Abstract
BACKGROUND:
Breast cancer is a leading cause of deaths worldwide. In Pakistan, one in every nine women develops breast cancer some time in her life. This high incidence of breast cancer and the poor socioeconomic conditions of Pakistan make breast self-examination (BSE) the best tool for the prevention and early diagnosis of breast cancer. Therefore, the aim of the study was to assess the knowledge, attitude, and practice of BSE among female college students of Karachi, Pakistan.
METHODS:
A cross-sectional study was conducted on 1000 students from June to December 2016. Data were collected using a pre-piloted questionnaire, and SPSS (version 20) was used for data analysis. Chi-square test was used to determine the significance of the difference in knowledge and attitude among participants who had performed BSE and those who had not. A P < 0.05 was considered statistically significant.
RESULTS:
The overall response rate was 90.9%. Although 71.4% of the women knew what BSE was, only 33.1% had performed it. Majority of the participants considered that BSE is important in the early detection of breast cancer. With 59.7% of the population having an adequate amount of knowledge, 87.2% had a positive attitude toward BSE. A medical background was found to be a significant predictor for adequate knowledge and a positive attitude toward BSE.
CONCLUSION:
Despite a positive attitude found among the population toward BSE, its knowledge and practice were inadequate. Educational interventions are required in Pakistan to encourage young women to perform BSE regularly so that breast abnormalities can be detected early on and mortalities can be minimized.
Keywords: Attitude, breast cancer, breast self-examination, college students, knowledge
Introduction
Breast cancer is the leading cause of death in women throughout the world.[1] Progression of breast cancer is more vigorous in younger women, especially of child-bearing age, as compared to older ones,[2] leading to a significant decrease in their survival rate. This increase in mortality is mainly due to late diagnosis of the disease, which is a consequence of lack of knowledge and awareness regarding breast cancer, primarily in the women of developing countries. Early detection of breast cancer increases the effectiveness of the treatment, which results in a better prognosis, reducing the morbidity and mortality rates.[3]
Many methods for detecting breast cancer early-on in its course are now available, of which the most convenient is breast self-examination (BSE). It is inexpensive, simple and does not require any specialized equipment or regular visits to the hospital, thus proving its usefulness in underdeveloped countries too, which lack resources. In addition, performing BSE on a regular basis makes women accustomed to the normal appearance and feel of their breasts and they are able to notice any changes in their breast as soon as they present.[4] About one in every eight women in North America and Western European countries is subject to breast cancer, and one in every 30 women loses her life to this merciless illness.[5] Early detection of breast cancer increased the 5-year survival rate to 85%, while detecting it further on in the course brought the survival rate down to 56%.[6] Therefore, the WHO proposes BSE as a method of immense value for decreasing the mortality rate by early detection of breast cancer,[7] especially in regions where mammography and regular clinical examinations are not feasible. However, despite its numerous advantages, BSE is still practiced on a very low scale, the frequency of which differs among different countries.
The incidence of breast cancer is rising all around the world, particularly in developing countries, where about 60% of all the global deaths occur due to breast cancer.[8] As a matter of fact, one in every nine women in Pakistan develops breast cancer some time in her life.[9] In a place like Pakistan, health-care facilities, such as breast cancer screening, are limited. Due to the deficit in resources and a lack of awareness about breast cancer and its screening modalities, only 9.5% of the urban and 4.8% of the Pakistani female rural population undergo clinical screening.[10] In addition, BSE brings with itself the embarrassment of handling the breasts, which prevents women from addressing their confusions and seeking guidance about how to perform the procedure correctly. Consequently, the disease is associated with high fatality rates as most patients present at later stages when treatment options are limited. Keeping the socioeconomic status of Pakistan in mind, BSE is the method of choice for the early detection of breast cancer, which is why we felt the need to conduct this research in Karachi.
