Abstract
Background
Interleukin 2 (IL-2) is a cytokine secreted by activated T cells. Studies exploring recombinant human interleukin 2 (rhuIL-2) as an adjunctive immunotherapeutic agent to treat tuberculosis (TB) have shown variable results; however, the true therapeutic efficacy of rhuIL-2 administration in TB patients has not been determined.
Methods
A systematic review to identify publications exploring the association between rhuIL-2-based immunotherapy for TB and outcomes (sputum culture conversion, sputum smear conversion, radiographic changes, and leukocyte phenotype changes) in patients with pulmonary TB published before June 8, 2018 was performed. Data were extracted and analyzed by two investigators independently.
Results
A total of 2,272 records were screened. Four randomized controlled trials (RCTs) comprising 656 pulmonary TB patients were finally included. The rhuIL-2 treatment could significantly improve the sputum culture conversion of TB (RR, 1.18; 95%CI: 1.03–1.36; I2 < 0.01; P = 0.019) after at least 3 months of anti-TB therapy and the sputum smear conversion of TB during anti-TB therapy. Treating multidrug-resistant tuberculosis (MDR-TB) with rhuIL-2 could improve the sputum culture conversion (RR, 1.28; 95%CI: 1.05–1.57; I2 < 0.01; P = 0.016) and smear conversion (RR, 1.28; 95%CI: 1.09–1.51; I2 < 0.01; P = 0.003) at the end of anti-TB treatment. Meanwhile, rhuIL-2-based adjunctive immunotherapy could expand the proliferation and conversion of CD4+ and natural killer (NK) cells. Three of the included studies suggested that radiographic changes could not be improved by the use of rhuIL-2 as adjunctive immunotherapy. Publication bias did not exist.
Conclusions
Based on this first meta-analysis, rhuIL-2-based adjunctive immunotherapy appears to expand the proliferation and conversion of CD4+ and NK cells, as well as improve the sputum culture (at 3 months and later) and smear conversion of TB patients.
Introduction
Tuberculosis (TB) is the most common serious infectious disease and a global health concern caused by Mycobacterium tuberculosis (M. TB) or M. bovis. According to reports published by the World Health Organization (WHO), millions of new TB cases occur each year, causing almost two million deaths annually [1–3]. The occurrence of human immunodeficiency virus (HIV)-associated TB and the growing incidence of multidrug-resistant M. TB (MDR-TB) isolates have generated this emergency. Therefore, it is necessary to develop better control strategies.
For many years, TB has been effectively controlled and cured by the combined chemotherapy of isoniazid, rifampicin, pyrazinamide, and ethambutol, which is recommended by the WHO[4–6]. However, adverse events (e.g., long-term administration, toxicity, and intolerance) are always accompanied with the chemotherapy. On the other hand, MDR-TB, defined as isolates resistant to both isoniazid and rifampicin with or without resistance to other anti-TB drugs, causes significant problems and constitutes an increasing public health concern globally [7–9].
Interleukin 2 (IL-2), a cytokine secreted by activated T cells, promotes the differentiation and proliferation of lymphoid cells as well as enhances the cell-mediated immune response to infections [10]. Therefore IL-2 has been used as an adjunctive immunotherapeutic agent to control some infectious diseases, such as leishmaniasis, leprosy, and HIV infection [11–13]. Beginning in 1988, several studies have demonstrated that IL-2 administration in murine mycobacteria models could limit the course of mycobacterial infection [14–16]. In 1995, Johnson et al. found that recombinant human IL-2 (rhuIL-2) administration in combination with conventional multidrug therapy (MDT) is safe and may potentiate the antimicrobial cellular immune response to TB [17]. Meanwhile, several clinical studies have suggested that rhuIL-2 administered as an adjunct to conventional MDT to TB patients could induce immune activation and enhance the antimicrobial response, with significant improvement in the rate of conversion of sputum smears [18–20]. It also has been reported that IL-2 administration may increase T cell regulatory activity and facilitate bacilli proliferation [21]. However, others have reported that daily treatment with rhuIL-2 during the first month of TB management did not enhance bacillary clearance or improve symptoms in patients with drug-susceptible TB [22]. The balance between the management cost and patient benefits should also be carefully pondered [23]. Many reviews have paid attention to the use of rhuIL-2 as an adjunctive immunotherapeutic agent to treat TB [23–26]. However, the true therapeutic efficacy of rhuIL-2 administration in TB patients has not been determined.
Here, we report the systematic review and meta-analysis for the therapeutic efficacy of rhuIL-2 administration in the management of TB.
Material and methods
This meta-analysis was performed following the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA).
Search strategy and data sources
The electronic databases (PubMed, Cochrane Library, EMBASE, and Web of Science) were searched by two investigators (HML and XYX) independently without language restriction from their inception until June 8, 2018. The search terms included “interleukin 2” OR “IL-2” OR “rhuIL-2” OR “recombinant human IL-2” AND “tuberculosis” OR “mycobacterium tuberculosis infection” OR “tuberculous lesion” OR “tuberculoses” OR “Kochs Disease” AND “randomized controlled study” OR “controlled clinical study” OR “randomized” OR “placebo” OR “randomly.”
Study selection
The inclusion criteria for this study were as follows: (1) patients who were diagnosed with HIV-seronegative TB or with culture-confirmed M. TB or M. bovis; (2) rhuIL-2 was applied as adjunctive immunotherapy; (3) the clinical trial was a randomized controlled trial (RCT); (4) outcomes of the clinical trial included sputum culture, sputum smear, radiographic changes, and leukocyte phenotype changes.
The exclusion criteria for this study were as follows: (1) review, conference summary, or case report; (2) basic research; (3) studies involving children or pregnant woman; (4) duplicate studies.
