Abstract
Background
Suicide in young people is one of most common cause of death; and deliberate self-harm (DSH) is important indicator of suicide. It is currently unclear how old the rate begins to increase or when it reaches to the same level with adults. The purpose of this study was to find beginning age of DSH and compare their characteristics with adults.
Methods
This study retrospectively reviewed 5 years of nationwide prospective registry named Emergency Department-based Injury In-depth Surveillance (EDIIS) registry composed of all injured patients who were admitted to twenty tertiary university hospital emergency departments. Injured patients aged 29 years or younger from January 1, 2011 to December 31, 2015 were included. Incidence rate of DSH in all age was described. Patients were stratified by age: early teenage (11–15 years), late teenage (16–19 years), and early adulthood (20–29 years). Data of early teenage group were compared to those of other groups for examining their characteristics.
Results
Among 588,549 injury patients, 8,400 patients reported DSH. The rate began to rise at age 11 and reach at age 16 which was equivalent to that of age 20 to 29. Early teenage had significantly higher excess mortality ratio based injury severity score (EMR-ISS) and had almost same level without significant difference in operation incidence or mortality compared to late teenage and early adulthood.
Conclusion
DSH rate began to rise at age 11, reaching adulthood level at age 16 in Korea.
Keywords: Suicide, Deliberate Self-harm, Self-harm, Teenage, Young People
Graphical Abstract
INTRODUCTION
Suicide in young people is one of major public health issues. Suicide is the second most common cause of death in young people worldwide.1 Adolescent suicide is also the most critical continuous health problem in Korea. Since 2001, suicide rate of Korea has not dropped under the secondary common cause of death among teenage adolescents with a rate of 7.2 person per 100,000 in 2014.2,3
Deliberate self-harm (DSH) is intentional self-poisoning or self-injury, irrespective of type of motive or the extent of suicidal intent.1,4,5 DSH is one important predictor of completed suicide.6,7,8,9,10 Risk of suicide increases 50 to 100 times within the first 12 months after an episode of self-harm compared to that in the general population.7,11 Exposure to self-harm and suicide of others (family and friends) is associated with young people self-harm because others' self-harm might provide behavioral model for immature adolescents.12,13,14 DSH is also important risk factor for multiple substance dependence syndrome in adulthood.15
It is well established that rates of suicide and suicide-related behaviors are generally increased with age in adolescents.16,17,18 However, there are few studies about DSH in early teenage (ET) under age 12 due to limited sample size or difficulty in estimating this age group.1,19 It is important to know the incidence and characteristics of DSH at all ages of young people because timely interventions can give us a chance to prevent its advancing to suicide.20 It could also help policy makers to provide appropriate prevention plan.
Therefore, the objective of this study was to identify self-harm incidence in ET under age 12 by reviewing a registry based on national surveillance database which included injury patients presented to emergency department (ED) during 5 years. Trends of prehospital characteristics and clinical information among different age groups were also examined and compared to those in adults to provide valuable clue to clinicians working on young people's mental health.
METHODS
National registry
Data from Emergency Department-based Injury In-depth Surveillance (EDIIS) database of Korea were retrospectively reviewed. EDIIS developed and operated by Korea Centers for Disease Control and Prevention (KCDC) is a nationwide injury database that includes all injured patients admitted to EDs across Korea. EDIIS database is a registry of all injured patients admitted to twenty university hospital EDs. This database has about 246 variables, including basic demographics, injury epidemiologic information, prehospital injury characteristics, initially assessed clinical findings at ED, diagnosis (coded by International Classification of Disease, Tenth Revision [ICD-10]), treatment in EDs, ED disposition, and patient outcome after admission. Primary information was acquired by physicians of each institution during their clinical practice and trained coordinators of EDIIS project who were assigned to each hospital. Physicians in ED get history from patients or caretaker and check the box of each variables in standardized injury registry. Coordinators collected data from the registry. Data from each ED were entered into a web-based database of KCDC. Quality improvement was conducted regularly by educating physician who works in ED for monthly rotation and getting feedback from KCDC to coordinators.
Selection of participants
Previous studies have examined age-related suicide and self-harm by dividing age according to their study objectives.16,21,22 Suicide report published by World Health Organization has grouped 15–29 years as “young adult.”23 Therefore, injured patients aged 29 years or younger among all cases registered in the EDIIS database from January 1, 2011 to December 31, 2015 were included in this study. Patients who were injured by assault or by unknown intention were excluded from this study. Those who had missing data for in-depth study variables were also excluded. Teenage adolescents were further divided into two groups stratified by age: 1) ET, 11 to 15 years; and 2) late teenage (LT), 16 to 19 years. Those who aged 20 to 29 were assigned into the group of early adulthood (EA).
Exposure
This study focused on cases of self-harm or suicide in young people. The variable “Intention of injury” in EDIIS registry was checked for all patients. DSH was defined as any non-fatal injury or poisoning reported by the patient or judged by a clinician to be self-inflicted, irrespective of whether there was an intention to die.12 According to the definition of self-harm, intention of injury in EDIIS registry was determined by ED physician who primarily took patient history.