In developing countries like Pakistan, awareness of breast cancer prevention is not well documented, and in places where it is reported, the results are poor[11] with practices of BSE ranging from 19% to 43.2% in Nigeria[5] and 0% to 52% in India.[12,13] This inadequate knowledge is the reason why females have a negative understanding of the prognosis of early detected cancer.[14] Screening is among the best ways to detect cancer at an early stage,[15] and BSE is one of the most satisfactory ways to screen for breast cancer, according to the American Cancer Society.[16] Research shows that performing BSE regularly decreases the rate of breast cancer cases with interfacing axillary lymph nodes by 3.1%.[17] Even with it being a convenient, quick, and inexpensive method, BSE practice rate is still very low. Therefore, the objectives of the study were as follows:
To assess the knowledge, attitude, and practices of BSE in college students
To identify the areas of gap in knowledge and attitude of BSE between students who perform and do not perform BSE
To identify the factors affecting the knowledge and positive attitude scores regarding BSE in students.
Methods
This descriptive cross-sectional study was conducted on female students from June 2016 to December 2016, in six prestigious institutions of Karachi, Pakistan, to assess their knowledge, practices, and attitude regarding BSE. Ethical approval was obtained from the Institutional Review Board of Dow University of Health Sciences.
Data were collected from the universities of both public and private sectors with three institutes having medical-related fields as their major program, whereas the remaining centers were related to engineering and business management. This ensured that students from most of the specialties were covered from all over the city to participate in our study, minimizing the chances of selection bias. Based on the assumption that 35% of the women had substantial knowledge about BSE in a developing country[18] and taking a 5% margin of error and 95% confidence level, the calculated sample size through the formula, n = (DEFF × Np [1 − p])/(d2/Z21-α/2× [N − 1] +p × [1 − p]) (where n = sample size) was 350. This was increased to 1000 to attain maximum representation from the study population. The questionnaires were stored in a safe place with only the authors having access to the data, and no public or published analysis or reports of assessment results identify individuals in such a way that responses, contributions, or analytic results can be attributed to them. Due to sensitivity of the topic, the female target population was approached by female data collectors only.
The target population consisted of all the female participants who wished to take part in the study, without any specific inclusion or exclusion criteria because all females were eligible to take part in the study. Participants were selected on the basis of non-probability convenience sampling. Participation in the study was voluntary. The aim of the study was explained and informed consent taken from each participant; those who were not willing to participate were excluded from the study. The questionnaire was originally produced in English language and was later translated to Urdu so that the participants could fill it in whichever language they found more convenient. It was back-translated to ensure the validity of the questionnaire. Confidentiality was ensured to the respondents and no incentive was proposed to them for participation in the study.
A self-administered research questionnaire, designed after going through several questionnaires from similar published studies,[4,11,19] was formulated as a tool for data collection. It comprised of 38 questions and was divided into four sections. The first section had four questions regarding the sociodemographic characteristics of the participants which included age, marital status, field of education, and the year of education of the students; the second and third sections contained 10 questions of knowledge and attitude each, with one extra question to assess the source of awareness of students, and 13 questions were incorporated in the last section of self-care practices. The questionnaire was pretested in a pilot study among 30 final-year medical students of Dow University of Health Sciences, following which necessary changes were made in the questionnaire and the responses were excluded from the final results. Partially filled forms were excluded from the study and the response rate was calculated accordingly.
Data analysis was performed on IBM-Statistical Package for the Social Sciences version 20. Mean age of the sample was obtained and frequency and percentages for sociodemographic characteristics and self-care practices of students were calculated. The responses to questions regarding the knowledge and attitude of BSE were divided according to the people who had and who had not performed BSE. Overall knowledge was scored out of 10; students scoring above 7, between 5 and 7, and below 5 were said to be substantially aware, partially aware, and not aware, respectively. Attitude, on the other hand, was scored out of 20, labeling a score of 17–20 as high attitude, 10–16 as moderate attitude, and below 10 as low attitude. Chi-square test was used to determine if there was any significant difference of knowledge and attitude between the two groups. A P < 0.05 was taken to be significant. Finally, multivariable logistic regression analysis was used to determine the association of sociodemographic characteristics of the sample with their overall knowledge and attitude regarding BSE, where knowledge and attitude score of <50% was termed as inadequate and low, respectively.