Data extraction
Data were extracted from the included studies by two investigators (CHG and SZ) independently. The first author, publication year, study population, age, sex ratio, dosage, time of rhuIL-2 use, sputum culture, sputum smear, radiographic changes, and leukocyte phenotype changes were collected using a predesigned electronic form.
Any key absent information was requested from the authors by e-mail. Studies were excluded if we did not get any response from the authors.
Quality assessment
Two investigators (LYZ and HML) independently reviewed all of the studies and assessed the methodological quality and risk of bias for each eligible study by the Cochrane Collaboration tool [27]. The sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other potential bias were included.
Statistical analyses
The data were analyzed using STATA v12.0 statistical software by two investigators (HML and RMZ) independently. For dichotomous variables (sputum culture, sputum smear, and radiographic changes), the relative risk (RR) and 95% confidence interval (CI) for each study were calculated. For continuous variables (leukocyte phenotype changes), the standard mean difference was calculated.
Heterogeneity was estimated by the I2 and the χ2 tests. The random-effects model was used when a significant heterogeneity (p ≤ 0.10 for the χ2 test or I2 ≥ 50%) was observed; otherwise, the fixed-effects model was applied. Both the Mantel-Haenszel test and inverse-variance weighting were used.
Publication bias was evaluated by a funnel plot. The z test was applied to determine the significance of the pooled index. P ≤ 0.05 was considered statistically significant.
Results
Literature search
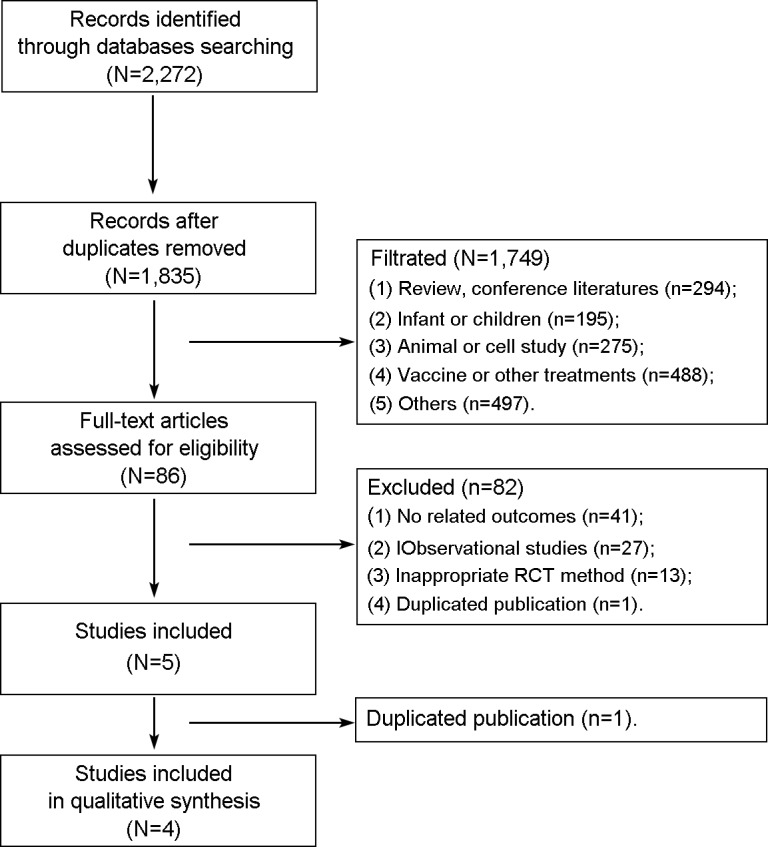
A total of 2,272 records were identified during the initial electronic database search. The information for primary exclusion is presented in Fig 1. After duplicates were removed, 1,835 records remained. Then, 1,749 records were excluded for different reasons, and 84 studies were analyzed. After reading the full texts, 81 studies were excluded, and 5 studies were included. However, the study performed by Shen et al. was also excluded because it was confirmed by one of the authors to be a duplicate study [20]. Finally, four studies (n = 656 patients) that met the inclusion criteria were included in this meta-analysis [28–30,18].
Fig 1. Flow diagram of the study selection process.
Patient characteristics
The demographics of the patients are summarized in Table 1. All of the patients were HIV seronegative and had TB as determined by culture-confirmed M. TB. The study performed by Chu et al. did not provide the detailed demographic information of the included patients [30]. The mean age of the included patients in the other three studies ranged from 35.0 to 44.2 years. Patients were diagnosed with pulmonary TB [30,29] or MDR-TB, which was defined as culture-confirmed M. TB resistant to isoniazid and rifampicin [18,28]. However, 85 patients had MDR-TB in the study performed by Chu et al. [30]. Two studies focused on newly diagnosed TB [28,29], while the other two studies analyzed retreatment for TB [18,30]. There were 114 relapsing cases in the study performed by Tan et al. [28]. None of the included studies provided clear comorbidities. One study was conducted in Uganda [29], one study was conducted in South Africa [18], and two studies were from China [28,30].
