–1.916 |
| Not insured | 0.698*** | 0.647–0.753 | 1.196*** | 1.131–1.264 |
| Constant | 0.658*** | 0.574–0.754 | 1.463*** | 1.273–1.682 |
Source: Authors’ analysis of the 1996 to 2014 Medical Expenditure Panel Surveys.
N = 437,235.
***p < .01, **p < .05, * p < .1.
From 1996 to 2014, the adjusted percentage with No USC and Facility USC increased 10 percent (from 18 to 20 percent) and 18 percent (from 36 to 42 percent), respectively (Figure 1). In contrast, Person USC decreased 43 percent (from 27 to 15 percent), and Person, in Facility USC decreased 16 percent though the directionality changed. From 1996 to 2007, the percentage with Person, in Facility USC decreased 36 percent but then increased 48 percent from 2008 to 2012.
Figure 1.
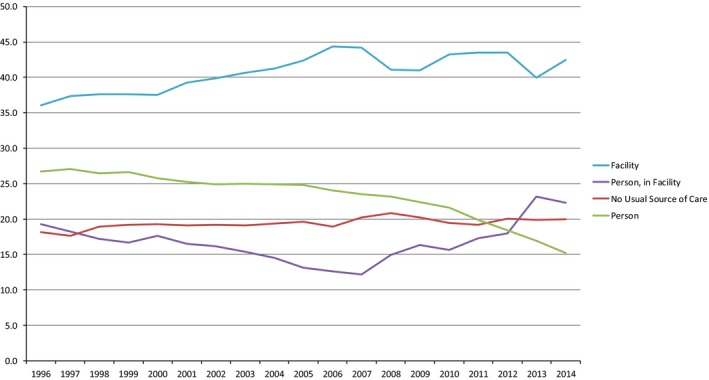
- Source: Authors’ analysis of the 1996–2014 Medical Expenditure Panel Surveys.
For the full sample, the odds of both ED visits and hospitalizations were lower for persons with a Person USC (Table 4). There is a significant interaction between No USC and income in both the ED and hospitalization models, as well as a significant interaction between Facility USC and income in the ED visit model. Given these findings, we estimated models for each income level. Among those with low incomes and relative to those with Person USCs, individuals with No USC were nearly 14 percent more likely to have an ED visit (OR: 1.138, 95% CI: 1.078–1.201). Those with a Facility USC were 12 percent more likely (1.118, 1.070–1.169). Similar findings were obtained using the hospitalization measure. Among those with high incomes, there were generally smaller and often nonsignificant associations between USC type and ED visits compared to those for the low‐income group. Among those with low income, the change in USC types between 1996 and 2014 corresponds to a 0.9 percent increase in individuals with ED visits, or an additional 167,749 people nationally over that time frame (Table S1) and a 0.8 percent increase in hospitalized individuals, or 66,368 additional people. Among the high income, the change in USC corresponds to a 0.4 percent increase in individuals with ED visits (72,119 people), and a 0.7 percent increase in individuals hospitalized (71,175 people).
Table 4.
