Abstract
Introduction
Type 2 diabetes is a significant problem among uninsured patients. Shared medical appointments (SMA) have been shown to improve outcomes in type 2 diabetes. We hypothesized that the SMA model could be adapted for a non-profit clinic in North Carolina that serves uninsured patients with diabetes that have incomes at/below 150% of the federal poverty line.
Research Design and Methods
We implemented and sustained a patient-driven, student-led SMA model that incorporated the monthly rotations of students, physician assistant, and undergraduate students as well as pharmacy residents and an endocrinologist who collectively provide diabetes care at the free clinic. SMA groups are ‘open’ cohorts and include 4–12 patients scheduled for the monthly clinic. Teams of transdisciplinary trainees work together to perform triage, medication reconciliation, brief history, and physical exam, after which patients participate in the SMA. The endocrinologist evaluates SMA patients individually during and after the visit.
Results
Between November 2015 and January 2017, we enrolled 29 patients in SMA. There was high variability in HbA1c at baseline. Among eight type 2 diabetes patients seen in endocrine clinic and with complete data one year before and after SMA implementation, the mean (SD) HbA1c before SMA was 9.7% ± 1.7% (83±7 mmol/ mol); mean HbA1c after SMA was 9.2% ± 1.8% (77 ± 8mmol/mol). The median HbA1c before SMA was 9.5% (80 mmol/mol); median HbA1c after SMA was 8.9% (74 mmol/mol). Overall, 6/8 patients showed decreased HbA1c after SMA although there was variability between individuals in response of glycemic control to SMA. SMA increased clinic efficiency and offered an opportunity to integrate transdisciplinary trainees. Trainees gain experience with novel models of care and the complexities of the patient experience of diabetes.
Conclusions
We hope this observation encourages others to implement such programs to enhance the evidence-base for SMA to address health disparities and increase the quality of free diabetes care.
Keywords: Type 2 diabetes, Shared medical appointments, Interdisciplinary, Free clinic
Introduction
Type 2 diabetes mellitus is a nationwide epidemic affecting 29.1 million people, or 9.3 percent of the US population [1], including many underserved patients in rural settings who are more likely to be uninsured, or underinsured, and more likely to defer care for financial reasons [2]. Currently, clinics in North Carolina struggle with the high burden and prevalence of type 2 diabetes in uninsured populations. This indication is concerning as the prevalence of both diseases and the burden of the associated complications continues to rise; the number of older US adults with diabetes is estimated to reach 68 million, or 25 percent of the population, by 2030 [3]. Thus, there is a compelling need to improve the quality of diabetes care in free clinics in order to prevent adverse outcomes and the associated economic burden of T2DM [4].
Shared medical appointments (SMA), which integrate group-based education with primary care visits, have been shown to improve outcomes in type 2 diabetes [5,6]. Recently, a growing body of literature has emphasized positives outcomes of SMA for patients with diabetes, including fewer emergency department visits and hospitalizations, improved glycemic control, improved diabetes knowledge and health behavior, and increased patient satisfaction [5]. Specifically, the SMA integrates group-based diabetes self-management education and training along with a primary care visit, which is thought to enhance peer support, increase motivation and medical adherence, and decrease disease distress [7].
We hypothesized the SMA model could be adapted for a nonprofit clinic that serves ~750 uninsured patients with incomes at/below 150% of the federal poverty level. Patients requiring endocrinology consultation are referred to an internal, monthly clinic, which offers infrastructure and resources for diabetes care but suffers from the common weaknesses of free clinics, including long wait times, complicated social histories, and limited time for patient education and discussion2. Our objective was to increase patient engagement and improve health outcomes in this underserved patient population by transitioning from the traditional clinical model to the patient-driven SMA model.
Research Design and Methods
Clinical structure
Prior to SMA implementation, each patient was seen under a traditional clinical model, with an individual appointment every three months unless otherwise indicated [8]. Under this traditional approach, patients were pulled from the waiting room, triaged by a PA or nursing student, and then placed in an individual exam room. Once in the exam room, the patient was seen by a pharmacy resident and a medical student for history and physical and then by the attending endocrinologist for their appointment. With this approach, patients typically waited between 30 and 120 minutes to see the endocrinologist for a standard 15-minute encounter.