Table 1. Patient demographics of the included trials.
| Source | Tan et al. [28] | Johnson et al. [29] | Chu et al. [30] | Johnson et al. [18] |
|---|---|---|---|---|
| Year of publication | 2017 | 2003 | 2003 | 1997 |
| Size (n) | 302 | 110 | 209 | 35 |
| Gender (M/F) | 168/134 | 75/35 | Unclear | 18/17 |
| Age (years) | 44.2 | 35.0 a | Unclear | 36.6 |
| Disease | MDR-TB | TB | TB b | MDR-TB |
| Initial drug resistance | Isoniazid and rifampin | No | No | Isoniazid and rifampin |
| New or retreatment | New, relapse | New | Retreatment | Retreatment |
| HIV | Seronegative | Seronegative | Seronegative | Seronegative |
| Comorbidities | Unclear | Unclear | Unclear | Unclear |
| Center | 14 multicenter | Single center | Unclear | Single center |
| Region | China | Uganda | China | South Africa |
M/F: male/female; TB: tuberculosis; MDR-TB: multidrug-resistant tuberculosis; HIV: human immunodeficiency virus.
a median.
b 85 patients were MDR-TB.
Treatment protocols
All of the included patients were randomly divided into the intervention or control group. The protocols of treatment are shown in Table 2. All of the included patients received chemotherapy. The drug doses were adjusted according to the patient weight. Treatment assignments were masked to the clinical and laboratory staff.
Table 2. Protocols of rhuIL-2 treatment.
| Source | Tan et al. [28] | Johnson et al. [29] | Chu et al. [30] | Johnson et al. [18] |
|---|---|---|---|---|
| Year of publication | 2017 | 2003 | 2003 | 1997 |
| Intervention group | ||||
| -Source | China | Canada | China | Canada |
| -Beginning time | After inclusion and allocation | After inclusion and allocation | After inclusion and allocation | After inclusion and allocation |
| -Delivery method | Subcutaneous injection | Intradermal injection | Intradermal injection | Intradermal injection |
| -Bolus dose | 50 × 104 U/mL | 225,000 IU | 200,000 IU |
DRG: 225,000 IU PRG: 450,000 IU |
| - Schedule | Once every other day for 30 days separately during months 1, 3, 5, and 7. | Twice daily during the first 30 days of anti-TB treatment | Once daily for 30 days, followed by 30 days 'rest', for two cycles. |
DRG: Twice daily for 30 consecutive days PRG: Daily at 12-h intervals for 5 days, followed by 9 days 'rest', for three cycles. |
| -Therapy period | 7 months | 30 days | 90 days | 30 days |
| Control group | Background drug regimen (chemotherapy) | Standard short-course chemotherapy with sterile 5% dextrose | Standard chemotherapy | Standard chemotherapy with diluent |
TB: tuberculosis; DRG: Daily rhuIL-2 groups; PRG: Pulse-therapy rhuIL-2 group.
Patients in the control group received an optimized anti-TB chemotherapy regimen with or without diluents. Separate from the chemotherapy, patients in the rhuIL-2 group received rhuIL-2 treatment, after inclusion and allocation.
Patients in the intervention group were treated with rhuIL-2. However, the treatment protocols in the four studies were slightly different. First, the source of rhuIL-2 was different. Two studies used rhuIL-2 that was produced in China [30,28], while two studies used proleukin, which was from Chiron Corp, Canada [18,29]. Second, the method of rhuIL-2 delivery was different. One study adopted subcutaneous injection [28], and three studies used intradermal injection [20,29,18,30]. Third, the bolus dose was different. Two different bolus doses (225,000 IU and 450,000 IU) of rhuIL-2 were used in the study performed by Johnson et al. [18], while the other studies used a dose of 200,000 IU [30], 225,000 IU [29], or 50 × 104 U/mL [28]. Fourth, the schedule of rhuIL-2 was different. Last, the length of rhuIL-2 therapy was different, ranging from 30 days to 8 months.
Methodological quality and risk of bias
The quality and bias of the included studies are shown in Table 3. All studies were randomized. Both a computer-generated randomization sequence and a table of random numbers were adopted to avoid selection bias. Two studies did not report the method of sequence generation [20,28]. Two studies used a centrally assigned method and a block size of 10 to avoid allocation bias [29,28]. Two studies applied blinding methods [20,29]. Placebos were used as a control in all studies.
Table 3. Quality and bias of the included trials.
| Source | Tan et al. [28] | Johnson et al. [29] | Chu et al. [30] | Johnson et al. [18] |
|---|---|---|---|---|
| Year of publication | 2017 | 2003 | 2003 | 1997 |
| Selection bias | ||||
| - Sequence generation | Unclear | Computer- generated | Computer-generated | Table of random numbers |
| - Allocation concealment | Centrally assigned method | Block size of 10 | Low Risk | Low Risk |
| Performance and detection bias | ||||
| - Blinding of participants and personnel | Low Risk | Double-blind | High Risk | High Risk |
| - Blinding of outcome assessment | Low Risk | Double-blind | High Risk | High Risk |
| Incomplete outcome data addressed | Low Risk | Low Risk | Low Risk | Low Risk |
| Selective reporting | Low Risk | Low Risk | Low Risk | Low Risk |
| Other bias | Low Risk | Low Risk | Low Risk | Low Risk |
Sputum culture conversion
All four of the included studies reported the sputum culture, which was assessed at different stages (from 1 to 24 months) of anti-TB treatment [30,29,18,28]. Sputum samples were cultured by different methods, such as the BACTECTM broth culture system [18,29] and Lowenstein–Jensen solid medium in a Mycobacterium Growth Indicator Tube [28].