Results
A total of 909 complete questionnaires were received, out of which 541 were from medical colleges, with an overall response rate of 90.9%. As shown in Table 1, almost all of the students (96.3%, n = 875) were unmarried and the mean age of the population was 20.2 ± 1.7 years.
Table 1.
Demographic characteristics (n=909)
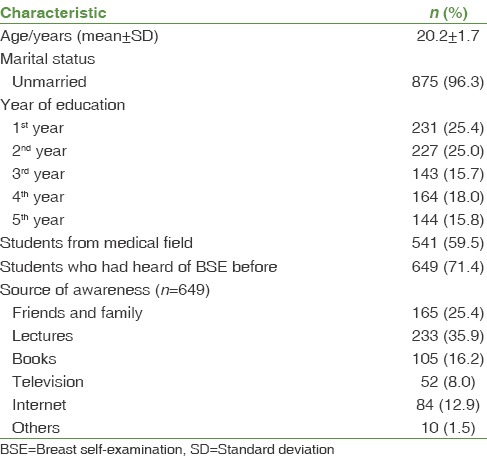
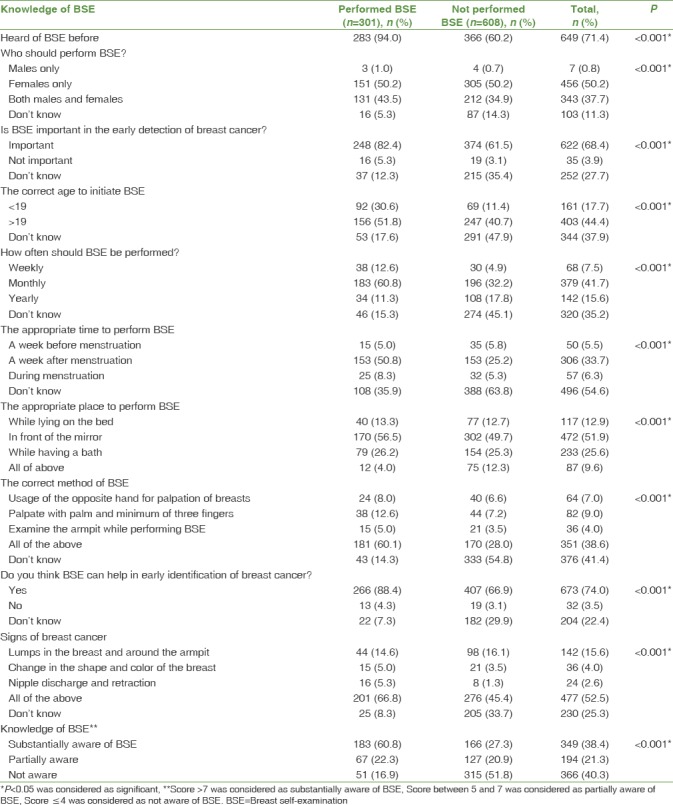
Table 2 compares the overall knowledge between students who had and had not performed BSE. Most of the women (71.4%, n = 649) had heard of BSE and their main source of information was through lectures (35.9%, n = 233) Majority of the students (68.4%, n = 622) acknowledged that BSE is an important tool for the early detection of breast cancer. Roughly only half of the students (44.4%, n = 403) responded correctly that the appropriate age to initiate BSE was >19 years. While 60.8% (n = 183) of those who had done BSE agreed that it should be a monthly routine, only 32.2% (n = 196) of the others approved of that and this difference was significant (P < 0.001). Likewise, while 60.1% (n = 181) of the students who performed BSE knew that the accurate method of BSE is to examine the armpits and palpate with the opposite hand using the palm and a minimum of three fingers, only 28% (n = 170) of the other group agreed with the same and this was a significant difference statistically (P < 0.001). Overall, where majority (60.8%, n = 183) of the students who carried out BSE had a substantial amount of knowledge, only 27.3% (n = 166) of those who did not perform BSE had the same.