Measurements and outcome
Self-harm incidence rate and 95% confidential interval (CI) were calculated for each age (0–29 years). Cut-off values where the rate of self-harm began to increase and reach the level of adults were determined. Primary outcome was self-harm rate according to age. Secondary outcome was comparison of characteristics of self-harm injury among age groups based on ET group, including demographic characteristics, prehospital information (such as ED visit date, ED visit time, ED visit method, injury place, and injury mechanism), and clinical information (such as patient risk factor for suicide, suicide history, mental status at the time of ED presentation, excess mortality ratio based injury severity score (EMR-ISS), ED disposition, mortality, and result after admission). Injury severity is measured by EMR-ISS from diagnosis; and mortality is calculated by combination of ED death and death after admission.
Statistical analysis
Continuous variables are expressed in average and standard deviation with 95% CIs while categorical variables are expressed in frequency and percentage. Frequency difference between two groups was examined using Pearson's χ2 analysis and Fisher's exact test. Average difference was examined using Student's t-test. P < 0.05 was considered statistically significant. Sensitivity analysis by even age division for three groups has done and appended for table (Appendixes 1, 2, 3). R version 3.4.0 (2017-04-21; R Foundation, Vienna, Austria) was used for all statistical analyses.
Ethics statement
This study was reviewed and approved by Institutional Review Board (IRB) of Samsung Medical Center (IRB No. SMC 2017-07-076). It satisfied requirements specified under the Ministerial Decree of Health and Welfare passed by the National Bioethics Committee. Informed consent was waived by IRB due to its retrospective nature.
RESULTS
Study population
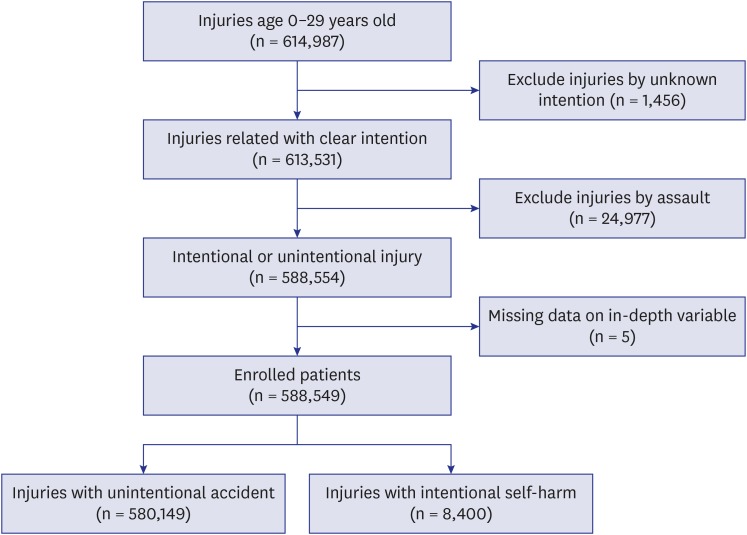
During the 5-year study period, a total of 614,987 patients under 30 years old with trauma cases were registered in the EDIIS database. The process to select our study subjected is shown in Fig. 1. Based on the inclusion and exclusion criteria of this study, a total of 588,549 patients were enrolled for final analysis. There were 8,400 total self-harm patients during the study period in age 0–29. The overall self-harm rate was 1.43%.
Fig. 1.
The flow diagram of the patients enrolled.
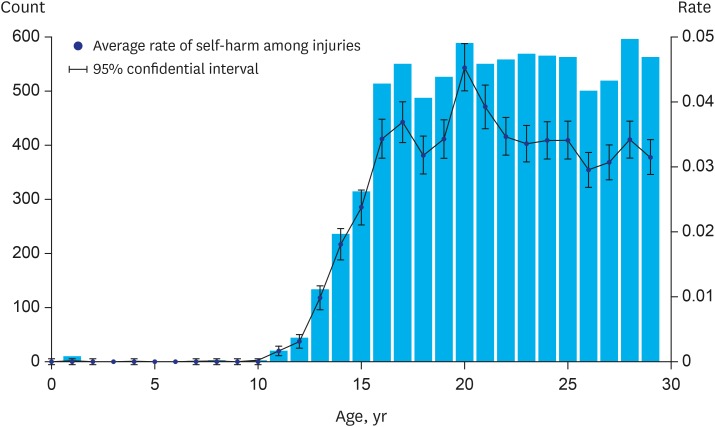
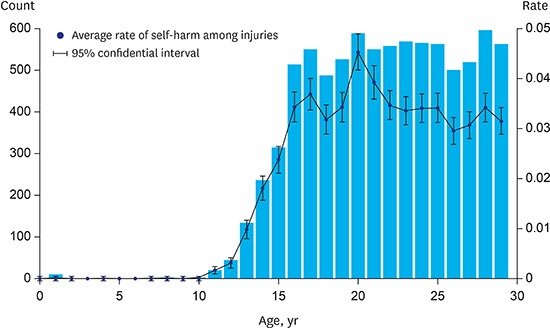
Self-harm incidence rate
The maximum DSH rate was observed at age 20 (5.16%; 95% CI, 4.75%–5.56%) while the lowest rate was at age 0 (0%). The rate began to rise at age 11 (0.18%; 95% CI, 0.10%–0.26%), reaching 3.89% (95% CI, 3.86%–3.92%) at age 16, which was equivalent to that at age 20 to 29 (3.91%; 95% CI, 3.48%–3.62%; P = 0.874) (Fig. 2).
