Abstract
Objectives
To determine the prevalence of high patella in adult patients with knee pain, and to correlate patellar height with symptoms of patellar instability, episode of patellofemoral dislocation and anterior pain in the knee; and also verify the concordance correlation between the Insall-Salvati and Caton-Deschamps indices.
Method
Cross-sectional study analyzing the medical records of patients with knee pain, using lateral view knee radiographs with 30° degrees of flexion and computed tomography. The values of the Insall-Salvati index and the Caton-Deschamps index were used to determine the patellar height.
Results
A total of 756 records were analyzed, resulting in 140 knees studied, 39% men and 61% women. Both indices produced statistically significant associations for the occurrence of high patella and signs of instability and episodes of dislocation, but there was no significant association for anterior knee pain. The Kappa index obtained when analyzing the concordance correlation between the Insall-Salvati index and Caton-Deschamps index points to a regular association between them.
Conclusion
Patients with high patella present a higher prevalence of instability. Having a high patella has no significant relationship with the presence of anterior knee pain. The Insall-Salvati and Caton-Deschamps indices demonstrate a regular agreement on the presentation of patellar heights results.
Keywords: Patella, Patellar dislocations, Chondromalacia patellae, Pain
Resumo
Objetivos
Determinar a prevalência de patela alta em pacientes adultos portadores de dor no joelho, correlacionar a altura patelar com sintomas de instabilidade patelar e dor anterior no joelho. Verificar índice de concordância entre os índices de Insall-Salvati e Caton-Deschamps.
Métodos
Estudo de corte transversal, com análise de prontuários de pacientes portadores de dor no joelho e radiografias em perfil do joelho a 30° graus de flexão e tomografia computadorizada. Usadas as medidas do Índice de Insall-Salvati e Índice de Caton-Deschamps para determinar a altura patelar.
Resultados
Foram analisados 756 prontuários, 140 joelhos, 39% de homens e 61% de mulheres. Para ambos os índices obtivemos associações estatisticamente significantes para a ocorrência de patela alta e sinais de instabilidade patelar, entretanto não houve associação significativa para a dor anterior no joelho. O índice Kappa obtido para analisar a relação de concordância entre o Índice de Insall-Salvati e Caton-Deschamps aponta para uma associação regular entre eles.
Conclusão
Pacientes portadores de patela alta apresentam maior prevalência de instabilidade na população estudada. Ter patela alta não apresenta relação significativa com a presença de dor anterior do joelho. Os Índices de Insall-Salvati e Caton-Deschamps apresentam concordância regular na apresentação dos resultados das alturas patelares.
Palavras-chave: Patela, Luxação da patela, Condromalácia patelar, Dor
Introduction
Patellofemoral pathology manifests itself in different clinical entities and may range from anterior knee pain (AKP) to patellofemoral instability (PFI).1 PFI is a common lesion that affects young and active individuals in most cases, accounting for 3% of all knee injuries.2
Among the anatomical alterations that affect the knee joint, patella alta (PA) is the one that is most associated with instability and recurrent dislocation. Lateral dislocation of the patella frequently occurs during the initial moment of the knee flexion movement, since the patella is less stable in the first degrees of flexion before it is accommodated more congruently in the trochlea.3 Given the importance of this condition, there are reports of over 100 procedures that aimed to treat and/or prevent PFI.3, 4
Despite the wide scientific production on painful knee syndromes, recent studies have described lesioned structures after patellar dislocation as well as the contribution of these structures to the control of physiological knee movement.4 Biomechanical studies have demonstrated that PA is one of the most important factors predisposing to PFI and AKP.1
This study is aimed at determining the prevalence of PA in adult patients with knee pain, to correlate patellar height with symptoms of PFI and of AKP for each index, and by verifying the agreement between the Insall-Salvati5 and Caton-Deschamps6 indices.