Logistic Regression: Usual Source of Care Types Associated Emergency Department Visits and Hospital Admissions, by Income Status
| All Respondents | Federal Poverty Level (FPL) Income Level | |||
|---|---|---|---|---|
| Odds Ratio (95% Confidence Interval) | Odds Ratio (95% Confidence Interval) | |||
| No Interaction | With Interaction | <200% FPL | ≥200% FPL | |
| A. Any Emergency Department Visit | ||||
| Usual Source of Care (USC) Type | ||||
| Person | 1 | 1 | 1 | 1 |
| No USC | 1.085 (1.043–1.130)*** | 1.008 (0.954–1.064) | 1.138 (1.078–1.201)*** | 1.044 (0.986–1.106) |
| Person, in Facility | 1.053 (1.018–1.089)*** | 1.036 (0.995–1.077)* | 1.071 (1.008–1.137)** | 1.040 (0.999–1.082)* |
| Facility | 1.062 (1.030–1.094)*** | 1.030 (0.992–1.069) | 1.118 (1.070–1.169)*** | 1.030 (0.992–1.070) |
| Low Income (<200% FPL) | 1.273 (1.238–1.308)*** | 1.179 (1.127–1.233)*** | ||
| Income‐USC Type Interaction | ||||
| No USC*Low Income | 1.198 (1.116–1.287)*** | |||
| Person, in Facility*Low Income | 1.045 (0.974–1.121) | |||
| Facility*Low Income | 1.091 (1.033–1.152)*** | |||
| Observations | 559,356 | 559,356 | 242,608 | 316,748 |
| B. Any Hospital Admission | ||||
| USC Type | ||||
| Person | 1 | 1 | 1 | 1 |
| No USC | 1.195 (1.132–1.260)*** | 1.071 (0.995–1.153)* | 1.249 (1.155–1.352)*** | 1.134 (1.049–1.227)*** |
| Person, in Facility | 1.057 (1.010–1.106)** | 1.059 (1.004–1.118)** | 1.058 (0.981–1.141) | 1.054 (0.998–1.113)* |
| Facility | 1.092 (1.051–1.135)*** | 1.081 (1.031–1.133)*** | 1.110 (1.047–1.177)*** | 1.081 (1.031–1.134)*** |
| Low Income (<200% FPL) | 1.242 (1.196–1.290)*** | 1.190 (1.119–1.265)*** | ||
| Income‐USC Type Interaction | ||||
| No USC*Low Income | 1.284 (1.158–1.423)*** | |||
| Person, in Facility*Low Income | 0.989 (0.902–1.084) | |||
| Facility*Low Income | 1.034 (0.962–1.111) | |||
| Observations | 559,356 | 559,356 | 242,608 | 316,748 |
Source: Authors’ analysis of the 1996 to 2014 Medical Expenditure Panel Surveys.
Analyzes are adjusted for gender, age, race, region, insurance, poverty status, education, reported health, year, and number of office‐based visits. We defined low income as earning less than 200% of the federal poverty level. Data on emergency department and hospitalizations are the totals reported for each survey year.
***p < .01, **p < .05, *p < .1.
Discussion
The powerful, salutary effects of having a USC have been documented for decades. Despite these benefits, we found an increase in the percentage with No USC and a drop in the percentage with Person USC and that these changes are associated with excess ED visits and hospital admissions. While this shift from clinicians to places may ultimately yield net positive effects, it also has the potential to degrade the relationships between patients and their clinicians that are foundational to proper health care.
Some of these findings may not come as a surprise, considering that individuals with USCs in hospitals and outpatient departments have to go there to see their USCs. Regardless, we believe it is important to quantify the impact of having USCs in facilities. Transitioning these individuals to USCs outside the hospital is an intervention worth exploring.
While we document that having a Person USC, rather than a place had positive effects on utilization, the impact was more consistent among low‐income individuals and with respect to ED visits. Although our methods do not allow us to disentangle how providers and facilities interact to enable access, others have found that patient–provider language concordance, after‐hours access, and longitudinal relationships are USC characteristics associated with reduced ED use (O'Malley 2013; Villani and Mortensen 2013; Haber, Wensky, and McCall 2016). We predict the types of USCs offered and their respective competencies will continue to evolve in response to policy changes. These trends and their influence on access will need to be closely monitored.
The rising percentage without a USC is not necessarily at odds with reports of improved access following the ACA. For example, Sommers found that the percentage of young adults (19–25 years old) without a USC fell following implementation of the provision, allowing them to stay on their parents’ private insurance until the age of 26 (Sommers et al. 2013). While we report an increase in the percentage without a USC combining all age groups over the study period, this increase preceded the ACA, and the percentage has declined slightly from 2008 to 2014. As Sommers notes, the ACA's insurance expansion explains some of this recent decline. Consistent with this interpretation, we found that persons without insurance are far less likely to have a USC than the insured.
Increasingly sensitive to prices and able to access medical information, patients are taking control of how and where they access care (Schroeder 2016). The health care industry has responded by offering walk‐in clinics and direct‐to‐consumer genetic and diagnostic tests. These developments encourage patients to be engaged self‐advocates but also call into question the future role of the personal physician. At the Keystone IV Conference, primary care leaders pondered a world where patients lacked an individual whom they could call “my doctor” (Green and Puffer 2016). As fewer Americans identify individuals as USCs, our findings suggest that USCs generally and individual USCs specifically continue to play an important role in facilitating access.