Fig. 2.
Incidence rate of deliberate self-harm in all age of 0–29.
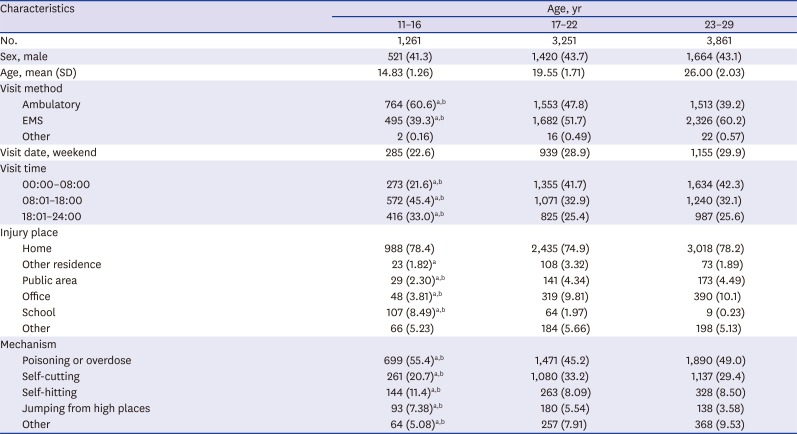
Injury characteristics
DSH patients were divided into three groups. Demographics and prehospital information of three groups are summarized in Table 1. There were 8,378 self-harm patients in three groups. Comparison was performed based on ET group (Table 2). There was no significant difference in sex proportion among three groups (P = 0.615). ED visit method, visit date, and visit time of ET group were significantly different from those of LT or EA group. ET group visited ED less frequently in the weekend than LT or EA group (ET vs. LT, 21.76% vs. 26.78%; P < 0.05 and ET vs. EA, 21.76% vs. 29.92%; P < 0.05, respectively). Self-harm method of the ET group was also significantly different from that of LT or EA group. ET group selected poisoning more than LT or EA group (ET vs. LT, 55.54% vs. 48.77%; P < 0.05 and ET vs. EA, 55.54% vs. 47.43%; P < 0.05, respectively). However, ET group (18.29%) had less (P < 0.05) self-cutting than LT or EA group (ET vs. LT, 18.29% vs. 28.81%; P < 0.05 and ET vs. EA, 18.29% vs. 31.41%; P < 0.05, respectively).
Table 1. Demographics and injury characteristics of overall injury.
| Characteristics | ET (11–15 yr) | LT (16–19 yr) | EA (20–29 yr) | Overall | |
|---|---|---|---|---|---|
| No. | 57,275 | 52,674 | 142,055 | 252,004 | |
| Sex, male | 41,752 (72.9) | 36,714 (69.7) | 84,210 (59.3) | 162,676 (64.6) | |
| Intention, self-harm | 749 (1.31) | 2,069 (3.93) | 5,555 (3.91) | 8,373 (3.32) | |
| Visit method | |||||
| Ambulatory | 48,074 (83.9) | 39,013 (74.1) | 109,999 (77.4) | 197,086 (78.2) | |
| EMS | 9,154 (16.0) | 13,593 (25.8) | 31,843 (22.4) | 54,590 (21.7) | |
| Other | 47 (0.10) | 68 (0.13) | 213 (0.14) | 328 (0.10) | |
| Visit date, weekend | 19,256 (33.6) | 18,784 (35.7) | 57,275 (40.3) | 95,315 (37.8) | |
| Visit time | |||||
| 00:00–08:00 | 3,976 (6.94) | 11,429 (21.7) | 41,143 (29.0) | 56,548 (22.4) | |
| 08:01–18:00 | 37,468 (65.4) | 23,692 (45.0) | 58,591 (41.2) | 119,751 (47.5) | |
| 18:01–24:00 | 15,831 (27.6) | 17,553 (33.3) | 42,321 (29.8) | 75,705 (30.0) | |
| Injury place | |||||
| Home | 15,030 (26.2) | 12,179 (23.1) | 34,504 (24.3) | 61,713 (24.5) | |
| Office | 2,228 (3.89) | 4,571 (8.67) | 18,774 (13.2) | 25,573 (10.1) | |
| Other | 12,829 (22.4) | 10,035 (19.1) | 33,045 (23.3) | 55,909 (22.2) | |
| Other residence | 384 (0.67) | 667 (1.26) | 2,318 (1.63) | 3,369 (1.34) | |
| Public area | 13,408 (23.4) | 18,797 (35.7) | 50,478 (35.5) | 82,683 (32.8) | |
| School | 13,396 (23.4) | 6,425 (12.2) | 2,936 (2.07) | 22,757 (9.03) | |
| Mechanism | |||||
| Collision | 18,280 (31.9) | 12,218 (23.2) | 25,433 (17.9) | 55,931 (22.2) | |
| Fall | 14,504 (25.3) | 10,998 (20.9) | 29,359 (20.7) | 54,861 (21.8) | |
| Other | 18,194 (31.8) | 22,116 (42.0) | 59,429 (41.8) | 99,739 (39.6) | |
| Poisoning | 784 (1.37) | 1,446 (2.75) | 4,430 (3.12) | 6,660 (2.64) | |
| Stabbing | 5,513 (9.63) | 5,896 (11.2) | 23,404 (16.5) | 34,813 (13.8) | |
Values are presented as number (%).