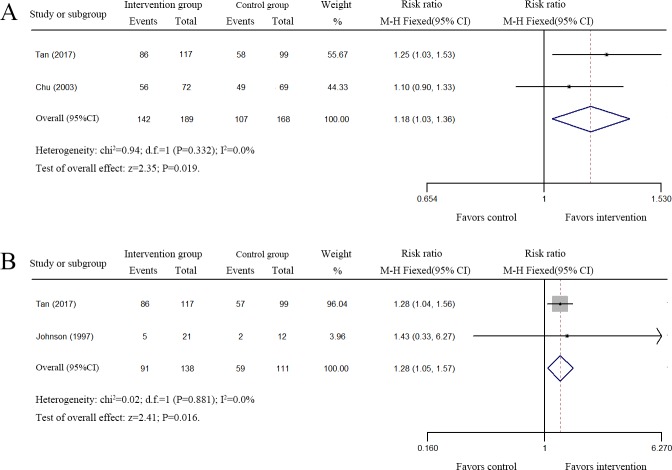
Two studies comprising 235 patients reported that rhuIL-2 treatment did not improve the sputum culture conversion after the first 2 months of anti-TB treatment (S1 and S2 Tables) [30,29]. In contrast, two studies comprising 357 patients reported that rhuIL-2 treatment did improve the sputum culture conversion at the third month of anti-TB treatment (RR, 1.18; 95%CI: 1.03–1.36; I2 < 0.01; P = 0.019) (Fig 2A, S1 and S2 Tables) [28,30]. In 2017, Tan et al. found that patients in the rhIL-2 group achieved sputum culture conversion at the end of 6, 12, 18, and 24 months of treatment, significantly higher than that of the patients in the control group (S1 Table) [28]. In 1977, Johnson et al. reported that conversion from a positive culture at the start of the study to a negative culture at the end of rhuIL-2 treatment occurred in four daily treated patients, in one pulse-treated patient, and in two placebo-treated patients [18].
Fig 2. Forest plots of the effect of rhuIL-2 treatment on sputum culture conversion.
A. Meta-analysis of the sputum culture conversion at the third month of anti-TB treatment. B. Meta-analysis of the sputum culture conversion of MDR-TB patients at the end of anti-TB treatment. Weights are calculated from both fixed and random effects models.
A pooled analysis to assess the changes in the sputum culture conversion of the MDR-TB patients at the end of anti-TB therapy was also performed. Two eligible studies comprising 249 MDR-TB patients were assessed [18,28]. As shown in Fig 2B, rhuIL-2 treatment did improve the sputum culture conversion of MDR-TB patients (RR, 1.28; 95%CI: 1.05–1.57; I2 < 0.01; P = 0.016).
Together, these results suggested that rhuIL-2 treatment could significantly improve the sputum culture conversion of TB patients treated for at least 3 months and improve the sputum culture conversion of MDR-TB patients at the end of anti-TB therapy.
Sputum smear conversion
Three studies comprising 446 patients reported the sputum smear, which was assessed by direct microscopy at different stages (from 1 week to 24 months) of anti-TB treatment (S3 Table) [30,18,28].
In 1977, Johnson et al. reported that there was a decreasing trend of a positive rate of sputum smear in the MDR-TB patients receiving continuous daily rhuIL-2 therapy [18]. In 2003, Chu et al. suggested that the sputum smear conversion was increased at the end of 1–2 months of treatment with rhuIL-2 [30]. In 2017, Tan et al. found that patients in the rhIL-2 group achieved sputum smear conversion at the end of 6, 12, 18, and 24 months of treatment, notably higher than that of patients in the control group [28]. At 3 months of anti-TB therapy, the rate of sputum smear conversion was slightly increased by rhuIL-2 treatment in the studies conducted by Tan et al. (69.23% vs. 59.60%) and Chu et al. (82.52% vs. 78.00%) [28,30].
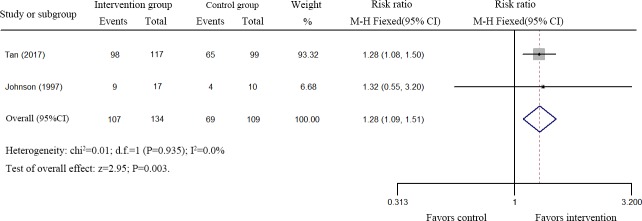
Two eligible studies comprising 249 MDR-TB patients were assessed [18,28]. As shown in Fig 3, rhuIL-2 treatment improved the sputum culture conversion of MDR-TB patients (RR, 1.28; 95%CI: 1.09–1.51; I2 < 0.01; P = 0.003) at the end of anti-TB treatment.
Fig 3. Forest plots of the effect of rhuIL-2 treatment on sputum smear conversion of MDR-TB patients.
Together, these results suggest that rhuIL-2 treatment could increase the sputum smear conversion of TB patients as well as improve the sputum smear conversion of MDR-TB patients at the end of anti-TB therapy.
Radiographic changes
Four studies comprised 547 patients reported the rate of radiographic changes, which was assessed by chest imaging as their diagnostic criteria, during anti-TB treatment [20,29,18,30]. As shown in S4 Table, both the number of repeated times and radiographic response definitions were different. Due to this reason, pooled data analysis was not performed.
Three of the four studies revealed that treatment with rhuIL-2 as adjunctive immunotherapy did not improve the radiographic changes of TB patients (S5 Table) [29,18,30]. In 2017, Tan et al. found that rhIL-2 treatment did improve the lung focus resolution of TB patients, but it did not affect the lung cavity closure (S5 Table) [28].
Based on the above results, we conclude that radiographic changes may not be improved by rhuIL-2 as an adjunctive immunotherapeutic agent.
Leukocyte phenotype changes
Leukocyte phenotypes were stained with the corresponding monoclonal antibodies and analyzed by flow cytometry at different time points in all of the included studies. However, pooled data analysis was not performed.