Table 2.
Knowledge (n=909)
Majority of the students from both groups revealed a positive attitude (87.1%, n = 792). Table 3 indicates that more of the students who had not performed BSE (24.3%, n = 148) found this practice to be embarrassing in contrast to the students who had performed it (14%, n = 42). This difference was significant (P < 0.001). More than half (55.1%, n = 501) of the respondents did not agree with receiving traditional healing when a lump is identified and about three-fourth (75.8%, n = 689) believed that all women should perform BSE. While 49.2% (n = 148) of the students who had performed BSE were not afraid to think about breast cancer, 41.9% (n = 255) of the students who had not performed were reluctant to think about it. This difference was found to be significant (P < 0.001). Only less than a third (28.7%, n = 261) of the participants were interested in doing BSE.
Table 3.
Attitude (n=909)
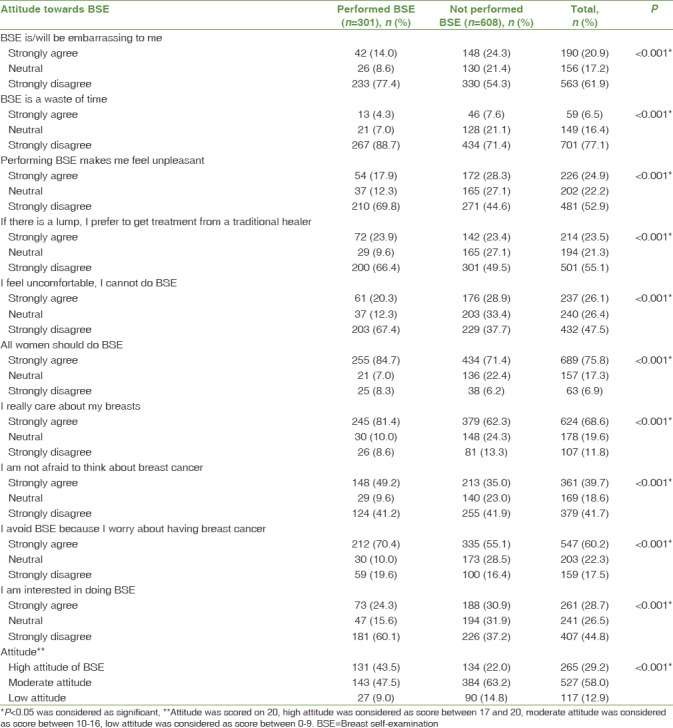
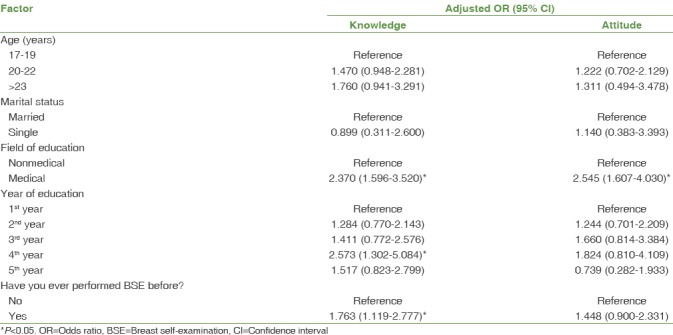
Table 4 shows that only one-third (33.1%, n = 301) of the women in our study had performed BSE previously. This was done predominantly as part of a routine medical checkup (37.2%, n = 112). The major reason why more than half of the population had not performed BSE was simply because they did not know how to perform it (52.1%, n = 317). Out of those who did perform BSE, majority (64.8%, n = 195) preferred to do it on their own. Most of the students (83.4%; n = 251) checked for nipple discharge and any unusual change in the shape and size of the breast during examination. Ultimately, on performing multivariate analysis [Table 5], a medical background, 4th year of education, and performance of BSE in the past were significantly associated (P < 0.05) with adequate knowledge, and a medical background was significantly (P < 0.05) associated with a positive attitude toward BSE.