ET = early teenage, LT = late teenage, EA = early adulthood, EMS = emergency medical system.
Table 2. Demographics and injury characteristics of self-harm subject.
| Characteristics | ET (11–15 yr) | LT (16–19 yr) | EA (20–29 yr) | |
|---|---|---|---|---|
| No. | 749 | 2,069 | 5,555 | |
| Sex, male | 310 (41.4) | 898 (43.4) | 2,397 (43.2) | |
| Age, mean (SD) | 14.04 (1.04) | 17.49 (1.12) | 24.47 (2.90) | |
| Visit method | ||||
| Ambulatory | 463 (61.8)a,b | 1,120 (54.1) | 2,247 (40.5) | |
| EMS | 285 (38.1)a,b | 945 (45.7) | 3,273 (58.9) | |
| Other | 1 (0.13) | 4 (0.19) | 35 (0.63) | |
| Visit date, weekend | 163 (21.8)a,b | 554 (26.8) | 1,662 (29.9) | |
| Visit time | ||||
| 00:00–08:00 | 120 (16.0)a,b | 732 (35.4) | 2,410 (43.4) | |
| 08:01–18:00 | 359 (47.9)a,b | 758 (36.6) | 1,766 (31.8) | |
| 18:01–24:00 | 270 (36.1)a,b | 579 (28.0) | 1,379 (24.8) | |
| Injury place | ||||
| Home | 583 (77.8) | 1,597 (77.2) | 4,261 (76.7) | |
| Other residence | 11 (1.47) | 57 (2.75) | 136 (2.45) | |
| Public area | 15 (2.00)a,b | 75 (3.62) | 253 (4.55) | |
| Office | 28 (3.74)a,b | 146 (7.06) | 583 (10.5) | |
| School | 73 (9.75)a,b | 90 (4.35) | 17 (0.13) | |
| Other | 39 (5.21) | 104 (5.03) | 305 (5.49) | |
| Self-harm method | ||||
| Poisoning or overdose | 416 (55.5)a,b | 1,009 (48.8) | 2,635 (47.4) | |
| Self-cutting | 137 (18.3)a,b | 596 (28.8) | 1,745 (31.4) | |
| Self-hitting | 87 (11.6)b | 203 (9.81) | 445 (8.01) | |
| Jumping from high places | 63 (8.41)b | 134 (6.48) | 214 (3.85) | |
| Other | 46 (6.14)b | 127 (6.14) | 516 (9.29) | |
Values are presented as number (%).
ET = early teenage, LT = late teenage, EA = early adulthood, SD = standard deviation, EMS = emergency medical system.
aP < 0.05 for ET-LT; bP < 0.05 for ET-EA.
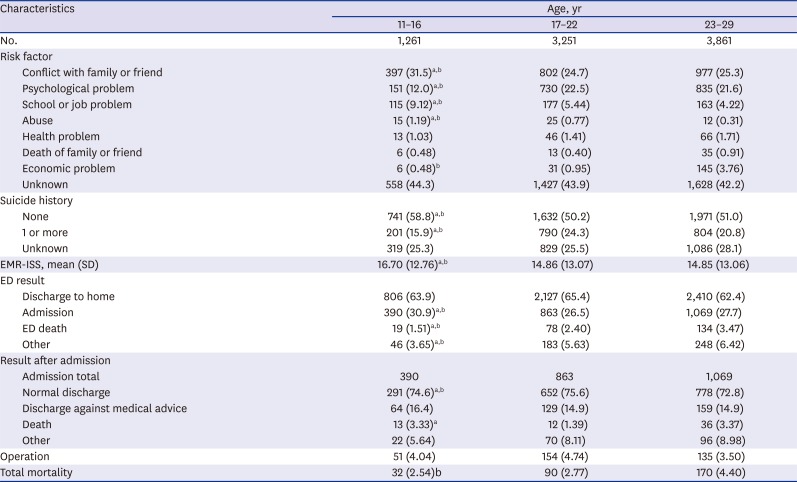
In-depth information and clinical outcome
Results of comparison of in-depth information and clinical outcome based on ET group are summarized in Table 3. Conflict with family or friends was the leading cause of DSH in all groups. Injury severity (17.17 ± 12.75) measured by EMR-ISS was significantly higher in the ET group compared to that in the other two groups. Mortality of the ET group was not significant different from that of LT or EA group (ET, 2.40%; LT, 2.75%; EA, 3.91%; ET vs. LT, P = 0.05 and ET vs. EA, P = 0.70, respectively). Substances used by self-poisoning patients are shown in Table 4. Almost half (43.75%) patients in the ET group used acetaminophen, which was significantly more than those in the other two groups.