Among those with USCs, we found a tiered system, with well‐educated, White, privately insured, high earners establishing care with Person, in Facility USCs and less educated, uninsured, poor Blacks identifying Facility USCs like EDs. In contrast to the rise of Facility USCs, Person USC is falling. The 2015 MEPS Medical Provider Component Medical Organization Survey provided information about these USCs by asking the practices directly about their organizational structures (Agency for Healthcare Research and Quality 2015). From this survey, we found that nearly 86 percent of the practices categorized as Person USCs have 1–3 physicians in practice. This decline in Person USCs tracks with the continued deterioration of solo and small practices (Liaw et al. 2016). The factors contributing to the resurgence of Person, in Facility USC since 2008 are still undetermined though we hypothesize that this trend represents the aggregation of solo and small practices into larger entities, such as PCMHs, ACOs, independent physician associations, and hospital systems. Within MEPS, the addition of the probing question to identify individual providers within facilities may have contributed to the increase, although we are unable to calculate the magnitude of its contribution.
While practice transformation has modernized primary care, there may be unintended consequences. To succeed in value‐based payment systems, practices have consolidated to achieve economies of scale (Fleming et al. 2011; Peterson et al. 2015). This transition and the adoption of EHRs contribute to an increase in the percentage of time spent performing administrative tasks (Woolhandler and Himmelstein 2014). Concurrently, providers have moved away from solo and small practice in favor of practice models that allow for reduced hours and improved work‐life balance (Association of American Medical Colleges 2015). We hypothesize that these trends and the simultaneous economic downturn partially explain our findings.
Starfield famously outlined the essential features of primary care as (1) first‐contact care, (2) ongoing person‐focused care, (3) comprehensiveness, and (4) coordination of care (Starfield, Shi, and Macinko 2005). Whether today's facility USCs or person USCs are more successful at achieving these tasks, and the quadruple aim (lower costs, better population health, better experience of care, and better clinician satisfaction with care) is unknown. Integrating principles from the model known as direct primary care, such as keeping panel sizes low, may allow improved continuity with individual providers (Alexander, Kurlander, and Wynia 2005; Wu et al. 2010).
Limitations
There are several limitations that should be considered when interpreting our findings. First, as with any survey, our findings are subject to recall bias. Second, the type of USC is reported by the respondent, who may or may not have accurate information about a practice's organizational structure. However, we contend that the USC response is a reflection of how the respondent perceives the USC and the degree to which clinicians and facilities contribute to care delivery. For instance, the respondent could identify a person, not in a facility when, in reality, the provider is affiliated with a larger entity. If the respondent does not perceive that the facility provides any additional value, then his/her relationship with the provider will overshadow his/her relationship with the facility. Third, in an attempt to streamline the analysis, we did not distinguish between facility subtypes. These subtypes can include a wide range of organizational structures from PCMHs to community health centers. Fourth, there are factors that influence USC that have likely gone unmeasured, such as the uptake of high deductible insurance plans. Finally, to account for self‐selection bias, we included measures of health and utilization, which may incompletely capture variation in morbidity.
Future Studies
Future studies should assess whether USC type is associated with differences in quadruple aim outcomes. To distinguish between the wide variety of facility types, we recommend that the Agency for Healthcare Research and Quality increase the number of facility categories within MEPS and track facility ownership.
Conclusions
From 1996 to 2014, the percentage of people in the United States without a USC increased. The percentage of people who named a person as their USC has decreased and is now lower than the percentage reporting a facility as their USC. Those reporting a Person, in Facility USC are trending up. We hypothesize that this migration toward facilities reflects the consolidation of clinicians into larger, more integrated organizations, a consequence of recent policies. These trends are associated with excess ED visits and hospital admissions. The size of the trend is sufficiently large as to have substantial effects on critical health policy goals and deserves monitoring and further assessment.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Methods for Calculating the Relative and Total Increase in Emergency Department Visits and Hospital Admissions Attributable to Usual Source of Care Changes, 1996–2014.
Table S2. Adjusted Percentage of Usual Source of Care (USC) Type, 1996–2014.