In 1977, Johnson et al. reported that daily rhuIL-2 treatment could increase the mean number of circulating natural killer (NK) cells (CD16+/CD56+) at the post-study timepoint, compared to the baseline NK cell numbers in the MDR-TB patients [18]. In 2003, Johnson et al. reported that the median percentage of CD4+/CD25+ T lymphocytes was greater after 2 and 6 weeks of anti-TB treatment in subjects receiving rhulL-2 than in those receiving placebo [29]. In the same year, Chu et al. suggested that compared with baseline measurements, rhuIL-2 treatment significantly increased the mean numbers of CD4+ and NK cells as well as the percentages of CD4+/CD8+ cells at 3 and 7 months [30]. In 2017, Tan et al. found that rhIL-2 treatment increased the percentages of CD3+CD8-interferon (IFN)-γ+ and CD4+CD25+Foxp3+ cells as well as decreased the percentage of CD3+CD8-IL-17+ cells compared to those in the control group at 6 months and 12 months (S6 Table) [28].
From the above results, we concluded that rhuIL-2 treatment could promote the proliferation and conversion of leukocytes.
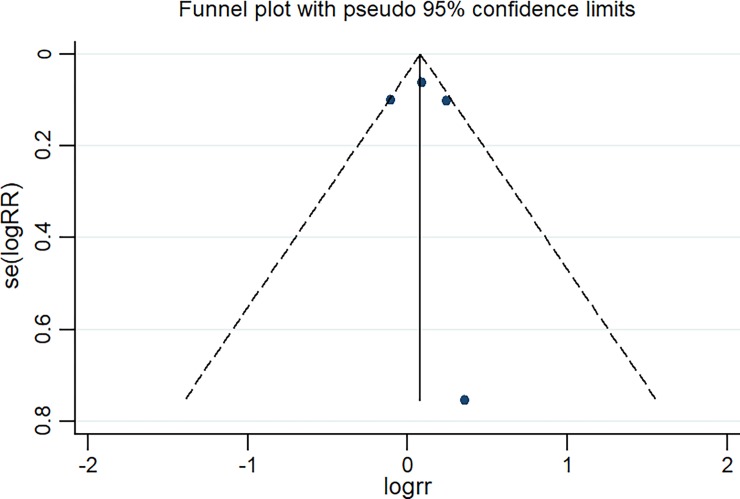
Publication bias
Publication bias was evaluated by a funnel plot. As shown in Fig 4, a funnel plot of the sputum culture conversion was established, and there was no publication bias (z = 0.34 [continuity corrected], Pr > |z| = 0.734 > 0.05).
Fig 4. Funnel plot of the four eligible studies that reported sputum culture conversion in pulmonary tuberculosis patients.
Discussion
In the past 30 years, IL-2-based adjunctive immunotherapy has attracted increasing attention. To the best of our knowledge, this is the first systemic review and meta-analysis to explore the effect of adjunctive therapy with rhuIL-2 during the treatment of patients with TB. Four clinical RCT studies comprising 656 pulmonary TB patients were included in this study. No publication bias existed. Pooled data analysis showed that treatment of TB patients with rhuIL-2 expanded the proliferation and conversion of CD4+ and NK cells as well as improved the sputum culture (at 3 months and later) and smear conversion of TB. Unfortunately, rhuIL-2 treatment did not enhance the radiographic changes.
Recent studies have proven that protective immunity against M. TB is based on cell-mediated immunity involving CD4 and CD8 T cells [31–33]. It is widely accepted that CD4 T cells play an important role in protective immunity against TB by secreting IFN-γ, tumor necrosis factor-α, and IL-2 [34–36]. However, the contribution of CD8 T cells to immunity against TB is still under debate. Some research suggests that CD8 T cells have a significant role in the control of M. TB infection [37–39], whereas others disagree [40–42]. Many studies have suggested that the use of IL-2 in vitro can restore some of the anti-bacterial reactivity of T cells [43]. In this study, we demonstrated that rhuIL-2-based adjunctive immunotherapy could expand the proliferation and conversion of CD4+ cells, but it did not affect the changes of CD8+ T cells.
NK cells are specialized lymphocytes of the innate immune system that are activated during the early response to pulmonary TB through NK cell-derived IFN-γ, which differentially regulates T cell-independent resistance and granulocyte function in M. TB infection [44–46]. Many studies have shown that IL-2 can augment the cytotoxic activity of NK cells [47]. We report here that the NK cell count was increased by rhuIL-2 treatment.
Based on the above results, we conclude that rhuIL-2-based adjunctive immunotherapy can expand the proliferation and conversion of CD4+ and NK cells, improve the function of host immunity, and manipulate the evolution and progression of pulmonary TB.
A negative acid fast bacilli test result in both the sputum smear and culture is a widely accepted technique to determine the effectiveness of treatment and the infectivity of a pulmonary TB patient [48–50]. Sputum smear- and culture-negative conversion rates are considered as prognostic markers of anti-TB treatment [51–53]. In this study, both sputum smear and culture conversion were assessed at different months of treatment. Three of the included trials reported that the sputum smear-negative conversion rates were significantly improved by rhuIL-2 treatment [30,18,28]. Meanwhile, rhuIL-2 treatment for at least 3 months significantly improved the sputum culture conversion of TB patients [28,29,18,30]. However, it has been reported that rhuIL-2 treatment did not enhance bacillary clearance in HIV-seronegative adults with drug-susceptible TB [29].
We also found that rhuIL-2 treatment could improve the sputum smear and culture conversion rates of MDR-TB patients in two of the included studies [18,28]. Therefore, the sputum smear and culture conversion rates could be improved by treating TB patients with rhuIL-2.