Table 3. In-depth information and clinical outcome of self-harm patients.
| Characteristics | ET (11–15 yr) | LT (16–19 yr) | EA (20–29 yr) | |
|---|---|---|---|---|
| No. | 749 | 2,069 | 5,555 | |
| Risk factor | ||||
| Conflict with family or friend | 240 (32.0)a,b | 552 (26.7) | 1,384 (24.9) | |
| Psychological problem | 86 (11.5)a,b | 388 (18.8) | 1,242 (22.4) | |
| School or job problem | 70 (9.35)b | 151 (7.30) | 234 (4.21) | |
| Abuse | 10 (1.34)b | 15 (0.72) | 27 (0.49) | |
| Health problem | 9 (1.20) | 19 (0.92) | 97 (1.75) | |
| Death of family or friend | 2 (0.27) | 11 (0.53) | 41 (0.74) | |
| Economic problem | 1 (0.13)a,b | 19 (0.92) | 162 (2.92) | |
| Unknown | 331 (44.2) | 914 (44.2) | 2,368 (42.6) | |
| Suicide history | ||||
| None | 469 (62.6)a,b | 1,075 (52.0) | 2,800 (50.4) | |
| 1 or more | 100 (13.4)a,b | 469 (22.7) | 1,226 (22.1) | |
| Unknown | 180 (24.0)b | 525 (25.4) | 1,529 (27.5) | |
| EMR-ISS, mean (SD) | 17.17 (12.8)a,b | 15.13 (12.7) | 14.86 (13.2) | |
| ED result | ||||
| Discharge to home | 469 (62.6) | 1,361 (65.8) | 3,513 (63.2) | |
| Admission | 249 (33.2)a,b | 550 (26.6) | 1,523 (27.4) | |
| ED death | 9 (1.20)b | 48 (2.32) | 174 (3.13) | |
| Other | 22 (2.94)a,b | 110 (5.32) | 345 (6.21) | |
| Result after admission | ||||
| Admission total | 249 | 550 | 1,523 | |
| Normal discharge | 187 (75.1) | 419 (76.2) | 1,115 (73.2) | |
| Discharge against medical advice | 41 (16.5) | 80 (14.6) | 231 (15.2) | |
| Death | 9 (3.61) | 9 (1.64) | 43 (2.82) | |
| Other | 12 (4.82)b | 42 (7.64) | 134 (8.80) | |
| Operation | 29 (3.87) | 90 (4.35) | 221 (3.98) | |
| Total mortality | 18 (2.40) | 57 (2.75) | 217 (3.91) | |
Values are presented as number (%).
ET = early teenage, LT = late teenage, EA = early adulthood, EMR-ISS = excess mortality ratio based injury severity score, SD = standard deviation, ED = emergency department.
aP < 0.05 for ET-LT; bP < 0.05 for ET-EA.
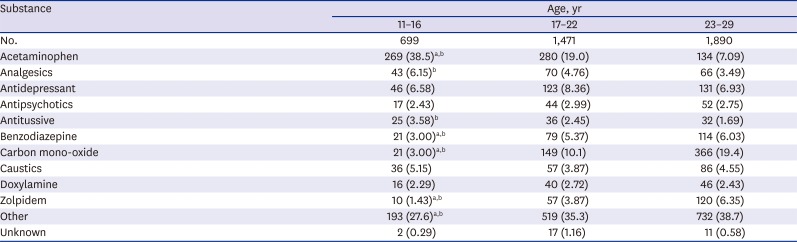
Table 4. Comparison for substance using self-poisoning.
| Substance | ET (11–15 yr) | LT (16–19 yr) | EA (20–29 yr) |
|---|---|---|---|
| No. | 416 | 1,009 | 2,635 |
| Acetaminophen | 182 (43.8)a,b | 268 (26.6) | 233 (8.84) |
| Analgesics | 26 (6.25)b | 59 (5.85) | 94 (3.57) |
| Antidepressant | 26 (6.25) | 65 (6.44) | 209 (7.93) |
| Antipsychotics | 8 (1.92) | 31 (3.07) | 74 (2.81) |
| Antitussive | 13 (3.13) | 35 (3.47) | 45 (1.71) |
| Benzodiazepine | 11 (2.64)b | 38 (3.77) | 165 (6.26) |
| Carbon mono-oxide | 12 (2.88)a,b | 75 (7.43) | 449 (17.0) |
| Caustics | 19 (4.57) | 43 (4.26) | 117 (4.44) |
| Doxylamine | 7 (1.68) | 24 (2.38) | 71 (2.69) |
| Zolpidem | 7 (1.68)b | 26 (2.58) | 154 (5.84) |
| Other | 104 (25.0)a,b | 335 (33.2) | 1,005 (38.1) |
| Unknown | 1 (0.24) | 10 (0.99) | 19 (0.72) |
Values are presented as number (%).
