Abstract
CONTEXT:
Infertility is one of the major stressful events in individual life, especially women. Self-efficacy means a person can perceive a potentially threatening and stressful situation as being amenable to influences of personal control.
AIMS:
This study was conducted to determine the acupressure effects on self-efficacy and pregnancy rate in infertile women under in vitro fertilization (IVF)/intracytoplasmic sperm injection treatment.
SETTINGS AND DESIGN:
This study was a randomized controlled trial in infertile women. It performed at Milad IVF Center, Mashhad, Iran, from September 2015 to August 2016.
MATERIALS AND METHODS:
The sample size was 144 participants. The participants were randomly divided into three groups: real and sham acupressure and control groups. Acupressure performed on the H7 and P6 acupoints on both the hands. The infertility self-efficacy scale was completed before and after intervention. Beta-human chorionic gonadotropin hormone assay was measured to determine pregnancy. Data analysis was done by Chi-square, Fisher's exact, paired sample t, Kruskal–Wallis, and ANOVA test and general linear model and multinomial logistic. Levels of significance were reported at P < 0.05.
RESULTS:
The mean age of women was 30.84 ± 5.34 years. The ovulation factor (P = 0.02) and spouse's job (P = 0.05) were statistically significant difference between the groups. The score of self-efficacy and frequency of clinical pregnancy were no significant difference among three groups. Using linear regression, only the score of primary self-efficacy (before intervention) was in a significant relationship with self-efficacy after the intervention (P < 0.001).
CONCLUSION:
To our results, we recommend more research for assessing acupressure effects on self-efficacy and clinical pregnancy rate in infertile women.
Keywords: Acupressure, infertility, pregnancy rate, self-efficacy, women
Introduction
Infertility is considered as an important stressor in the life, and insolvency, grief, depression, anxiety, sexual dysfunction, low self-esteem, and rejection from friends and community are undesirable consequences that most infertile couples experience.[1,2] This stressful event is suggested as a negative and frustrating event for couples, especially women.[3]
It is obvious that invasive procedures such as daily injections, frequent sampling of blood and sperm, and ultrasounds, and the imposed financial burden lead to a lot of stress. Although the couples try to adapt to the methods of treatment, the sufferings of some who do not have that ability for this match will be doubled.[4]
One of the worst aspects of stress associated with infertility is uncertainty about the future,[5] so 30% of couples unfinished the treatment process due to so much psychological pressure.[6,7]
The researchers believe that although infertility as a source of psychological pressure can endanger the health of an infertile person, the extent of its effect somewhat depends on cognitive evaluation and coping skills of a person.[5] One's belief in themselves and their abilities is very effective on the extent of anxiety which experiences in critical and risky conditions.
In infertile patients, self-efficacy is the patients’ perception of their abilities to use the psychological skills to control the emotions related to medical treatment of infertility. What is certain is that an infertile person with high self-efficacy gains more emotional stability and will be more insistent for treatment.[8,9]
A variety of nonpharmacological interventions are used in infertile or low fertile women.[10]
Acupressure principles are similar to acupuncture, with the difference that the needle is not used and the points of acupuncture are stimulated by finger pressure or special tools.[11,12]
In acupressure, it is believed that stimulation of certain points of the body balances the flow of vital energy and will remove the problem.[13,14] Kovárová et al., in an exploratory study, observed a significant increase in infertile women's self-efficacy after four sessions of treatment with acupuncture.[15] No study has been done on the effect of acupressure on self-efficacy in infertile women, and contradictory results had been obtained from the studies of the effect of acupuncture on the fertility rate. Cheong et al. did not observe any evidence of overall benefit of acupuncture on improving the rate of live birth;[16] while the systematic review and meta-analysis of Zheng et al. showed that the common clinical pregnancy rate of all acupuncture groups was significantly higher than control groups.[17] Therefore, the aim of this study was to determine the acupressure effects on self-efficacy and pregnancy rate in infertile women undergoing in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) treatment.