Pulmonary TB always produces a broad spectrum of radiographic abnormalities. Chest X-ray is the primary radiologic evaluation method for suspected or confirmed pulmonary TB [54]. In this meta-analysis, all of the included studies applied chest X-ray to evaluate the resolution of TB lesions during anti-TB therapy [29,18,30,28]. We found that rhlL-2 treatment did not increase the rate of chest radiographic improvement in pulmonary TB patients. However, the most recent study found that patients receiving rhIL-2 tended to have a greater improvement of focus resolution in the short term, compared to those in the control group at the end of anti-TB therapy [28]. More research is required to confirm these findings.
Study limitations
Several important limitations regarding this study should be noted. First, the patients came from China, Uganda, and South Africa. Therefore, the representation and reliability of the results are poor. Second, we did not evaluate some prospective observational studies that involved rhuIL-2-based adjunctive immunotherapy on TB patients. Third, the protocols of rhuIL-2 intervention (rhuIL-2 source, beginning times, delivery methods, dosages, schedules, and therapy period) of rhuIL-2 were different in each study. Fourth, many methods were used among the studies. For example, one study did not clearly state the randomization methods, and only one study was performed in a double-blind manner, while the remaining three were not. Finally, the diagnostic criteria of the radiographic changes were not unified.
Given these findings, more prospective RCTs with a large sample size and a strict design are necessary in future studies.
Conclusions
Treating TB with rhuIL-2 could expand the proliferation and conversion of CD4+ and NK cells as well as improve the sputum culture (at 3 months and later) and smear conversion of TB. However, rhuIL-2 treatment did not enhance the radiographic changes. Large scale, well-designed, multicenter clinical trials are necessary in the future.
Supporting information
(PDF)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
(PDF)
Acknowledgments
We acknowledge Prof. Dadong Liu’s kind help in providing language help, writing assistance and data analysis.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Zumla A, George A, Sharma V, Herbert RH, Baroness Masham of I, Oxley A, et al. The WHO 2014 global tuberculosis report—further to go. Lancet Glob Health. 2015; 3(1): e10–12. 10.1016/S2214-109X(14)70361-4 [DOI] [PubMed] [Google Scholar]
- 2.Vashishtha VM. WHO Global Tuberculosis Control Report 2009: Tuberculosis elimination is a distant dream. Indian Pediatr. 2009; 46(5): 401–402. [PubMed] [Google Scholar]
- 3.Dye C, Scheele S, Dolin P, Pathania V, Raviglione MC. Consensus statement. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. WHO Global Surveillance and Monitoring Project. JAMA. 1999; 282(7): 677–686. [DOI] [PubMed] [Google Scholar]
- 4.Villemagne B, Crauste C, Flipo M, Baulard AR, Deprez B, Willand N. Tuberculosis: the drug development pipeline at a glance. Eur J Med Chem. 2012; 51(1–16. [DOI] [PubMed] [Google Scholar]
- 5.Mdluli K, Kaneko T, Upton A. The tuberculosis drug discovery and development pipeline and emerging drug targets. Cold Spring Harb Perspect Med. 2015; 5(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dobbs TE, Webb RM. Chemotherapy of Tuberculosis. Microbiol Spectr. 2017; 5(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoffner S. Multidrug-resistant tuberculosis: The problem and some priorities in controlling it. Int J Mycobacteriol. 2016; 5 Suppl 1(S59. [DOI] [PubMed] [Google Scholar]
- 8.Yew WW, Leung CC. Management of multidrug-resistant tuberculosis: Update 2007. Respirology. 2008; 13(1): 21–46. 10.1111/j.1440-1843.2007.01180.x [DOI] [PubMed] [Google Scholar]
- 9.Lee SK, Tan KK, Chew SK, Snodgrass I. Multidrug-resistant tuberculosis. Ann Acad Med Singapore. 1995; 24(3): 442–446. [PubMed] [Google Scholar]
- 10.Kelso A, MacDonald HR, Smith KA, Cerottini JC, Brunner KT. Interleukin 2 enhancement of lymphokine secretion by T lymphocytes: analysis of established clones and primary limiting dilution microcultures. J Immunol. 1984; 132(6): 2932–2938. [PubMed] [Google Scholar]
- 11.Akuffo H, Kaplan G, Kiessling R, Teklemariam S, Dietz M, McElrath J, et al. Administration of recombinant interleukin-2 reduces the local parasite load of patients with disseminated cutaneous leishmaniasis. J Infect Dis. 1990; 161(4): 775–780. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan G, Britton WJ, Hancock GE, Theuvenet WJ, Smith KA, Job CK, et al. The systemic influence of recombinant interleukin 2 on the manifestations of lepromatous leprosy. J Exp Med. 1991; 173(4): 993–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Teppler H, Kaplan G, Smith KA, Montana AL, Meyn P, Cohn ZA. Prolonged immunostimulatory effect of low-dose polyethylene glycol interleukin 2 in patients with human immunodeficiency virus type 1 infection. J Exp Med. 1993; 177(2): 483–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeevan A, Asherson GL. Recombinant interleukin-2 limits the replication of Mycobacterium lepraemurium and Mycobacterium bovis BCG in mice. Infect Immun. 1988; 56(3): 660–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bermudez LE, Young LS. Tumor necrosis factor, alone or in combination with IL-2, but not IFN-gamma, is associated with macrophage killing of Mycobacterium avium complex. J Immunol. 1988; 140(9): 3006–3013. [PubMed] [Google Scholar]