ET = early teenage, LT = late teenage, EA = early adulthood.
aP < 0.05 for ET-LT; bP < 0.05 for ET-EA.
DISCUSSION
Most previous studies on self-harm have used samples presenting to general hospitals9,12,24,25 or surveys usually from school-based community.26,27,28,29 Because only about one in eight adolescents would present to hospital after self-harm,27 there were some variations in results about characteristics of adolescent self-harm according to study design. In addition, few studies have studied subjects under age 12 years due to small sample size and difficulty in estimation. For these reasons, self-harm is known to be uncommon in young people under 12 years old.1,24
This study used large size samples from ED based injury registry and found that DSH rate began to elevate at age 11. The rate increased onward, reaching plateau (level of EA) at age 16. Age 11 found in this study was earlier than those reported in previous studies.1,30 Several reasons might account for this result in social context. First, bullying in elementary school is a common recent social problem in Korea.31 Our study showed that relation problem and school problem were more significant and common risk factors of DSH in ET with to other age groups. This may have resulted in more DSH at earlier age. Second, relationship between academic stress and suicide might be another reason.32 Intensive private education in Korea usually starts at low grade of elementary school. This might have caused high pressure to have academic achievement, thus affecting ET.
Another interesting finding of this study was that the female to male ratio was not significantly different among groups (ET, LT, and EA). This is incompatible with results from previous studies in western countries showing that female to male ratio tends to be high in ET group. It is then decreased with increasing age.24,33 Such difference may be due to cultural difference. This might also be due to methodological difference since this study was based on injury surveillance system rather than a survey.
The most frequent method of DSH in ET was self-poisoning or overdose. This is consistent with results of previous studies showing that ET have higher rates of self-poisoning than adolescents taken as a whole.12,22 The most common substance used in self-poisoning in ET was acetaminophen. In the late 1990s, self-poisoning by using acetaminophen brought out legislation to limit the number of analgesic tablets per pack sold over the counter.34 The regulation has been successful in reducing fatal liver failure after self-poisoning.35 Results of our study revealed that acetaminophen and analgesics were still frequent substances used for self-poisoning. Additional step should be considered to regulate their accessibility to acetaminophen and analgesics.
Clinical outcome related in-depth variables such as operation incidence and mortality rate in ET were not significantly different from those in LT or EA. EMR-ISS in ET was found to be significantly higher than that in the other two groups. This result may be due to impulsive response which plays a critical role in suicide of younger population.36 Considering the continuity of self-harm and suicide, recognizing risk group early with close observation after ED presentation is important to prevent tragedy in this age group.
Repetition of DSH is also frequent in adolescents.37 Even though suicidal history is uncommon in ET, the risk of suicide after self-harm is approximately 10 times more frequent than expected.38 Multidisciplinary treatment is important for ET in ED. After discharge, close follow up is needed to prevent sequential suicidal attempt. Upstream suicide prevention prior to the onset of suicidal behavior has been proven to have strong potential to reduce youth suicide rates.36
Strengths of our study is that this is a large ED-based nationwide study on DSH with few missing data. To the best of our knowledge, this study has the largest sample size in Asia. Our results gave us some clues on proper intervention timing for young people suicide. Moreover, our results on suicide rates in Korea might provide powerful information for other countries where it is difficult to gather large samples of self-harm patient due to low incidence.
This study also has some limitations. First, because data used for this study were surveillance data of patients from participating hospitals, there might be sampling bias. However, participating hospitals located in 13 of 17 provinces in Korea. Therefore, sampling bias was minimized. Still, these university hospitals locate in urban area than in rural, there might be possibility of selection bias. Second, the registry included only patients who visited ED. Cases of successfully completed suicide or non-emergent injuries caused by self-harm might have been missed out, causing selection bias. This short-coming made it difficult to compare results of this study with death causes of national statistics directly.3 Third, the registry did not include follow up results of injured patients after being discharged from the hospital. Further study is needed to evaluate the long-term outcome such as 1-year survival or re-attempt of DSH.39 Fourth, there are significant amounts of unknown data. Although the sample size was large enough to produce statistically significant results, unknown data might have influenced the outcome in various ways. However, other studies on DSH have faced similar limitations due to the nature of DSH patients.27
In conclusion, DSH in adolescent began to increase at age 11, reaching adulthood level at age 16. The mortality of DSH in ET group was as high as that in older groups. The severity of self-harm was the highest in ET. Therefore, early education before elevation of self-harm at age 11 and timely intervention are needed to reduce the rapid increase of suicide in ET.
Appendix 1
Sensitivity test by even divided age for demographics and injury characteristics
Values are presented as number (%).
SD = standard deviation, EMS = emergency medical system.
aP < 0.05 between age 11–16 and age 17–22; bP < 0.05 between age 11–16 and age 23–29.
Appendix 2
Sensitivity test by even divided age for in-depth information and clinical outcome
Values are presented as number (%).