Table 4.
Practices, (n=301)
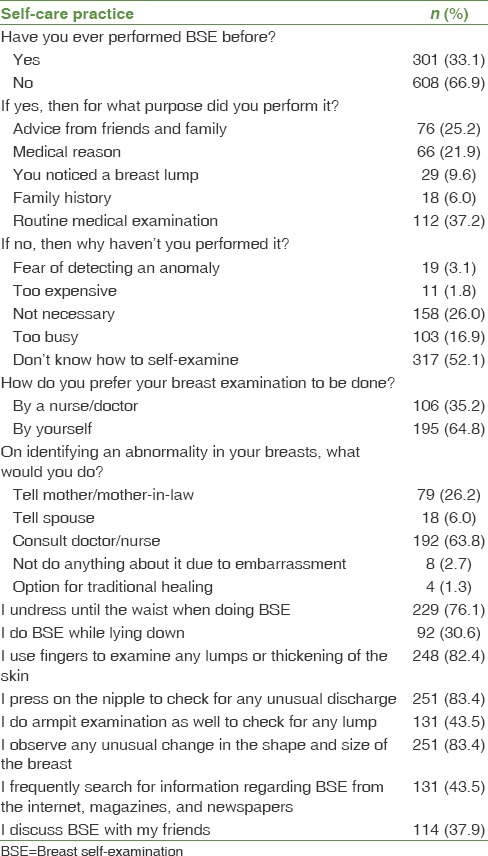
Table 5.
Multivariate logistic regression
Discussion
Since breast cancer is difficult to prevent, it becomes increasingly important to find ways to detect it at an early stage, as that has been shown to improve patient mortality.[20] One of the easiest and safest methods to identify any breast abnormality is BSE, making it essential for all females to be aware of it and to practice it regularly. Females from both medical and non-medical programs were included in the survey as both the population groups are equally at risk of acquiring breast cancer and should not only have adequate knowledge about BSE but should also exhibit a positive attitude, which can help in performing it consistently.
The poor knowledge of almost half of the participants in our study (40.3%) regarding BSE was comparable with the results of a study done in Turkey, where it was seen that only 34.6% of the population was well aware of the procedure of BSE.[4] On the other hand, much better knowledge was observed in a research conducted in Iran (79.8%)[11] and in one conducted by Hacihasanoǧlu and Gözüm (68.1%).[21] In addition, two-thirds of the population in both Iran and Iraq were of the view that the ideal time to perform BSE was after their monthly cycle[11] and before menopause,[22] respectively; while our outcomes showed that only one-third of the females said that it should be performed a week following menstruation. It was also seen that a high percentage (74%) of the students were aware that regular BSE could lead to the early detection of breast cancer. This was in line with a study in Iran that stated that 94.2% of the people agreed that early detection of breast cancer would be helpful in providing a standard life for the affected individual.[11] Likewise, in Nigeria, although only a few women practice BSE, a good proportion (52.3%) of them see BSE as a good screening method for breast cancer.[23] This, along with the results of our research, reflects on the fact that people appreciate the importance of BSE. However, the gap in knowledge in other fields of BSE emphasizes on the need to raise awareness among women about the correct method and timing of BSE.
Despite the lack of proper knowledge, it was encouraging to see that, like in our study (87.2%), a positive attitude toward BSE among females was seen in other parts of the world too, such as in Nigeria (80%)[24] and Shahroud (78%).[25] In contrast, nearly half of the female students interviewed in Jordan (45.5%) agreed that they would examine their breasts if it was beneficial for them.[20] A study conducted in Western Massachusetts also showed a positive attitude among all ethnicities,[26] whereas 75.88% of the participants in Shahrekord had a moderate attitude toward BSE.[27] On the other hand, it was also observed that more than half of the women (60.2%) avoided BSE because they were afraid of having breast cancer, despite the fact that the same percentage of women (61.5%) in Buea, Cameroon, believed the opposite.[19] The observed positive attitude indicates that a majority of the women are inclined toward BSE but have not been provided with the correct knowledge and incentive to practice it. It should be explained that early detection of breast cancer by the frequent practice of BSE is valuable as it could increase their chances of survival through prompt and effective treatment.