Materials and Methods
This randomized clinical trial study was performed from September 2015 to August 2016 in Milad Infertility Center, Mashhad, Iran. This study was a clinical trial with registration code IRCT 201506072924N2 and was approved by the Ethics Committee of Mashhad University of Medical Sciences with reference number IR.MUMS.REC.1394.313. The study population was infertile women undergoing IVF/ICSI treatment. The sample size was based on Smith et al.'s study and considering self-efficacy variable.[18] We used the formula of mean estimation in two independent groups to determine the sample size. With α set at 0.05 and power at 0.8, and considering 5%–10% probability of sample loss, a sample size of 144 participants was obtained. Inclusion criteria were individuals aged 20–45 years, Iranians, female or male infertility, primary infertility, and no history of using acupressure. Sampling method was purposefully based on the inclusion criteria. Then, the questionnaires of sociodemographic information and Persian version infertility self-efficacy (ISE) scale[19] were completed for them. ISE questionnaire has 16 items and has been designed by Cousineau et al., and its reliability and internal consistency have been confirmed by calculating the Cronbach's alpha coefficient (α = 0.94).[8] The scale of this questionnaire was Likert five options, with a score of 16–80 and no cutoff point, with more scores indicating more self-efficacy. In Jamshidimanesh et al.'s study, the validity and reliability of Persian translation of this questionnaire were examined, and its internal consistency reliability was α = 0.89 by the Cronbach's alpha coefficient.[19]
Exclusion criteria were unwillingness to continue the study. For women who were enrolled in the study after signing the informed consent, acupressure was performed and taught to them by the researcher. The researcher received the necessary training for acupressure through the acupuncturist. The samples were allocated into three groups using Fleiss randomized table:[20] real acupressure, sham acupressure, and control groups. Patients received acupressure treatment with IVF/ICSI treatments. The numbers of acupressure sessions were 12 sessions that four sessions were performed once a week by the researcher, and in coordination with the patient, the other eight sessions were done by the patient.
The points used for acupressure were P6 and H7 on both the hands which were pressed for up to 3 min. A criterion for proper performing of acupressure was feeling of heaviness in the area which was pressed. In the sham acupressure group, the improper points were used; these points were within 2 cm distance of the main points. The control group received only IVF/ICSI treatments. Acupressure was performed until a day before embryo transfer. Infertility ISE was completed at the end of intervention by participants to determine the effect of acupressure on ISE. Self-efficacy questionnaire was completed before and after intervention and up to 1 day before embryo transfer by infertile women. Pregnancy rate was assessed by determining the level of blood β-human chorionic gonadotropin (HCG) 16 days after embryo transfer. β-HCG scores of 50 or above indicate the pregnancy.
Statistical analysis
Data were analyzed by descriptive statistics including mean and standard deviation (SD) and inferential statistics such as Chi-square, Fisher exact, paired sample t, Kruskal–Wallis, and one-way ANOVA test and general linear model and multinomial logistic were used to determine the effect of confounding variables on self-efficacy. P < 0.05 was considered statistically significant. SPSS statistical software (Statistical Product and Services Solutions, version 16, SPSS Inc., Chicago, IL, USA) was used.
Results
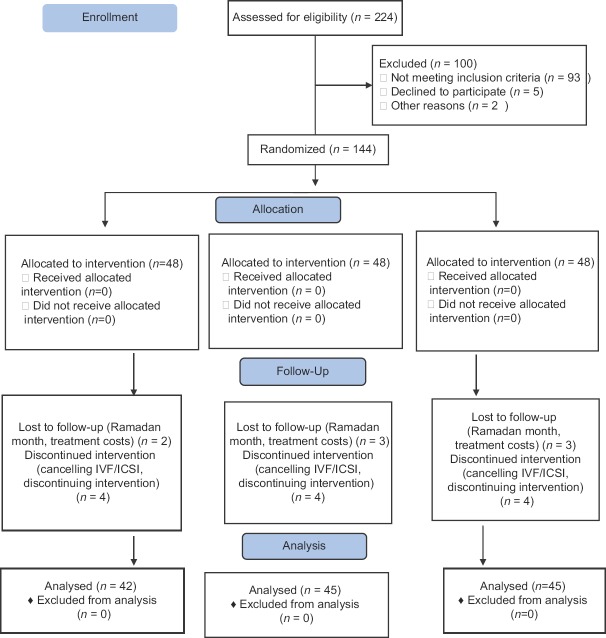
We assessed 224 infertile women for eligibility. A total of 144 participants were recruited into the study, and then, 12 participants were withdrawn from the study for various reasons (cancelling cycle, discontinuing intervention, costs, and Ramadan month). Finally, we performed data analysis on the 132 participants [Figure 1].