EMR-ISS = excess mortality ratio based injury severity score, SD = standard deviation, ED = emergency department.
aP < 0.05 between age 11–16 and age 17–22; bP < 0.05 between age 11–16 and age 23–29.
Appendix 3
Sensitivity test by even divided age for substance using self-poisoning
Values are presented as number (%).
aP < 0.05 between age 11–16 and age 17–22; bP < 0.05 between age 11–16 and age 23–29.
Footnotes
Funding: This research was supported by Samsung Medical Center. This research was supported by a fund by Research of Korea Centers for Disease Control and Prevention (2017).
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Jung KY, Cha WC. Data curation: Jung KY. Formal analysis: Jung KY, Cha WC. Methodology: Cha WC. Supervision: Kim T, Hwang SY, Lee TR, Yoon H, Shin TG, Cha WC, Jeon HJ. Validation: Kim T, Yoon H, Shin TG, Sim MS, Cha WC. Visualization: Jung KY, Shim MS. Writing - original draft: Jung KY. Writing - review & editing: Jung KY, Cha WC.
References
- 1.Hawton K, Saunders KE, O'Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379(9834):2373–2382. doi: 10.1016/S0140-6736(12)60322-5. [DOI] [PubMed] [Google Scholar]
- 2.Im Y, Oh WO, Suk M. Risk factors for suicide ideation among adolescents: five-year national data analysis. Arch Psychiatr Nurs. 2017;31(3):282–286. doi: 10.1016/j.apnu.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Lim D, Ha M, Song I. Trends in the leading causes of death in Korea, 1983–2012. J Korean Med Sci. 2014;29(12):1597–1603. doi: 10.3346/jkms.2014.29.12.1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Self-harm SK. Lancet. 2005;366(9495):1471–1483. doi: 10.1016/S0140-6736(05)67600-3. [DOI] [PubMed] [Google Scholar]
- 5.Sahlin H, Kuja-Halkola R, Bjureberg J, Lichtenstein P, Molero Y, Rydell M, et al. Association between deliberate self-harm and violent criminality. JAMA Psychiatry. 2017;74(6):615–621. doi: 10.1001/jamapsychiatry.2017.0338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85. doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- 7.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181(3):193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 8.Cooper J, Kapur N, Webb R, Lawlor M, Guthrie E, Mackway-Jones K, et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry. 2005;162(2):297–303. doi: 10.1176/appi.ajp.162.2.297. [DOI] [PubMed] [Google Scholar]
- 9.Hawton K, Bergen H, Cooper J, Turnbull P, Waters K, Ness J, et al. Suicide following self-harm: findings from the Multicentre Study of self-harm in England, 2000–2012. J Affect Disord. 2015;175:147–151. doi: 10.1016/j.jad.2014.12.062. [DOI] [PubMed] [Google Scholar]
- 10.Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C. Suicide following deliberate self-harm. Am J Psychiatry. 2017;174(8):765–774. doi: 10.1176/appi.ajp.2017.16111288. [DOI] [PubMed] [Google Scholar]
- 11.Hawton K, Fagg J. Suicide, and other causes of death, following attempted suicide. Br J Psychiatry. 1988;152(3):359–366. doi: 10.1192/bjp.152.3.359. [DOI] [PubMed] [Google Scholar]
- 12.Hawton K, Hall S, Simkin S, Bale L, Bond A, Codd S, et al. Deliberate self-harm in adolescents: a study of characteristics and trends in Oxford, 1990–2000. J Child Psychol Psychiatry. 2003;44(8):1191–1198. doi: 10.1111/1469-7610.00200. [DOI] [PubMed] [Google Scholar]
- 13.De Leo D, Heller TS. Who are the kids who self-harm? An Australian self-report school survey. Med J Aust. 2004;181(3):140–144. doi: 10.5694/j.1326-5377.2004.tb06204.x. [DOI] [PubMed] [Google Scholar]
- 14.O'Connor RC, Rasmussen S, Hawton K. Predicting deliberate self-harm in adolescents: a six month prospective study. Suicide Life Threat Behav. 2009;39(4):364–375. doi: 10.1521/suli.2009.39.4.364. [DOI] [PubMed] [Google Scholar]
- 15.Moran P, Coffey C, Romaniuk H, Degenhardt L, Borschmann R, Patton GC. Substance use in adulthood following adolescent self-harm: a population-based cohort study. Acta Psychiatr Scand. 2015;131(1):61–68. doi: 10.1111/acps.12306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diggins E, Kelley R, Cottrell D, House A, Owens D. Age-related differences in self-harm presentations and subsequent management of adolescents and young adults at the emergency department. J Affect Disord. 2017;208:399–405. doi: 10.1016/j.jad.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 17.Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry. 2002;1(3):181–185. [PMC free article] [PubMed] [Google Scholar]
- 18.Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, et al. Youth risk behavior surveillance - United States, 2011. MMWR Surveill Summ. 2012;61(4):1–162. [PubMed] [Google Scholar]