Although the attitude was heartening, the practice rates were disappointing, showing that only one-third of the participants performed BSE, a result which was mimicked in studies conducted in Nigeria and Buea, Cameroon, which had practice rates of 19%[28] and 35%,[18] respectively. Nevertheless, extremes of percentages were seen in other places of the world, with 90.3% of the health-care providers in Sau Paulo[17] and only 6% of the respondents in Iran[29] practicing BSE on a regular basis. The result of this research indicates that in our country, the application of BSE in relation with its awareness is higher as compared to many of the other countries. If we focus on enhancing the awareness of BSE further, it would help in increasing the percentage of the population that practices it and hence aids in the early detection of breast cancer. Keeping in mind how various studies have shown that media is the most commonly encountered source of awareness of BSE,[4,23,24] mass media coverage should be given high priority.
Even though our study showed that the majority of the participants (64.8%) preferred to carry out BSE themselves, contrasting results were seen in a study conducted in Iran which showed that almost all of the women (96.7%) preferred to have a female doctor do their breast examination.[11] Since not everyone is skilled to properly perform BSE, it is strongly suggested that at least once, BSE should be done by a medical professional so that potential cases can be picked up at their earliest stage. This would also be beneficial for the general population as medical personnel would be able to teach them the correct method, which in turn would reduce their need to frequently visit the hospital for a checkup and prevent them from missing abnormalities due to incorrect methods.
It was noted that a positive attitude regarding BSE was significantly associated with having prior medical education and the year of education (P < 0.001). These results were aided by the outcome of the investigation conducted in Iran where the contrast between the academic certificate and positive attitude was also significant (P < 0.05).[11] Moreover, in Iran, it was also observed that age and marital status were not associated with a higher level of knowledge, which was revealed in our multivariate analysis as well.[11] However, the study in Ardebil contradicted our results as it showed that age and marital status did have an effect on people's knowledge regarding BSE.[30] Furthermore, it has been proven that the incidence of breast cancer decreases with practicing BSE,[31] and our study shows how higher knowledge is significantly associated with the practice of BSE.
The study has some limitations. The sample includes female students from six colleges only and hence cannot be generalized to the entire population of Pakistan, especially with the use of self-administered questionnaires which may have accounted for the higher level of education only. The participants of the study were enrolled by convenience sampling; random or cluster sampling would have been a better approach to decrease selection bias. Furthermore, the conclusion was based on self-reports only without any objective measures to assess the participants, which might have led to an overestimate of their knowledge. Hence, it is recommended to perform further studies using a larger sample from various cities of Pakistan.
Conclusion
A positive attitude was seen among all the students. However, females who carried out BSE had a better knowledge as opposed to those who did not. Nevertheless, the overall knowledge of our population was low which showed that majority of the women had never performed BSE. Improvement in the knowledge and practice rates of BSE would allow the detection of breast cancer at an early stage which could consequently lower mortality rates. Moreover, this will help females overcome their reservations about freely discussing their concerns about breast cancer and its related issues. Therefore, it is essential to conduct public interventions that increase awareness and encourage women to practice BSE on a regular basis. The lack of resources in breast-screening modalities in Pakistan further highlights the need for such programs. At large, these educational workshops should also emphasize on the correct techniques of BSE so that women are able to apply their knowledge effectively and perform it on a monthly basis. Likewise, all universities, be it medical or otherwise, should also organize similar sessions so that students can have increased awareness regarding BSE at an earlier age.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We acknowledge the contribution of the females who participated in this study and appreciate the efforts of all the students who helped in data collection.