Material and methods
This is a cross-sectional study with a sample of patients medical records who were followed-up at two outpatient clinics specialized in knee disorders from January 1, 2015 to December 31, 2015. Patients with specific complaints of AKP and PFI were selected. The presence of AKP described in medical records, the existence of a lateral view radiograph of the affected knee, and computed tomography (CT) was verified. In each radiograph, the knee flexion angle was measured using a 20-cm goniometer (Promedix®). These images were studied using the Dicom Image Viewer® (Pixelmed) image metric analysis software, in accordance with the physical examination technique for the measurement of patellar heights from the Insall-Salvati5 and Caton-Deschamps indexes.6 TT-TG distance, patellar height, trochlear groove angle, and supratrochlear spur measurement were evaluated with the help of the institution's radiologist, who followed the protocol for cases of patellar instability and AKP. Patellar height was measured through two indices in patients with 30° angulation. The Insall-Salvati Index5 was measured by the ratio between the length of the patellar ligament (LT) and the size of the patella (LP). The Caton-Deschamps index6 was measured by the ratio between the length of the distance from the lower edge of the patellar articular surface to the anterosuperior tibial angle (AT) and the length of the patellar articular surface (PA).7 The authors complied with the requirements of Resolution 466/2012 and other CONEP standards and resolutions. The project of this study was submitted to and approved by the Research Ethics Committee under opinion No. 45551315.7.0000.0049. In the results of this study, the patients’ name or medical record number, as well as the name of the attending physicians, were not identified. Data were recorded on an Excel® worksheet and analyzed using Graphpad Prism 6 Trial® software. The Pearson's chi-squared test (χ2) was used for qualitative variables. In these analyses, the probability of type I error <5% (p < 0.05) was considered significant. To evaluate the degree of agreement, the Kappa index was applied, whose values have the following correspondences: 0, null or poor agreement; >0 to 0.20, low agreement; from to 0.21 to 0.40, regular agreement; from 0.41 to 0.60, fair agreement; from 0.61 to 0.80, good agreement; and from 0.81 to 1, excellent agreement.
Results
A total of 756 patients medical records were evaluated in two outpatient clinics specialized in knee symptoms. Of these, 644 were excluded due to the absence of radiographs or inadequacy of the knee flexion angle when the image was obtained, lack of relevant clinical data for the study, and appointments due to complaints in other joints despite the fact that the outpatient clinics are intended for patients with pathologies of the knee. After the exclusion criteria, 112 records were considered possible totaling 140 knees to be analyzed.
Male subjects (44) represented 39% of the sample, with a mean age of 50.27 years. Of these, the right knee was affected in 50% of the sample and 50% the left; 62% had AKP and 35% had PFI. Female patients (68) represented 61% of the sample, with a mean age of 52.18 years. The right knee was affected in 48% of the sample, and 52% the left; 69% had AKP and 25% had PFI.
Correlation measurements between the patellar heights and gender of the patients were calculated for each proposed index. For the Insall-Salvati index,5 a weak association was observed between these variables (chi-squared = 0.40, p > 0.81); the Caton-Deschamps index6 presented a similar value for this correlation (chi-squared = 0.36, p > 0.85).
Fig. 1 shows the absolute frequency of patellar heights according to the Insall-Salvati index5: 94 presented normal height, 40 had PA, and six presented low patellar height; in the Caton-Deschamps index,6 124 presented normal height, 12 had PA and presented low patellar height.
Fig. 1.
Absolute frequency of patellar height per index.
The correlations between the Insall-Salvati index5 and the AKP and PFI variables were assessed. A weak association and statistically significant dispersion were observed regarding patellar height and the occurrence of AKP (chi-squared = 2.32, p > 0.3); for the relationship between patellar height and signs of PFI, the association was statistically significant (chi-squared = 7.80, p < 0.02).
Fig. 2 presents the percentage distribution of the variables AKP and PFI according to the patellar heights obtained by the Insall-Salvati index.5 Among the patients with AKP, 30 (32.4%) had PA, 60 (64.4%) had normal patellar height, and three (3.2%) presented low patellar height. For those with PFI, 18 (45%) had PA, 20 (50%) had normal patellar height, and two (5%) presented low patellar height.
Fig. 2.
Percentage distribution of variables in the Insall-Salvati index.5
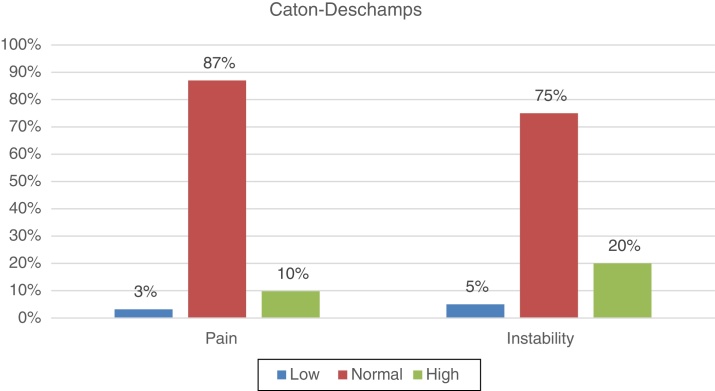
Likewise, the correlations between the Caton-Deschamps Index6 and the AKP and PFI variables were obtained. A weak correlation was observed between AKP and patellar height (chi-squared = 0.59, p > 0.74); PFI and patellar height were significantly correlated (chi-squared = 10.5, p < 0.005).