- 19.Sheftall AH, Asti L, Horowitz LM, Felts A, Fontanella CA, Campo JV, et al. Suicide in elementary school-aged children and early adolescents. Pediatrics. 2016;138(4):e20160436. doi: 10.1542/peds.2016-0436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greydanus DE, Bacopoulou F, Tsalamanios E. Suicide in adolescents: a worldwide preventable tragedy. Keio J Med. 2009;58(2):95–102. doi: 10.2302/kjm.58.95. [DOI] [PubMed] [Google Scholar]
- 21.Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L. Age- and sex-related risk factors for adolescent suicide. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1497–1505. doi: 10.1097/00004583-199912000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Olfson M, Gameroff MJ, Marcus SC, Greenberg T, Shaffer D. Emergency treatment of young people following deliberate self-harm. Arch Gen Psychiatry. 2005;62(10):1122–1128. doi: 10.1001/archpsyc.62.10.1122. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Preventing Suicide: A Global Imperative. Geneva: World Health Organization; 2014. [Google Scholar]
- 24.Hawton K, Harriss L. Deliberate self-harm by under-15-year-olds: characteristics, trends and outcome. J Child Psychol Psychiatry. 2008;49(4):441–448. doi: 10.1111/j.1469-7610.2007.01852.x. [DOI] [PubMed] [Google Scholar]
- 25.Kerfoot M. Deliberate self-poisoning in childhood and early adolescence. J Child Psychol Psychiatry. 1988;29(3):335–343. doi: 10.1111/j.1469-7610.1988.tb00721.x. [DOI] [PubMed] [Google Scholar]
- 26.Sourander A, Aromaa M, Pihlakoski L, Haavisto A, Rautava P, Helenius H, et al. Early predictors of deliberate self-harm among adolescents. A prospective follow-up study from age 3 to age 15. J Affect Disord. 2006;93(1-3):87–96. doi: 10.1016/j.jad.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 27.Madge N, Hewitt A, Hawton K, de Wilde EJ, Corcoran P, Fekete S, et al. Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) Study. J Child Psychol Psychiatry. 2008;49(6):667–677. doi: 10.1111/j.1469-7610.2008.01879.x. [DOI] [PubMed] [Google Scholar]
- 28.Stallard P, Spears M, Montgomery AA, Phillips R, Sayal K. Self-harm in young adolescents (12–16 years): onset and short-term continuation in a community sample. BMC Psychiatry. 2013;13(1):328. doi: 10.1186/1471-244X-13-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawton K, Rodham K, Evans E, Weatherall R. Deliberate self harm in adolescents: self report survey in schools in England. BMJ. 2002;325(7374):1207–1211. doi: 10.1136/bmj.325.7374.1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bresin K, Schoenleber M. Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. 2015;38:55–64. doi: 10.1016/j.cpr.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Yang SJ, Kim JM, Kim SW, Shin IS, Yoon JS. Bullying and victimization behaviors in boys and girls at South Korean primary schools. J Am Acad Child Adolesc Psychiatry. 2006;45(1):69–77. doi: 10.1097/01.chi.0000186401.05465.2c. [DOI] [PubMed] [Google Scholar]
- 32.Ang RP, Huan VS. Relationship between academic stress and suicidal ideation: testing for depression as a mediator using multiple regression. Child Psychiatry Hum Dev. 2006;37(2):133–143. doi: 10.1007/s10578-006-0023-8. [DOI] [PubMed] [Google Scholar]
- 33.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2001;40(4):427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 34.O'Rourke M, Garland MR, McCormick PA. Ease of access is a principal factor in the frequency of paracetamol overdose. Ir J Med Sci. 2002;171(3):148–150. doi: 10.1007/BF03170503. [DOI] [PubMed] [Google Scholar]
- 35.Hawton K, Simkin S, Deeks J, Cooper J, Johnston A, Waters K, et al. UK legislation on analgesic packs: before and after study of long term effect on poisonings. BMJ. 2004;329(7474):1076. doi: 10.1136/bmj.38253.572581.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bridge JA, Asti L, Horowitz LM, Greenhouse JB, Fontanella CA, Sheftall AH, et al. Suicide trends among elementary school-aged children in the United States from 1993 to 2012. JAMA Pediatr. 2015;169(7):673–677. doi: 10.1001/jamapediatrics.2015.0465. [DOI] [PubMed] [Google Scholar]
- 37.Hawton K, Fagg J, Simkin S, Bale E, Bond A. Deliberate self-harm in adolescents in Oxford, 1985–1995. J Adolesc. 2000;23(1):47–55. doi: 10.1006/jado.1999.0290. [DOI] [PubMed] [Google Scholar]
- 38.Hawton K, Harriss L. Deliberate self-harm in young people: characteristics and subsequent mortality in a 20-year cohort of patients presenting to hospital. J Clin Psychiatry. 2007;68(10):1574–1583. [PubMed] [Google Scholar]
- 39.Heerde JA, Toumbourou JW, Hemphill SA, Herrenkohl TI, Patton GC, Catalano RF. Incidence and course of adolescent deliberate self-harm in Victoria, Australia, and Washington State. J Adolesc Health. 2015;57(5):537–544. doi: 10.1016/j.jadohealth.2015.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]