Figure S1. Algorithm for Categorizing the Usual Source of Care Types.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the American Academy of Family Physicians and the University of Colorado School of Medicine.
Disclosures: None.
Disclaimer: None.
References
- Agency for Healthcare Research and Quality . 2015. “Medical Expenditure Panel Survey Medical Provider Component Medical Organizations Survey (MOS)” [accessed on June 9, 2017]. Available at https://meps.ahrq.gov/survey_comp/misc_survey/mpc/2015/MOS_15.htm
- Agency for Healthcare Research and Quality and Quality . 2008. Medical Expenditure Panel Survey Provider Roster Section, October 16.
- Alexander, G. C. , Kurlander J., and Wynia M. K.. 2005. “Physicians in Retainer (‘Concierge’) Practice. A National Survey of Physician, Patient, and Practice Characteristics.” Journal of General Internal Medicine 20 (12): 1079–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of American Medical Colleges . 2015. The Complexities of Physician Supply and Demand: Projections from 2013 to 2025, May 22.
- Bindman, A. B. , Grumbach K., Osmond D., Vranizan K., and Stewart A. L.. 1996. “Primary Care and Receipt of Preventive Services.” Journal of General Internal Medicine 11 (5): 269–76. [DOI] [PubMed] [Google Scholar]
- Bliss, E. B. , Meyers D. S., Phillips R. L. Jr, Fryer G. E., Dovey S. M., and Green L. A.. 2004. “Variation in Participation in Health Care Settings Associated with Race and Ethnicity.” Journal of General Internal Medicine 19 (9): 931–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownlee, S. 2008. Overtreated. New York City, NY: Bloomsbury USA. [Google Scholar]
- Casalino, L. P. , Pesko M. F., Ryan A. M., Mendelsohn J. L., Copeland K. R., Ramsay P. P., Sun X., Rittenhouse D. R., and Shortell S. M.. 2014. “Small Primary Care Physician Practices Have Low Rates of Preventable Hospital Admissions.” Health Affairs 33: 10–1377. [DOI] [PubMed] [Google Scholar]
- Coller, R. J. , Klitzner T. S., Saenz A. A., Lerner C. F., Nelson B. B., and Chung P. J.. 2015. “The Medical Home and Hospital Readmissions.” Pediatrics 136 (6): e1550–60. [DOI] [PubMed] [Google Scholar]
- Collins, S. R. , Rasmussen P. W., Doty M. M., and Beutel S.. 2014. “Too High a Price: Out‐of‐Pocket Health Care Costs in the United States. Findings from the Commonwealth Fund Health Care Affordability Tracking Survey. September–October 2014.” Issue Brief (Commonwealth Fund) 29: 1–11. [PubMed] [Google Scholar]
- Collins, S. R. , Rasmussen P. W., Beutel S., and Doty M. M.. 2015. “The Problem of Underinsurance and How Rising Deductibles Will Make It Worse. Findings From the Commonwealth Fund Biennial Health Insurance Survey, 2014.” Issue Brief (Commonwealth Fund) 13: 1–20. [PubMed] [Google Scholar]
- Congressional Budget Office . 2014. Updated Estimates of the Effects of the Insurance Coverage Provisions of the Affordable Care Act, April 2014, May 26,
- Corbie‐Smith, G. , Flagg E. W., Doyle J. P., and O'Brien M. A.. 2002. “Influence of Usual Source of Care on Differences by Race/Ethnicity in Receipt of Preventive Services.” Journal of General Internal Medicine 17 (6): 458–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe, J. E. , Fryer G. E., Phillips R., and Green L.. 2003. “Receipt of Preventive Care Among Adults: Insurance Status and Usual Source of Care.” American Journal of Public Health 93 (5): 786–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe, J. E. , Tillotson C. J., Lesko S. E., Wallace L. S., and Angier H.. 2011. “The Case for Synergy between a Usual Source of Care and Health Insurance Coverage.” Journal of General Internal Medicine 26 (9): 1059–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVoe, J. E. , Tillotson C. J., Wallace L. S., Lesko S. E., and Pandhi N.. 2012. “Is Health Insurance Enough? A Usual Source of Care May Be More Important to Ensure a Child Receives Preventive Health Counseling.” Maternal and Child Health Journal 16 (2): 306–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovey, S. , Weitzman M., Fryer G., Green L., Yawn B., Lanier D., and Phillips R.. 2003. “The Ecology of Medical Care for Children in the United States.” Pediatrics 111 (5 Pt 1): 1024–9. [DOI] [PubMed] [Google Scholar]