Fig. 3 presents the percentage distribution of the variables AKP and PFI according to the patellar heights obtained by the Caton-Deschamps index.6 Among the patients with AKP, nine (10%) had PA, 81 (87%) had normal patellar height, and three (3%) presented low patellar height. For those with PFI, eight (20%) had PA, 30 (75%) had normal patellar height, and two (5%) presented low patellar height.
Fig. 3.
Percentage distribution of the variables in the Caton-Deschamps index.6
The statistical analysis using the Kappa index to access the agreement between the results of measurements of the patellar heights obtained by the two indices proposed in this study presented a result of k = 0.36 (p < 0.001), which indicates a fair agreement between the Insal-Salvati5 and Caton-Deschamps indices.6
Discussion
In most studies researched, the majority of AKP patients were female.8, 9, 10, 11, 12, 13, 14 The present study corroborates this finding, as 60.3% of the sample were female. In addition, PFI and AKP symptoms were found to be more prevalent in women, but the difference between this prevalence in males and females was not statistically significant. Among the studied parameters, only patellar dislocation episodes presented an equivalent prevalence (4%) between genders; this data is in agreement with other studies, which indicates a greater number of cases in female patients.
In the present study, no statistically significant difference was observed in the relationship of patellar height obtained by the two proposed indices and gender; both presented similar absolute results for PA and normal or low patellar height. Although some studies indicate that women have higher patellar height than men, in the analyzed population no correlation between the patellar height and gender was observed. Insall and Salvatti,5 in the classic 1971 study in which they described the technique for measuring indices, also did not observe a statistically significant difference between genders and their patellar heights.
Symptoms of joint instability are frequent findings in patients with patellar height alterations. PA has been shown to be an important factor that favors this complaint. In 1994, in a series of 435 knees that underwent surgery due to instability symptoms, Dejour et al.1 reported that 77% had PA according to the Caton-Deschamps index,6 and no evidence of PA was observed in their control group. According to the data presented, in the present study the correlation between PFI and patellar height calculated with both the Insall-Salvati index (p < 0.02) and the Caton-Deschamps index (p < 0.02) was statistically significant, which strengthens the hypothesis set forth by Dejour et al.1 that PA is the primary factor in PFI.
Although some authors indicate a close relationship between the episodes of dislocation and PA, according to other recent biomechanical studies and the present findings, the authors believe that PA alone is not sufficient to provoke episodes of dislocation in the absence of soft tissue deficiency.2 In the present series, the authors found data with statistical significance that tended toward 0, which points to the relationship of the PA in the Insall-Salvati5 (p < 0.009) and Caton-Deschamps6 (p < 0.005) indices and in episodes of patellar dislocation.
Biomechanical analyzes have indicated that PA is a major factor in the onset of patellofemoral chondropathy and AKP.15, 16 Despite the characteristic symptomatology of AKP in these cases, in the present study a weak statistical correlation was observed between these two parameters, both for the correlation of patellar height with the Insall-Salvati index5 and with the Caton-Deschamps index,6 p < 0.3 and <0.74, respectively. This finding confirms previous studies that discourage surgical treatment that aims in correcting patellar height exclusively for treating patients with AKP.17, 18, 19 Evidence indicates that a rehabilitation protocol based on muscular balance of the entire lower limb presents satisfactory results in pain control and improvement of the functionality of patients with isolated AKP.20, 21, 22 The analysis of the biomechanical alterations of the lower limbs in patients with AKP is the most important focus for symptom improvement.22
The Insall-Salvati5 and Caton-Deschamps6 indices for evaluating patellar height have been used in a large part of the studies that have aimed at analyzing the biomechanics of the patellofemoral joint. However, there is no consensus on the levels of agreement between the results found for each measurement.23, 24
In the present sample, a regular agreement level was observed between patellar height results obtained using the Insall-Salvati5 and Caton-Deschamps6 indices.
Conclusion
In the population evaluated in this study, patients with PA presented a higher prevalence of patellofemoral instability, despite the lack of correlation between PA and AKP. The Insall-Salvati and Caton-Deschamps indices presented a regular agreement regarding patellar height results.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Clínica Ortopédica Traumatológica (COT), Salvador, BA, Brazil.