- 16.Bermudez LE, Stevens P, Kolonoski P, Wu M, Young LS. Treatment of experimental disseminated Mycobacterium avium complex infection in mice with recombinant IL-2 and tumor necrosis factor. J Immunol. 1989; 143(9): 2996–3000. [PubMed] [Google Scholar]
- 17.Johnson BJ, Ress SR, Willcox P, Pati BP, Lorgat F, Stead P, et al. Clinical and immune responses of tuberculosis patients treated with low-dose IL-2 and multidrug therapy. Cytokines Mol Ther. 1995; 1(3): 185–196. [PubMed] [Google Scholar]
- 18.Johnson BJ, Bekker LG, Rickman R, Brown S, Lesser M, Ress S, et al. (1997) rhuIL-2 adjunctive therapy in multidrug resistant tuberculosis: a comparison of two treatment regimens and placebo. Tubercle and lung disease 78 (3–4):195–203 [DOI] [PubMed] [Google Scholar]
- 19.Chu NH, Zhu LZ, Yie ZZ, Yuan SL, Wang JY, Xu JL, et al. [A controlled clinical study on the efficacy of recombinant human interleukin-2 in the treatment of pulmonary tuberculosis]. Zhonghua Jie He He Hu Xi Za Zhi. 2003; 26(9): 548–551. [PubMed] [Google Scholar]
- 20.Shen H, Min R, Tan Q, Xie W, Wang H, Pan H, et al. (2015) The beneficial effects of adjunctive recombinant human interleukin-2 for multidrug resistant tuberculosis. Archives of Medical Science 11 (3):584–590. 10.5114/aoms.2015.52362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin CH, Hunig T. Efficient expansion of regulatory T cells in vitro and in vivo with a CD28 superagonist. Eur J Immunol. 2003; 33(3): 626–638. 10.1002/eji.200323570 [DOI] [PubMed] [Google Scholar]
- 22.Johnson JL, Ssekasanvu E, Okwera A, Mayanja H, Hirsch CS, Nakibali JG, et al. Randomized trial of adjunctive interleukin-2 in adults with pulmonary tuberculosis. Am J Respir Crit Care Med. 2003; 168(2): 185–191. 10.1164/rccm.200211-1359OC [DOI] [PubMed] [Google Scholar]
- 23.Bini EI, Hernandez-Pando R. New chemotherapy and immunotherapy for tuberculosis. Current Respiratory Medicine Reviews. 2014; 10(2): 74–87. [Google Scholar]
- 24.Neelam R, Subhas S, Ram Mohan Gupta V, Devanna N, Pati Nikunja B. A review on new approaches and current therapies involved in the treatment and prophylaxis of tuberculosis. International Research Journal of Pharmacy. 2012; 3(12): 46–50. [Google Scholar]
- 25.Dheda K, Schwander SK, Zhu B, van Zyl-Smit RN, Zhang Y. The immunology of tuberculosis: From bench to bedside. Respirology. 2010; 15(3): 433–450. 10.1111/j.1440-1843.2010.01739.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rao NA. New drugs in resistant tuberculosis. Journal of the Pakistan Medical Association. 2007; 57(5): 252–256. [PubMed] [Google Scholar]
- 27.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011; 343(d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan Q, Min R, Dai GQ, Wang YL, Nan L, Yang Z, et al. Clinical and Immunological Effects of rhIL-2 Therapy in Eastern Chinese Patients with Multidrug-resistant Tuberculosis. Sci Rep. 2017; 7(1): 17854 10.1038/s41598-017-18200-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Johnson JL, Ssekasanvu E, Okwera A, Mayanja H, Hirsch CS, Nakibali JG, et al. (2003) Randomized trial of adjunctive interleukin-2 in adults with pulmonary tuberculosis. American journal of respiratory and critical care medicine 168 (2):185–191. 10.1164/rccm.200211-1359OC [DOI] [PubMed] [Google Scholar]
- 30.Chu NH, Zhu LZ, Yie ZZ, Yuan SL, Wang JY, Xu JL, et al. A controlled clinical study on the efficacy of recombinant human interleukin-2 in the treatment of pulmonary tuberculosis. Chin J Tuberc Respir Dis. 2003; 26(9): 548–551. [PubMed] [Google Scholar]
- 31.Jones BE, Young SM, Antoniskis D, Davidson PT, Kramer F, Barnes PF. Relationship of the manifestations of tuberculosis to CD4 cell counts in patients with human immunodeficiency virus infection. Am Rev Respir Dis. 1993; 148(5): 1292–1297. 10.1164/ajrccm/148.5.1292 [DOI] [PubMed] [Google Scholar]
- 32.Green AM, Difazio R, Flynn JL. IFN-gamma from CD4 T cells is essential for host survival and enhances CD8 T cell function during Mycobacterium tuberculosis infection. J Immunol. 2013; 190(1): 270–277. 10.4049/jimmunol.1200061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Prezzemolo T, Guggino G, La Manna MP, Di Liberto D, Dieli F, Caccamo N. Functional Signatures of Human CD4 and CD8 T Cell Responses to Mycobacterium tuberculosis. Front Immunol. 2014; 5(180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Darrah PA, Patel DT, De Luca PM, Lindsay RW, Davey DF, Flynn BJ, et al. Multifunctional TH1 cells define a correlate of vaccine-mediated protection against Leishmania major. Nat Med. 2007; 13(7): 843–850. 10.1038/nm1592 [DOI] [PubMed] [Google Scholar]
- 35.Caccamo N, Guggino G, Joosten SA, Gelsomino G, Di Carlo P, Titone L, et al. Multifunctional CD4(+) T cells correlate with active Mycobacterium tuberculosis infection. Eur J Immunol. 2010; 40(8): 2211–2220. 10.1002/eji.201040455 [DOI] [PubMed] [Google Scholar]