References
- 1.Hortobagyi GN, de la Garza Salazar J, Pritchard K, Amadori D, Haidinger R, Hudis CA, et al. The global breast cancer burden: Variations in epidemiology and survival. Clin Breast Cancer. 2005;6:391–401. doi: 10.3816/cbc.2005.n.043. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg R, Levy-Schwartz R. Breast cancer in women younger than 40 years. Int J Fertil Womens Med. 2003;48:200–5. [PubMed] [Google Scholar]
- 3.Elmore JG, Armstrong K, Lehman CD, Fletcher SW. Screening for breast cancer. JAMA. 2005;293:1245–56. doi: 10.1001/jama.293.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karayurt O, Ozmen D, Cetinkaya AC. Awareness of breast cancer risk factors and practice of breast self examination among high school students in Turkey. BMC Public Health. 2008;8:359. doi: 10.1186/1471-2458-8-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okobia MN, Bunker CH, Okonofua FE, Osime U. Knowledge, attitude and practice of Nigerian women towards breast cancer: A cross-sectional study. World J Surg Oncol. 2006;4:11. doi: 10.1186/1477-7819-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hallal JC. The relationship of health beliefs, health locus of control, and self concept to the practice of breast self-examination in adult women. Nurs Res. 1982;31:137–42. [PubMed] [Google Scholar]
- 7.World Health Organization Regional Office for the Eastern Mediterranean. Towards a Strategy for Cancer Control in the Eastern Mediterranean Region. 1st ed. Cairo: World Health Organization Regional Office for the Eastern Mediterranean; 2010. [Google Scholar]
- 8.Battaglia F, Plotti F, Zullo M, Panici P, Plotti G, Brown L, et al. Gynecologic cancer. Cancer. 2006;16:29–35. [Google Scholar]
- 9.Tfayli A, Temraz S, Abou Mrad R, Shamseddine A. Breast cancer in low- and middle-income countries: An emerging and challenging epidemic. J Oncol 2010. 2010:490631. doi: 10.1155/2010/490631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heartfile. Islamabad, Pakistan: Heartfile, Ministry of Health and World Health Organization; 2006. Population-Based Surveillance of Non-Communicable Diseases: 1st round, 2005. [Google Scholar]
- 11.Reisi M, Javadzade SH, Sharifirad G. Knowledge, attitudes, and practice of breast self-examination among female health workers in Isfahan, Iran. J Educ Health Promot. 2013;2:46. doi: 10.4103/2277-9531.117417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta SK. Impact of a health education intervention program regarding breast self examination by women in a semi-urban area of Madhya Pradesh, India. Asian Pac J Cancer Prev. 2009;10:1113–7. [PubMed] [Google Scholar]
- 13.Yadav P, Jaroli DP. Breast cancer: Awareness and risk factors in college-going younger age group women in Rajasthan. Asian Pac J Cancer Prev. 2010;11:319–22. [PubMed] [Google Scholar]
- 14.Obeidat RF, Lally RM. Health-related information exchange experiences of Jordanian women at breast cancer diagnosis. J Cancer Educ. 2013;11:290. doi: 10.1007/s13187-013-0574-x. [DOI] [PubMed] [Google Scholar]
- 15.Banaian SH, Kazemian A, Soleiman KH. Knowledge, attitude, practice among women referred to health centers in Broojen about screening methods of breast cancer. J Shahrekord Univ Med Sci. 2005;7:28–34. [Google Scholar]
- 16.Harris DM, Miller JE, Davis DM. Racial differences in breast cancer screening, knowledge and compliance. J Natl Med Assoc. 2003;95:693–701. [PMC free article] [PubMed] [Google Scholar]