References
- 1.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2(1):19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 2.Koh J.L., Stewart C. Patellar instability. Orthop Clin North Am. 2015;46(1):147–157. doi: 10.1016/j.ocl.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 3.Greiwe R.M., Saifi C., Ahmad C.S., Gardner T.R. Anatomy and biomechanics of patellar instability. Oper Tech Sports Med. 2010;18(2):62–67. [Google Scholar]
- 4.Atkin D.M., Fithian D.C., Marangi K.S., Stone M.L., Dobson B.E., Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472–479. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- 5.Insall J., Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 6.Caton J., Deschamps G., Chambat P., Lerat J.L., Dejour H. Patella infera. A propos of 128 cases. Rev Chir Orthopédique Réparatrice Appar Mot. 1982;68(5):317–325. [PubMed] [Google Scholar]
- 7.Phillips C.L., Silver D.A., Schranz P.J., Mandalia V. The measurement of patellar height: a review of the methods of imaging. J Bone Joint Surg Br. 2010;92(8):1045–1053. doi: 10.1302/0301-620X.92B8.23794. [DOI] [PubMed] [Google Scholar]
- 8.Ghanem I., Wattincourt L., Seringe R. Congenital dislocation of the patella. Part I: pathologic anatomy. J Pediatr Orthop. 2000;20(6):812–816. doi: 10.1097/00004694-200011000-00023. [DOI] [PubMed] [Google Scholar]
- 9.Buchner M., Baudendistel B., Sabo D., Schmitt H. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med. 2005;15(2):62–66. doi: 10.1097/01.jsm.0000157315.10756.14. [DOI] [PubMed] [Google Scholar]
- 10.Fithian D.C., Nomura E., Arendt E. Anatomy of patellar dislocation. Oper Tech Sports Med. 2001;l.9(3):102–111. [Google Scholar]
- 11.Fithian D.C., Paxton E.W., Stone M.L., Silva P., Davis D.K., Elias D.A. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 12.Dejour D., Le Coultre B. Osteotomies in patello-femoral instabilities. Sports Med Arthrosc. 2007;15(1):39–46. doi: 10.1097/JSA.0b013e31803035ae. [DOI] [PubMed] [Google Scholar]
- 13.Palmu S., Kallio P.E., Donell S.T., Helenius I., Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–470. doi: 10.2106/JBJS.G.00072. [DOI] [PubMed] [Google Scholar]
- 14.Chotel F., Bérard J., Raux S. Patellar instability in children and adolescents. Orthop Traumatol Surg Res. 2014;100(1 Suppl.):S125–S137. doi: 10.1016/j.otsr.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 15.Marks K.E., Bentley G. Patella alta and chondromalacia. J Bone Joint Surg Br. 1978;60(1):71–73. doi: 10.1302/0301-620X.60B1.627582. [DOI] [PubMed] [Google Scholar]
- 16.Lancourt J.E., Cristini J.A. Patella alta and patella infera. Their etiological role in patellar dislocation, chondromalacia, and apophysitis of the tibial tubercle. J Bone Joint Surg Am. 1975;57(8):1112–1115. [PubMed] [Google Scholar]
- 17.Lan T.Y., Lin W.P., Jiang C.C., Chiang H. Immediate effect and predictors of effectiveness of taping for patellofemoral pain syndrome: a prospective cohort study. Am J Sports Med. 2010;38(8):1626–1630. doi: 10.1177/0363546510364840. [DOI] [PubMed] [Google Scholar]
- 18.Hunter D.J., Harvey W., Gross K.D., Felson D., McCree P., Li L. A randomized trial of patellofemoral bracing for treatment of patellofemoral osteoarthritis. Osteoarthritis Cartilage. 2011;19(7):792–800. doi: 10.1016/j.joca.2010.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCarthy M.M., Strickland S.M. Patellofemoral pain: an update on diagnostic and treatment options. Curr Rev Musculoskelet Med. 2013;6(2):188–194. doi: 10.1007/s12178-013-9159-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang S.N., Bates B.T., Dufek J.S. Contributions of lower extremity joints to energy dissipation during landings. Med Sci Sports Exerc. 2000;32(4):812–819. doi: 10.1097/00005768-200004000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Earl J.E., Hoch A.Z. A proximal strengthening program improves pain, function, and biomechanics in women with patellofemoral pain syndrome. Am J Sports Med. 2011;39(1):154–163. doi: 10.1177/0363546510379967. [DOI] [PubMed] [Google Scholar]
- 22.Crossley K., Bennell K., Green S., Cowan S., McConnell J. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30(6):857–865. doi: 10.1177/03635465020300061701. [DOI] [PubMed] [Google Scholar]
- 23.Seyahi A., Atalar A.C., Koyuncu L.O., Cinar B.M., Demirhan M. Blumensaat line and patellar height. Acta Orthop Traumatol Turc. 2006;40(3):240–247. [PubMed] [Google Scholar]
- 24.Seil R., Müller B., Georg T., Kohn D., Rupp S. Reliability and interobserver variability in radiological patellar height ratios. Knee Surg Sports Traumatol Arthrosc. 2000;8(4):231–236. doi: 10.1007/s001670000121. [DOI] [PubMed] [Google Scholar]