- Fleming, N. S. , Culler S. D., McCorkle R., Becker E. R., and Ballard D. J.. 2011. “The Financial and Nonfinancial Costs of Implementing Electronic Health Records in Primary Care Practices.” Health Affairs (Project Hope) 30 (3): 481–9. [DOI] [PubMed] [Google Scholar]
- Fryer Jr, G. E. , Green L. A., Dovey S. M., Yawn B. P., Phillips R. L., and Lanier D.. 2003. “Variation in the Ecology of Medical Care.” Annals of Family Medicine 1 (2): 81–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green, L. A. , and Puffer J. C.. 2016. “Reimagining Our Relationships with Patients: A Perspective from the Keystone IV Conference.” Journal of the American Board of Family Medicine 29 (suppl 1): S1–11. [DOI] [PubMed] [Google Scholar]
- Grumbach, K. , Keane D., and Bindman A.. 1993. “Primary Care and Public Emergency Department Overcrowding.” American Journal of Public Health 83 (3): 372–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haber, S. G. , Wensky S. G., and McCall N. T.. 2016. “Reducing Inpatient Hospital and Emergency Room Utilization Among Nursing Home Residents The Role of Patient‐Provider Relationships.” Journal of Aging and Health 29: 1–29. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . 2013. Better Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Janke, A. T. , Brody A. M., Overbeek D. L., Bedford J. C., Welch R. D., and Levy P. D.. 2015. “Access to Care Issues and the Role of EDs in the Wake of the Affordable Care Act.” American Journal of Emergency Medicine 33 (2): 181–5. [DOI] [PubMed] [Google Scholar]
- Kangovi, S. , Barg F. K., Carter T., Long J. A., Shannon R., and Grande D.. 2013. “Understanding Why Patients of Low Socioeconomic Status Prefer Hospitals Over Ambulatory Care.” Health Affairs 32 (7): 1196–203. [DOI] [PubMed] [Google Scholar]
- Kim, K. , Jeon H., and Lee J.‐H.. 2017. “Having a Physician Rather Than a Place as a Usual Source of Care Would Be Better — From 2012 Korea Health Panel Data.” Journal of Korean Medical Science 32 (1): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, M. Y. , Kim J. H., Choi I. K., Hwang I. H., and Kim S. Y.. 2012. “Effects of Having Usual Source of Care on Preventive Services and Chronic Disease Control: A Systematic Review.” Korean Journal of Family Medicine 33 (6): 336–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambrew, J. M. , DeFriese G. H., Carey T. S., Ricketts T. C., and Biddle A. K.. 1996. “The Effects of Having a Regular Doctor on Access to Primary Care.” Medical Care 34 (2): 138–51. [DOI] [PubMed] [Google Scholar]
- Liaw, W. , Petterson S., Rabin D. L., and Bazemore A.. 2014. “The Impact of Insurance and a Usual Source of Care on Emergency Department Use in the United States.” International Journal of Family Medicine 2014: 842847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaw, W. , Jetty A., Petterson S., and Peterson L.. 2016. “Solo and Small Practices Are a Vital, Diverse Part of Primary Care.” Annals of Family Medicine 14: 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebhaber, A. , and Grossman J. M.. 2007. “Physicians Moving to Mid‐Sized, Single‐Specialty Practices.” Tracking Report/Center for Studying Health System Change 18: 1–5. [PubMed] [Google Scholar]
- O'Brien, G. M. , Stein M. D., Zierler S., Shapiro M., O'Sullivan P., and Woolard R.. 1997. “Use of the ED as a Regular Source of Care: Associated Factors beyond Lack of Health Insurance.” Annals of Emergency Medicine 30 (3): 286–91. [DOI] [PubMed] [Google Scholar]
- O'Malley, A. S. 2013. “After‐Hours Access To Primary Care Practices Linked with Lower Emergency Department Use and Less Unmet Medical Need.” Health Affairs 32 (1): 175–83. [DOI] [PubMed] [Google Scholar]
- Pancholi, M. 2004. “Statistical Brief #32: Reasons for Lacking a Usual Source of Care: 2001 Estimates for the U. S. Civilian Noninstitutionalized Population” [accessed on July 21, 2016]. Available at https://meps.ahrq.gov/data_files/publications/st32/stat32.shtml
- Patient‐Centered Primary Care Collaborative . 2007. Joint Principles of the Patient‐Centered Medical Home, May 18.