- 36.Mattila JT, Diedrich CR, Lin PL, Phuah J, Flynn JL. Simian immunodeficiency virus-induced changes in T cell cytokine responses in cynomolgus macaques with latent Mycobacterium tuberculosis infection are associated with timing of reactivation. J Immunol. 2011; 186(6): 3527–3537. 10.4049/jimmunol.1003773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okada H, Kalinski P, Ueda R, Hoji A, Kohanbash G, Donegan TE, et al. Induction of CD8+ T-cell responses against novel glioma-associated antigen peptides and clinical activity by vaccinations with {alpha}-type 1 polarized dendritic cells and polyinosinic-polycytidylic acid stabilized by lysine and carboxymethylcellulose in patients with recurrent malignant glioma. J Clin Oncol. 2011; 29(3): 330–336. 10.1200/JCO.2010.30.7744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Billeskov R, Vingsbo-Lundberg C, Andersen P, Dietrich J. Induction of CD8 T cells against a novel epitope in TB10.4: correlation with mycobacterial virulence and the presence of a functional region of difference-1. J Immunol. 2007; 179(6): 3973–3981. [DOI] [PubMed] [Google Scholar]
- 39.Chen CY, Huang D, Wang RC, Shen L, Zeng G, Yao S, et al. A critical role for CD8 T cells in a nonhuman primate model of tuberculosis. PLoS Pathog. 2009; 5(4): e1000392 10.1371/journal.ppat.1000392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Pinxteren LA, Cassidy JP, Smedegaard BH, Agger EM, Andersen P. Control of latent Mycobacterium tuberculosis infection is dependent on CD8 T cells. Eur J Immunol. 2000; 30(12): 3689–3698. [DOI] [PubMed] [Google Scholar]
- 41.Urdahl KB, Liggitt D, Bevan MJ. CD8+ T cells accumulate in the lungs of Mycobacterium tuberculosis-infected Kb-/-Db-/- mice, but provide minimal protection. J Immunol. 2003; 170(4): 1987–1994. [DOI] [PubMed] [Google Scholar]
- 42.Leveton C, Barnass S, Champion B, Lucas S, De Souza B, Nicol M, et al. T-cell-mediated protection of mice against virulent Mycobacterium tuberculosis. Infect Immun. 1989; 57(2): 390–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gaffen SL, Liu KD. Overview of interleukin-2 function, production and clinical applications. Cytokine. 2004; 28(3): 109–123. 10.1016/j.cyto.2004.06.010 [DOI] [PubMed] [Google Scholar]
- 44.Yoneda T, Kasai M, Ishibashi J, Nishikawa K, Tokunaga T, Mikami R. NK cell activity in pulmonary tuberculosis. Br J Dis Chest. 1983; 77(2): 185–188. [DOI] [PubMed] [Google Scholar]
- 45.Junqueira-Kipnis AP, Kipnis A, Jamieson A, Juarrero MG, Diefenbach A, Raulet DH, et al. NK cells respond to pulmonary infection with Mycobacterium tuberculosis, but play a minimal role in protection. J Immunol. 2003; 171(11): 6039–6045. [DOI] [PubMed] [Google Scholar]
- 46.Feng CG, Kaviratne M, Rothfuchs AG, Cheever A, Hieny S, Young HA, et al. NK cell-derived IFN-gamma differentially regulates innate resistance and neutrophil response in T cell-deficient hosts infected with Mycobacterium tuberculosis. J Immunol. 2006; 177(10): 7086–7093. [DOI] [PubMed] [Google Scholar]
- 47.Granucci F, Zanoni I, Pavelka N, Van Dommelen SL, Andoniou CE, Belardelli F, et al. A contribution of mouse dendritic cell-derived IL-2 for NK cell activation. J Exp Med. 2004; 200(3): 287–295. 10.1084/jem.20040370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kurbatova EV, Gammino VM, Bayona J, Becerra MC, Danilovitz M, Falzon D, et al. Predictors of sputum culture conversion among patients treated for multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2012; 16(10): 1335–1343. 10.5588/ijtld.11.0811 [DOI] [PubMed] [Google Scholar]
- 49.Liu Z, Shilkret KL, Ellis HM. Predictors of sputum culture conversion among patients with tuberculosis in the era of tuberculosis resurgence. Arch Intern Med. 1999; 159(10): 1110–1116. [DOI] [PubMed] [Google Scholar]
- 50.Guler M, Unsal E, Dursun B, Aydln O, Capan N. Factors influencing sputum smear and culture conversion time among patients with new case pulmonary tuberculosis. Int J Clin Pract. 2007; 61(2): 231–235. 10.1111/j.1742-1241.2006.01131.x [DOI] [PubMed] [Google Scholar]
- 51.Dominguez-Castellano A, Muniain MA, Rodriguez-Bano J, Garcia M, Rios MJ, Galvez J, et al. Factors associated with time to sputum smear conversion in active pulmonary tuberculosis. Int J Tuberc Lung Dis. 2003; 7(5): 432–438. [PubMed] [Google Scholar]
- 52.Kim TC, Blackman RS, Heatwole KM, Kim T, Rochester DF. Acid-fast bacilli in sputum smears of patients with pulmonary tuberculosis. Prevalence and significance of negative smears pretreatment and positive smears post-treatment. Am Rev Respir Dis. 1984; 129(2): 264–268. [PubMed] [Google Scholar]
- 53.Kurbatova EV, Cegielski JP, Lienhardt C, Akksilp R, Bayona J, Becerra MC, et al. Sputum culture conversion as a prognostic marker for end-of-treatment outcome in patients with multidrug-resistant tuberculosis: a secondary analysis of data from two observational cohort studies. Lancet Respir Med. 2015; 3(3): 201–209. 10.1016/S2213-2600(15)00036-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ryu YJ. Diagnosis of pulmonary tuberculosis: recent advances and diagnostic algorithms. Tuberc Respir Dis (Seoul). 2015; 78(2): 64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
(DOC)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.