Figure 1.
Recruitment and participant flow through the trial based on consort diagram
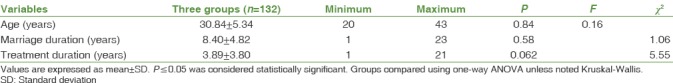
Most women (51, 35.5%) and their spouses (55, 38.2%) had university education. The job of most women (110, 77%) was homemakers and the job of majority of spouses (56, 39.5%) was self-employed. Other demographic characteristics of the women are showed in Table 1. Chi-square and Fisher exact tests were used to determine the frequency and percentage of nominal qualitative variables such as woman's job, spouse's job, cause of infertility, previous treatment methods, and treatment protocol before the intervention as the groups’ separated.
Table 1.
Sociodemographic characteristics in participants
According to the results, cause of infertility in terms of ovulation (P = 0.02) and spouse's job (P = 0.05) between groups had statistically significant relationship.
Values are expressed as mean ± SD. P ≤ 0.05 was considered statistically significant.
Groups were compared using one-way ANOVA unless noted Kruskal–Wallis test.
Kruskal–Wallis test was used to determine the qualitative variables such as educational level of women and spouse's education in the studied groups. Based on the results, no statistically significant relationship was observed between these variables in the studied groups.
Self-efficacy was normally distributed before (P = 0.35) and after (P = 0.09) the intervention. There was no statistically significant difference in self-efficacy before and after the intervention among three groups. No statistically significant difference was observed in the groups of real acupressure, sham acupressure, and control [Table 2].
Table 2.
Mean, standard deviation, and infertility self-efficacy changes in three groups
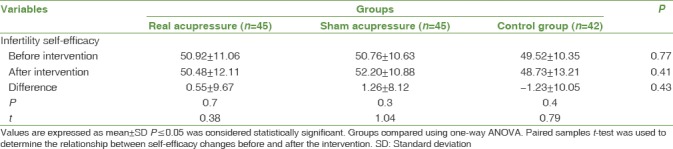
Values are expressed as mean ± SD. P ≤ 0.05 was considered statistically significant.
Groups were compared using one-way ANOVA. Paired samples t-test was used to determine the relationship between self-efficacy changes before and after the intervention.
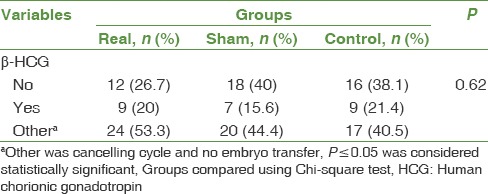
Three groups were similarly distributed in terms of pregnancy rate. No statistically significant difference was observed between the study groups and pregnancy rate [Table 3].
Table 3.