To increase efficiency and patient-provider interactions, we implemented the SMA model.
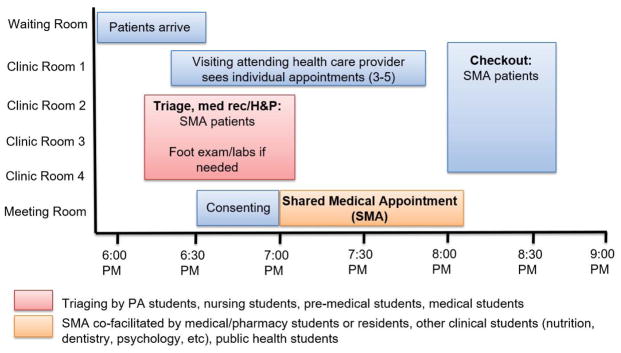
The basic flow of the SMA model includes elements of an individual patient visit, such as the collection of vital signs, history and physical exam, medication adjustments, referrals, and laboratory procedures related to diabetes care, but then adds the group education and interactive component to the visit. The need to integrate all components of an individual medical appointment with the 60–90 minute group discussion was challenging. In response to this challenge, we developed transdisciplinary teams to expedite patient intake. Teams— comprised of physician assistant, medical, nursing, and pharmacy trainees— worked together to perform triage, medication reconciliation, brief history, and physical exam, after which patients participated in the SMA (Figure 1). Students performed skills for which they had received prior training in their professional training. For example, physician assistant students took patient vitals, pharmacist residents performed medical reconciliation, and medical students took history and physicals. The SMA discussion is typically mediated by a medical student with optional contribution from undergraduate students, nursing students, and pharmacy residents after patient triage is complete. The SMA discussion is entirely patient-led. Our role was to integrate teach-points on topics including pathogenesis, complications, understanding laboratory values, healthy nutrition, physical activity, and engagement, consistent with standards of care and patient materials provided by the American Diabetes Association when opportunities arose during discussion {Association, 2018 #4706}. The endocrinologist evaluates SMA patients individually during and after the visit.
Figure 1. SMA model to maximize transdisciplinary student skills.
The basic flow of the SMA model includes elements of an individual patient visit, such as the collection of vital signs, history and physical exam, medication adjustments, referrals, and laboratory procedures related to diabetes care, but then adds the group education and interactive component to the visit. Prior to beginning the SMA, all patients signed informed consent. At the end of the SMA, patients are individually seen by the attending endocrinologist for medical management and check out. The SMA lasts approximately 60–90 minutes and is predominantly student-led. The SMA may run simultaneously with individual appointments where the provider can see individual appointments as a student leads the SMA. A patient may be flagged for individual appointment for non-diabetes endocrinology care or non-English speaking.
Implementation methods
Prior to each clinic, multidisciplinary teams were briefed about the clinic flow and trained in patient handoffs. The model has been sustained over several cycles of rotating students. As an opt-out model, our SMA groups are ‘open’ cohorts in which all patients who were scheduled for the evening clinic were directed to SMA for default. Each monthly SMA includes 4–12 patients scheduled for the monthly clinic. Our study included all patients with physician-diagnosed type 2 diabetes* and an HbA1c > 6.5%. Patients who were not primary English speakers and patients with endocrine referrals not related to diabetes (i.e. hyperthyroidism) were excluded from the SMA.
We documented group visit attendance in medical charts using a standard template. All participants provided informed consent. The study was approved by Institutional Review Board at the University of North Carolina at Chapel Hill.
Statistical methods
To separate the effect of SMA from potential confounding due to newly established endocrinology care, we compared outcomes before and after SMA among patients with type 2 diabetes who received specialized care throughout the entire study period. For these patients, we performed retrospective chart review extending through January 2015 to collected HbA1c measures up to 12 months prior to SMA enrollment. All patients had previously been seen by an endocrinologist specialist prior to SMA and continued to see an endocrinologist after SMA. As a result, the only change in their standard of care was the SMA visit instead of a traditional clinic visit. We collected measures of SMA through January of 2017. For data analysis, we compared HbA1c measures from 12 months prior to SMA with HbA1c measures 12 months following SMA using boxplots and comparing individuals’ ranges before and after SMA.