- 17.Carelli I, Pompei LM, Mattos CS, Ferreira HG, Pescuma R, Fernandes CE, et al. Knowledge, attitude and practice of breast self-examination in a female population of metropolitan São Paulo. Breast. 2008;17:270–4. doi: 10.1016/j.breast.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 18.Suh MA, Atashili J, Fuh EA, Eta VA. Breast self-examination and breast cancer awareness in women in developing countries: A survey of women in Buea, Cameroon. BMC Res Notes. 2012;5:627. doi: 10.1186/1756-0500-5-627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nde FP, Assob JC, Kwenti TE, Njunda AL, Tainenbe TR. Knowledge, attitude and practice of breast self-examination among female undergraduate students in the University of Buea. BMC Res Notes. 2015;8:43. doi: 10.1186/s13104-015-1004-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suleiman AK. Awareness and attitudes regarding breast cancer and breast self-examination among female Jordanian students. J Basic Clin Pharm. 2014;5:74–8. doi: 10.4103/0976-0105.139730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hacihasanoǧlu R, Gözüm S. The effect of training on the knowledge levels and beliefs regarding breast self-examination on women attending a public education centre. Eur J Oncol Nurs. 2008;12:58–64. doi: 10.1016/j.ejon.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 22.Alwan NA, Al-Attar WM, Eliessa RA, Madfaie ZA, Tawfeeq FN. Knowledge, attitude and practice regarding breast cancer and breast self-examination among a sample of the educated population in Iraq. East Mediterr Health J. 2012;18:337–45. doi: 10.26719/2012.18.4.337. [DOI] [PubMed] [Google Scholar]
- 23.Isara AR, Ojedokun CI. Knowledge of breast cancer and practice of breast self examination among female senior secondary school students in Abuja, Nigeria. J Prev Med Hyg. 2011;52:186–90. [PubMed] [Google Scholar]
- 24.Motilewa OO, Ekanem US, Ihesie CA. Knowledge of breast cancer and practice of self-breast examination among female undergraduates in Uyo, Akwa Ibom State, Nigeria. Int J Community Med Public Health. 2015 Nov;2(4):361–366. [Google Scholar]
- 25.Alai Nejad F, Abasian M, Delvarian Zadeh M. Knowledge, attitude and practice of health workers about breast self examination in Shahrood. Knowl Health J. 2007;2:23–7. [Google Scholar]
- 26.Armin J, Torres CH, Vivian J, Vergara C, Shaw SJ. Breast self-examination beliefs and practices, ethnicity, and health literacy: Implications for health education to reduce disparities. Health Educ J. 2014;73:274–84. doi: 10.1177/0017896912471048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Danesh A, Amiri M, Ramezani A, Tazhibi M, Ganji F. Knowledge, attitude, practice among female workers in Shahrekord education organization about breast self examination. J Shahrekord Univ Med Sci. 2002;4:47–52. [Google Scholar]
- 28.Gwarzo UM, Sabitu K, Idris SH. Knowledge and practice of breast-self examination among female undergraduate students of Ahmadu Bello University Zaria, Northwestern Nigeria. Ann Afr Med. 2009;8:55–8. doi: 10.4103/1596-3519.55766. [DOI] [PubMed] [Google Scholar]
- 29.Haji-Mahmoodi M, Montazeri A, Jarvandi S, Ebrahimi M, Haghighat S, Harirchi I, et al. Breast self-examination: Knowledge, attitudes, and practices among female health care workers in Tehran, Iran. Breast J. 2002;8:222–5. doi: 10.1046/j.1524-4741.2002.08406.x. [DOI] [PubMed] [Google Scholar]
- 30.Dadkhah B, Mohammadi M. Knowledge, attitude and practice of women in Ardabil about breast self-examination, 2000. J Ardabil Univ Med Sci. 2002;2:14–20. [Google Scholar]
- 31.Alwan NA, Al-Diwan JK, Wafa'M AA, Eliessa RA. Knowledge, attitude & practice towards breast cancer & breast self examination in Kirkuk University, Iraq. Asian Pac J Reprod. 2012;1:308–11. [Google Scholar]