Pregnancy rate in all three groups
General linear model was used to determine the independent variables affecting the self-efficacy variable. The qualitative variables entered into the model included spouse's job, cause of infertility (male, ovulation, tubal), previous treatment methods (ovarian stimulation), and the study groups. The quantitative variables entered into the model included duration of treatment, and self-efficacy before the intervention. Then, we excluded variables that were P > 0.15 manually by backward method, and finally, the variables of groups, ovulation factor, and self-efficacy before the intervention remained. The real acupressure group had more self-efficacy than the control group but was not statistically significant (P = 0.27). The patients with no ovulation factor as the cause of infertility had more self-efficacy than those with ovulation factor but were not statistically significant (P = 0.15). The primary self-efficacy was effective on self-efficacy after the intervention so that primary self-efficacy (P < 0.001) was effective in reducing self-efficacy after the intervention. The duration of treatment had a significant relationship with the pregnancy rate; each 1 year increase in duration of treatment decreases the probability of pregnancy rate as 21% compared to no occurrence of pregnancy (P = 0.025, odds ratio = 0.79). The groups were not effective in pregnancy occurrence with adjustment of independent variables of treatment duration and the history of ovulation induction treatments. The patients who had a history of ovulation induction treatments than those who did not have, the possibility of being in the other situations (canceled cycles or lack embryo transfer) was decreased as 66% compared to no occurrence of pregnancy [Table 4].
Table 4.
Acupressure on self-efficacy and pregnancy rate and independent variables
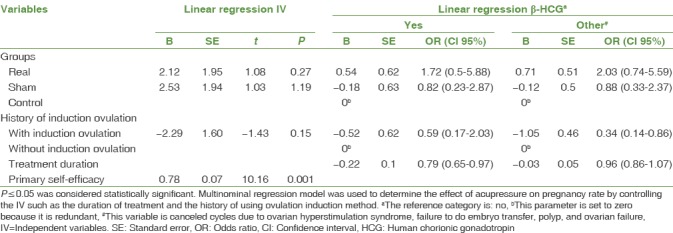
Multinominal regression model was used to determine the effect of acupressure on pregnancy rate by controlling the independent variables such as the duration of treatment and the history of using ovulation induction method.
Discussion
To the best of our knowledge, this is the first randomized controlled trial to determine the acupressure effect on ISE and pregnancy rate in infertile women undergoing IVF/ICSI treatment. The results of this study showed no significant difference in the studied groups in terms of self-efficacy before and after the intervention of acupressure and its changes. These findings were in contrast to the findings of the studies of Kovárová et al. and Smith et al.[15,18] The results of Kovárová et al.'s study showed that the total score of self-efficacy increased after four sessions of treatment with acupuncture compared to baseline score (P = 0.008).[15] Smith et al.'s study also showed improving ISE in the acupuncture group compared with the control group.[18] The two mentioned studies did not have the sham group in their studies; however, we had three groups (real acupressure, sham acupressure, and control groups) in our study.
Our results were in contrast with the results of the study by Pasha et al. They compared the pharmaceutical and the nonpharmaceutical strategies for improving ISE in infertile women. Their results showed that two groups of receiving cognitive-behavioral therapy and fluoxetine had more mean ISE than the control group.[21] They did not use acupressure or acupuncture for ISE in infertile women.
In our study, no statistically significant difference was observed between the studied groups and pregnancy occurrence. Our results were similar to the results of the studies of Manheimer et al., Cheong et al., and El-Toukhy et al. In a systematic review and meta-analysis of Manheimer et al., no statistically significant difference was observed between acupuncture and control groups with combining trials or limiting the results to control group-sham or the trials without controlled adjuvant therapy, so that in the trials with smaller control group, clinical pregnancy showed more effects from adjuvant acupuncture and vice versa.[22]
Cheong et al. also found no evidence of the overall benefit of acupuncture in improving the rate of live birth regardless of acupuncture during the time of oocyte extract or day of embryo transfer.[16] The results of El-Toukhy et al.'sstudy also suggest that acupuncture during the time of embryo transfer does not make a difference in the rate of clinical pregnancy,[23] while our findings are inconsistent with the results of Zheng et al.'s systematic review and meta-analysis. Their results showed that the rate of common clinical pregnancy of all acupuncture groups was significantly higher than all control groups.[17]
In our study, self-efficacy variables after the intervention, groups, and ovulation factor have affected by the self-efficacy before the intervention. Hence, the real acupressure group had more self-efficacy than the control group but was not statistically significant. The patients with no ovulation as the cause of infertility had more self-efficacy than those with ovulation as the cause of infertility but were not statistically significant. The primary self-efficacy was effective on self-efficacy after the intervention so that primary self-efficacy was effective in reducing self-efficacy after the intervention. No similar study which evaluated the independent variables on self-efficacy of infertile women in acupressure or acupuncture groups was found.