Results
The first SMA was held in November 2015. Between November 2015 and January 2017, we consented and enrolled 29 patients in SMA. These patients were a mix of patients seen within the endocrine clinic and those who were newly referred from primary care. Eight patients had complete retrospective data for evaluation. Supplemental Table S1 depicts follow-up time, the number of HbA1c measures, and HbA1c outcomes pre- and post- SMA intervention. In general, opt-out rates were low (<20%). Patients opted out if they were unable to stay for the SMA, if they had a significant other with them, or if they were concerned about privacy.
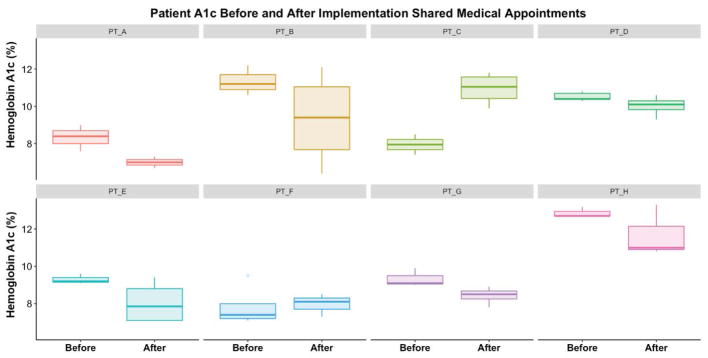
Table 1 depicts characteristics and HbA1c measures collected from eight patients with type 2 diabetes seen in the endocrinology clinic and with complete data one year before and after SMA implementation. Baseline HbA1c was variable. The mean (SD) HbA1c before SMA was 9.7% ± 1.7% (83 ± 7 mmol/mol); mean HbA1c after SMA was 9.2% ± 1.8% (77 ± 8mmol/mol). The median HbA1c before SMA was 9.5% (80 mmol/mol); median HbA1c after SMA was 8.9% (74 mmol/mol). Overall, 6/8 patients showed decreased HbA1c after SMA although HbA1c was variable within individuals (Figure 2). Comparison of median and interquartile measures demonstrates high between-person variability in response of glycemic control to SMA.
Table 1.
Participant Characteristics and Hemoglobin A1c Measures Pre- and Post- Shared Medical Appointment.
| Characteristics, n (%) | |
|---|---|
| Female, n (%) | 5 (63%) |
| Non-Hispanic White, n (%) | 2 (25%) |
| Pre-Shared Medical Appointment, mean (SD) | |
| Retrospective follow-up time (days) | 260 (72) |
| Number of HbA1c measures | 3.4 (0.9) |
| HbA1c (%) | 9.7 (1.6) |
| Post-Shared Medical Appointment, mean (SD) | |
| Prospective follow-up time (days) | 285 974.6) |
| Number of HbA1c measures | 3.6 (0.5) |
| HbA1c (%) | 9.2 (1.4) |
Abbreviations: SD = Standard Deviation; HbA1c = Hemoglobin A1c.
Figure 2. Distribution of HbA1c measures from 6 months pre- and post- exposure to SMA across 10 patients with type 2 diabetes.
Patients were seen for specialized endocrinology care and had continuous follow-up data one year before and after SMA enrollment. Mean (SD) HbA1c before SMA was 9.7% ± 1.7% (83±7 mmol/mol); mean HbA1c after SMA was 9.2% ± 1.8% (77 ± 8mmol/mol).
Discussion
We have implemented a SMA model to serve uninsured patients with type 2 diabetes at a free clinic. We discuss the impact of SMA on diabetes outcomes, clinic efficiency, and trainee experiences.