- Peterson, L. E. , Baxley E., Jaen C. R., and Phillips R. L.. 2015. “Fewer Family Physicians Are in Solo Practices.” Journal of the American Board of Family Medicine 28 (1): 11–2. [DOI] [PubMed] [Google Scholar]
- Phillips, R. L. , Dodoo M. S., Green L. A., Fryer G. E., Bazemore A. W., McCoy K. I., and Petterson S. M.. 2009. “Usual Source of Care: An Important Source of Variation in Health Care Spending.” Health Affairs (Project Hope) 28 (2): 567–77. [DOI] [PubMed] [Google Scholar]
- Schroeder, S. A. 2016. “Social Justice as the Moral Core of Family Medicine: A Perspective from the Keystone IV Conference.” Journal of the American Board of Family Medicine 29 (suppl 1): S69–71. [DOI] [PubMed] [Google Scholar]
- Sommers, B. D. , Buchmueller T., Decker S. L., Carey C., and Kronick R.. 2013. “The Affordable Care Act Has Led to Significant Gains in Health Insurance and Access to Care for Young Adults.” Health Affairs 32 (1): 165–74. [DOI] [PubMed] [Google Scholar]
- Sox, C. M. , Swartz K., Burstin H. R., and Brennan T. A.. 1998. “Insurance or a Regular Physician: Which Is the Most Powerful Predictor of Health Care?” American Journal of Public Health 88 (3): 364–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spatz, E. S. , Sheth S. D., Gosch K. L., Desai M. M., Spertus J. A., Krumholz H. M., and Ross J. S.. 2014. “Usual Source of Care and Outcomes Following Acute Myocardial Infarction.” Journal of General Internal Medicine 29 (6): 862–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield, B. , Shi L., and Macinko J.. 2005. “Contribution of Primary Care to Health Systems and Health.” Milbank Quarterly 83 (3): 457–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villani, J. , and Mortensen K.. 2013. “Nonemergent Emergency Department Use among Patients with a Usual Source of Care.” Journal of the American Board of Family Medicine 26 (6): 680–91. [DOI] [PubMed] [Google Scholar]
- Weber, E. J. , Showstack J. A., Hunt K. A., Colby D. C., and Callaham M. L.. 2005. “Does Lack of a Usual Source of Care or Health Insurance Increase the Likelihood of an Emergency Department Visit? Results of a National Population‐Based Study.” Annals of Emergency Medicine 45 (1): 4–12. [DOI] [PubMed] [Google Scholar]
- Woolhandler, S. , and Himmelstein D. U.. 2014. “Administrative Work Consumes One‐Sixth of U.S. Physicians’ Working Hours and Lowers Their Career Satisfaction.” International Journal of Health Services: Planning, Administration, Evaluation 44 (4): 635–42. [DOI] [PubMed] [Google Scholar]
- Wu, W. N. , Bliss G., Bliss E. B., and Green L. A.. 2010. “Practice Profile. A Direct Primary Care Medical Home: The Qliance Experience.” Health Affairs (Project Hope) 29 (5): 959–62. [DOI] [PubMed] [Google Scholar]
- Xu, K. T. 2002. “Usual Source of Care in Preventive Service Use: A Regular Doctor Versus a Regular Site.” Health Services Research 37 (6): 1509–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Methods for Calculating the Relative and Total Increase in Emergency Department Visits and Hospital Admissions Attributable to Usual Source of Care Changes, 1996–2014.
Table S2. Adjusted Percentage of Usual Source of Care (USC) Type, 1996–2014.
Figure S1. Algorithm for Categorizing the Usual Source of Care Types.