Infertile women participating in this study were in the third decade of life; the women in the studies of Smith et al. and Kovárová et al. were also in their third decade of life.[15,18]
In our study, most participants had university education that was similar to the education of women participating in the study of Kovárová et al.[15] However, in Smith et al.'s study, most women had finished high school education.[18] In our study, the majority of women were not employed; however, in the studies of Smith et al. and Kovárová et al., most women had full-time jobs.[15,18]
The strengths of our study were that the participants did not report any side effects following acupressure. Furthermore, acupressure is an easy and inexpensive method that can be taught to others.
One limitation of this study was lack of similar study about acupressure effect on self-efficacy and occurrence of pregnancy for comparing with our results; however, the results were merely compared with the studies of acupuncture. Another limitation was that in the studies of acupuncture, the effect of self-efficacy on pregnancy occurrence had not been evaluated.
Conclusion
Despite that in our study, acupressure did not statistically improve self-efficacy and pregnancy occurrence in infertile women; however, clinically, the real acupressure group had more self-efficacy followed by acupressure compared with the control group. Finally, according to the results of this study and the lack of similar studies, performing more researches is recommended.
Financial support and sponsorship
This article was derived from a PhD thesis supported by the Deputy of Research of Mashhad University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study was derived from a PhD thesis approved by Mashhad University of Medical Sciences with proposal code of 940238. We wish to thank the Deputy of Research for their financial support. Further, we would like to thank Dr. N. Khadem, Head of Milad IVF Center, and other staff for their cooperation in this research.
References
- 1.Malik SH, Coulson NS. Computer-mediated infertility support groups: An exploratory study of online experiences. Patient Educ Couns. 2008;73:105–13. doi: 10.1016/j.pec.2008.05.024. [DOI] [PubMed] [Google Scholar]
- 2.Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology. 2004;63:126–30. doi: 10.1016/j.urology.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 3.Hatamloye Saedabadi M, Hashemi Nosratabad T. The comparison of psychological well-being and marital satisfaction in the fertile and infertile women. Health Psychol. 2012;1:20–31. [Google Scholar]
- 4.Galhardo A, Cunha M, Pinto-Gouveia J. Measuring self-efficacy to deal with infertility: Psychometric properties and confirmatory factor analysis of the Portuguese version of the infertility self-efficacy scale. Res Nurs Health. 2013;36:65–74. doi: 10.1002/nur.21516. [DOI] [PubMed] [Google Scholar]
- 5.Cousineau TM, Domar AD. Psychological impact of infertility. Best Pract Res Clin Obstet Gynaecol. 2007;21:293–308. doi: 10.1016/j.bpobgyn.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Boivin J, Griffiths E, Venetis CA. Emotional distress in infertile women and failure of assisted reproductive technologies: Meta-analysis of prospective psychosocial studies. BMJ. 2011;342:d223. doi: 10.1136/bmj.d223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hassanin IM, Abd-El-Raheem T, Shahin AY. Primary infertility and health-related quality of life in upper Egypt. Int J Gynaecol Obstet. 2010;110:118–21. doi: 10.1016/j.ijgo.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 8.Cousineau TM, Green TC, Corsini EA, Barnard T, Seibring AR, Domar AD, et al. Development and validation of the infertility self-efficacy scale. Fertil Steril. 2006;85:1684–96. doi: 10.1016/j.fertnstert.2005.10.077. [DOI] [PubMed] [Google Scholar]