Meta analyses have shown a modest effect of SMA on HbA1c that is variable across interventions [5]. There is evidence that the effect may be negligible in uninsured populations [9]. Our pilot data suggests high between-patient variability but indicates a favorable effect. Of note, even small improvements in glycemic control may translate to decreased rates of diabetic complications and avoidable patient medical expenses among Alamance County adult residents, as each 1% HbA1c reduction is associated with a 21% reduction in diabetes-related death risk, 14% reduction in heart attacks, and 37% reduction in microvascular (diabetes-related kidney disease, amputations, and blindness) [10].
The SMA was acceptable to clinic staff, where there were minimal disruptions to scheduling procedures (all patients were scheduled for the same time), check in (patients are queried if they could like to participate in the SMA or an individual appointment), and check out procedures. This SMA model accommodated a higher number of patients per monthly clinic individual appointments (approximately 10– 12 versus 6–8 total patients per clinic, respectively). Under a traditional model and a 3-hour clinic, physicians would need to see a patient every 15-minutes to accommodate a patient load of 10–12 people. This level of efficiency is often not feasible with uninsured patients with several comorbidities and barriers to health. Moreover, in a SMA model patients spend less time isolated in waiting rooms and instead time with providers is maximized. The SMA increased time for education and emphasizes patient-directed discussion as compared to individual appointments.
Through work in teams and exposure to patient narratives in the SMA, trainees involved in SMA gained experience with novel models of care, the challenges of diabetes care, and the complexities of the patient experience of diabetes. Critically, the SMA discussion component can be led by trainees, which allows for the inclusion of inter-professional trainees from a breath of clinical or public health programs who are able to discuss and address numerous behavioral changes and interventions that may otherwise be missed in a traditional medical appointment.
A limitation of the SMA is the open-cohort model. Open cohort means that that all patients who were scheduled for the clinic were enrolled in SMA; there were not closed groups that met consistently at regular intervals. A closed cohort would simplify statistical analyses and facilitate the use of structured educational materials, the utility of which is limited with a variable mix of old and new patients in each visit. However, our SMA model reflects the challenges of real-life implementation, in which patients may be scheduled in clinic at different intervals, attendance is variable, and the SMA needed to accommodate all patients schedule for the standing clinic.
Limitations of this work included the small number of patients for whom outcome measurements were available, which reflects the limited number of patients seen per month at the clinic and the challenges associated with providing free medical care, including loss-to-follow-up and inconsistent attendance [2]. Future studied are needed to explore the efficacy of student-led SMA at larger settings including free clinics or community health centers, including potential confounders and modifiers of the effect. In addition, there was no control group of individuals with type 2 diabetes who did not participate in the SMA, as the SMA was an opt out model. To address this limitation in analysis, we collected retrospective data in a matched study design so that each individual could serve as their own control with regards to testing the effect of SMA. Patients were seeing the essentially same set of UNC volunteer physician providers before and after SMA, so standards of practice of care likely did not change.
Small sample sizes also prohibit complex statistical modeling, including adjustments for confounders or longitudinal studies. We propose that our matched study design is adequate to control for individual characteristics that may confound the effect of SMA on HbA1c, as each individual serves as their own control. Although our pilot study was designed to evaluate the aggregate effect of SMA on HbA1c, it would be helpful to explore the medication and behavior changes that may modify or mediate these effects in the future.
The results may be affected by selection bias. We enrolled 29 patients but included 8 in this analysis for whom there was complete retrospective data available to facilitate a matched study design. Therefore, participants in our study may not be representative of patients for whom there was not retrospective data available. Finally, we did not collect data to evaluate student knowledge of diabetes, communication skills, satisfaction; structured informant interviews would be useful to qualitatively assess these aspects in future work.
Strengths of the study included the development, implementation, and evaluation of a novel model for diabetes care in a free clinic. The study of SMA in a free clinic carries significant implications for increasing the quality of care for underserved patients with type 2 diabetes, a vulnerable patient population. Moreover, our analysis was designed to isolate the effect of SMA from the effects of initiating specialized diabetes care. We provide a multi-faceted report to suggest that implementing SMA for type 2 diabetes at a free clinic may be effective for patient outcomes as well as overall clinic efficiency and student educational experiences.