- 9.Lawrance L, McLeroy KR. Self-efficacy and health education. J Sch Health. 1986;56:317–21. doi: 10.1111/j.1746-1561.1986.tb05761.x. [DOI] [PubMed] [Google Scholar]
- 10.Coulson C, Jenkins J. Complementary and alternative medicine utilisation in NHS and private clinic settings: A United Kingdom survey of 400 infertility patients. J Exp Clin Assist Reprod. 2005;2:5. doi: 10.1186/1743-1050-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang CH, Lee BH, Sohn SH. A possible mechanism underlying the effectiveness of acupuncture in the treatment of drug addiction. Evid Based Complement Alternat Med. 2008;5:257–66. doi: 10.1093/ecam/nem081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beal MW. Acupuncture and acupressure. Applications to women's reproductive health care. J Nurse Midwifery. 1999;44:217–30. doi: 10.1016/s0091-2182(99)00054-3. [DOI] [PubMed] [Google Scholar]
- 13.Hoseinabadi R, Nourozi K, Pouresmail Z, Karimlu M, Maddah Sadat SB, Cheraghi MA. The effect of acupressure on quality of sleep in Iranian elderly nursing home residents. Complement Ther Clin Pract. 2010;16:81–5. doi: 10.1016/j.ctcp.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 14.Huang MI, Nir Y, Chen B, Schnyer R, Manber R. A randomized controlled pilot study of acupuncture for postmenopausal hot flashes: Effect on nocturnal hot flashes and sleep quality. Fertil Steril. 2006;86:700–10. doi: 10.1016/j.fertnstert.2006.02.100. [DOI] [PubMed] [Google Scholar]
- 15.Kovárová P, Smith CA, Turnbull DA. An exploratory study of the effect of acupuncture on self-efficacy for women seeking fertility support. Explore (NY) 2010;6:330–4. doi: 10.1016/j.explore.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Cheong YC, Dix S, Hung Yu Ng E, Ledger WL, Farquhar C. Acupuncture and assisted reproductive technology. Cochrane Database Syst Rev. 2013;7 doi: 10.1002/14651858.CD006920.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zheng CH, Huang GY, Zhang MM, Wang W. Effects of acupuncture on pregnancy rates in women undergoing in vitro fertilization: A systematic review and meta-analysis. Fertil Steril. 2012;97:599–611. doi: 10.1016/j.fertnstert.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Smith CA, Ussher JM, Perz J, Carmady B, de Lacey S. The effect of acupuncture on psychosocial outcomes for women experiencing infertility: A pilot randomized controlled trial. J Altern Complement Med. 2011;17:923–30. doi: 10.1089/acm.2010.0380. [DOI] [PubMed] [Google Scholar]
- 19.Jamshidimanesh M, Alimanesh N, Behbodi M, Haghani H. Effect of an educational package on self-efficacy of infertile women. Payesh. 2015;2:227–37. [Google Scholar]
- 20.Fleiss JL. Design and Analysis of Clinical Experiments. CanadaJohn Wiley & Sons. 2011 [Google Scholar]
- 21.Pasha H, Faramarzi M, Esmailzadeh S, Kheirkhah F, Salmalian H. Comparison of pharmacological and nonpharmacological treatment strategies in promotion of infertility self-efficacy scale in infertile women: A randomized controlled trial. Iran J Reprod Med. 2013;11:495–502. [PMC free article] [PubMed] [Google Scholar]
- 22.Manheimer E, van der Windt D, Cheng K, Stafford K, Liu J, Tierney J, et al. The effects of acupuncture on rates of clinical pregnancy among women undergoing in vitro fertilization: A systematic review and meta-analysis. Hum Reprod Update. 2013;19:696–713. doi: 10.1093/humupd/dmt026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Toukhy T, Sunkara SK, Khairy M, Dyer R, Khalaf Y, Coomarasamy A, et al. A systematic review and meta-analysis of acupuncture in in vitro fertilisation. BJOG. 2008;115:1203–13. doi: 10.1111/j.1471-0528.2008.01838.x. [DOI] [PubMed] [Google Scholar]