Conclusions
Our pilot data suggests that we have increased clinic efficiency and modestly improved health outcomes among uninsured patients via implementation of a patient-driven, student-led SMA model. We predict that SMA may be effectively tailored to leverage clinic- and patient-specific features to increase the quality of free diabetes care [6]. Moreover, we show that SMA may be an educational opportunity to integrate transdisciplinary students in the free-clinic context to offer improved outcomes. This model may be extended to other student-run clinics to address public health issues such as diabetes, prediabetes, and other cardiovascular disease risk factors among underserved patients. We hope this observation encourages others to implement such programs to enhance the evidence-base for SMA to address health disparities.
Supplementary Material
Acknowledgments
The authors have no conflicts of interest to disclose. ARK and NFB were supported as 2016–2017 Albert Schweitzer Fellows. This work supported by the NC Albert Schweitzer Fellowship and 1UL1TR001111 from the Clinical and Translational Science Award program of the National Center for Advancing Translational Sciences, NIH. ARK is supported by funding from the National Institute of Diabetes and Digestive and Kidney Disease of the National Institutes of Health under Award Number F30DK113728. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of North Carolina at Chapel Hill (1). REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources. This work was made possible by significant contribution from student volunteers and staff at the free clinic [12].
Footnotes
- A hemoglobin A1c (HbA1c) level of 6.5% or higher; the test should be performed in a laboratory using a method that is certified by the National Glycohemoglobin Standardization Program (NGSP) and standardized or traceable to the Diabetes Control and Complications Trial (DCCT) reference assay, or
- A fasting plasma glucose (FPG) level of 126 mg/dL (7 mmol/L) or higher; fasting is defined as no caloric intake for at least 8 hours, or
- A 2-hour plasma glucose level of 200 mg/dL (11.1 mmol/L) or higher during a 75-g oral glucose tolerance test (OGTT), or
- A random plasma glucose of 200 mg/dL (11.1 mmol/L) or higher in a patient with classic symptoms of hyperglycemia (ie, polyuria, polydipsia, polyphagia, weight loss) or hyperglycemic crisis [11].
References
- 1.Prevention CfDCa. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States. 2014. [Google Scholar]
- 2.Mallow JA, Theeke LA, Barnes ER, Whetsel T, Mallow BK. Free Care Is Not Enough: Barriers to Attending Free Clinic Visits in a Sample of Uninsured Individuals with Diabetes. doi: 10.4236/ojn.2014.413097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trebak F, Alaoui A, Alexandre D, El Ouezzani S, Anouar Y, Chartrel N, et al. Impact of aflatoxin B1 on hypothalamic neuropeptides regulating feeding behavior. Neurotoxicology. 2015;49:165–173. doi: 10.1016/j.neuro.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Edelman D, Gierisch JM, McDuffie JR, Oddone E, Williams JW. Shared medical appointments for patients with diabetes mellitus: a systematic review. Journal of general internal medicine. 2015;30:99–106. doi: 10.1007/s11606-014-2978-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramdas K, Darzi A. Adopting Innovations in Care Delivery—The Case of Shared Medical Appointments. The New England journal of medicine. 2017;376:1105–1107. doi: 10.1056/NEJMp1612803. [DOI] [PubMed] [Google Scholar]
- 7.Burke RE, O’Grady ET. Group visits hold great potential for improving diabetes care and outcomes, but best practices must be developed. Health Aff (Millwood) 2012;31:103–9. doi: 10.1377/hlthaff.2011.0913. [DOI] [PubMed] [Google Scholar]
- 8.Chamberlain JJ, Rhinehart AS, Shaefer CF, Neuman A. Diagnosis and Management of Diabetes: Synopsis of the 2016 American Diabetes Association Standards of Medical Care in DiabetesSynopsis of the 2016 ADA Standards of Medical Care in Diabetes. Annals of internal medicine. 2016;164:542–552. doi: 10.7326/M15-3016. [DOI] [PubMed] [Google Scholar]
- 9.Mallow JA, Theeke LA, Barnes ER, Whetsel T. Examining dose of diabetes group medical visits and characteristics of the uninsured. Western journal of nursing research. 2015;37:1033–1061. doi: 10.1177/0193945914529190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes care. 2010;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.